Zaire Ebola virus (ZEBOV) is the most lethal Ebola virus species and one of the most virulent human pathogens, causing a severe hemorrhagic fever syndrome that ends in the death of 90% of symptomatic patients within a few days (11). ZEBOV caused numerous human outbreaks in Central Africa between 1976 and 2008 and also devastated wild populations of nonhuman primates (2, 10, 13). Recent studies show that ZEBOV infection induces profound suppression of adaptive immunity, characterized by massive B- and T-lymphocyte apoptosis both in humans and in experimentally infected animals (1, 3, 5–6, 14).
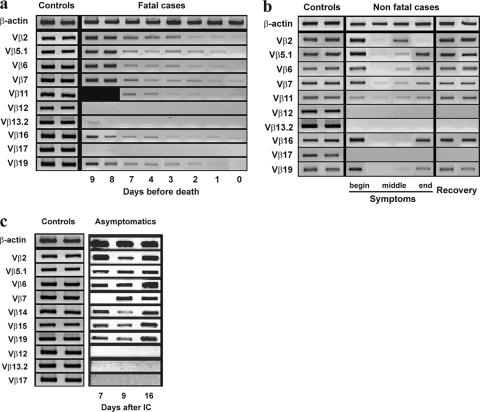
Lymphocytes are not infected by ZEBOV, and the mechanisms leading to this massive lymphocyte apoptosis are unclear. As the final shock-like syndrome associated with fatal ZEBOV infection resembles the toxic shock syndrome observed during infections with Gram-positive bacteria with superantigen (SAg) activity, we wondered if ZEBOV might also exhibit SAg activity. SAgs are microbial proteins that bind simultaneously to major histocompatibility complex class II molecules and to the T-cell receptor (TCR) Vβ region. This “bridge” skews the T-cell repertoire by amplifying specific T-cell Vβ subsets, which then are either rapidly deleted by activated cell death or become anergic (4, 7). Thus, we examined the TCR Vβ repertoire of peripheral blood mononuclear cells isolated from acutely infected patients by using PCR-based methods. Surprisingly, TCR Vβ12, Vβ13.2, and Vβ17 mRNA expression was undetectable throughout the symptomatic phase in ZEBOV victims, in survivors but also in three of seven asymptomatic individuals identified during the 1996 Booué outbreak in Gabon (9) (Fig. 1). Furthermore, expression of the other TCR-Vβ chains in deceased patients diminished as the disease progressed, reaching very low levels the day before death. In contrast, mRNA expression of the other Vβ chains was normally upregulated to the same level as β-actin mRNA in asymptomatic individuals but also at the beginning and end of the symptomatic phase and after recovery in survivors.
Fig. 1.
Reverse transcription (RT)-PCR analysis of the TCR Vβ repertoire during human Ebola virus infection. Agarose gel electrophoresis of PCR products obtained with various (n = 20) combinations of Vβ gene family-specific and Cβ oligonucleotide primers was performed. Kinetics of mRNA expression of 10 TCR Vβ species in 10 uninfected control subjects (two are shown), fatal cases, nonfatal cases, and asymptomatically infected individuals are shown. (a) RT-PCR analysis of mRNA in eight fatal cases. The time before death is indicated at the bottom. (b) RT-PCR analysis of mRNA in four nonfatal cases during the symptomatic phase and in two of these cases a few days after symptoms ended. Each patient with a nonfatal case was sampled three times during the course of the disease, and two were also sampled a few days after symptoms ended. (c) RT-PCR analysis of mRNA in three asymptomatic individuals 7, 9, and 23 days following initial contact (IC).
Together, these data show that, whatever the clinical outcome, human ZEBOV infection is associated with mRNA downregulation of three TCR Vβ subsets, indicating either anergy or deletion of the three corresponding T-lymphocyte populations. These results are consistent with ZEBOV SAg activity, the first time that it is suggested in the Filoviridae family. Whereas a large number of bacterial SAgs have been identified, only two families of viruses have SAg activity in humans, namely, Herpesviridae and Rhabdoviridae (8, 12).
These findings may represent the “missing link” in our understanding of ZEBOV pathogenicity. The SAg activity of ZEBOV might contribute to the extraordinarily rapid and profound T-lymphocyte depletion observed during fatal infection. The high viral load observed during fatal ZEBOV infection, together with the simultaneous targeting of three Vβ T-cell subsets observed here, would elicit massive lymphocyte activation, rapidly resulting in the deletion of large populations of Vβ12-, Vβ13.2-, and Vβ17-bearing T cells. The loss of mRNA expression of the other Vβ T cells would be due to the proportionally small decline in these subsets.
Acknowledgments
We thank the Gabonese and Congolese Ministries of Health and the World Health Organization International Response Team for their assistance with epidemiological studies and blood sampling.
This work was funded by a grant from the Agence Nationale pour la Recherche (appel MIME 2006, ANR-06-MIME-022-01) and a Fonds de Solidarité Prioritaire grant from the Ministère des Affaires Etrangères de la France (FSP 2002005700). The Centre International de Recherches Médicales de Franceville is supported by the Government of Gabon, Total-Fina-Elf Gabon, and the Ministère des Affaires Etrangères, France.
Footnotes
Published ahead of print on 9 February 2011.
The authors have paid a fee to allow immediate free access to this article.
Contributor Information
Pierre Becquart, MIVEGEC, UMR (IRD-CNRS-UM) 224, Institut de Recherche pour le Développement, Franceville, Gabon.
Nadia Wauquier, Unité des Maladies Virales Émergentes, Centre International de Recherches Médicales de Franceville, Franceville, Gabon.
Sylvain Baize, Unité de Biologie des Infections Virales Emergentes, Institut Pasteur, IFR128-Biosciences Gerland-Lyon Sud, Lyon, France.
REFERENCES
- 1. Baize S., et al. 1999. Defective humoral responses and extensive intravascular apoptosis are associated with fatal outcome in Ebola virus-infected patients. Nat. Med. 5:1–5 [DOI] [PubMed] [Google Scholar]
- 2. Bermejo M., et al. 2006. Ebola outbreak killed 5000 gorillas. Science 314:1564. [DOI] [PubMed] [Google Scholar]
- 3. Bradfute S. B., Warfield K. L., Bavari S. 2008. Functional CD8+ T cell responses in lethal Ebola virus infection. J. Immunol. 180:4058–4066 [DOI] [PubMed] [Google Scholar]
- 4. Fraser J. D., Proft T. 2008. The bacterial superantigen and superantigen-like proteins. Immunol. Rev. 225:226–243 [DOI] [PubMed] [Google Scholar]
- 5. Geisbert T. W., Jahrling P. B. 2004. Exotic emerging viral diseases: progress and challenges. Nat. Med. 10:S110–S121 [DOI] [PubMed] [Google Scholar]
- 6. Hensley L., Young H. A., Jahrling P. B., Geisbert T. W. 2002. Proinflammatory response during Ebola virus infection of primate models: possible involvement of the tumor necrosis factor receptor superfamily. Immunol. Lett. 80:169–179 [DOI] [PubMed] [Google Scholar]
- 7. Herman A., Kappler J. W., Marrack P., Pullen A. M. 1991. Superantigens: mechanism of T-cell stimulation and role in immune responses. Annu. Rev. Immunol. 9:745–772 [DOI] [PubMed] [Google Scholar]
- 8. Lafon M., et al. 1992. Evidence for a viral superantigen in humans. Nature 358:507–510 [DOI] [PubMed] [Google Scholar]
- 9. Leroy E. M., et al. 2000. Human asymptomatic Ebola infection and strong inflammatory response. Lancet 355:2210–2215 [DOI] [PubMed] [Google Scholar]
- 10. Leroy E. M., et al. 2004. Multiple Ebola virus transmission events and rapid decline of central African wildlife. Science 303:387–390 [DOI] [PubMed] [Google Scholar]
- 11. Sanchez A., Geisbert T. W., Feldmann H. 2007. Filoviridae: Marburg and Ebola viruses, p. 1409–1448 In Knipe D. M., Howley P. M. (ed.), Fields virology. Lippincott Williams & Wilkins, Philadelphia, PA [Google Scholar]
- 12. Sutkowski N., et al. 1996. An Epstein-Barr virus-associated superantigen. J. Exp. Med. 184:971–980 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Walsh P. D., et al. 2003. Catastrophic ape decline in western equatorial Africa. Nature 422:611–614 [DOI] [PubMed] [Google Scholar]
- 14. Wauquier N., Becquart P., Padilla C., Baize S., Leroy E. M. 2010. Human fatal Zaire Ebola virus infection is associated with an aberrant innate immunity and massive lymphocyte apoptosis. PLoS Neg. Trop. Dis. 4:e837. [DOI] [PMC free article] [PubMed] [Google Scholar]