Abstract
Glycemic variability has become a major concern over the years as growing evidence is gathered on its detrimental impact on the risk of diabetes complications. Glycated hemoglobin, although ubiquitous in clinical practice, does not adequately summarize short-term glycemic variability. This gap may be addressed through the use of continuous glucose monitoring, which continuously estimates glycemia based on interstitial fluid glucose concentration. As the amount of collected data is substantial, variability of the glycemic pattern can be analyzed in context of its direction, periodicity, and amplitude. As freely available variability calculation tools are limited in number and complexity, the authors have devised a simple-to-use Web-based application, “GlyCulator,” allowing for rapid computation of glucose variability parameters from continuous glucose monitoring data.
Keywords: continuous glucose monitoring, diabetes, glycemic variability, statistical analysis
Background
Glycemic variability was documented to increase metabolic stress and mortality in acute states.1–5 An increasing number of studies show that sole use of glycated hemoglobin (HbA1c), the cornerstone of long-term monitoring of metabolic control, is not sufficient to adequately assess the metabolic status of patients with diabetes. The risk of developing diabetes-related complications is related not only to long-term glycemic variability,6 but may also be related to short-term glucose variability from peaks to nadirs.4 Oscillating glucose concentration may exert more deleterious effects than sustained chronic hyperglycemia on endothelial function and oxidative stress, two key players in the development and progression of cardiovascular diseases in diabetes.7 Such short-term fluctuations, however, may be detectable by means of continuous glucose monitoring (CGM)—a method that measures glycemia continuously over a period of several days. A large amount of resulting data is, however, cumbersome to use in research studies and requires some simplification and transformation into usable parameters. To address the evident paucity of glucose variability calculation tools, the authors have devised a Web-based application for rapid computation of numerous glucose variability parameters from CGM data: “GlyCulator.”
Parameters of Glycemic Variability
Percentage of glucose values above or below a given threshold measured as the percentage of hyperglycemia (levels between 126 and 180 mg/dl) and hypoglycemia (levels below 70.2 mg/dl) episodes. These are the most clinically applicable and intuitive parameters of glycemic variability, though they are difficult to use for research purposes.8
The standard deviation (SD) of mean glycemia of CGM data is probably the simplest tool for assessment of glycemic variability.9 Calculation of this parameter provides information for both minor and major fluctuations but not does distinguish them. For a more detailed assessment of day-to-day variability, several methods based on SD can be marked out, such as the average SD within corresponding time points of multiple days (SDw), SD between multiple days within corresponding time points (SDb hh:mm), SD between daily means (SDdm), and SD between days within corresponding time points after including variation of daily means (SDb hh:mm//dm).10,11
Percentage coefficient of variation (%CV) is the ratio of SD to mean. This parameter describes the magnitude sample values and the variation within them and allows for standardized comparisons between patients with different levels of mean glycemia.
Mean amplitude of glycemic excursions (MAGE), together with mean and SD, is the most popular parameter for assessing glycemic variability and is calculated based on the arithmetic mean of differences between consecutive peaks and nadirs of differences greater than one SD of mean glycemia. It is designed to assess major glucose swings and exclude minor ones.12
Weighted average of glucose values (MR) provides a measure of stability of glycemia in comparison with an arbitrary assigned “ideal” glucose value, “R,” initially set to 100 mg/dl. It is obtained as mean of values transformed using the following formula: 1000 × |log10(glucose/100)|3.13
J index is a measure of quality of glycemic control based on the combination of information from the mean and SD calculated as 0.001 × (mean + SD)2.14
The mean of daily differences (MODD) index provides an estimation of interday glycemic variability. This parameter is calculated as the mean of absolute differences between glucose values at corresponding time points of consecutive days.15
Continuous overall net glycemic action (CONGA) is similar to SD but assesses glucose variability within a predetermined time window. Calculation of this parameter is based on the assessment of the differences between glucose values measured at regular time intervals, then on the SD of these differences.16
Fractal dimension (FD) is an experimental method, based on the works of Higuchi and currently adapted by the authors, that describes glucose variability of high frequency and small amplitude. The calculation is based on the changes of glucose values between subsequent measurements using the Higuchi algorithm.17,18
Firmware Design and Methods
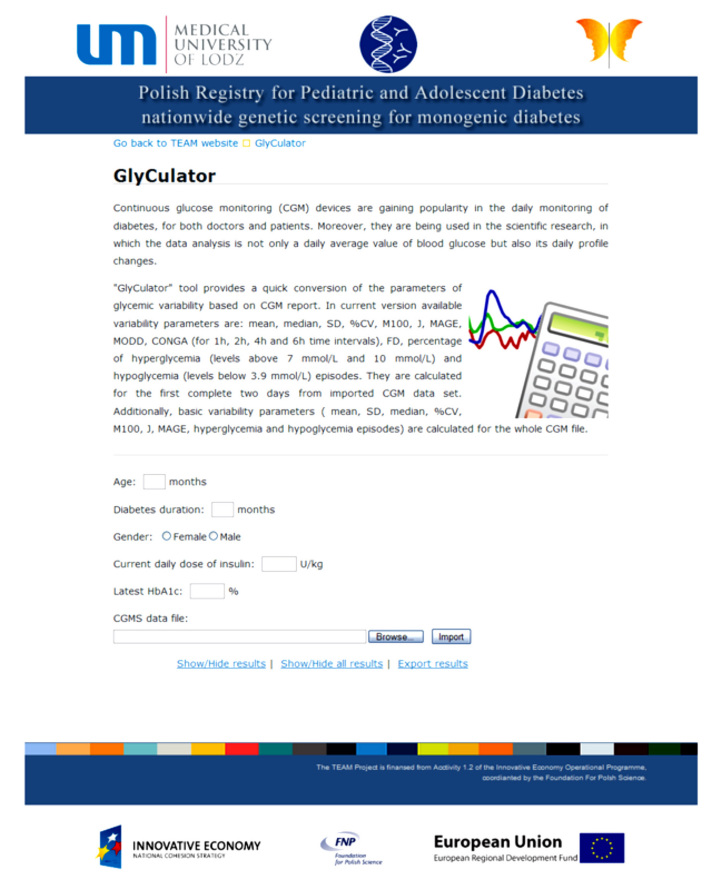
“GlyCulator” is an application designed to evaluate glycemic variability based on data collected by means of a CGM device. The application is available in two versions. A platform-independent Web-based interface is presented in Figure 1. This version is available online at www.pediatria.umed.pl/team/glyculator. A more complex Windows-based tool shown in Figure 2 can be installed on a computer running any contemporary Microsoft Windows operating system (Microsoft.Net Framework v.4.0 or above is required). This version is available on request from the authors. Both versions share the same core functionality of reading data previously exported from any CGM device.
Figure 1.
Graphic user interface screen image presenting the Web-based application.
Figure 2.
Graphic user interface screen image presenting the Windows-based application.
The main requirement is that the CGM data need to be exported to a Microsoft Excel 2003 file (.xls file). The choice of this file format was based on its popularity and the fact that most CGM devices provide some “export to Excel” functionality.
After loading a data set, the user is prompted to select the sheet and columns with measurement date and time and corresponding blood glucose sensor value. Each file will be assigned with a unique identifier for collective database construction. In the Windows-based version, the following settings can be adjusted: number of readings per day/hour (default set to 288/12) and initial time point (default set to noon), which gives an option to analyze specific periods (i.e., days or nights). Moreover, the user can choose units (mmol/liter or mg/dl) and reading mode (single file or batch import). In both versions available, variability parameters are mean, median, SD, SDw, SDb hh:mm, SDdm, SDb hh:mm//dm, %CV, M100, J, MAGE, MODD, CONGA (for 1, 2, 4, 6, and 24 h time intervals), FD, and percentage of hyperglycemia (levels between 7 and 10 mmol/liter) and hypoglycemia (levels below 3.9 mmol/liter) episodes. All parameters are calculated for the first complete two days from the imported CGM data set. Additionally, basic variability parameters (mean, SD, median, %CV, M100, J, MAGE, and hyperglycemia and hypoglycemia episodes) are calculated for the whole CGM file. Optionally, GlyCulator allows the user to enter additional clinical data, such as patient’s age, gender, duration of the diabetes, current daily dose of insulin, and latest HbA1c level and link them with the imported patient CGM file. The Windows-based version allows multiple file analyses of all .xls files stored in the chosen directory, provided they have the same structure of columns containing date/time stamps and corresponding sensor values. After calculation, a summary report can be saved as an excel database file for further analysis. Additionally, the Web-based version allows the user to preview results before saving to .xls.
Conclusions
Glycemic variability has become a major concern over the years as growing evidence has been gathered on its detrimental impact on oxidative stress1,19,20 and dysregulation of adipokine secretion.2 Clinically, glycemic variability was associated with greater mortality in intensive care,3,5 increased rate of diabetes complications,21 and postprandial beta-cell dysfunction.22 However, data on the significance of glycemic variability is not as unequivocal as one could expect, with reports abolishing its importance altogether mixing with those in favor.6,23,24 The features discouraging use of glycemic variability as a parameter in clinical practice and trials are the difficulty of interpreting numerous parameters describing this phenomenon and a limited number of computational opportunities allowing rapid calculation of glycemic variability parameters in CGM data. Clinical benefits of using these devices have been well documented and range from reduced frequency of hypoglycemia to improved metabolic control.9,25,26 In order to facilitate access to glycemic variability parameters, the authors developed an application for quantifying the most popular glucose variability parameters, including a novel measurement currently tested by the group (FD). The Web-based application allows input of several clinical parameters to facilitate database construction and integration of variability data with clinical characteristics. As parameters included in the current version are by no means a conclusive list, further development, based on the suggestions of users and the development of novel glucose variability measurements, is warranted. The software was mainly intended for research purposes and use with short CGM recordings (∼72 h, with two complete days), although the algorithms used allow reconfiguration and analysis of longer data traces, with a modified software version available on demand.
Abbreviations
- (%CV)
percentage coefficient of variation
- (CGM)
continuous glucose monitoring
- (CONGA)
continuous overall net glycemic action
- (FD)
fractal dimension
- (HbA1c)
glycated hemoglobin
- (MAGE)
mean amplitude of glycemic excursions
- (MODD)
mean of daily differences
- (SD)
standard deviation
References
- 1.Sun J, Xu Y, Sun S, Sun Y, Wang X. Intermittent high glucose enhances cell proliferation and VEGF expression in retinal endothelial cells: the role of mitochondrial reactive oxygen species. Mol Cell Biochem. 2010;343(1-2):27–35. doi: 10.1007/s11010-010-0495-5. [DOI] [PubMed] [Google Scholar]
- 2.Sun J, Xu Y, Deng H, Sun S, Dai Z, Sun Y. Intermittent high glucose exacerbates the aberrant production of adiponectin and resistin through mitochondrial superoxide overproduction in adipocytes. J Mol Endocrinol. 2010;44(3):179–185. doi: 10.1677/JME-09-0088. [DOI] [PubMed] [Google Scholar]
- 3.Krinsley JS. Glycemic variability in critical illness and the end of Chapter 1. Crit Care Med. 2010;38(4):1206–1208. doi: 10.1097/CCM.0b013e3181d3aba5. [DOI] [PubMed] [Google Scholar]
- 4.Monnier L, Mas E, Ginet C, Michel F, Villon L, Cristol JP, Colette C. Activation of oxidative stress by acute glucose fluctuations compared with sustained chronic hyperglycemia in patients with type 2 diabetes. JAMA. 2006;295(14):1681–1687. doi: 10.1001/jama.295.14.1681. [DOI] [PubMed] [Google Scholar]
- 5.Hermanides J, Vriesendorp TM, Bosman RJ, Zandstra DF, Hoekstra JB, Devries JH. Glucose variability is associated with intensive care unit mortality. Crit Care Med. 2010;38(3):838–842. doi: 10.1097/CCM.0b013e3181cc4be9. [DOI] [PubMed] [Google Scholar]
- 6.Kilpatrick ES, Rigby AS, Atkin SL. A1C variability and the risk of microvascular complications in type 1 diabetes: data from the Diabetes Control and Complications Trial. Diabetes Care. 2008;31(11):2198–2202. doi: 10.2337/dc08-0864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Monnier L, Colette C, Owens DR. Glycemic variability: the third component of the dysglycemia in diabetes. Is it important? How to measure it? J Diabetes Sci Technol. 2008;2(6):1094–1100. doi: 10.1177/193229680800200618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Clarke W, Kovatchev B. Statistical tools to analyze continuous glucose monitor data. Diabetes Technol Ther. 2009;11(Suppl 1):S45–54. doi: 10.1089/dia.2008.0138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rodbard D, Bailey T, Jovanovic L, Zisser H, Kaplan R, Garg SK. Improved quality of glycemic control and reduced glycemic variability with use of continuous glucose monitoring. Diabetes Technol Ther. 2009;11(11):717–723. doi: 10.1089/dia.2009.0077. [DOI] [PubMed] [Google Scholar]
- 10.Rodbard D. Interpretation of continuous glucose monitoring data: glycemic variability and quality of glycemic control. Diabetes Technol Ther. 2009;11(Suppl 1):S55–67. doi: 10.1089/dia.2008.0132. [DOI] [PubMed] [Google Scholar]
- 11.Rodbard D. New and improved methods to characterize glycemic variability using continuous glucose monitoring. Diabetes Technol Ther. 2009;11(9):551–565. doi: 10.1089/dia.2009.0015. [DOI] [PubMed] [Google Scholar]
- 12.Service FJ, Molnar GD, Rosevear JW, Ackerman E, Gatewood LC, Taylor WF. Mean amplitude of glycemic excursions, a measure of diabetic instability. Diabetes. 1970;19(9):644–655. doi: 10.2337/diab.19.9.644. [DOI] [PubMed] [Google Scholar]
- 13.Wójcicki JM. Mathematical descriptions of the glucose control in diabetes therapy. Analysis of the Schlichtkrull “M”-value. Horm Metab Res. 1995;27(1):1–5. doi: 10.1055/s-2007-979895. [DOI] [PubMed] [Google Scholar]
- 14.Wójcicki JM. “J”-index. A new proposition of the assessment of current glucose control in diabetic patients. Horm Metab Res. 1995;27(1):41–42. doi: 10.1055/s-2007-979906. [DOI] [PubMed] [Google Scholar]
- 15.Molnar GD, Taylor WF, Ho MM. Day-to-day variation of continuously monitored glycaemia: a further measure of diabetic instability. Diabetologia. 1972;8(5):342–348. doi: 10.1007/BF01218495. [DOI] [PubMed] [Google Scholar]
- 16.McDonnell CM, Donath SM, Vidmar SI, Werther GA, Cameron FJ. A novel approach to continuous glucose analysis utilizing glycemic variation. Diabetes Technol Ther. 2005;7(2):253–263. doi: 10.1089/dia.2005.7.253. [DOI] [PubMed] [Google Scholar]
- 17.Fendler W, Tucholski K, Walenciak L, Jarosz-Chobot P, Mlynarski W. Fractal dimension analysis of continuous glucose monitoring data in screening for hypoglycemia-prone patients with type 1 diabetes – preliminary report. 2nd Advanced Technologies and Treatments for Diabetes. 2009 [Google Scholar]
- 18.Higuchi T. Approach to an irregular time series on the basis of the fractal theory. Physica D. 1988;31(2):277–283. [Google Scholar]
- 19.Monnier L, Colette C, Leiter L, Ceriello A, Hanefeld M, Owens D, Tajima N, Tuomiletho J, Davidson J, PGR Group The effect of glucose variability on the risk of microvascular complications in type 1 diabetes. Diabetes Care. 2007;30(1):185–186. doi: 10.2337/dc06-1594. [DOI] [PubMed] [Google Scholar]
- 20.Fendler WM, Mlynarski WM. Insulin therapy in very-low-birth-weight infants. N Engl J Med. 2009;360(5):535–536. [PubMed] [Google Scholar]
- 21.Takao T, Ide T, Yanagisawa H, Kikuchi M, Kawazu S, Matsuyama Y. The effect of fasting plasma glucose variability on the risk of retinopathy in type 2 diabetic patients: retrospective long-term follow-up. Diabetes Res Clin Pract. 2010;89(3):296–302. doi: 10.1016/j.diabres.2010.03.027. [DOI] [PubMed] [Google Scholar]
- 22.Kohnert KD, Augstein P, Zander E, Heinke P, Peterson K, Freyse EJ, Hovorka R, Salzsieder E. Glycemic variability correlates strongly with postprandial beta-cell dysfunction in a segment of type 2 diabetic patients using oral hypoglycemic agents. Diabetes Care. 2009;32(6):1058–1062. doi: 10.2337/dc08-1956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kilpatrick ES, Rigby AS, Atkin SL. The effect of glucose variability on the risk of microvascular complications in type 1 diabetes. Diabetes Care. 2006;29(7):1486–1490. doi: 10.2337/dc06-0293. [DOI] [PubMed] [Google Scholar]
- 24.Service FJ, O’Brien PC. The effect of glucose variability on the risk of microvascular complications in type 1 diabetes. Diabetes Care. 2007;30(1):186–188. doi: 10.2337/dc06-1782. [DOI] [PubMed] [Google Scholar]
- 25.Leinung M, Thompson S, Nardacci E. Benefits of continuous glucose monitor use in clinical practice. Endocr Pract. 2010;16(3):371–375. doi: 10.4158/EP09287.OR. [DOI] [PubMed] [Google Scholar]
- 26.Kudva YC, Basu A, Jenkins GD, Pons GM, Vogelsang DA, Rizza RA, Smith SA, Isley WL. Glycemic variation and hypoglycemia in patients with well-controlled type 1 diabetes on a multiple daily insulin injection program with use of glargine and ultralente as basal insulin. Endocr Pract. 2007;13(3):244–250. doi: 10.4158/EP.13.3.244. [DOI] [PubMed] [Google Scholar]