Abstract
Young men who have sex with men are disproportionately affected by HIV/AIDS, yet relatively little is known about the most effective theoretical frameworks for preventive interventions with this population. This study investigated the fit of the Information-Motivation-Behavioral Skills (IMB) model for predicting sexual risk among a sample of ethnically diverse young men who have sex with men aged 14-21. Path analysis results indicated that the IMB model predicted a moderate amount of variance in primary and secondary sexual risk for young men who have sex with men (r2 = .26 and .21, respectively). Fit of this model was acceptable on most indicators of model fit for primary and secondary risk.
Keywords: youth, HIV, sexual risk, Information-Motivation-Behavior Skills Model
Estimates from the Centers for Disease Control and Prevention (CDC, 2009) indicate more than 56,000 adolescents ages 13-24 were living with HIV/AIDS in 2006—and nearly 20,000 new HIV infections occur among young people each year (Hall et al., 2008). The problem of HIV/AIDS among youth may be much greater, however, since fewer than 25% of sexually active high school students are tested for HIV/AIDS, which could leave thousands more young people currently infected but unaware of their status (CDC, 2009).
Men who have sex with men (adolescents and adults) are the risk group that has been most severely affected by the HIV/AIDS epidemic as well as the only group with increasing HIV infection rates (CDC, 2010). Infection rates among young men who have sex with men (YMSM) ages 13-24 are roughly 10 times higher than those of the MSM community overall, with YMSM accounting for more than half of all HIV/AIDS cases among youth (Agwu & Ellen, 2009). Among YMSM, youth of color are at even greater risk, with African American YMSM in particular experiencing a 15% increase in HIV infections between 2003-2006 (Agwu & Ellen, 2009).
To curb these high infection rates we need new effective interventions that are anchored in health behavior theory and appropriate for this particular youth population. However, we need to know more about which conceptual models have greatest utility for predicting HIV-related risk behaviors among YMSM.
One explanatory model for reducing HIV risk behaviors that has potential with this population is the Information-Motivation- Behavioral skills (IMB) model (Fisher & Fisher, 1992). This model posits that individuals will initiate and maintain HIV preventive behaviors if they are well-informed, are motivated to prevent HIV infection, and perceive themselves as possessing the behavioral skills to act successfully (Fisher, Willcutts, Misovich, & Weinstein, 1998). According to the model, HIV prevention information and motivation each have a direct effect on behavior as well as a combined effect through behavioral skills.
The IMB model represents an extension of other individual-level health behavior models that have been used in HIV prevention research. Perceived preventive skills are included from Social Cognitive Theory (Bandura, 1986), and the IMB model's motivation component combines the constructs of attitudes and social norms from the Theory of Reasoned Action (Fishbein & Ajzen, 1975). As noted by Fisher, Fisher, Williams, and Malloy (1994), although other models (e.g., AIDS Risk Reduction Model) have identified information, motivation and skills as key factors in HIV prevention, the IMB model represents “the first attempt to specify the specific linkages among these constructs and to suggest methods for applying an information, motivation, behavioral skills conceptualization to design AIDS-prevention interventions” (p. 241).
The IMB model has shown promise with young adult (Kiene & Barta, 2006; Mustanski, Donenberg & Emerson, 2006) and adult (Anderson et al., 2006; Crosby et al., 2008) populations in the U.S. as well as internationally (Cornman, Schmiege, Bryan, Benziger & Fisher, 2007; Kalichman et al., 2006). Findings of studies using the IMB model with ethnic minority youth suggest that the model is robust for urban youth of color. The model explained 75% of the variance in HIV risk behaviors in a study of ethnic minority high school males drawn from a geographical area with high rates of adolescent HIV infection (Fisher, William, Fisher, & Malloy, 1999), and in a study of urban minority high school youth (Bryan, Fisher & Fisher, n.d., as cited in Fisher & Fisher, 2000). Previous studies of HIV risk with sexual minority youth that included some of the IMB constructs found that safer sexual behaviors were associated with perceptions of social norms (Rotheram-Borus, Marelich & Srinivasan, 1999; Rosario, Mahler, Hunter, & Gwadz (1999), self-efficacy (Rotheram-Borus, Reid, Rosario & Kasen, 1995; Rotheram-Borus, Marelich & Srinivasan, 1999), behavioral intentions and prevention skills (Rosario, Mahler, et al., 1999), and positive attitudes toward safer sex (Rotheram-Borus et al., 1995).
Studies investigating the IMB model among adult MSM have reported mixed results, particularly with regard to the constructs of HIV prevention information and behavioral skills self-efficacy. Some studies have reported that, despite the robust associations found among IMB model variables, information was not a consistent predictor of sexual risk behavior among adult MSM (Fisher & Fisher, 1992; Kalichman, Picciano & Roffman, 2008). The direct effect of the skills self-efficacy construct has been supported by most studies with MSM (e.g., deVroom, deWit & Sandfort, 1996, as cited in Fisher & Fisher, 2000; Fisher & Fisher, 1992; Kalichman et al., 2008) but not all (Benotsch et al., 2007).
There are no known studies that have empirically tested the IMB model with YMSM. Given that YMSM are different from both heterosexual youth and adult MSM in ways that may have important implications for HIV prevention, it is necessary to assess the fit of the IMB model for this population. If the IMB model is predictive of HIV-related sexual risk reduction behaviors among YMSM, it can be used as a theoretical framework for new intervention development using the IMB constructs (information, motivation, perceived behavioral skills) as key intervention targets. This paper, therefore, addresses the following research question: To what extent does the IMB model predict HIV-related sexual risk behaviors for YMSM?
Methods
Sample
Cross-sectional data were collected as part of a larger study on HIV risk and sexual identity development at a lesbian, bisexual, gay and transgender (LBGT) community center in a large Midwestern city from January to May, 2006. A convenience sample of 156 self-identified young men who have sex with men between the ages of 14-21 was drawn from youth who attended the center's activities and drop-in programs.
Procedures
Interviews were conducted approximately every other weekend, primarily during the evening drop-in program for youth, with a range of 11-27 completed interviews per weekend. On each night of data collection, youth in attendance at the center were informed about the study and offered an opportunity to participate. Voluntary informed consent was obtained from all participants over age 18. For participants under the age of 18, assent was obtained along with consent from the agency's Youth Director who served as a youth advocate (in lieu of parental consent) and evaluated on a case-by-case basis whether participation in the study was in the youth's best interest. This procedure, similar to those used in previous studies with sexual minority youth (Dube, 2000; Rotheram-Borus, Reid, Rosario, & Kasen, 1995; Savin-Williams, 2001), was enacted to protect respondents who were not “out” to parents about their sexual identity and for whom standard parental consent procedures could result in rejection of or harm to the youth (Rotheram-Borus et al., 1995). This study received approval from the Institutional Review Board of Washington University in St. Louis and received a federal Certificate of Confidentiality.
Participants completed a self-administered written questionnaire in a large, private room at the community center where they had been recruited. Because youth typically attended center activities with friends, participants were recruited in their friendship groups (i.e., friends who were also in attendance that night) to increase comfort and participation. Respondents completed the survey in self-chosen groups of 2 to 5 youths, but all youth were also offered the option of completing it privately if they preferred (although none requested this). To ensure privacy, participants were seated several seats apart from one another. The Principle Investigator (PI) read all survey instructions aloud to the group at the start of each interview. The PI was available to answer questions about the survey but waited outside the door of the room until each group was finished to further ensure privacy. Respondents completed the survey in 20 to 30 minutes and received $10 for participating.
Measures
The survey instrument was piloted with non-sample sexual minority male youth prior to data collection. Piloting procedures included interview run-throughs to establish the burden of interview, flow of interview, and suitability of instruments for this population.
HIV prevention information and motivation were assessed using subscales from Fisher and colleagues’ Teen Health Survey (Fisher, Fisher, Bryan, & Misovich, 2002). Self-efficacy was assessed with scales previously used in research with sexual minority youth (Rotheram-Borus et al., 1997). Sexual risk behaviors were assessed using two scales created for this study.
Information
Participants’ level of HIV/AIDS information was measured using the nine-item “AIDS Information Heuristics” subscale (α=.75†; range of 0-9).1
Motivation
The motivation component of the IMB model is made up of three constructs: HIV prevention attitudes, norms, and intentions. Youth's motivation to prevent HIV infection was measured using three scales: (1) the HIV prevention attitudes measure (α=.63†; α=.60*) included three items (e.g., “If I have sex during the next two months, using condoms every time would be [Very bad to Very good]”), (2) HIV prevention norms were assessed with six items on perceived social support from peers (α=.60†; α=.79*) and sexual partners ( α=.69†; α=.79*) (e.g., “Friends that I respect think I should use condoms every time, if I have sex during the next two months.”), and (3) HIV prevention intentions were assessed with three items (α=.66†; α=.58) (e.g., “If I have sex during the next two months, I'm planning to use condoms every time.”). The possible range for all motivation subscale scores was 3-15.
Self-efficacy for behavioral skills
Respondents’ perceived self-efficacy to perform key HIV preventive skills was assessed using two subscales: (1) The condom use self-efficacy scale (α=.72†; α=.58*; range 3-15) included three items (e.g., “I can use a condom with a sex partner, even if the room is dark.”), and (2) the safer-sex negotiation self-efficacy scale (α=.83†; α=.69*; range 5-25) included five items (e.g., “I can ask a new sex partner to use condoms.”), both with five response options ranging from “Certain I can do it” to “Can't do it at all.”
These subscales were selected based on previous use in research with ethnically diverse sexual minority youth (Rotheram-Borus et al., 1997) consistent with Fisher and Fisher's (1992) recommendation on the use of population-specific measures. The two subscales on condom use and safer sex negotiation were also consistent with the a priori conceptualization of sexual risk in this study as “primary” or “secondary” as described below.
Sexual risk behaviors
A review of the literature revealed no established standard of sexual risk behavior measures associated with the IMB model. Previous studies have utilized myriad configurations of sexual risk, from a single outcome variable (e.g., frequency of condom use with last sexual partner) to a scale of relative risk created by researchers for a specific study. In the current study, two subscales were created based on an a priori conceptualization of sexual risk behaviors as either primary or secondary risk in relation to HIV infection (e.g., Basen-Engquist et al. 2001; Coyle et al., 1999; Fisher et al., 1994).
Primary sexual risk behaviors were conceptualized as those behaviors that can directly result in HIV transmission (e.g., unprotected intercourse), whereas sexual risk behaviors that can lead indirectly to HIV infection by exacerbating one's risk (e.g., sex while under the influence) were considered secondary sexual risk behaviors. The items used to create the primary sexual risk scale (i.e., abstinence and condom use variables) were identical to those used in Fisher and colleagues’ (2002) intervention study with ethnically diverse high school students. However, none of the studies using the IMB model are known to have used a scale of secondary sexual risk.
The primary sexual risk behavior scale (α=.63) included five items. Two questions assessed whether the respondent had ever had vaginal and/or anal intercourse (“Yes/No”), and three items assessed frequency of condom use for vaginal and anal intercourse (response set of “Always” to “Never”). The secondary sexual risk behavior scale (α=.60) included two items assessing the frequency of safer sex discussion with vaginal and anal sex partners in the last two months and two items assessing sex while under the influence (e.g., “During the past two months, how often have you or your partner had sex [either vaginal or anal] while under the influence of alcohol or drugs?”). Each item had a response option ranging from “Always” to “Never.”
Data Analysis
Intercooled Stata (Version 9) was used for data cleaning, coding, and preliminary analysis. AMOS (Version 6.0) was used for model testing.
Multivariate single imputation (Saunders et al., 2006) was conducted to address the small percentage (less than 1%) of missing data and allow for retention of full statistical power for analysis. This method of imputation by chained equations ([MICE]; Van Buuren, Boshuizen, & Knook, 1999) conducts multiple regression procedures with all remaining variables in the dataset and replaces missing values based on distributions of the data including random variation to reflect uncertainty (von Hippel, 2005).
Principal Factors Analysis (PFA) with promax rotation was used to establish underlying factor structure for all model components comprised of multiple variables. This was done to determine if each subscale of the motivation component (i.e., attitudes, norms, and intentions) and the skills self-efficacy component (i.e., condom use self-efficacy and negotiation self-efficacy) of the model formed one dimension. Consistent with the theoretical model, factor analysis of the three motivation variables indicated one underlying factor, as did factor analysis of the two skills self-efficacy variables.
Bivariate analyses were conducted using Mann-Whitney U tests and Spearman's rho due to variable skewness. Path analysis was used to determine the fit of the IMB model for YMSM and was conducted using maximum likelihood method (ML).
Path analysis involved three steps: (1) an initial model fitting, (2) model modification (i.e., adding parameters), and (3) model trimming or eliminating parameters, as described by Schumaker and Lomax (2004). First, the IMB model was specified in Amos as indicated by Fisher and Fisher (1992). A specification search was conducted to seek a better fitting model (Schumaker & Lomax), and modification indices were used to add parameters to the initial model. Modification indices represent the expected amount of change in chi-square if a given parameter were to be added to the model, and indicate that an important path was not included in the initially fitted model (Pedhazer, 1994). Finally, the model was trimmed by eliminating parameters based on statistical significance (Schumaker & Lomax). Path analysis results were examined using chi-square, root mean square error of approximation (RMSEA), goodness-of-fit index (GFI), parsimonious goodness-of-fit index (PGFI), and the Tucker & Lewis index (TLI).
Results
Sample demographics
As displayed in Table 1, the study sample (n=156) consisted of male youth ages 14 to 21 years old with a mean age of 18.64 (SD = 2.10). The racial/ethnic composition of the sample was 67% African American, 19% Caucasian, 8% biracial, 4% Hispanic, and 2% American Indian. The majority of participants self-identified as gay (72%), with a minority identifying as bisexual (19%) or other (9%). Most of the sample reported a male gender identity (92%) while a smaller number identified as transgender (8%).
Table 1.
Demographic Characteristics of Sample
| Characteristics | n | % |
|---|---|---|
| Race/Ethnicity | ||
| African American | 105 | 67.31 |
| Caucasian | 29 | 18.59 |
| Biracial | 13 | 8.33 |
| Hispanic | 6 | 3.85 |
| American Indian | 3 | 1.92 |
| Sexual Orientation | ||
| Gay | 112 | 71.79 |
| Bisexual | 30 | 19.23 |
| Other | 14 | 8.97 |
| Gender Identity | ||
| Male | 144 | 92.31 |
| Transgender | 12 | 7.69 |
| X̄ | Med | |
| Age (years) | 18.64 | 18 |
Descriptive results indicated that youths were fairly knowledgeable about HIV/AIDS transmission and prevention; the median score for the information scale was seven out of nine items answered correctly.
Youth in this sample reported very positive attitudes toward condoms and strong intentions to engage in condom-related preventive behaviors in the next two months. Respondents also indicated very strong support from friends and slightly less from their sexual partners for the three condom use behaviors assessed. Youths reported moderate to high perceived self-efficacy for both subscales, indicating that they were fairly confident in their ability to enact HIV prevention skills.
The two sexual risk scales were computed by summing z-scored sexual risk variables. For primary sexual risk items, youth reported high levels of sexual activity. Nearly all youths in the sample (92.31%) reported ever having anal sex with another male, and nearly half (44.23%) had ever had vaginal sex with a female. Only six percent of youths had never had anal or vaginal sex in their lifetimes. A majority of respondents (69.23%) indicated that they had had anal sex during the previous two months, while 15% reported having vaginal sex in the last two months. Of note, only half of the respondents reported always using a condom for vaginal sex (54.2%) and anal sex (50.0%) during the last two months. Fewer youth (40.38%) indicated that they had always used a condom with their last sexual partner.
A smaller, but sizable percentage of youth reported secondary sexual risk behaviors. One quarter of the sample (25%) reported having sex under the influence of drugs or alcohol during the previous two months as sometimes, usually, or always, while a smaller number of youths (14.10%) indicated that they had sometimes, usually, or always used alcohol or drugs purposefully to improve their sexual experience during the last two months. One fifth (20%) of the youth in this sample indicated having safer sex discussions with their sexual partner only sometimes, rarely, or never before having vaginal sex. However, a majority of youths (58.34%) reported that safer sex discussions occurred only sometimes, rarely, or never for their anal sex encounters during the previous two months. The medians, standard deviations and correlations for each model variable are displayed in Table 2.
Table 2.
Descriptive Statistics and Spearman Correlations among Model Variables
| 1. | 2. | 3. | 4. | 5. | |
|---|---|---|---|---|---|
| 1. Information | 1.00 | ||||
| 2. Motivation i | 0.32*** | 1.00 | |||
| 3. Skills Self-Efficacy i | 0.38*** | 0.48*** | 1.00 | ||
| 4. Primary Sexual Risk Behaviors ii | - 0.33*** | - 0.17* | - 0.04 | 1.00 | |
| 5. Secondary Sexual Risk Behaviors ii | - 0.29*** | - 0.17* | - 0.06 | 0.71*** | 1.00 |
| Median | 7 | 0.28 | 0.35 | -0.21 | -0.17 |
| Inter-quartile Range | 6, 8 | - 0.53, 0.81 | -0.42, 0.76 | -1.87, 2.16 | -1.88, 1.83 |
p < .05
**p < .01
p < .001
PC factor analysis was used to compute variables 2 and 3, thus they have approximate means and standard deviations of 0 and 1, respectively.
Sexual risk variables were z-scored before being computed as a summative scale, therefore they have means approximately equal to zero
Path analysis
Path analysis was used to determine whether the IMB model predicted primary and secondary sexual risk behaviors for this sample of YMSM. Because bivariate analysis indicated that youth of color reported significantly more primary sexual risk behaviors (z = - 4.32, p < .01) and secondary sexual risk behaviors (z = - 4.30, p < .01) than Caucasian youth, race/ethnicity was controlled for in path analysis.
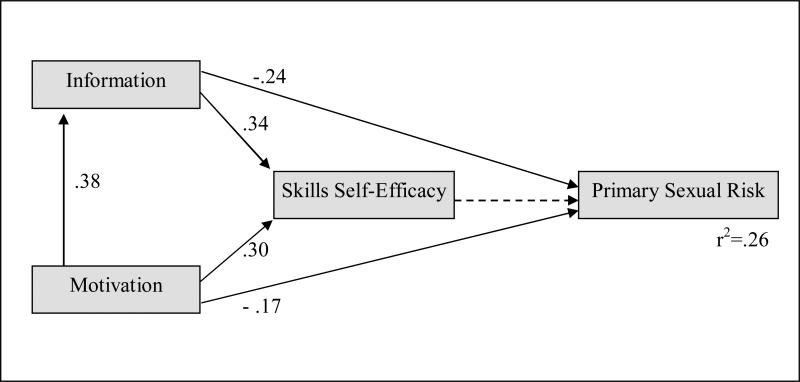
Results for primary sexual risk behaviors (see Figure 1) indicated support for model fit with a non-significant model chi-square (χ2 = 4.50, df = 3, p = .21) and a relative chi-square (i.e., χ2/df) value of 1.50 which was within the acceptable range. The TLI value of 0.96 also indicated good model fit. The GFI indicated excellent model fit at 0.99, however, the PGFI, which takes into account model complexity, was very low (0.20). Similarly, the RMSEA was just outside the acceptable range of 0.05 or less (RMSEA = 0.06), and the wide confidence interval for RMSEA (0.00 – 0.16) also suggested that the model was not well specified (i.e., that some model parameters could be found to be non-zero if a larger sample size were available).
Figure 1.
Path analysis of the IMB model to predict primary sexual risk behaviors among sexual minority youth. p < .05 for all solid paths. Dotted line indicates non-significant path from original IMB model. Parameters are standardized estimates.
Overall, model fit results were favorable and suggested that the IMB model was a fairly good predictor of primary sexual risk for YMSM. As stipulated in the original IMB model, more risky primary sexual behaviors were predicted by less HIV prevention information and motivation; lower levels of information and motivation also predicted lower self-efficacy for preventive skills. Self-efficacy was not, however, a significant predictor of primary sexual risk. The final model accounted for a modest amount of the variance (26%) in primary sexual risk behaviors.
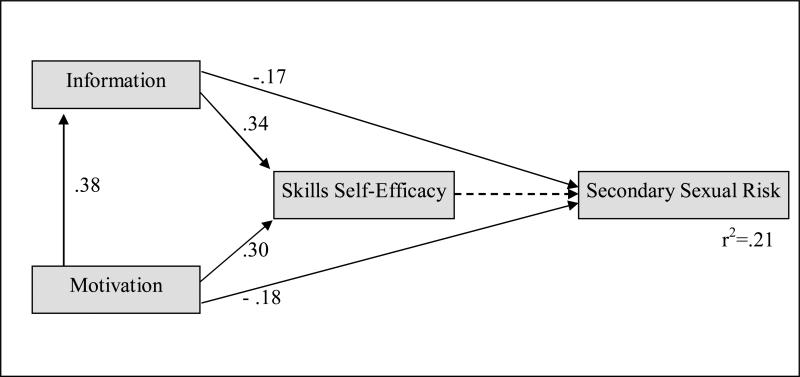
Path analysis results for secondary sexual risk behaviors (see Figure 2) were similar with a non-significant model chi-square (χ2 = 3.25, df = 3, p = .36) and a relative chi-square of 1.08, both indicating support for model fit. The RMSEA was well within the acceptable range of 0.05 or less (RMSEA = 0.03), although the slightly wide confidence interval for RMSEA (0.00 – 0.14) was beyond the suggested range to suggest strong support for fit between the model and the data. As for primary sexual risk behaviors, the GFI and TLI indicated excellent fit for the IMB model (0.99 and 0.99), while the PGFI again remained too low (0.20) to indicate adequate model fit when accounting for model complexity.
Figure 2.
Path analysis of the IMB model to predict secondary sexual risk behaviors among sexual minority youth. p < .05 for all solid paths. Dotted line indicates non-significant path from original IMB model. Parameters are standardized estimates.
These results indicate that the IMB model fit the data reasonably well for this sample of YMSM. Consistent with the hypothesized model, having less HIV prevention information and less HIV prevention motivation predicted lower self-efficacy and greater secondary sexual risk behaviors. However, self-efficacy was not a significant predictor of secondary sexual risk for these youth. The fitted model accounted for a modest amount of variance (21%) in secondary sexual risk behaviors.
Discussion
This study investigated how well constructs of the IMB model (i.e., HIV prevention information, motivation, and skills self-efficacy) predicted sexual risk behaviors among YMSM, a population at high risk for HIV infection. A majority of the relationships among constructs of the IMB model were supported by the data: YMSM in this sample who were better informed about and more motivated to prevent HIV infection had greater perceived skills to prevent HIV infection and lower primary and secondary sexual risk. However, skills self-efficacy was not a significant predictor of either primary or secondary sexual risk for these youth.
Current study findings were consistent with two previous studies of adult MSM which reported that the behavioral skills component of the model was not significantly associated with sexual risk (Benotsch et al., 2007; Fisher et al., 1994). Contrary to previous studies with both adult MSM (Fisher et al., 1994; Kalichman et al., 2008) and heterosexual ethnic minority high school youth (Fisher, Williams, Fisher, & Malloy, 1999), the current study found that HIV prevention information was significantly associated with both primary and secondary sexual risk for YMSM.
One possible explanation for the self-efficacy finding is that the YMSM in this study were more like adult MSM than their heterosexual youth counterparts in that believing oneself to be capable of enacting HIV-preventive skills (e.g., condom use) may not significantly influence actual risky sexual behaviors. Measurement of the skills self-efficacy construct may have also contributed to this finding. The current study utilized a self-efficacy scale comprised of two subscales (i.e., safer sex negotiation and condom use), each with moderate to high internal consistency reliability and previously used in research with ethnically diverse sexual minority youth (Rotheram-Borus et al., 1997). The choice to use this scale was consistent with Fisher and Fisher's (1992) recommendation that, when possible, each IMB component should include population-specific content and measures. However, univariate results suggest a ceiling effect for the two self-efficacy variables, as respondents reported being very confident in their ability to effectively engage in the two HIV preventive behaviors (i.e., negotiating safer sex and using condoms). For example, more than half of the sample (53.85%) reported being “certain I can do it” for all five condom negotiation self-efficacy items, and more than 60% reported the same high level of confidence on the three condom use self-efficacy items.
The challenges inherent in accurate assessment of the construct of self-efficacy are discussed at length by Forsyth and Carey (1998), who report that ceiling effects for self-efficacy measures in HIV prevention research are common due to social desirability bias, reliance on self-reports, and use of measures lacking in contextual information and sensitivity. Thus, a ceiling effect may have effectively obscured a relationship that existed between skills self-efficacy and sexual risk behaviors among these youth.
The significant relationship between HIV prevention information and sexual risk found in this study is notable given the previous research with adult MSM and heterosexual ethnic minority youth suggesting that information may have an indirect rather than direct effect on behavior. HIV prevention information scores were relatively high among this sample with a median score of 7 out of 9 correct. Yet the fact that each question was answered incorrectly by an average of one quarter of the respondents indicates clear knowledge deficits. These findings along with increasing HIV infection rates call into question whether adequate information about HIV transmission and prevention is reaching this population. YMSM of color in particular, who may feel disconnected from both a largely white peer group and the typical heteronormative approaches of many sex education programs in schools, may benefit from HIV prevention information specific to sex between men of color.
In early discussions of the IMB model, Fisher and colleagues (1994) noted that the model's specific causal elements and pathways “will prove to be more or less powerful determinants of preventive behavior for specific populations and for specific AIDS-preventive acts” (p. 242). More research is needed to establish the reliability of these constructs for predicting HIV-preventive behavior among YMSM.
When interpreting these study findings, the following limitations should be considered. First, this study used a convenience sample of youth recruited from an LBGT community center, which limits generalizability of findings to the larger population of young men who have sex with men—particularly to those who do not regularly attend organizations or groups that cater to sexual minorities. However, two previous studies investigated HIV risk among sexual minority youth from LBGT-centered organizations in New York City and Los Angeles who were similar demographically to the current sample (Rotheram-Borus, Hunter, & Rosario, 1994; Rotheram-Borus, Rosario, et al., 1994; Rotheram-Borus, Reid, & Rosario, 1994; Rosario, Mahler, Hunter, & Gwadz, 1999; Rosario, Meyer-Bahlburg et.al, 1999). Although these studies did not test the IMB model, reports of sexual risk behaviors were very similar to those reported in the current study, suggesting that study findings may be generalizable to sexual minority male youth who attend LBGT organizations in metropolitan areas of the U.S. As such, findings from this study can be used to inform future development of HIV preventive interventions for YMSM who attend LBGT community organizations similar to the study site. It is also important to acknowledge that, while interventions to reach YMSM who attend LBGT-focused organizations are certainly needed, there are other young sexual minority males who would likely not be reached by such programs. These harder to reach youth include young people questioning their sexual identity and those too shy to attend a public center, YMSM of color who feel disconnected from the largely white visible LBGT community, and rural youth. Further research is needed to assess the utility of the IMB model with these young people.
Second, study results were based on cross-sectional data, which has limited utility for investigating causality. Third, this study relied on self-report data from youth, which can threaten reliability and validity of data (Ostrow, Kessler, Stover, & Pequegnat, 1993; Ostrow & Kalichman, 2000). Because social desirability was not assessed, it is not known whether interviewer characteristics or other factors could have increased participants’ likelihood of responding in socially desirable ways. However, several strategies were used to facilitate accurate self-reports of respondents’ behaviors, including (a) limiting the recall period to the last two months prior to the interview, (b) emphasizing response confidentiality before and during the interview, and (c) informing subjects that their answers would be used to improve programs for sexual minority youth. Finally, the proportion of variance (21-26%) in sexual risk explained by the IMB model suggests that other important factors outside the individual-level scope of the model are impacting the HIV risk of YMSM.
Conclusion
This study is the first known investigation of the utility of the IMB model for predicting sexual risk behaviors among YMSM. These findings enhance our understanding of the sexual risk behaviors of YMSM and provide a theoretical foundation for the development of enhanced preventive interventions tailored for this population. It is critical to develop effective HIV-risk reduction interventions for YMSM as the incidence of HIV among this population is increasing (CDC, 2010) and YMSM are drastically underrepresented in the existing HIV prevention research. The present results suggest that intervention targets for YMSM should include provision of accurate information and promotion of motivation to use condoms and make other healthy decisions. However, more research is needed to investigate the influence of skills self-efficacy on sexual risk behaviors among YMSM and to explore innovative methods of assessing this construct with youth.
LBGT community centers like the data collection site for this study are well positioned to incorporate comprehensive HIV prevention programming or refine existing programs based on study findings. Other LBGT-focused organizations, particularly those which are youth-run, could also be helpful in extending the reach of HIV prevention programs to youth of color, homeless youth, and youth living in rural areas or without transportation.
Many social service professionals may think of HIV prevention as something outside their practice area, particularly if they do not work in LBGT-focused settings or with youth who are considered high risk for HIV. However, YMSM are likely to interact with these practitioners in a variety of social service settings including homeless shelters, schools, child welfare agencies, crisis hotlines, and suicide prevention programs. Each setting provides a unique opportunity for practitioners to integrate information about HIV transmission and prevention into their existing work with youth. This may require social service professionals themselves to become better educated in order to provide youth with accurate and updated information. Fortunately, there are many ways practitioners can do this such as attending training sessions conducted by local health departments and AIDS Service Organizations or exploring reputable websites such as The Body (www.thebody.com) or AVERT (www.avert.org) which provide comprehensive educational materials and online quizzes.
Finally, given the amount of variance in sexual risk explained by the IMB model, we can assume that factors beyond the individual-level focus of the model play an important role in sexual risk behaviors. Some of these factors may involve the nature of the relationship with one's sexual partner (e.g., power differentials), gender or sexual identity norms, and substance use in the context of sexual activity. For YMSM, the development of one's sexual identity and cultural norms and values of the LBGT community may certainly play a role.
Beyond individual-level factors and relationship dynamics, it is also important to consider contextual factors that are unique to the sexual health of YMSM, particularly for YMSM of color. With HIV infection rates of African American YMSM nearly double those of white and Hispanic YMSM (CDC, 2010), specialized prevention efforts are needed which take into account the unique experiences and multiple marginalized identities of YMSM of color. As noted by Peterson and Jones (2009), effective HIV prevention interventions with African American MSM must attend to the contextual and societal factors that uniquely affect their risk, including the overlapping impacts of racism and heterosexism, stigma, and poverty. Social service practitioners who value cultural competence and understand the impact of multiple oppression could make a valuable contribution to the growing dialogue on how to develop culturally relevant HIV prevention interventions for YMSM of color.
A sizable body of research exists on the prevention of sexually transmitted infections (STI) among African American adolescent females including large randomized trials (e.g., DiClemente et.al, 2004; DiClemente, et al., 2009; Jemmott, Jemmott, Braverman & Fong, 2005). These studies provide a strong empirical base for the identification of key intervention targets and strategies for tailoring interventions to address specific contextual factors related to risk among African American females. Young men who have sex with men would benefit from such large scale targeted research efforts. The IMB model may offer an effective theoretical foundation for HIV preventive interventions with YMSM. Research which incorporates these elements along with social and structural factors specific to YMSM—and with particular emphasis on the experiences of YMSM of color—is needed if we are to implement culturally-relevant interventions to prevent HIV infection among these youth.
Acknowledgments
This research was supported by the National Institutes of Health (F31MH077529) and the Comorbidity and Addictions Center, Washington University in St. Louis. The author gratefully acknowledges youth and staff at Affirmations Gay and Lesbian Community Center for their participation in this study.
Footnotes
A † symbol indicates scale alphas for the current study; a * symbol refers to original alphas.
References
- Agwu A, Ellen J. Rising rates of HIV infection among young US men who have sex with men. Concise Reviews of Pediatric Infectious Diseases. 2009;28:633–634. doi: 10.1097/INF.0b013e3181afcd22. [DOI] [PubMed] [Google Scholar]
- Anderson ES, Wagstaff DA, Heckman TG, Winett RA, Roffman RA, Solomon LJ, Sikkema KA. Information-Motivation-Behavioral Skills (IMB) model: Testing direct and mediated treatment effects on condom use among women in low-income housing. Annals of Behavioral Medicine. 2006;31(1):70–79. doi: 10.1207/s15324796abm3101_11. [DOI] [PubMed] [Google Scholar]
- Bandura A. Social foundations of thought and action: A social cognitive theory. Prentice Hall; Upper Saddle Rivr, NJ: 1986. [Google Scholar]
- Basen-Engquist K, Coyle KK, Parcel G, Kirby D, Banspach SW, Carvajal SC, Baumler E. Schoolwide effects of a multicomponent HIV, STD, and pregnancy prevention program for high school students. Health Education and Behavior. 2001;28(2):166–185. doi: 10.1177/109019810102800204. [DOI] [PubMed] [Google Scholar]
- Benotsch EG, Nettles CD, Wong F, Redmann J, Boschini J, Pinkerton SD, Mikytuck JJ. Sexual risk behavior in men attending Mardi Gras celebrations in New Orleans, Louisiana. Journal of Community Health. 2007;32(5):343–355. doi: 10.1007/s10900-007-9054-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention HIV testing among high school students — United States, 2007. Morbidity and Mortality Weekly Report. 2009;58(24):665–668. [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention HIV and AIDS among gay and bisexual men among African Americans. 2010 June;:1–3. Fact sheet prepared by the CDC. 2010. [Google Scholar]
- Cornman DH, Schmiege SJ, Bryan A, Benziger TJ, Fisher JD. An Information-Motivation-Behavioral Skills (IMB) model-based HIV prevention intervention for truck drivers in India. Social Science & Medicine. 2007;64:1572–1584. doi: 10.1016/j.socscimed.2006.11.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coyle K, Basen-Engquist K, Kirby D, Parcel G, Banspach S, Harrist R, Weil M. Short-term impact of Safer Choices: A multicomponent, school-based HIV, other STD, and pregnancy prevention program. Journal of School Health. 1999;69(5):181–188. doi: 10.1111/j.1746-1561.1999.tb06383.x. [DOI] [PubMed] [Google Scholar]
- Crosby RA, Salazar LF, Yarber WL, Sanders SA, Graham CA, Head S, Arno JN. A theory-based approach to understanding condom errors and problems reported by men attending an STI clinic. AIDS and Behavior. 2008;12:412–418. doi: 10.1007/s10461-007-9264-1. [DOI] [PubMed] [Google Scholar]
- DiClemente RJ, Wingood GM, Harrington KF, Lang DL, Davies SL, Hook EW, Robillard A. Efficacy of an HIV prevention intervention for African American adolescent girls: A randomized controlled trial. Journal of American Medical Association. 2004;292(2):171–179. doi: 10.1001/jama.292.2.171. [DOI] [PubMed] [Google Scholar]
- DiClemente RJ, Wingood GM, Rose ES, Sales JM, Lang DL, Caliendo AM, Crosby RA. Efficacy of sexually transmitted disease/Human Immunodeficiency Virus sexual risk–reduction intervention for African American adolescent females seeking sexual health services: A randomized controlled trial. Archives of Pediatric Adolescent Medicine. 2009;163(12):1112–1121. doi: 10.1001/archpediatrics.2009.205. [DOI] [PubMed] [Google Scholar]
- Dube EM. The role of sexual behavior in the identification process of gay and bisexual males—Statistical data included. Journal of Sex Research. 2000;37(2):123–132. [Google Scholar]
- Fishbein M, Ajzen I. Belief, attitude, intention, and behavior: An introduction to theory and research. Addison-Wesley; Reading, MA: 1975. [Google Scholar]
- Fisher JD, Fisher WA, Williams SS, Malloy TE. Empirical tests of an information-motivation-behavioral skills model of AIDS-preventive behavior with gay men and heterosexual university students. Health Psychology. 1994;13(3):238–250. doi: 10.1037//0278-6133.13.3.238. [DOI] [PubMed] [Google Scholar]
- Fisher JD, Fisher WA. Theoretical approaches to individual-level change in HIV risk behavior. In: Peterson J, DiClemente R, editors. Handbook of HIV Prevention. Kluwer Academic/Plenum Publishers; New York: 2000. pp. 3–55. [Google Scholar]
- Fisher JD, Willcutts DLK, Misovich SJ, Weinstein B. Dynamics of sexual risk behavior in HIV-infected men who have sex with men. AIDS and Behavior. 1998;2(2):101–113. [Google Scholar]
- Fisher WA, Fisher JD. Understanding and promoting AIDS preventive behavior: A conceptual model and educational tools. Canadian Journal of Human Sexuality. 1992;1(3):99–106. [Google Scholar]
- Fisher WA, Williams SS, Fisher JD, Malloy TE. Understanding AIDS risk behavior among sexually active urban adolescents: An empirical test of the Information-Motivation-Behavioral Skills Model. AIDS and Behavior. 1999;3(1):13–23. [Google Scholar]
- Fisher JD, Fisher WA, Bryan AD, Misovich SJ. Information-Motivation-Behavioral Skills model-based HIV risk behavior change intervention for inner-city high school youth. Health Psychology. 2002;21(2):177–186. [PubMed] [Google Scholar]
- Forsyth AD, Carey MP. Measuring self-efficacy in the context of HIV risk reduction: Research challenges and recommendations. Health Psychology. 1998;17(6):559–568. doi: 10.1037//0278-6133.17.6.559. [DOI] [PubMed] [Google Scholar]
- Hall HI, Song R, Rhodes P, Prejean J, Qian A, Lee LM, Janssen RS. Estimation of HIV incidence in the United States. Journal of the American Medical Association. 2008;300(5):520–529. doi: 10.1001/jama.300.5.520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jemmott JB, Jemmott LS, Braverman PK, Fong GT. HIV/STD risk reduction interventions for African American and Latino adolescent girls at an adolescent medicine clinic: A randomized controlled trial. Archives of Pediatric Adolescent Medicine. 2005;159(5):440–449. doi: 10.1001/archpedi.159.5.440. [DOI] [PubMed] [Google Scholar]
- Kalichman SC, Picciano JF, Roffman RA. Motivation to reduce HIV risk behaviors in the context of the Information, Motivation and Behavioral skills (IMB) model of HIV prevention. Health Psychology. 2008;13(5):680–689. doi: 10.1177/1359105307082456. [DOI] [PubMed] [Google Scholar]
- Kalichman SC, Simbayi LC, Cain D, Jooste S, Skinner D, Cherry C. Generalizing a model of health behaviour change and AIDS stigma for use with sexually transmitted infection clinic patients in Cape Town, South Africa. AIDS Care. 2006;18(3):178–182. doi: 10.1080/09540120500456292. [DOI] [PubMed] [Google Scholar]
- Kiene SM, Barta WD. A brief individualized computer-delivered sexual risk reduction intervention increases HIV/AIDS preventive behavior. Journal of Adolescent Health. 2006;39:404–410. doi: 10.1016/j.jadohealth.2005.12.029. [DOI] [PubMed] [Google Scholar]
- Mustanski B, Donenberg G, Emerson E. I can use a condom, I just don't: The importance of motivation to prevent HIV in adolescent seeking psychiatric care. AIDS and Behavior. 2006;10:753–762. doi: 10.1007/s10461-006-9098-2. [DOI] [PubMed] [Google Scholar]
- Ostrow DG, Kessler RC, Stover E, Pequegnat W. Design, measurement, and analysis issues in AIDS mental health research. In: Ostrow DG, Kessler RC, editors. Methodological issues in AIDS behavioral research. Plenum Press; New York: 1993. pp. 1–16. [Google Scholar]
- Ostrow DG, Kalichman S. Methodological issues in HIV behavioral interventions. Design, measurement, and analysis issues in AIDS mental health research. In: Peterson J, DiClemente R, editors. Handbook of HIV prevention. Kluwer Academic/Plenum Publishers; New York: 2000. pp. 67–80. 2000. [Google Scholar]
- Pedhazer EJ. Multiple regression in behavioral research: Explanation and prediction. 3rd ed. Harcourt Brace Publishers; Orlando, FL: 1994. 1997. [Google Scholar]
- Peterson JL, Jones KT. HIV prevention for black men who have sex with men in the United States. American Journal of Public Health. 2009;99(6):976–980. doi: 10.2105/AJPH.2008.143214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosario M, Mahler K, Hunter J, Gwadz M. Understanding the unprotected sexual behaviors of gay, lesbian, and bisexual youths: An empirical test of the Cognitive-Environmental Model. Health Psychology. 1999;18(3):272–280. doi: 10.1037//0278-6133.18.3.272. [DOI] [PubMed] [Google Scholar]
- Rosario M, Meyer-Bahlburg HFL, Hunter J, Gwadz M. Sexual risk behaviors of gay, lesbian, and bisexual youths in New York City: Prevalence and correlates. AIDS Education and Prevention. 1999;11(6):476–496. [PubMed] [Google Scholar]
- Rotheram-Borus MJ, Marelich WD, Srinivasan S. HIV risk among homosexual, bisexual, and heterosexual male and female youths. Archives of Sexual Behavior. 1999;28(2):159–177. doi: 10.1023/a:1018719922709. [DOI] [PubMed] [Google Scholar]
- Rotheram-Borus MJ, Reid H, Rosario M, Kasen S. Determinants of safer sex patterns among gay/bisexual male adolescents. Journal of Adolescence. 1995;18(1):3–15. [Google Scholar]
- Rotheram-Borus MJ, Hunter J, Rosario M. Suicidal behavior and gay-related stress among gay and bisexual male adolescents. Journal of Adolescent Research. 1994a;9(4):498–508. [Google Scholar]
- Rotheram-Borus MJ, Rosario M, Meyer-Bahlburg HFL, Koopman C, Dopkins SC, Davies M. Sexual and substance use acts of gay and bisexual male adolescents in New York City. Journal of Sex Research. 1994b;31(1):47–57. [Google Scholar]
- Rotheram-Borus MJ, Reid H, Rosario M. Factors mediating changes in sexual HIV risk behaviors among gay and bisexual male adolescents. American Journal of Public Health. 1994c;84(12):1938–1946. doi: 10.2105/ajph.84.12.1938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rotheram-Borus MJ, Murphy DA, Coleman CL, Kennedy M, Reid HM, Cline TR, Kipke M. Risk acts, health care, and medical adherence among HIV+ youths in care over time. AIDS and Behavior. 1997;1(1):43–52. [Google Scholar]
- Saunders JA, Morrow-Howell N, Spitznagel E, Doré P, Proctor EK, Pescarino R. Imputing missing data: A comparison of methods for social work researchers. Social Work Research. 2006;30(1):19–31. [Google Scholar]
- Savin-Williams RC. A critique of research on sexual minority youths. Journal of Adolesence. 2001;24(1):5–13. doi: 10.1006/jado.2000.0369. [DOI] [PubMed] [Google Scholar]
- Schumaker RE, Lomax RG. A beginner's guide to structural equation modeling. 2nd ed. Lawrence Erlbaum Associates; New Jersey: 2004. [Google Scholar]
- Van Buuren S, Boshuizen HC, Knook DL. Multiple imputation of missing blood pressure covariates in survival analysis. Statistics in Medicine. 1999;18(6):681–694. doi: 10.1002/(sici)1097-0258(19990330)18:6<681::aid-sim71>3.0.co;2-r. [DOI] [PubMed] [Google Scholar]
- von Hippel PT. Multiple imputation: A review and some new results; Paper presented at the Ohio State University Department of Sociology Brownbag; Columbus, OH. 2005, June. [Google Scholar]