Abstract
There is a great need for empirical evidence to inform clinical prevention and management of overweight and obesity. Application of virtual reality (VR) methods to this research agenda could present considerable advantages. Use of VR methods in basic and applied obesity prevention and treatment research is currently extremely limited. However, VR has been employed for social and behavioral research in many other domains where it has demonstrated validity and utility. Advantages of VR technologies as research tools include the ability to situate hypothetical research scenarios in realistic settings, tight experimental control inherent in virtual environments, the ability to manipulate and control any and all scenario elements, and enhanced behavioral measurement opportunities. The means by which each of these features could enhance obesity prevention and management research is discussed and illustrated in the context of an example research study. Challenges associated with the application of VR methods, such as technological limitations and cost, are also considered. By employing experimental VR methods to interrogate clinical encounters and other health-related situations, researchers may be able to elucidate causal relationships, strengthen theoretical models, and identify potential targets for intervention. In so doing, researchers stand to make important contributions to evidence-based practice innovation in weight management and obesity prevention.
Keywords: health care, methodology, obesity, virtual reality
Introduction
Use of virtual reality (VR) methods in basic and applied obesity prevention and management research is currently limited. However, VR has been employed as a methodology for conducting social and behavioral research in many other domains where it has demonstrated validity and utility. Previous reports describe several features of the technology that make it particularly suitable for these research applications.1–5 The present discussion focuses on how these capabilities can enhance research aimed at identifying pathways and intervention targets through which to improve obesity prevention and treatment.
Clinical obesity prevention and treatment has presented several challenging issues and questions. Key among these are gaps in our collective knowledge about the best way to promote and achieve prevention and management goals within the health care system. There are several barriers to effective clinical weight management. Obesity is under-recognized and undertreated in primary care and in health care systems, generally.6–9 Several barriers to addressing and treating overweight and obesity have been identified among clinicians. In addition to critical system-level factors (e.g., reimbursement, time), many clinicians perceive weight counseling to be a difficult and sometimes futile task. They report a lack of training and low levels of confidence in their ability to treat patients' weight. Clinicians also sometimes report the perception that patients are not sufficiently motivated or compliant. Finally, they recognize a lack of effective interventions to treat obesity.8,10
The weight management efforts that do occur are often ineffective over the long term.11,12 Indeed, there is a lack of proven, evidence-based approaches for sustained obesity treatment.13,14 From the perspective of the patient, behavior change can be incredibly difficult to initiate and sustain.15 In addition, clinicians' initiation of weight management discussions can be negatively perceived.8,16 Many overweight and obese patients report feeling blamed and stigmatized by their providers,17 which may lead to care avoidance.18 Therefore, despite the enormous visibility of obesity prevention and weight management campaigns, and despite formal recommendations that providers screen patients for obesity and provide weight management counseling,19 clinical weight management efforts frequently falter. There is a clear need for empirical evidence on what works to promote provider confidence in provision of weight-related care, to encourage life-long health-promoting behaviors among patients, and to foster therapeutic relationships between patients who are overweight and their providers.
Research aimed at understanding these processes could gain much from adoption of VR methods. Virtual reality enables creation of simulated clinical or health-related scenarios wherein researchers can directly manipulate theoretically important variables. This is critical because the clinical system is exceedingly complex, and many key theoretical variables are deeply intertwined. Each patient and each clinician comes to the health care interaction with an array of beliefs, attitudes, and behavioral tendencies (e.g., communication patterns, biases, beliefs about obesity etiology). Each encounter adds its own set of variables (e.g., shared history and shared understanding between clinician and patient), as do the medical and social systems in which the encounters are embedded. By breaking these complex encounters apart and employing experimental methods to interrogate them, researchers can elucidate causal relationships, strengthen theoretical models, and identify potential targets for intervention. Use of experimental methods is rarely possible in real clinical settings. There is therefore a need for naturalistic simulations in which to investigate patient and clinician behavior.20,21 This is an area where VR platforms stand to make a considerable contribution.
Immersive Virtual Reality
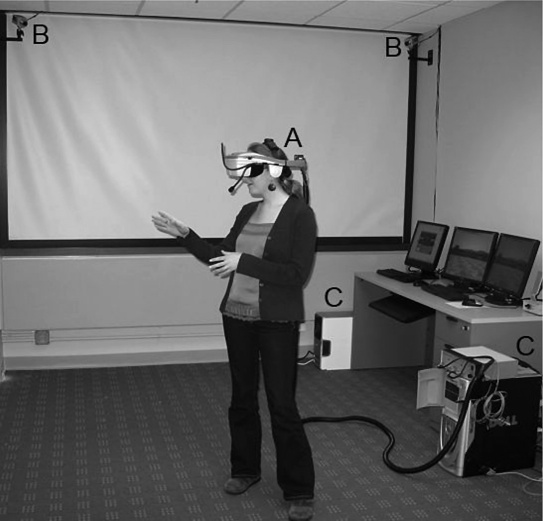
There are multiple formats that VR systems can take. For the purposes of this discussion, the primary focus is on immersive VR (i.e., systems that envelop the users' senses). One common configuration of immersive VR equipment employs a head-mounted display in which users view three-dimensional computer-generated images. Users are often free to move naturally while wearing the display. Their position and orientation can be tracked and used to control their point of view and events in the virtual environment (Figure 1).
Figure 1.
Illustration of immersive VR equipment: (A) head-mounted display, (B) tracking cameras, and (C) tracking and rendering computers.
Currently, use of VR platforms for basic and applied obesity prevention and treatment research is extremely limited. However, the validity of VR methods for behavioral research has been demonstrated in several other domains. For example, several studies have indicated that experiences in VR can translate to and affect behavior in real environments.22–27 Previous work has also shown that individuals behave similarly between experiments conducted in VR environments and those conducted in real settings.5 Indeed, interpersonal interactions with virtual humans have been shown to elicit very real social processes.28–31 This body of evidence suggests that research investigating processes related to obesity prevention and treatment in virtual scenarios is likely to apply to real-world clinical situations.
Blascovich, Loomis, and colleagues3,4 have identified several dimensions on which VR can be advantageous for experimental social, and behavioral research. These include the ability to situate hypothetical research scenarios in realistic settings, the tight experimental control inherent in creation of VR environments, the unprecedented ability to manipulate and control scenario elements, and the opportunity for direct behavioral measurement. Each of these advantages clearly applies to research aimed at informing obesity prevention and treatment practices.
Research Example
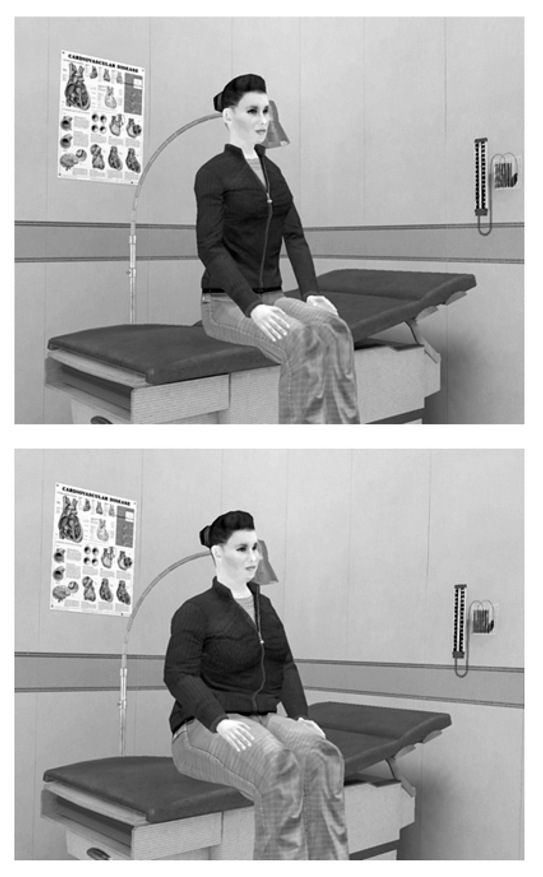
To illustrate how each of these methodological advantages applies to obesity research, it will be useful to consider them in the context of an example study. Persky and Eccleston32 designed a study to assess how patient weight elicits biased attitudes and behavior among medical students. This study employed an immersive VR clinic environment to simulate a basic encounter with a virtual patient who was visibly either obese or nonobese (Figure 2). Medical student participants were immersed in the virtual clinic by wearing a head-mounted display and were able to move naturally through the clinic environment (e.g., by walking). Participants' communication and nonverbal behaviors were tracked and recorded by the VR system.
Figure 2.
Screenshot from example research study of nonobese and obese versions of a virtual patient in a VR clinical environment.
Results of this study revealed that medical students exhibited more bias-related attitudes toward the obese than the nonobese version of the virtual patient. These included more negative stereotyping, perceptions that the patient would be less adherent, and increased attributions of responsibility for causing her symptoms (knee pain, shortness of breath). Participants also made less visual contact with the obese than the nonobese patient during the medical encounter. In contrast, the study found no clear evidence of bias in clinical recommendations and decisions about the patient's care. These findings contribute to our understanding of the nature and source of weight bias in clinical interactions and can inform attempts to reduce this bias.
Potential Advantages of Applying Immersive Virtual Reality Methods
In this example study, medical student participants were randomly assigned to interact with a virtual patient who was portrayed as being either obese or nonobese. By using VR, it was possible for participants to interact with patients who differed solely on the characteristic under study (i.e., weight). All other patient characteristics, communications, and behaviors were held constant. By doing so, the example study demonstrated that the patient's body size alone was sufficient to elicit biased reactions from medical students in isolation from other factors often confounded with body size (e.g., comorbid health conditions, communication styles33,34). This is a clear example of the first advantage of using a VR platform for experimental research. That is, VR allows presentation and control of any object or characteristic, even those that are difficult or impossible to change or control in real life.3,4
In future obesity prevention and treatment research, a near endless array of clinical or interpersonal factors could be manipulated in a VR research environment. It is particularly powerful that VR enables complete control over virtual humans. For example, in addition to visible weight, it may be profitable to study the impact of a virtual patient's or clinician's gender, race, attractiveness, and so on.28,35–39 Work of this nature could illuminate social factors (such as racial or gender match between patient and provider) that influence weight-related medical encounters. In future research, it may also be useful to control nonverbal behavior of virtual humans. In the example study, nonverbal behavior was held constant between the obese and nonobese patient. However, nonverbal behaviors could instead be manipulated to study their effects.40 In doing so, we could learn more about subtle behaviors that influence the outcomes of weight-related communication between patients and providers. Beyond personal behaviors and characteristics, VR allows the creation of any desired scenario, whether or not that scenario could or would occur in reality. This capability might be especially promising for assessing the impact of potential future health care innovations on weight-related medical encounters. For example, simulating a weight-focused medical encounter that integrates genomic information can help us gauge the impact of these technologies before they become widely available.41
Also advantageous is that, within VR, hypothetical research scenarios can be situated in realistic, tangible environments. In the example study, participants interacted with an embodied virtual patient within an immersive, visually realistic clinical environment. Unlike traditional methodologies (e.g., written vignettes), study participants can interact with and react to actual experimental stimuli in environments that contain realistic cues. For this reason, VR research environments are posited to heighten the external validity of research findings.4
A related advantage of using VR is that, by the very nature of the technology, every element in a research scenario is tightly controlled. Therefore, researchers are able to create situations that isolate variables of interest and eliminate extraneous variables and confounds. Moreover, due to this tight control, every study participant can have the exact same experience. This allows near perfect replication between participants, studies, laboratories, or time points. This level of experimental control was evident in the example study in that the virtual patient behaved identically in every interaction with every study participant.
The ability of VR research platforms to provide both high levels of control and high levels of realism is one of its greatest assets.3,4 In traditional research settings,the more realistic an experimental situation is, the less control researchers typically have over the environment.42 For example, the more an environment approaches a real clinic, the less control researchers tend to have over features like event timing, interruptions, and background noise. Virtual reality simulations can overcome this dilemma.
Finally, VR environments can not only be designed to create and experimentally vary study elements, but also be constructed to serve as behavioral measures. Behavioral measures play a crucial role in obesity prevention and management research but are often difficult to design, administer, and quantify. In VR environments, it becomes a relatively simple matter to unobtrusively record and analyze nonverbal behaviors like visual gaze and interpersonal distance that occur in clinical or other interpersonal scenarios.30 In the example study, the VR system automatically collected data that allowed for objective assessment of participants' visual contact with the virtual patient (a proxy for eye contact). The study demonstrated that medical students' level of visual contact with the patient differed depending on the patient's weight. This finding is important because nonverbal behaviors like eye contact relate to patient satisfaction in medical visits.43 Furthermore, previous work has determined that gaze behavior in some VR situations can be indicative of psychological constructs like inter-personal attention and bias.38,40
In addition to embedding nonverbal behavioral assessment in interpersonal VR scenarios, researchers can also develop virtual environments whose primary purpose is to measure a particular behavior of interest. This approach can facilitate assessment of real, quantifiable behaviors in a realistic-looking environment while participants are actually situated in a controlled laboratory. Like other VR environments, those designed for use as behavioral measures can be created to reflect any desired scenario, most notably those related to dietary intake or physical activity. At the same time, because they are virtual, researchers have control over all elements of the measurement scenario and can assess behavior in precise and fine-grained ways. For example, in our group, we are currently testing the effects of a dietary intervention using a virtual environment wherein users select food from a buffet table. Researchers can thereby directly measure several aspects of participant behavior, including not only the types and amounts of foods they select, but also patterns, order, and timing of these choices. Assessment of participant behaviors in a laboratory environment can require fewer resources than behavioral assessment in analogous “real” environments. In addition, virtual scenarios, unlike real environments, are stable over time and therefore may allow for better reliability in longitudinal assessments and for more exact replication between participants and studies. Although there is currently no published work employing virtual simulations to measure obesity-related lifestyle behaviors, such measures have been successfully developed to assess other related health behaviors.44,45
Potential Challenges of Applying Immersive Virtual Reality Methods
Although this article has reviewed several potentially advantageous features of VR platforms for enhancing basic and applied obesity prevention and management research, it is important to note that these features are not necessarily beneficial for all investigations. There is frequent temptation to use novel tools for their own sake. It is important to recognize that many, if not most, research questions can be adequately addressed using traditional methods. There are several challenges and tradeoffs in employing the VR methods that have been previously described.1,2,46 These include current technological limitations of computer graphics, software, and VR hardware. For example, the extent to which participants can engage in spontaneous, natural communication with virtual humans has been limited by the need for developments in artificial intelligence, voice recognition software, and databases that catalog appropriate verbal responses for research scenarios. There are, however, several strategies that can be used to constrain or simulate communication such that interactions can feel psychologically real to the user and elicit natural social behavior.21
There has also been much discussion about the potential for some VR environments to cause motion sickness in some individuals (i.e., cybersickness).47 While this possibility is important to consider in the design of virtual environments, several studies have suggested that symptoms rates in VR environments used in social or medical research can be quite low.48,49
Cost of acquiring the necessary equipment is another obvious concern. Virtual reality equipment can already be purchased at varying degrees of quality at varying price points, though top-quality equipment can be quite expensive. As the cost of computer hardware continues to decrease, it is expected that costs of VR hardware will also diminish. Costs of developing VR scenarios or “worlds” are another important consideration. Developing some types of virtual worlds can be costly, particularly those that do not build on existing programs or infrastructure. Cost assessments, however, should consider that once an experimental scenario is created, it can be used for many iterations, replicated in any facility with the required equipment, and altered for use in future work. In all, it is important to consider the potential challenges and drawbacks as well as potential advantages when considering integration of VR methods in obesity prevention and management research programs.
Conclusion
The studies and ideas described here barely scratch the surface of what is possible in the application of VR to basic and applied obesity prevention and treatment research. Virtual-reality-enabled research is ready to be applied to establish important causal relationships and strengthen theoretical models that explain obesity-related communi-cation and behavior. In so doing, we can contribute to evidence-based intervention and practice innovation to enhance obesity prevention and weight management.
Abbreviations
- VR
virtual reality
References
- 1.Fox J, Arena D, Bailenson JN. Virtual reality: A survival guide for the social scientist. J Media Psychol. 2009;21(3):95–113. [Google Scholar]
- 2.Persky S, McBride CM. Immersive virtual environment technology: a promising tool for future social and behavioral genomics research and practice. Health Commun. 2009;24(8):677–682. doi: 10.1080/10410230903263982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Blascovich J, Loomis J, Beall A, Swinth K, Hoyt C, Bailenson J. Immersive virtual environment technology as a research tool for social psychology. Psychol Inquiry. 2002;13:103–125. [Google Scholar]
- 4.Loomis JM, Blascovich JJ, Beall AC. Immersive virtual environment technology as a basic research tool in psychology. Behav Res Methods Instrum Comput. 1999;31(4):557–564. doi: 10.3758/bf03200735. [DOI] [PubMed] [Google Scholar]
- 5.McCall C, Blascovich J. How, when, and why to use digital experimental virtual environments to study social behavior. Soc Person Psychol Compass. 2009;3:744–758. [Google Scholar]
- 6.Tham M, Young D. The role of the general practitioner in weight management in primary care–a cross sectional study in general practice. BMC Fam Pract. 2008;9:66. doi: 10.1186/1471-2296-9-66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Thande NK, Hurstak EE, Sciacca RE, Giardina EG. Management of obesity: A challenge for medical training and practice. Obesity (Silver Spring) 2009;17(1):107–113. doi: 10.1038/oby.2008.478. [DOI] [PubMed] [Google Scholar]
- 8.Hayden MJ, Dixon JB, Piterman L, O'Brien PE. Physician attitudes, beliefs, and barriers towards the management and treatment of adult obesity: a literature review. Aust J Prim Health. 2008;14(3):9–18. [Google Scholar]
- 9.Stafford RS, Farhat JH, Misra B, Schoenfeld DA. National patterns of physician activities related to obesity management. Arch Fam Med. 2000;9(7):631–638. doi: 10.1001/archfami.9.7.631. [DOI] [PubMed] [Google Scholar]
- 10.Kushner RF. Tackling obesity: is primary care up to the challenge? Arch Intern Med. 2010;170(2):121–123. doi: 10.1001/archinternmed.2009.479. [DOI] [PubMed] [Google Scholar]
- 11.Mann T, Tomiyama AJ, Westling E, Lew AM, Samuels B, Chatman J. Medicare's search for effective obesity treatments: diets are not the answer. Am Psychol. 2007;62(3):220–233. doi: 10.1037/0003-066X.62.3.220. [DOI] [PubMed] [Google Scholar]
- 12.Jeffery RW, Drewnowski A, Epstein LH, Stunkard AJ, Wilson GT, Wing RR, Hill DR. Long-term maintenance of weight loss: current status. Health Psychol. 2000;19(1 Suppl):5–16. doi: 10.1037/0278-6133.19.suppl1.5. [DOI] [PubMed] [Google Scholar]
- 13.Tsai AG, Wadden TA. Treatment of obesity in primary care practice in the United States: a systematic review. J Gen Intern Med. 2009;24(9):1073–1079. doi: 10.1007/s11606-009-1042-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dansinger ML, Tatsioni A, Wong JB, Chung M, Balk EM. Meta-analysis: the effect of dietary counseling for weight loss. Ann Intern Med. 2007;147(1):41–50. doi: 10.7326/0003-4819-147-1-200707030-00007. [DOI] [PubMed] [Google Scholar]
- 15.Kumanyika SK, Van Horn L, Bowen D, Perri MG, Rolls BJ, Czajkowski SM, Schron E. Maintenance of dietary behavior change. Health Psychol. 2000;19(1 Suppl):42–56. doi: 10.1037/0278-6133.19.suppl1.42. [DOI] [PubMed] [Google Scholar]
- 16.Bocquier A, Verger P, Basdevant A, Andreotti G, Baretge J, Villani P, Paraponaris A. Overweight and obesity: knowledge, attitudes, and practices of general practitioners in France. Obes Res. 2005;13(4):787–795. doi: 10.1038/oby.2005.89. [DOI] [PubMed] [Google Scholar]
- 17.Puhl RM, Heuer CA. The stigma of obesity: a review and update. Obesity (Silver Spring) 2009;17(5):941–964. doi: 10.1038/oby.2008.636. [DOI] [PubMed] [Google Scholar]
- 18.Amy NK, Aalborg A, Lyons P, Keranen L. Barriers to routine gynecological cancer screening for White and African-American obese women. Int J Obes (Lond) 2006;30(1):147–155. doi: 10.1038/sj.ijo.0803105. [DOI] [PubMed] [Google Scholar]
- 19.U.S. Preventive Services Task Force. Screening for obesity in adults: recommendations and rationale. Ann Intern Med. 2003;139(11):930–932. doi: 10.7326/0003-4819-139-11-200312020-00012. [DOI] [PubMed] [Google Scholar]
- 20.Roter DL. Observations on methodological and measurement challenges in the assessment of communication during medical exchanges. Patient Educ Couns. 2003;50(1):17–21. doi: 10.1016/s0738-3991(03)00074-0. [DOI] [PubMed] [Google Scholar]
- 21.Persky S. Employing immersive virtual environments for innovative experiments in health care communication. Patient Educ Couns. 2011 doi: 10.1016/j.pec.2010.12.007. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Riva G. Virtual reality in psychotherapy: review. Cyberpsychol Behav. 2005;8(3):220–230. doi: 10.1089/cpb.2005.8.220. [DOI] [PubMed] [Google Scholar]
- 23.Parsons TD, Rizzo AA. Affective outcomes of virtual reality exposure therapy for anxiety and specific phobias: a meta-analysis. J Behav Ther Exp Psychiatry. 2008;39(3):250–261. doi: 10.1016/j.jbtep.2007.07.007. [DOI] [PubMed] [Google Scholar]
- 24.Johnsen K, Raij A, Stevens A, Lind DS, Lok B. The validity of a virtual human experience for interpersonal skills education. Presented at: 25th SIGCHI Conference on Human Factors in Computing Systems; April 28–May 3; San Jose, CA. 2007. [Google Scholar]
- 25.Raij AB, Johnsen K, Dickerson RF, Lok BC, Cohen MS, Duerson M, Pauly RR, Stevens AO, Wagner P, Lind DS. Comparing interpersonal interactions with a virtual human to those with a real human. IEEE Trans Vis Comput Graph. 2007;13(3):443–457. doi: 10.1109/TVCG.2007.1036. [DOI] [PubMed] [Google Scholar]
- 26.Deladisma AM, Cohen M, Stevens A, Wagner P, Lok B, Bernard T, Oxendine C, Schumacher L, Johnsen K, Dickerson R, Raij A, Wells R, Duerson M, Harper JG, Lind DS, Association for Surgical Education Do medical students respond empathetically to a virtual patient? Am J Surg. 2007;193(6):756–760. doi: 10.1016/j.amjsurg.2007.01.021. [DOI] [PubMed] [Google Scholar]
- 27.Fox J, Bailenson J, Binney J. Virtual experiences, physical behaviors: the effect of presence on imitation of an eating avatar. Presence. 2009;18(4):294–303. [Google Scholar]
- 28.Rossen B, Johnsen K, Deladisma A, Lind S, Lok B. Berlin: Springer; 2008. Virtual humans elicit skin-tone bias consistent with real-world skin-tone biases. Intelligent virtual agents: lecture notes in computer science; pp. 237–244. [Google Scholar]
- 29.Hoyt CL, Blascovich J, Swinth KR. Social inhibition in immersive virtual environments. Presence. 2003;12(2):183–195. [Google Scholar]
- 30.Bailenson JN, Blascovich J, Beall AC, Loomis JM. Interpersonal distance in immersive virtual environments. Pers Soc Psychol Bull. 2003;29(7):819–833. doi: 10.1177/0146167203029007002. [DOI] [PubMed] [Google Scholar]
- 31.Slater M, Antley A, Davison A, Swapp D, Guger C, Barker C, Pistrang N, Sanchez-Vives MV. A virtual reprise of the Stanley Milgram obedience experiments. PLoS One. 2006;1:e39. doi: 10.1371/journal.pone.0000039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Persky S, Eccleston CP. Medical student bias and care recommenda-tions for an obese versus non-obese virtual patient. Int J Obes (Lond) 2010 doi: 10.1038/ijo.2010.173. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Miller CT, Rothblum ED, Barbour L, Brand PA, Felicio D. Social interactions of obese and nonobese women. J Pers. 1990;58(2):365–380. doi: 10.1111/j.1467-6494.1990.tb00234.x. [DOI] [PubMed] [Google Scholar]
- 34.Must A, Spadano J, Coakley EH, Field AE, Colditz G, Dietz WH. The disease burden associated with overweight and obesity. JAMA. 1999;282(16):1523–1529. doi: 10.1001/jama.282.16.1523. [DOI] [PubMed] [Google Scholar]
- 35.Yee N, Bailenson J. The Proteus effect: the effect of transformed self-representation on behavior. Human Commun Res. 2007;33(3):271–290. [Google Scholar]
- 36.Hoyt CL, Aguilar L, Kaiser CR, Blascovich J, Lee K. The self-protective and undermining effects of attributional ambiguity. J Exp Soc Psychol. 2007;43(6):884–893. [Google Scholar]
- 37.Schmid Mast M, Hall JA, Roter DL. Disentangling physician sex and physician communication style: their effects on patient satisfaction in a virtual medical visit. Patient Educ Couns. 2007;68(1):16–22. doi: 10.1016/j.pec.2007.03.020. [DOI] [PubMed] [Google Scholar]
- 38.McCall C, Blascovich J, Young A, Persky S. Proxemic behaviors as predictors of aggression towards black (but not white) males in an immersive virtual environment. Soc Influence. 2009;4:138–154. [Google Scholar]
- 39.Fox J, Bailenson JN. Virtual self-modeling: the effects of vicarious reinforcement and identification on exercise behaviors. Media Psychol. 2009;12(1):1–25. [Google Scholar]
- 40.Bailenson JN, Beal A, Loomis J, Blascovich J, Turk M. Transformed social interaction, augmented gaze, and social influence in immersive virtual environments. Human Commun Res. 2005;31(4):511–537. [Google Scholar]
- 41.Persky S, Eccleston CP. Impact of genetic causal information on medical students' encounters with an obese virtual patient: health promotion and social stigma. Ann Behav Med. 2010 doi: 10.1007/s12160-010-9242-0. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Rosenthal R, Rosnow RL. Essentials of behavioral research: methods and data analysis. Boston: McGraw-Hill; 1991. [Google Scholar]
- 43.Roter DL, Frankel RM, Hall JA, Sluyter D. The expression of emotion through nonverbal behavior in medical visits. Mechanisms and outcomes. J Gen Intern Med. 2006;21(Suppl 1):S28–34. doi: 10.1111/j.1525-1497.2006.00306.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Gorini A, Griez E, Petrova A, Riva G. Assessment of the emotional responses produced by exposure to real food, virtual food and photographs of food in patients affected by eating disorders. Ann Gen Psychiatry. 2010;9:30. doi: 10.1186/1744-859X-9-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Traylor AC, Bordnick PS, Carter BL. Using virtual reality to assess young adult smokers' attention to cues. Cyberpsychol Behav. 2009;12(4):373–378. doi: 10.1089/cpb.2009.0070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Rizzo A, Kim GJ. A SWOT analysis of the field of virtual reality rehabilitation and therapy. Presence. 2005;14(2):119–146. [Google Scholar]
- 47.Stanney KM, Mourant RR, Kennedy RS. Human factors issues in virtual environments: a review of the literature. Presence. 1998;7(4):327–351. [Google Scholar]
- 48.Bailenson JN, Yee N. A longitudinal study of task performance, head movements, subjective report, simulator sickness, and transformed social interaction in collaborative virtual environments. Presence. 2006;15(6):699–716. [Google Scholar]
- 49.Schneider SM, Prince-Paul M, Allen MJ, Sliverman P, Talaba D. Virtual reality as a distraction intervention for women receiving chemotherapy. Oncol Nurs Forum. 2004;31(1):81–88. doi: 10.1188/04.ONF.81-88. [DOI] [PubMed] [Google Scholar]