Abstract
Objective
To determine if a complete anterior cruciate ligament (ACL) tear, a frequent incidental finding on MRIs of individuals with established knee osteoarthritis (OA), increases the risk for further knee OA progression.
Methods
We examined 265 participants (43% women) with symptomatic knee OA in a 30-month, prospective, natural history study of knee OA. The more symptomatic knee was imaged using MRI at baseline, 15- and 30-months. Cartilage was scored at the medial and lateral tibiofemoral joint and at the patellofemoral joint using the WORMS semiquantitative method. Complete ACL tear was determined on baseline MRI. At each visit, knee pain was assessed using a knee-specific visual analogue scale and physical function was assessed using the WOMAC physical function subscale.
Results
There were 49 participants (19%) with complete ACL tear at baseline. Adjusting for age, body mass index, gender and baseline cartilage scores, complete ACL tear increased the risk for cartilage loss at the medial tibiofemoral compartment (OR: 1.8, 95% CI: 1.1, 3.2). However, following adjustment for the presence of medial meniscal tears, no increased risk for cartilage loss was further seen (OR: 1.1, 95% CI: 0.6, 1.8). Knee pain and physical function were similar over follow-up between those with and without a complete ACL tear.
Conclusions
Individuals with knee osteoarthritis and incidental complete ACL tear have an increased risk for cartilage loss that appears to be mediated by concurrent meniscal pathology. The presence of a complete ACL tear did not influence the level of knee pain or physical function over short term follow-up.
Keywords: Anterior Cruciate Ligament, Knee Osteoarthritis, MRI, Knee Pain, Articular Cartilage, Menisci
INTRODUCTION
Among those with established knee osteoarthritis, an estimated 20–35% have an incidental anterior cruciate ligament (ACL) tear identified by MRI 1–3, many of whom have no recollection of prior trauma 1. The etiology and significance of an incidental ACL tear identified in those with knee osteoarthritis remains unclear. Histologically, the ACL from those with knee osteoarthritis has degenerative changes within it 4, and therefore may be prone to rupture without major trauma. The ACL is the main restraint of anterior tibial translation at the knee 5,6; traumatic ruptures of the ACL in young healthy knees have been associated with an increased risk for knee osteoarthritis 7–9 due, in part, to the subsequent anteroposterior and rotational instability at the knee 6. At present time, it is unknown whether an incidental ACL tear in those with established knee osteoarthritis accelerates the risk for further progression, structurally, symptomatically or both. If an incidental complete ACL tear was associated with accelerated progression of structural changes and/or symptoms in those with established knee osteoarthritis, further study on identifying appropriate, targeted, therapeutic interventions for such individuals would be warranted. In a large cohort of older men and women participating in a 30 month natural history study of symptomatic knee osteoarthritis that included longitudinal knee MRI evaluations, we examined whether the presence of a complete ACL tear at baseline increases the likelihood for cartilage loss and worsening pain and function at the knee.
METHODS
Study Participants
Study participants were enrolled in the Boston Osteoarthritis of the Knee Study (BOKS), a 30-month natural history study of symptomatic knee osteoarthritis whose recruitment has been described in detail elsewhere 10,11. Potential participants had to have answered yes to the following two questions: “Do you have pain, aching or stiffness in one or both knees on most days” and “Has a doctor ever told you that you have knee arthritis?” A subsequent interview was conducted to exclude other forms of arthritis. Eligible participants all had to have an osteophyte present on radiographs of their symptomatic knee, be able to walk, with or without the aid of a cane, and be willing to participate in the longitudinal study. There were 324 subjects (201 men and 123 women) who met eligibility criteria. All participants met American College of Rheumatology criteria for symptomatic knee osteoarthritis 12. The majority of men in the study received their care through the Veterans Administration (VA) Boston Healthcare System and had been recruited from their clinics, while the majority of women were recruited from the community 10,11.
Study Overview
Examinations were conducted at baseline, 15- and 30-months and included imaging studies of knees and questionnaire data. Subjects were also weighed, with shoes off, on a balance beam scale, and height was measured. The institutional review boards of Boston University Medical Center and the VA Boston Healthcare System approved the baseline and follow-up evaluations.
Knee MRI Protocols
At baseline, participants without contraindications underwent MR imaging of the more symptomatic knee, which was imaged again at 15- and 30-months. MRIs were acquired on a General Electric Signa 1.5-Tesla MRI system (GE Medical Systems, Milwaukee, Wisconsin) using a phased-array knee coil. An anchoring device for the ankle and knee were used to ensure uniformity of positioning between patients and for follow-up. The imaging protocol included sagittal spin-echo proton density- and T2-weighted images as well as coronal and axial fat-suppressed spin-echo proton-density- and T2-weighted images (repetition time, 2200 msec; time to echo, 20/80 msec; slice thickness, 3 mm; interslice gap, 1 mm; 1 excitation; field of view, 11–12 cm; matrix, 256×192 pixels).
Cartilage Morphology Scoring and Assessment of Cartilage Loss
Cartilage morphology at the tibiofemoral and patellofemoral joint was assessed using the Whole-Organ MRI Score (WORMS) semi-quantitative method for knee osteoarthritis 13. As previously described, there were a total of three trained readers who scored all MRIs unblinded to sequence, and the majority of subjects (86%) with longitudinal MRIs were read by both a musculoskeletal radiologist and a musculoskeletal researcher from the Osteoporosis and Arthritis Research Group of the University of California, San Francisco, reading together 14. Cartilage morphology was scored on all 5 regions of the tibiofemoral joint (central and posterior femur; anterior, central and posterior tibia) each for the medial and lateral compartment (see Figure 1). Cartilage morphology at the patellofemoral joint was scored at all 4 regions: the medial and lateral surfaces of the patella and anterior femur (see Figure 1). Cartilage morphology was scored by readers using a 0–6 scale: 0=normal thickness and signal; 1=normal thickness but increased signal on T2-weighted images; 2=solitary focal defect of less than 1 cm in greatest width; 3=areas of partial-thickness defects (< 75% of the region) with areas of preserved thickness; 4=diffuse partial-thickness loss of cartilage (≥75% of the region); 5=areas of full-thickness loss (<75% of the region) with areas of partial thickness loss; 6=diffuse full-thickness loss (≥75% of the region) 13. Intraclass correlation coefficient (ICC) for intra- and inter-rater agreement on cartilage readings ranged from 0.72–0.97 and 0.80–0.94, respectively.
Figure 1.
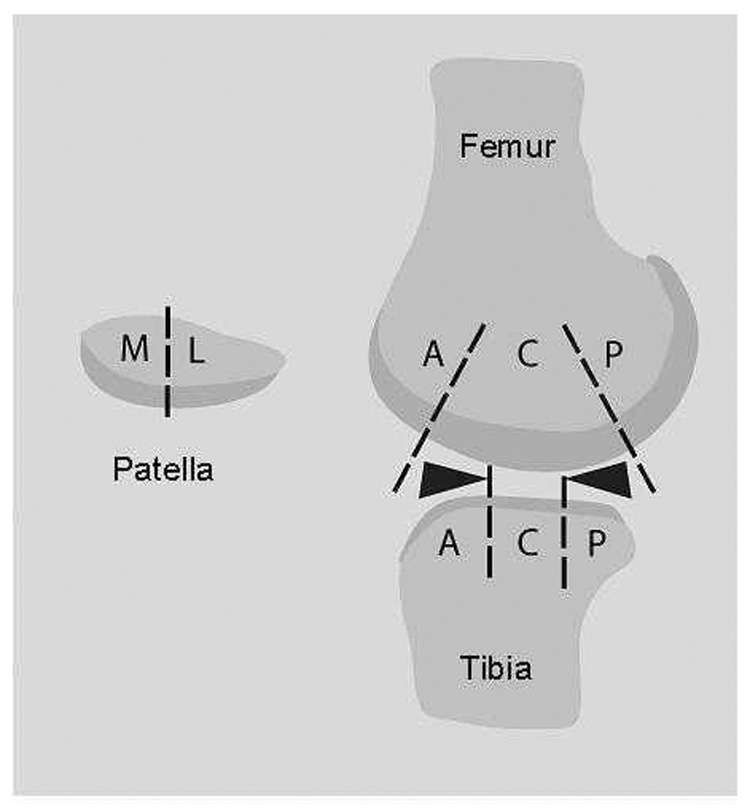
Cartoon of the knee (sagittal view) and patella illustrating the 5 cartilage plates of the tibiofemoral joint (central femur, posterior femur, anterior tibia, central tibia, posterior tibia) and 4 plates of the patellofemoral joint (medial and lateral patella and anterior femur). A=anterior; C=central; P=posterior; M=medial; L=lateral.
For the purposes of analyses, the original WORMS scores of 0 and 1 were collapsed to 0, the original scores of 2 and 3 were collapsed to 1, and the original scores of 4, 5 and 6 were considered 2, 3 and 4, respectively, in the new scale, as previously reported 14. This was done as grade 1 represents a change in signal in cartilage of otherwise normal morphology, while grades 2 and 3 represent similar types of morphologic abnormalities scores. Furthermore, grade 1 and 2 were infrequent among the MRIs read in our study population. Using this new scale, cartilage loss over follow-up at each region was defined as an increase in score, ranging from 0 (no loss) to 4 (maximal loss).
ACL Tear
The presence of an ACL tear at baseline was determined using sagittal and coronal views and scored on a 0–2 scale, with 0= normal, 1= partial tear and 2= complete tear. A complete tear was defined as complete disruption of ACL fibers with ligament discontinuity (see Figure 2), while a partial tear was defined as a residual straight and tight ACL fiber in at least one pulse sequence. All ACL tears were read by one board certified musculoskeletal radiologist (weighted kappa = 0.75), separate from the cartilage scoring. Because partial ACL tears may still protect against anteroposterior translation of the tibia, our analyses focused on the effects of a complete ACL tear at the knee.
Figure 2.

Sagittal proton density MR image showing complete ACL tear (arrows) with normal appearance of the posterior cruciate ligament (PCL) (arrowhead).
Osteophytes
Moderate to large posterior tibial osteophytes, either medially or laterally, could serve to stabilize the anterior tibial translation at the knee, and so were considered as potential confounders in our analyses. Osteophytes were read on sagittal and axial MRI views by the same readers scoring cartilage. Osteophytes were scored on a 0–7 scale: 0=none, 1=equivocal, 2=small, 3=small-moderate, 4=moderate, 5=moderate-large, 6=large, 7=very large 13. The ICC for intra- and inter-rater reliability for osteophyte scores ranged from 0.75–0.99 and 0.77–0.88, respectively.
Meniscal Tear
Meniscal tears were also considered as potential confounders in analyses. The anterior horn, body segment and posterior horn of each of the medial and lateral menisci were graded from 0 to 4 based on both the sagittal and coronal images: 0 = intact; 1 = minor radial tear or parrot-beak tear; 2 = nondisplaced tear or prior surgical repair; 3 = displaced tear or partial resection; 4 = complete maceration / destruction or complete resection 13. Meniscal tears were read by the same readers scoring the cartilage and the ICC for intra- and inter-rater reliability for readings of meniscal tear ranged from 0.92–0.97 for each. For the purposes of this analysis, we summed the scores for each meniscus separately, so meniscal tear scores for either the medial or lateral meniscus could range from 0–12.
Knee Pain and Function
At baseline and all follow-up visits, participants were asked to rate the severity of pain in each knee over the past week, which they scored by using a 100-mm visual analogue scale (VAS), generating a score from 0 (no pain) to 100 (most severe pain possible). At all visits, function was also determined using the WOMAC physical function subscale 15, assessed using a Likert scale (0–68, higher scores indicating worse physical function).
Statistical Analyses
Statistical analyses were performed using SAS software, (SAS Institute Inc, Cary, North Carolina). Descriptive statistics were performed using Student’s t-tests for continuous variables and Chi-square tests for categorical variables. For longitudinal analyses, we used 30 month follow-up data unless not available, in which case 15 month data were used.
Cartilage loss in each knee region took on whole number values from 0 (no loss) to 4 (maximum loss) and was analyzed as ordered categories using the proportional odds logistic regression model. A generalized estimating equation correction was applied to regression models to account for the association in the cartilage loss outcome between regions within a knee compartment or joint. We used this model to determine if a complete ACL tear increased the risk for cartilage loss at any of the 5 regions within the medial or lateral compartment of the tibiofemoral joint, adjusted for age, body mass index (BMI), gender and baseline cartilage score at each region. We performed similar adjusted analyses to examine the effect of a complete ACL tear on cartilage loss at any of the 4 regions in the patellofemoral joint. Since large posterior tibial osteophytes may serve to stabilize the anterior translation of the tibia at the knee joint in ACL deficient knees, we explored whether adjustment for large (score > 4) posterior tibial osteophytes change any observed association with cartilage loss at the tibiofemoral or patellofemoral joint. We further adjusted for meniscal tears to determine whether any observed associations between ACL tear and cartilage loss at the tibiofemoral joint are confounded by concomitant meniscal damage.
We examined whether there were differences between those with or without a complete ACL tear in mean VAS knee pain scores (using the knee specific VAS pain score for the knee that was imaged in analyses) and WOMAC physical function scores, at baseline as well as follow-up, adjusted for age, BMI, gender and cartilage scores. We also performed a linear regression analysis to examine the difference between change in scores over follow-up, defined as the change in score from baseline to longest available follow-up, between those who did or did not have a complete ACL tear, adjusted for baseline age, BMI, gender and baseline cartilage score. We again explored whether the presence of a large osteophyte or meniscal tear influenced results.
RESULTS
There were 317 participants who had no contraindications to baseline knee MRI, and 277 (87%) underwent follow-up knee MRI at either 15-months, 30-months, or both 14. There were no differences between those who were and were not followed, respectively, in baseline age (mean ± SD: 66 ± 9 vs. 66 ± 10 years), BMI (30.8 ± 5.7 vs. 29.1 ± 5.6 kg/m2), Kellgren and Lawrence (K&L) grade (54% vs. 55% with K&L grade >2), or presence of a complete ACL tear (18% vs. 14%), but those who were not followed tended more often to be men (59% vs. 83%, p< 0.01). We excluded 12 subjects who had MRIs unreadable for cartilage loss (n=10) or ACL tear (n=2). The baseline characteristics of the 265 participants who were included in our analyses are outlined in Table 1 and are similar to the 277 who were followed.
Table 1.
Baseline characteristics of 265 men and women with symptomatic knee osteoarthritis
| Baseline Characteristics (mean ± SD) or % | |
|---|---|
| Age, years | 67 ± 9 |
| Body Mass Index, kg/m2 | 31.5 ± 5.7 |
| Women, N(%) | 113 (43%) |
| % Knees with Kellgren &Lawrence Grade ≥ 2 | 76% |
| % Knees with Maximal Cartilage Morphology | |
| Scores ≥ 1* at any region: | |
| Medial Tibiofemoral Compartment | 86% |
| Lateral Tibiofemoral Compartment | 63% |
| Patellofemoral Joint | 91% |
| VAS Knee Specific Pain, 0–100mm | 43.4 ± 25.0 |
| WOMAC physical function, 0–68 | 23.8 ± 11.4 |
baseline maximal cartilage morphology score at one or more regions within a compartment or joint; equivalent to original WORMS cartilage morphology score (0–6 scale) of 2 or greater.
Among the 265 participants (152 men, 113 women) who had MRI follow-up, 49 (18.5%) had a complete ACL tear, while 21 (8%) had a partial tear at baseline. There were 223 (84%) who provided 30 month data (48 (21.5%) with complete ACL tear and 175 (78.5%) without complete ACL tear). The remaining 42 (16%) provided 15-month data. At baseline, those with a complete ACL tear were more likely to have greater cartilage pathology in the medial tibiofemoral compartment, a history of knee injury or surgery, large posterior tibial osteophytes and meniscal tears, and greater knee pain (Table 2).
Table 2.
Baseline characteristics of those with and without a complete ACL tear in 265 men and women with symptomatic knee osteoarthritis
| Complete ACL Tear | ||
|---|---|---|
| Baseline Characteristics (mean ±SD) or % |
Yes (N=49) |
No (N=216) |
| Age, years | 68 ± 10 s | 66 ± 9 |
| Body Mass Index, kg/m2 | 32.2 ± 5.6 | 31.3 ± 5.8 |
| Women, N (%) | 15 (31%) | 98 (45%) |
| % Knees with Kellgren & Lawrence Grade ≥ 2 | 100%* | 71% |
| % Knees with injury † | 51%* | 24% |
| % Knees with prior surgery † | 43%* | 23% |
| % with Meniscectomy | 12%* | 3% |
| % with Ligament repair | 16%* | 2% |
| % with Arthroscopy | 29% | 18% |
| % with Other | 4%* | 1% |
| % Knees with Cartilage Morphology Scores ≥ 1†† at: | ||
| Medial Tibiofemoral Compartment | 98%* | 83% |
| Lateral Tibiofemoral Compartment | 63% | 63% |
| Patellofemoral Joint | 88% | 92% |
| Posterior Tibial Osteophytes (% knees with score >4) | ||
| Medial | 35%* | 9% |
| Lateral | 19%* | 3% |
| Meniscal Pathology (% knees with score > 6) | ||
| Medial | 58%* | 17% |
| Lateral | 29%* | 8% |
| VAS Knee Specific Pain, 0–100mm | 51.0 ± 25.6* | 41.6 ± 24.6 |
| WOMAC physical function, 0–68 | 26.7 ± 9.7 | 23.2 ± 11.7 |
statistically different between the two groups (p <0.05)
based on self-report only
equivalent to original WORMS cartilage morphology score (0–6 scale) of 2 or greater, at any region
Cartilage Loss at the Tibiofemoral Joint
Over follow-up, 123 knees (46%) had loss of cartilage at one region or more in the medial compartment of the tibiofemoral joint. Compared to those without one, those with a complete ACL tear had an increased risk for cartilage loss at the medial compartment (OR=1.8, 95% CI: 1.1, 3.2), adjusting for age, BMI, gender and baseline cartilage scores (Table 3). Adjusting for the presence of a large posterior tibial osteophyte did not change the risk (OR=1.9, 95% CI: 1.1, 3.4). However, when we adjusted for medial meniscal tear score, a complete ACL tear no longer was an independent risk for cartilage loss. (Table 3)
Table 3.
Cartilage loss over follow-up among 265 men and women with symptomatic knee osteoarthritis, with and without a complete ACL tear.
| Proportion of Regions within Knee Compartment or Joint with Loss of Cartilage* | Odds Ratio† (95% Confidence Interval) | ||||
|---|---|---|---|---|---|
| Complete ACL Tear | Unadjusted | Adjusted for age, BMI and gender | Adjusted for age, BMI, gender and meniscus†† | ||
| Yes | No | ||||
| Tibiofemoral Joint | |||||
| Medial Compartment | 53% | 45% | 1.9 (1.1, 3.3) | 1.8 (1.1, 3.2) | 1.1 (0.6, 1.8) |
| Lateral Compartment | 29% | 21% | 1.4 (0.7, 2.7) | 1.6 (0.8, 3.0) | 1.0 (0.4, 2.2) |
| Patellofemoral Joint | 10% | 14% | 0.8 (0.5, 1.4) | 0.8 (0.5, 1.4) | -- |
cartilage loss within a region defined as an increase in score over follow-up of at least 1 or more
all odds ratios were adjusted for baseline cartilage scores of the compartment or joint of interest
medial meniscal tear scores were used in analyses for the medial tibiofemoral joint and lateral meniscal tear scores were used in analyses for the lateral tibiofemoral joint
There were 59 knees (22%) which had loss of cartilage at one region or more in the lateral tibiofemoral compartment. Those with a complete ACL tear also had a modest but nonsignificantly increased risk for lateral compartment cartilage loss (OR: 1.6, 95% CI: 0.8, 3.0). (Table 3) Adjusting for the presence of a large posterior tibial osteophyte appeared to attenuate the risk for cartilage loss in this compartment (OR=1.2, 95% CI: 0.6, 3.0). When we adjusted for lateral meniscal tears, there was no association between a complete ACL tear and cartilage loss in the lateral tibiofemoral compartment. (Table 3)
We also explored whether a complete ACL tear would have a greater effect on cartilage loss within certain regions of either the medial or lateral tibiofemoral compartment, but found none.
Cartilage Loss at the Patellofemoral Joint
Over follow-up, 35 knees (13%) showed loss of cartilage at one region or more in the patellofemoral joint. A complete ACL tear at baseline did not increase the risk for cartilage loss at the patellofemoral joint (adjusted OR=0.8, 95% CI: 0.5, 1.4). (Table 3) Adjustment for large posterior tibial osteophytes had no effect on results (adjusted OR=0.6, 95% CI: 0.4, 1.2). Again, we found no specific regions within the patellofemoral joint that were more susceptible to cartilage loss in the presence of a complete ACL tear.
Knee Pain and Physical Function
While those with a complete ACL tear tended to have greater knee pain and worse physical function at baseline and follow-up, following adjustment for potential confounders, only knee pain at baseline was significantly greater in those with a complete ACL tear, with no statistical differences seen between groups in either follow-up knee pain, or baseline and follow-up physical function. (Table 4) Further adjustment for large posterior tibial osteophytes or meniscal scores did not change these findings.
Table 4.
Knee pain and function at baseline and follow-up among 265 men and women with symptomatic knee osteoarthritis, with and without a complete ACL tear
| Complete ACL Tear | ||
|---|---|---|
| Yes (N=49) |
No (N=216) |
|
| Adjusted Least Squares Mean (95% CI)* | ||
| Knee Specific VAS Pain Score (0–100mm) | ||
| Baseline | 50.0 (42.8, 57.1)† | 41.6 (38.2, 44.9) |
| Follow-Up | 45.3 (38.1, 52.5) | 39.8 (36.4, 43.2) |
| WOMAC Physical Function Score (0–68) | ||
| Baseline | 25.8 (22.7, 29.0) | 23.2 (21.7, 24.7) |
| Follow-Up | 25.8 (22.3, 29.3) | 22.3 (21.8, 25.2) |
adjusted for age, body mass index, gender and cartilage score
statistically different between two groups (p<0.05)
There was no significant difference in change in pain or function over follow-up between those who did and did not have a complete ACL tear either before or after adjustment for potential confounders. For those with and without a complete ACL tear, the adjusted mean change in VAS pain score was −4.6, 95% CI: −12.2 to 2.9, vs. −1.6, 95% CI: −5.2 to −2.0, respectively; the adjusted mean change in WOMAC physical function score was 0.1, 95% CI: −2.7 to 2.9, vs. 0.6, 95% CI: −0.7 to 2.0, respectively; negative scores signify an improvement in the pain or function score at follow-up.
All results were similar for men and women, except for the baseline knee pain scores, where we found no significant difference between groups among women.
DISCUSSION
In this longitudinal study of 265 older men and women with knee osteoarthritis, followed for up to 30 months, we found the presence of a complete ACL tear at baseline increased the risk for greater cartilage loss at the medial tibiofemoral compartment of the knee. However, once the presence of concurrent medial meniscal tears were taken into account, there was no independent risk of complete ACL tear on cartilage loss. There was also a trend for an increase in cartilage loss at the lateral compartment, but this too appeared to be related to concurrent meniscal pathology in the lateral tibiofemoral compartment. We observed no association between a complete ACL tear and cartilage loss at the patellofemoral joint. Although those with a complete ACL tear tended to have greater knee pain at baseline, over follow-up we found no overall differences in pain severity or degree of function between those who did or did not have a complete ACL tear once potential confounders were taken into account.
A complete ACL tear in those with established knee osteoarthritis may result from different mechanisms than the acute ACL tear in younger persons, especially since many have no recollection of a significant knee injury which would have resulted in an ACL tear 1. It may result from repetitive minor trauma which eventually attenuates the ACL so that it tears 4. Degenerative changes within the knee joint leading to a narrow intertrochanteric notch has also been suggested as leading to ACL tear in those with knee osteoarthritis 16–18. Regardless of the mechanism for ACL tear, ACL deficient knees are more unstable, and the translational shear force on the cartilage has been speculated as a risk factor for accelerated cartilage degeneration 6. Indeed, transection of the ACL, without injury to the other structures of the knee, is an animal model for osteoarthritis 19,20. Quadriceps femoris muscle dysfunction, which is frequently seen in those with an ACL tear 21, may play a role in the development and progression of osteoarthritis in ACL deficient knees. On the other hand, several investigators have also demonstrated an association between ACL tears and presence of meniscal tears, especially medially 22–24. While any injury to the knee could result in concurrent meniscal damage and ACL tear, some have demonstrated that ACL tears themselves may cause secondary meniscal damage 22,24, which, in turn, could contribute to cartilage loss.
It has been unclear whether an incidental ACL tear identified in an individual with established knee osteoarthritis reflects disease severity and/or contributes further to progression of cartilage loss at the knee. We do not know when the ACL tear occurred in our participants prior to their baseline MRI. Furthermore, meniscal tears were more frequent among those with a complete ACL tear, and it remains unknown in our study population whether these may have occurred at the time of the ACL tear, or was the result of the ACL tear, as some have reported 22,24. Nevertheless, our findings suggest that concurrent meniscal pathology, which may have occurred at the time of possible knee injury causing the ACL tear, or which resulted from an ACL tear, or which was independent of the ACL tear, is responsible for the accelerated cartilage loss, at least seen over short term follow-up, in osteoarthritic knees with an incidental complete ACL tear. The etiology of ACL tear in the absence of significant trauma and its relation to meniscal tears in those with established knee osteoarthritis deserve further investigation.
Interestingly, at baseline, those with an incidental complete ACL tear did have greater knee pain, particularly men, however we did not find a relation between ACL tear and change in knee pain or function over the period of follow-up. Although those with a complete ACL tear had greater cartilage loss over follow-up, cartilage is aneural, and so unlikely to be a direct source of symptoms. Meniscal tears, which were more frequent among those with ACL tear and which appeared to be contributing to this greater risk for cartilage loss in ACL deficient knees, were not associated with knee pain or function in this study population 25. While we did not observe an association between complete ACL tear and progression of symptoms over short-term follow-up, we do acknowledge that adequate detection of changes in symptoms over time among those with knee osteoarthritis can be challenging due to the fluctuation in symptoms frequently noted with this condition.
Our study has limitations. As participants were recruited largely from the VA, we had more men than women in our study. Trauma among veterans may also be higher than in the general population. Nevertheless, the prevalence of incidental ACL tear in our study population was similar to what has been reported by other groups 2,3. While we had some information available related to self-report of prior surgery to the knees, we do not have confirmed reports of the types of surgery to adequately assess their potential impact on study results. Furthermore, we also note that information on analgesic use and treatment for knee osteoarthritis was assessed but was too limited to adequately determine its influence on our findings. We did not have a clinical assessment of knee laxity in our study participants. Too few in our cohort had a partial ACL tear to examine for an association with loss of cartilage, however since we would not have expected a knee with a partial ACL tear to have anteroposterior instability as seen with a complete ACL tear, we would not have anticipated finding an increased risk of cartilage loss in this group. Indeed, in exploratory analyses, no apparent increased risk was observed. Those with a complete ACL tear were more likely to have longer follow-up, however in additional analyses taking into account duration of follow-up, our overall findings remained unchanged. Since our follow-up was limited to 30 months, we were not able to determine whether those with a complete ACL tear would have had greater risk of subsequent cartilage loss, or symptom progression, regardless of meniscal pathology, had longer follow-up been available.
In summary, over relatively short-term follow-up, we found that individuals with symptomatic knee osteoarthritis and incidental complete ACL tear are more likely to have accelerated cartilage loss at the medial tibiofemoral compartment that is due to concomitant meniscal tears, while symptoms remain relatively unchanged. How such individuals should be best managed remains unclear and requires further investigation.
Acknowledgements
The authors would like to thank the study participants for generously giving their time. The authors would also like to thank all the field staff on this project for their hard work over the years of this study.
Supported by an Osteoarthritis Biomarkers Grant from the Arthritis Foundation; NIH grant AR47785; and a grant from the Bayer Corporation.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest Statement: Dr. Amin has received an honorarium from Merck & Co.
The study sponsors had no role in the study design; in the collection, analysis and interpretation of data; in the writing of the manuscript; and in the decision to submit the manuscript for publication.
REFERENCES
- 1.Hill CL, Seo GS, Gale D, Totterman S, Gale ME, Felson DT. Cruciate ligament integrity in osteoarthritis of the knee. Arthritis & Rheumatism. 2005;52(3):794–799. doi: 10.1002/art.20943. [DOI] [PubMed] [Google Scholar]
- 2.Link TM, Steinbach LS, Ghosh S, Ries M, Lu Y, Lane N, et al. Osteoarthritis: MR imaging findings in different stages of disease and correlation with clinical findings. Radiology. 2003;226(2):373–381. doi: 10.1148/radiol.2262012190. [DOI] [PubMed] [Google Scholar]
- 3.Chan WP, Lang P, Stevens MP, Sack K, Majumdar S, Stoller DW, et al. Osteoarthritis of the knee: comparison of radiography, CT, and MR imaging to assess extent and severity. AJR. American Journal of Roentgenology. 1991;157(4):799–806. doi: 10.2214/ajr.157.4.1892040. [DOI] [PubMed] [Google Scholar]
- 4.Cushner FD, La Rosa DF, Vigorita VJ, Scuderi GR, Scott WN, Insall JN. A quantitative histologic comparison: ACL degeneration in the osteoarthritic knee. Journal of Arthroplasty. 2003;18(6):687–692. doi: 10.1016/s0883-5403(03)00256-0. [DOI] [PubMed] [Google Scholar]
- 5.Chan WP, Peterfy C, Fritz RC, Genant HK. MR diagnosis of complete tears of the anterior cruciate ligament of the knee: importance of anterior subluxation of the tibia. AJR. American Journal of Roentgenology. 1994;162(2):355–360. doi: 10.2214/ajr.162.2.8310927. [DOI] [PubMed] [Google Scholar]
- 6.Almekinders LC, Pandarinath R, Rahusen FT. Knee stability following anterior cruciate ligament rupture and surgery. The contribution of irreducible tibial subluxation. Journal of Bone & Joint Surgery American. 2004;86(5):983–987. doi: 10.2106/00004623-200405000-00014. [DOI] [PubMed] [Google Scholar]
- 7.Roos H, Adalberth T, Dahlberg L, Lohmander LS. Osteoarthritis of the knee after injury to the anterior cruciate ligament or meniscus: the influence of time and age. Osteoarthritis & Cartilage. 1995;3(4):261–267. doi: 10.1016/s1063-4584(05)80017-2. [DOI] [PubMed] [Google Scholar]
- 8.Lohmander LS, Ostenberg A, Englund M, Roos H. High prevalence of knee osteoarthritis, pain, and functional limitations in female soccer players twelve years after anterior cruciate ligament injury. Arthritis & Rheumatism. 2004;50(10):3145–3152. doi: 10.1002/art.20589. [DOI] [PubMed] [Google Scholar]
- 9.von Porat A, Roos EM, Roos H. High prevalence of osteoarthritis 14 years after an anterior cruciate ligament tear in male soccer players: a study of radiographic and patient relevant outcomes. Annals of the Rheumatic Diseases. 2004;63(3):269–273. doi: 10.1136/ard.2003.008136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Felson DT, Chaisson CE, Hill CL, Totterman SM, Gale ME, Skinner KM, et al. The association of bone marrow lesions with pain in knee osteoarthritis. Annals of Internal Medicine. 2001;134(7):541–549. doi: 10.7326/0003-4819-134-7-200104030-00007. see comment. [DOI] [PubMed] [Google Scholar]
- 11.Felson DT, McLaughlin S, Goggins J, LaValley MP, Gale ME, Totterman S, et al. Bone marrow edema and its relation to progression of knee osteoarthritis. Annals of Internal Medicine. 2003;139(5 Pt 1):330–336. doi: 10.7326/0003-4819-139-5_part_1-200309020-00008. [DOI] [PubMed] [Google Scholar]
- 12.Altman R, Asch E, Bloch D, Bole G, Borenstein D, Brandt K, et al. Diagnostic and Therapeutic Criteria Committee of the American Rheumatism Association. Development of criteria for the classification and reporting of osteoarthritis. Classification of osteoarthritis of the knee. Arthritis & Rheumatism. 1986;29(8):1039–1049. doi: 10.1002/art.1780290816. [DOI] [PubMed] [Google Scholar]
- 13.Peterfy CG, Guermazi A, Zaim S, Tirman PF, Miaux Y, White D, et al. Whole-Organ Magnetic Resonance Imaging Score (WORMS) of the knee in osteoarthritis. Osteoarthritis & Cartilage. 2004;12(3):177–190. doi: 10.1016/j.joca.2003.11.003. [DOI] [PubMed] [Google Scholar]
- 14.Amin S, LaValley MP, Guermazi A, Grigoryan M, Hunter DJ, Clancy M, et al. The relationship between cartilage loss on magnetic resonance imaging and radiographic progression in men and women with knee osteoarthritis. Arthritis & Rheumatism. 2005;52(10):3152–3159. doi: 10.1002/art.21296. [DOI] [PubMed] [Google Scholar]
- 15.Bellamy N, Buchanan WW, Goldsmith CH, Campbell J, Stitt LW. Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. Journal of Rheumatology. 1988;15(12):1833–1840. [PubMed] [Google Scholar]
- 16.Wada M, Tatsuo H, Baba H, Asamoto K, Nojyo Y. Femoral intercondylar notch measurements in osteoarthritic knees. Rheumatology. 1999;38(6):554–558. doi: 10.1093/rheumatology/38.6.554. [DOI] [PubMed] [Google Scholar]
- 17.Hernigou P, Garabedian JM. Intercondylar notch width and the risk for anterior cruciate ligament rupture in the osteoarthritic knee: evaluation by plain radiography and CT scan. Knee. 2002;9(4):313–316. doi: 10.1016/s0968-0160(02)00053-4. [DOI] [PubMed] [Google Scholar]
- 18.Leon HO, Blanco CE, Guthrie TB, Martinez OJ. Intercondylar notch stenosis in degenerative arthritis of the knee. Arthroscopy. 2005;21(3):294–302. doi: 10.1016/j.arthro.2004.11.019. [DOI] [PubMed] [Google Scholar]
- 19.Brandt KD. Transection of the anterior cruciate ligament in the dog: a model of osteoarthritis. Seminars in Arthritis & Rheumatism. 1991;21(3) Suppl 2:22–32. doi: 10.1016/0049-0172(91)90037-z. [DOI] [PubMed] [Google Scholar]
- 20.Vilensky JA, O'Connor BL, Brandt KD, Dunn EA, Rogers PI, DeLong CA. Serial kinematic analysis of the unstable knee after transection of the anterior cruciate ligament: temporal and angular changes in a canine model of osteoarthritis. Journal of Orthopaedic Research. 1994;12(2):229–237. doi: 10.1002/jor.1100120212. [DOI] [PubMed] [Google Scholar]
- 21.Williams GN, Barrance PJ, Snyder-Mackler L, Buchanan TS. Altered quadriceps control in people with anterior cruciate ligament deficiency. Medicine & Science in Sports & Exercise. 2004;36(7):1089–1097. doi: 10.1249/01.mss.0000131959.20666.11. [DOI] [PubMed] [Google Scholar]
- 22.Smith GN, Mickler EA, Albrecht ME, Myers SL, Brandt KD. Severity of medial meniscus damage in the canine knee after anterior cruciate ligament transection. Osteoarthritis & Cartilage. 2002;10(4):321–326. doi: 10.1053/joca.2002.0520. [DOI] [PubMed] [Google Scholar]
- 23.Maffulli N, Binfield PM, King JB. Articular cartilage lesions in the symptomatic anterior cruciate ligament-deficient knee. Arthroscopy. 2003;19(7):685–690. doi: 10.1016/s0749-8063(03)00403-1. [DOI] [PubMed] [Google Scholar]
- 24.Tandogan RN, Taser O, Kayaalp A, Taskiran E, Pinar H, Alparslan B, et al. Analysis of meniscal and chondral lesions accompanying anterior cruciate ligament tears: relationship with age, time from injury, and level of sport. Knee Surgery, Sports Traumatology, Arthroscopy. 2004;12(4):262–270. doi: 10.1007/s00167-003-0398-z. [DOI] [PubMed] [Google Scholar]
- 25.Bhattacharyya T, Gale D, Dewire P, Totterman S, Gale ME, McLaughlin S, et al. The clinical importance of meniscal tears demonstrated by magnetic resonance imaging in osteoarthritis of the knee. Journal of Bone & Joint Surgery - American Volume. 2003;85(A-1):4–9. doi: 10.2106/00004623-200301000-00002. see comment. [DOI] [PubMed] [Google Scholar]


