Abstract
Virtual reality (VR), a system of human–computer interaction that allows researchers and clinicians to immerse people in virtual worlds, is gaining considerable traction as a research, education, and treatment tool. Virtual reality has been used successfully to treat anxiety disorders such as fear of flying and post-traumatic stress disorder, as an aid in stroke rehabilitation, and as a behavior modification aid in the treatment of attention deficit disorder. Virtual reality has also been employed in research on addictive disorders. Given the strong evidence that drug-dependent people are highly prone to use and relapse in the presence of environmental stimuli associated with drug use, VR is an ideal platform from which to study this relationship. Research using VR has shown that drug-dependent people react with strong craving to specific cues (e.g., cigarette packs, liquor bottles) as well as environments or settings (e.g., bar, party) associated with drug use. Virtual reality has also been used to enhance learning and generalization of relapse prevention skills in smokers by reinforcing these skills in lifelike environments. Obesity researchers and treatment professionals, building on the lessons learned from VR research in substance abuse, have the opportunity to adapt these methods for investigating their own research and treatment questions. Virtual reality is ideally suited to investigate the link between food cues and environmental settings with eating behaviors and self-report of hunger. In addition, VR can be used as a treatment tool for enhancing behavior modification goals to support healthy eating habits by reinforcing these goals in life–like situations.
Keywords: addictions, food cues, obesity, technology, virtual reality
Introduction
Two women, cigarettes and drinks in hand, welcome you to the party as you walk in the door. Music is playing in the background, and you can feel it vibrating through the floor as you walk across the room toward a couple at a table drinking and eating pizza. While they talk with you, you cannot help but notice the smell of pizza wafting up from the open pizza box on the table. Wandering past a bar area, you smell the scent of beer, and outside a sliding glass door, the smell of cigarette smoke is evident as a group of smoking partygoers greets you and offers you a cigarette. The scene appears to be a pretty typical social gathering until you remember that this is not a party at all; you are in virtual reality (VR).
Advances in computer and graphic display technology have provided scientists and clinicians the ability to create virtual worlds, such as the one described, and to immerse people in the experience of those worlds for a variety of research and treatment purposes. The technology of VR involves a human–computer interaction that goes beyond simple presentations and observations similar to video game play. In VR, users are provided enhanced active participation within a three-dimensional virtual world that reacts in real time without a predefined script, simulating a real-world experience.
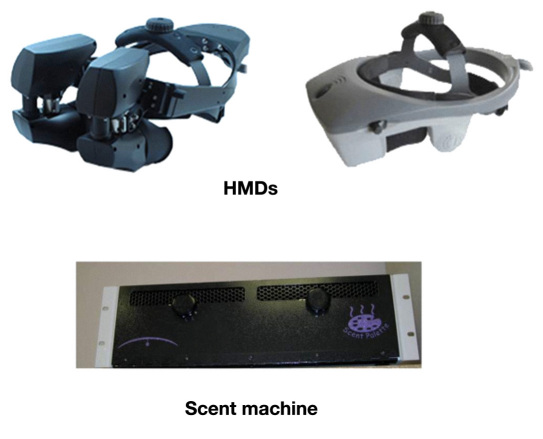
Several pieces of integrated equipment are required to provide access to the VR world. Users wear a head-mounted display (HMD) (see Figure 1) providing visuals through a wraparound visor screen in the first-person perspective (i.e., as if they were looking around in the real world). Surround sound is delivered through noise-cancelling headphones. Tracking devices attached to the HMD allow the user to navigate and become immersed in a complex environment in which they can explore and interact with three-dimensional virtual stimuli. Expanding the sensory experience for users, olfactory stimuli are presented using a scent machine (see Figure 1). Both ambient scents (e.g., smoke-filled bar, gas station) and specific scents (e.g., pizza, beer, marijuana smoke) can be presented throughout the VR environment. A typical clinical and research VR equipment setup is depicted in Figure 2. One of the key advantages of VR in research is the ability to present visual, auditory, tactile, olfactory, and contextual cues under full control of the researcher throughout the experiment.1–5 This allows researchers to create specific scenarios to test specific research questions.
Figure 1.
Virtual reality HMDs and scent machine (HMD photos courtesy of NVIS, Inc.).
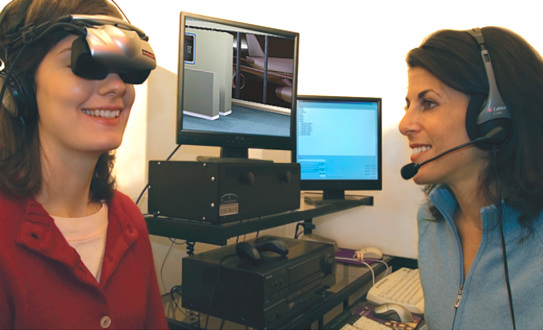
Figure 2.
Clinical VR equipment setup (photo credit Atticus Graybill, Virtually Better, Inc.).
Cue Reactivity and Exposure
An example of a basic VR application derives from a decades-old paradigm in addiction research. It is well established in laboratory studies that drug-dependent persons are reactive to stimuli associated with drug use, in the form of increased craving, physiological arousal, and drug-seeking behaviors. This phenomenon is known in the field as cue reactivity. A popular method for assessing substance use behaviors and abuse liability involves exposing users to drug stimuli (e.g., photos of cigarettes, bottles of liquor, “works” kit) and assessing craving level, attention, mood states, and basic physiology (e.g., heart rate, skin conductance). These responses (usually compared to responses to drug-neutral stimuli) are believed to index the psychological and motivational substrates of the addictive process, and these contribute to continuing substance use, as well as relapse in users attempting to remain abstinent. Craving, an intense desire to consume a substance, is the most robust and most studied of cue reactivity responses, as most drug-dependent persons report craving as the most troublesome barrier to abstinence.
Historically, cue reactivity laboratory paradigms have used simple cue presentations, such as photographs of cigarettes, videos of addicts in a shooting gallery, imagery scripts of substance-use situations, or in vivo methods (e.g., handling a liquor bottle), because the craving response is most often conceptualized as a cue-bound phenomenon, with these cues as the most obvious to trigger craving. However, drug-dependent persons, in their natural environment, are exposed to much more complex stimuli than these simple cues. Exposing substance users only to proximal stimuli (e.g., beer, cigarettes) in a laboratory or clinic environment is unlike typical substance use environments. In this approach, users experience increased craving and reactivity to the proximal cues; however, the total context (e.g., bar, party with social interactions) is missing and leaves unassessed a key component that also may be responsible for craving. Studies demonstrate that proximal cues presented alone (e.g., devoid of context) and substance use contexts devoid of proximal cues both lead to increased craving, supporting the notion that exposure methods should incorporate contextual cues, cues lacking in traditional approaches.6,7 To solve limitations of previous cue exposure approaches and increase ecological validity, VR applications are ideal, bringing more lifelike environments into the clinic and laboratory settings. While a VR scene never truly reproduces life experience, it has the necessary advantage of verisimilitude combined with researcher or therapist control over the situation.
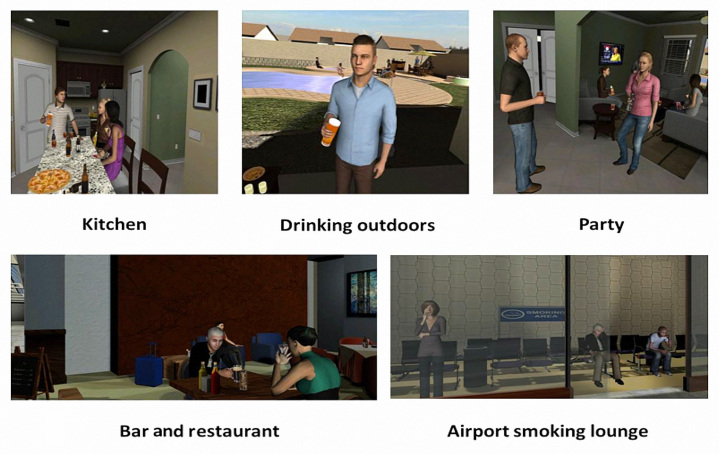
The first use of a novel VR immersive cue reactivity program for nicotine dependence was developed by Bordnick and colleagues4,5 in 2004. Virtual reality cue reactivity is built on the foundation of traditional cue methods but goes farther and allows exposure to realistic real-world stimuli in congruent use settings. Virtual reality programs provide exposure to drug stimuli in a VR environment, allowing users to experience complex environmental contexts and social interactions comparable to a real-world context. Advances in technology and equipment have led to rapid development and increased realism of VR environments for drug and alcohol exposures. Figure 3 depicts the latest advanced VR cue exposure environments for alcohol and nicotine that have been developed with VR software companies (World Viz, LLC, and Virtually Better, Inc.) funded by National Institutes of Health research grants.
Figure 3.
Screenshots of VR alcohol and nicotine exposure environments.
Since 2000, several pioneering researchers have incorporated VR-based technologies into addiction research and treatment. A growing body of research exploring VR cue reactivity and nicotine,4,5,8–13 alcohol,2 marijuana,3 cocaine,14 methamphetamine,15 and heroin16 has emerged since 2001, showing increased reactivity for drug cues compared to neutral cues.2–5,11,14
When new methods emerge, questions arise concerning validity. Because VR is a relatively new cue reactivity/exposure method and demonstrating effects is paramount, effect sizes are critical. Effect sizes are used as a common metric to determine the effect of a treatment or measurement method, and they are often defined using d, which is the difference between craving means (neutral versus drug) divided by their pooled standard deviation.17 In VR cue studies, craving effect sizes found in an alcohol cue study averaged 2.0,2 a marijuana study averaged 1.29,3 and nicotine studies averaged 1.6 in nicotine-dependent cigarette smokers.5 These large effect sizes are important for comparing differences between contexts, cue types, and delivery methods, which may be difficult to detect with the smaller effects often obtained in traditional cue methods (e.g., laboratory studies). Furthermore, craving self-reports are specific measurements, historically containing little error contri-bution, so the effect sizes can be interpreted with confidence. Overall, VR cue reactivity is now supported by 10 years of research on drugs of abuse.
Virtual Reality Applications for Addiction Treatment
Going beyond cue reactivity assessment, Bordnick and colleagues are collaborating to develop VR-based cognitive behavioral treatment programs for nicotine and alcohol dependence, supported by National Institutes of Health grants (studies in progress). Virtual reality cognitive behavioral therapy (CBT) for substance dependence combines traditional CBT/relapse prevention training with exposure and skill practice in VR-based environments (e.g., bar, party, smoking lounge in an airport).
In traditional cognitive behavioral treatment of addiction, coping skills are practiced in a clinical setting, such as a role play or therapeutic interview, using a gradual hierarchy of taxing situations, culminating with skills rehearsal in vivo.18 Clients use the skills in increasingly realistic situations. Ultimately, “the center stage of therapeutic change programs is not the therapist’s office but the real world in which the client lives.”19 Virtual reality offers an in-therapy experience that more closely resembles the real world than the office does. Virtual reality CBT fulfills the goals of systematic behavioral modification recommended by Kanfer and Phillips,20 such as acquiring and practicing skills in an environment that closely resembles the real world setting in which they will be performed. In the case of learning skills to resist overeating, environments such as parties and potlucks can be presented in VR, settings that will occur in the client’s naturally occurring life, and the skills will be directly transferable.
Overall, the high degree of reactivity found in cue reactivity studies forms the basis for VR’s power as an adjunct to traditional CBT therapy. State-dependent learning theory suggests that having substance-dependent individuals practice coping skills while in an elevated state of craving (and immersed in a high-risk environment) should have enhanced generalization to real-world settings compared to the effects of talk therapy or role playing in office settings. Indeed, these methods have been successfully employed for treatment of fear of flying;21 social phobia;22 claustrophobia;23 post-traumatic stress disorder in soldiers24 and in World Trade Center workers and rescuers;25 and attention deficit hyperactivity disorder;26,27 and for stroke rehabilitation.28
How Can Advances in Virtual Reality Cue Reactivity and Treatment Research Be Used in the Study of Obesity?
Traditional exposure methods in eating disorders have paralleled the methods used in addiction. In order to expand traditional methods, limited VR environments have been tested in eating disorders. Virtual reality food cues and related environments have been shown to evoke craving, anxiety, and mood states upon exposure.29–34 Gorini and associates29 demonstrated that VR and real food cues were equally effective at increasing craving and anxiety in participants with eating disorders. This line of research is important and provides support for the use of VR exposure methods to evoke behavioral and emotional responses in the laboratory that are similar to in vivo-evoked responses, which are important for engaging patients toward change. Building on lessons learned from VR research in substance abuse, obesity researchers and treatment professionals can further leverage scientific gains and develop additional VR applications for the assessment of eating behaviors (food cues) and interventions to teach coping skills. One can envision a clinician having access to a variety of VR high-risk eating contexts (e.g., restaurants, parties, stressful events, convenience stores, supermarkets) at the click of a mouse. Virtual reality has the potential to enhance assessment, treatment, and education in obesity as well as research and treatment of eating disorders.
Assessment
In substance abuse, exposure to drug and alcohol cues is used to assess relapse, craving, and behaviors related to relapse. Studies have demonstrated a common dopamine link related to drug and food addiction.35,36 Virtual-reality-based assessment tools such as cue reactivity/exposure can offer obesity and eating disorder researchers a method to assess behavioral, cognitive, and emotional responses to food and related environments in the laboratory or clinical office setting. Exposure to food cues has been linked to binge eating and early onset of food addiction.37,38 In eating disorders, VR assessments can provide both clinicians and patients the ability identify eating stimuli, social situations, and physical contexts that are difficult to manage in the real world and lead to increased anxiety, craving, and negative emotional responses. Eating disorder assessments can benefit from substance abuse research and realize the same direct benefits, affording the opportunity to assess real-world behaviors that have been otherwise irreproducible in controlled clinical settings.
Treatment
Cognitive and behavioral therapies are commonly used in the treatment of eating disorders and food addiction. In traditional eating disorders treatment, exposure exercises and skills practice are conducted in the clinician’s office using role plays, imagery, and simulated food to teach eating strategies and lifestyle modifications. Virtual reality can expand traditional cognitive and behavioral treatment approaches by providing exposure to realistic high-risk environments (e.g., restaurant, social situations involving food, stressful events) in the office where all aspects of the experience are controlled by the clinician, thus providing a bridge from the clinical setting to the real world as a first step in assessment and treatment. For example, a patient could be exposed to a VR restaurant that consists of an exact replica of a real-world restaurant, complete with other patrons and service staff who interact and offer chances to order food. Food choices can be made through a joystick or game pad and then served complete with scent cues. The flexibility of VR allows the exposure to be tailored to fit a patient’s specific skill level and deficits. Clinicians are able to teach behavioral change techniques, coping skills, stress management, and cognitive strategies during critical periods in the VR environments, thus allowing patients to learn and practice skills in real time, simulating the real world. Based on state-dependent learning theory, having patients practice and learn skills in high-risk environments should lead to increased generalization of these therapeutic gains into the real world, thus supporting the role of VR exposure in treatment.
Education
Virtual reality has been a valuable tool in education and training across a variety of disciplines. In health and nutrition education of patients and students, VR methods can be used to teach nutrition and healthy behaviors. Patients are often provided information in handouts about making lifestyle changes toward healthy eating. To improve these methods, VR can be used to teach patients about making healthy choices and lifestyle changes through active participation in VR simulations. For example, patients could visit a virtual grocery store or restaurant and learn about making healthy food choices and avoiding locations in the market that are likely to contain high-caloric foods. Virtual reality simulations would also expand education by providing environments to teach both clinicians and patients how to control or cope with both environmental and specific food cues.
In nursing, public health, and medical programs, VR and related technologies can be used to teach diagnostic skills, assessment strategies, and patient education using simulated patients (virtual patients). Virtual patients have been successfully used to assess clinician bias related to obesity.39 Using virtual patients for clinician assessment should be the building block for the development of simulations designed to train best practices for conveying health and prevention information. Virtual reality training and simulations may provide a critical missing link to improve clinician training and current patient communication practices.
Conclusion
Virtual reality applications have been successfully deployed in behavioral science research and treatment since 1995. In substance abuse, VR has led to changes in cue exposure and delivery of cognitive behavioral interventions. The use of VR in eating disorder areas has been limited. Given the strong behavioral and biological parallels between food and drug addiction, advances realized in substance abuse should be expected when incorporating VR in obesity research and treatment. Clinicians and researchers in eating disorders should embrace VR and other computer-based technologies to expand assessment, treatment, and education approaches. In addition, many of the current environments that have been developed for other areas (e.g., anxiety, addiction, driving) can be modified or used as-is to save development costs and time to implementation in eating research. Overall, scientific gains and knowledge using VR approaches in addictions, anxiety, medicine, and rehabilitation are poised to help explore new dimensions in eating research, with a strong possibility of significant progress in research and treatment goals.
Acknowledgments
We are thankful to World Viz, LLC (Andy Beall and Masaki Miyanohara), and Virtually Better, Inc. (Josh Spitalnick, Mirtha Ferrer, and Emlyn Murphy), for VR development and programming.
Abbreviations
- (CBT)
cognitive behavioral therapy
- (HMD)
head-mounted display
- (VR)
virtual reality
References
- 1.Bordnick PS. Virtual reality technologies for research and education in obesity and diabetes. Bethesda: National Heart, Lung, and Blood Institute; 2010. Motivation and self-monitoring: vr/addiction and virtual humans. [Google Scholar]
- 2.Bordnick PS, Traylor A, Copp HL, Graap KM, Carter B, Ferrer M, Walton AP. Assessing reactivity to virtual reality alcohol based cues. Addict Behav. 2008;33(6):743–756. doi: 10.1016/j.addbeh.2007.12.010. [DOI] [PubMed] [Google Scholar]
- 3.Bordnick PS, Copp HL, Traylor A, Graap KM, Carter BL, Walton A, Ferrer M. Reactivity to cannabis cues in virtual reality environments. J Psychoactive Drugs. 2009;41(2):105–112. doi: 10.1080/02791072.2009.10399903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bordnick PS, Graap KM, Copp HL, Brooks J, Ferrer M. Virtual reality cue reactivity assessment in cigarette smokers. Cyberpsychol Behav. 2005;8(5):487–492. doi: 10.1089/cpb.2005.8.487. [DOI] [PubMed] [Google Scholar]
- 5.Bordnick PS, Graap KM, Copp HL, Brooks J, Ferrer M, Logue B. Utilizing virtual reality to standardize nicotine craving research: a pilot study. Addict Behav. 2004;29(9):1889–1894. doi: 10.1016/j.addbeh.2004.06.008. [DOI] [PubMed] [Google Scholar]
- 6.Paris MM. Does context in virtual reality influence craving to smoke?. Presented at: Amercian Psychological Association 118th Annual Meeting; San Diego, CA: 2010. August 12–15. [Google Scholar]
- 7.Conklin CA, Perkins KA, Robin N, McClernon FJ, Salkeld RP. Bringing the real world into the laboratory: personal smoking and nonsmoking environments. Drug Alcohol Depend. 2010;111(1-2):58–63. doi: 10.1016/j.drugalcdep.2010.03.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Baumann SB. Paper presented at: Cyber Therapy. San Diego, CA: 2004. Smoking Cues in a Virtual World Provoke Craving in Cigarette Smokers as Demonstrated by Neurobehavioral and fMRI Data. [Google Scholar]
- 9.Baumann SB, Sayette MA. Smoking cues in a virtual world provoke craving in cigarette smokers. Psychol Addict Behav. 2006;20(4):484–489. doi: 10.1037/0893-164X.20.4.484. Dec. [DOI] [PubMed] [Google Scholar]
- 10.Bordnick PS, Traylor AC, Graap KM, Copp HL, Brooks J. Virtual reality cue reactivity assessment: a case study in a teen smoker. Appl Psychophysiol Biofeedback. 2005;30(3):187–193. doi: 10.1007/s10484-005-6376-0. [DOI] [PubMed] [Google Scholar]
- 11.Lee JH, Lim Y, Wiederhold BK, Graham SJ. A functional magnetic resonance imaging (FMRI) study of cue-induced smoking craving in virtual environments. Appl Psychophysiol Biofeedback. 2005;30(3):195–204. doi: 10.1007/s10484-005-6377-z. [DOI] [PubMed] [Google Scholar]
- 12.Traylor AC, Bordnick PS, Carter BL. Assessing craving in young adult smokers using virtual reality. Am J Addict. 2008;17(5):436–440. doi: 10.1080/10550490802268876. [DOI] [PubMed] [Google Scholar]
- 13.Traylor AC, Bordnick PS, Carter BL. Using virtual reality to assess young adult smokers’ attention to cues. Cyberpsychol Behav. 2009;12(4):373–378. doi: 10.1089/cpb.2009.0070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Saladin ME, Brady KT, Graap K, Rothbaum BO. A preliminary report on the use of virtual reality technology to elicit craving and cue reactivity in cocaine dependent individuals. Addict Behav. 2006;31(10):1881–1894. doi: 10.1016/j.addbeh.2006.01.004. [DOI] [PubMed] [Google Scholar]
- 15.Culbertson C, Nicolas S, Zaharovits I, London ED, De La Garza R, 2nd, Brody AL, Newton TF. Methamphetamine craving induced in an online virtual reality environment. Pharmacol Biochem Behav. 2010;96(4):454–460. doi: 10.1016/j.pbb.2010.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kuntze MF, Stoermer R, Mager R, Roessler A, Mueller-Spahn F, Bullinger AH. Immersive virtual environments in cue exposure. Cyberpsychol Behav. 2001;4(4):497–501. doi: 10.1089/109493101750527051. [DOI] [PubMed] [Google Scholar]
- 17.Cohen J. 2nd ed. Hillsdale: Lawrence Erlbaum Associates; 1988. Statistical power analysis for the behavioral sciences. [Google Scholar]
- 18.Meichenbaum D. Stress inoculation training for coping with stressors. Clin Psychol. 1996;49:4–7. [Google Scholar]
- 19.Kanfer FH, Schefft BK. Champaign: Research Press; 1988. Guiding the process of therapeutic change; pp. 234–235. [Google Scholar]
- 20.Kanfer FH, Phillips JS. Behavior therapy: a panacea for all ills or a passing fancy? Arch Gen Psych. 1966;15:114–128. [Google Scholar]
- 21.Rothbaum BO, Hodges L, Smith S, Lee JH, Price L. A controlled study of virtual reality exposure therapy for the fear of flying. J Consult Clin Psychol. 2000;68(6):1020–1026. doi: 10.1037//0022-006x.68.6.1020. [DOI] [PubMed] [Google Scholar]
- 22.Anderson PL, Zimand E, Hodges LF, Rothbaum BO. Cognitive behavioral therapy for public-speaking anxiety using virtual reality for exposure. Depress Anxiety. 2005;22(3):156–158. doi: 10.1002/da.20090. [DOI] [PubMed] [Google Scholar]
- 23.Botella C, Baños RM, Villa H, Perpiñá C, García-Palacios A. Virtual reality in the treatment of claustrophobic fear: a controlled, multiple-baseline design. Behav Ther. 2000;31(3):583–595. [Google Scholar]
- 24.Rizzo AA, Graap K, Perlman K, McLay RN, Rothbaum BO, Reger G, Parsons T, Difede J, Pair J. Virtual Iraq: initial results from a VR exposure therapy application for combat-related PTSD. Stud Health Technol Inform. 2008;132:420–425. [PubMed] [Google Scholar]
- 25.Difede J, Cukor J, Jayasinghe N, Patt I, Jedel S, Spielman L, Giosan C, Hoffman HG. Virtual reality exposure therapy for the treatment of posttraumatic stress disorder following September 11, 2001. J Clin Psychiatry. 2007;68(11):1639–1647. [PubMed] [Google Scholar]
- 26.Clancy TA, Rucklidge JJ, Owen D. Road-crossing safety in virtual reality: a comparison of adolescents with and without ADHD. J Clin Child Adolesc Psychol. 2006;35(2):203–215. doi: 10.1207/s15374424jccp3502_4. [DOI] [PubMed] [Google Scholar]
- 27.Rizzo AA, Buckwalter JG, Bowerly T, van der Zang C, Humphrey L, Neumann U, Chua C, Kyriakakis C, van Rooyen A, Sisemore D. The virtual classroom: A virtual reality environment for the assessment and rehabilitation of attention deficits. Cyberpsychol Behav. 2000;3(3):483–499. [Google Scholar]
- 28.Lam YS, Man DW, Tam SF, Weiss PL. Virtual reality training for stroke rehabilitation. NeuroRehabilitation. 2006;21(3):245–253. [PubMed] [Google Scholar]
- 29.Gorini A, Griez E, Petrova A, Riva G. Assessment of the emotional responses produced by exposure to real food, virtual food and photographs of food in patients affected by eating disorders. Ann Gen Psychiatry. 2010;9:30. doi: 10.1186/1744-859X-9-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Legenbauer T, Vögele C, Rüddel H. Anticipatory effects of food exposure in women diagnosed with bulimia nervosa. Appetite. 2004;42(1):33–40. doi: 10.1016/S0195-6663(03)00114-4. [DOI] [PubMed] [Google Scholar]
- 31.Ferrer-García M, Gutiérrez-Maldonado J, Caqueo-Urízar A, Moreno E. The validity of virtual environments for eliciting emotional responses in patients with eating disorders and in controls. Behav Modif. 2009;33(6):830–854. doi: 10.1177/0145445509348056. Nov. [DOI] [PubMed] [Google Scholar]
- 32.Gutiérrez-Maldonado J, Ferrer-García M, Caqueo-Urízar A, Letosa-Porta A. Assessment of emotional reactivity produced by exposure to virtual environments in patients with eating disorders. Cyberpsychol Behav. 2006;9(5):507–513. doi: 10.1089/cpb.2006.9.507. [DOI] [PubMed] [Google Scholar]
- 33.Carter FA, Bulik CM, McIntosh VV, Joyce PR. Cue reactivity as a predictor of outcome with bulimia nervosa. Int J Eat Disord. 2002;31(3):240–250. doi: 10.1002/eat.10041. [DOI] [PubMed] [Google Scholar]
- 34.Riva G, Bacchetta M, Baruffi M, Rinaldi S, Molinari E. Experiential cognitive therapy: a VR based approach for the assessment and treatment of eating disorders. Stud Health Technol Inform. 1998;58:120–135. [PubMed] [Google Scholar]
- 35.Volkow ND, Wise RA. How can drug addiction help us understand obesity? Nat Neurosci. 2005;8(5):555–560. doi: 10.1038/nn1452. [DOI] [PubMed] [Google Scholar]
- 36.Volkow ND, Wang GJ, Fowler JS, Telang F. Overlapping neuronal circuits in addiction and obesity: evidence of systems pathology. Philos Trans R Soc Lond B Biol Sci. 2008;363(1507):3191–3200. doi: 10.1098/rstb.2008.0107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Fedoroff IC, Polivy J, Herman CP. The effect of pre-exposure to food cues on the eating behavior of restrained and unrestrained eaters. Appetite. 1997;28(1):33–47. doi: 10.1006/appe.1996.0057. [DOI] [PubMed] [Google Scholar]
- 38.Sobik L, Hutchison K, Craighead L. Cue-elicited craving for food: a fresh approach to the study of binge eating. Appetite. 2005;44(3):253–261. doi: 10.1016/j.appet.2004.12.001. [DOI] [PubMed] [Google Scholar]
- 39.Persky S, Eccleston CP. Medical student bias and care recommendations for an obese versus non-obese virtual patient. Int J Obes (Lond) 2010 doi: 10.1038/ijo.2010.173. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]