Abstract
Although oral exposure to H5N1 highly pathogenic avian influenza viruses is a risk factor for infection in humans, it is unclear how oral exposure to these virus results in lethal respiratory infections. To address this issue, we inoculated ferrets and hamsters with two highly pathogenic H5N1 strains. These viruses, inoculated directly into the stomach, were isolated from the large intestine and the mesenteric lymph nodes within 1 day of inoculation and subsequently spread to multiple tissues, including lung, liver, and brain. Histopathologic analysis of ferrets infected with virus via direct intragastric inoculation revealed lymph folliculitis in the digestive tract and mesenteric lymph nodes and focal interstitial pneumonia. Comparable results were obtained with the hamster model. We conclude that, in mammals, ingested H5N1 influenza viruses can disseminate to nondigestive organs, possibly through the lymphatic system of the gastrointestinal tract.
INTRODUCTION
Since 1997, over 500 cases of human H5N1 influenza A virus infection have reported, with more than 300 deaths worldwide (WHO [http://www.who.int/csr/disease/avian_influenza /country/cases_table_2011_01_13/en/index.html]). These viruses remain enzootic in birds in many countries, posing a serious pandemic threat. Contact with sick birds is the most common risk factor for human infection; however, some patients are known to have consumed raw duck blood prior to the onset of their influenza-like illness. This fact highlights the importance of reports that some mammalian species, including domestic cats, leopards, tigers, and dogs, have been infected with H5N1 viruses after consuming virus-contaminated meat (5, 9, 10, 14, 16, 17).
Many patients infected with H5N1 viruses, regardless of the exposure route, develop viral pneumonia. During the early phase of human H5N1 infection, viruses are rarely isolated from the upper respiratory tract (1, 4), probably because the receptor molecules for H5N1 viruses, namely, oligosaccharides terminating with sialic acid (SA) bound to galactose by α-2,3 linkages (SAα2,3Gal), are abundant predominantly on the cells of the lower respiratory tract in humans (15, 19). Therefore, we posed the question, How might H5N1 viruses reach the lower respiratory tract, the site of severe infection in most humans, after oral exposure?
Among the several reports of oral H5N1 infections in mammals, particularly felines (5, 9, 10, 14, 17), an experiment in cats by Rimmelzwaan et al. (14) suggests two possible routes of virus entry following oral H5N1 virus exposure: the blood and the intestinal lumen. However, the latter possibility was not experimentally demonstrated in the study by Rimmelzwaan et al. since viral exposure through the respiratory tract after the consumption of virus-infected raw chicken was not excluded.
Therefore, we designed our study to investigate the intestinal viral invasion route. Our results with ferret and hamster models implicate the digestive tract in H5N1 virus invasion in mammals.
MATERIALS AND METHODS
Viruses.
A/Vietnam/UT3062/04 (UT3062; H5N1) and A/Vietnam/1203/04 (VN1203; H5N1) were propagated in Madin-Darby canine kidney (MDCK) cells. For studies of virus dissemination through the digestive system, we also prepared homogenates of 10- to 11-day-old chicken embryos infected with these virus strains.
Animal experiments. (i) Ferrets.
For intranasal infection, virus (0.5 ml; 6.0 log10 median tissue culture infectious dose [TCID50] of VN1203 or 6.2 log10 TCID50 of UT3062) was inoculated into the nostrils of 12 3-month-old ferrets (Marshall BioResources, North Rose, NY) anesthetized with isoflurane. To introduce virus directly into the stomachs of ferrets, 12 animals swallowed three petroleum-coated gelatin capsules containing homogenates of virus-infected chicken embryos (a total of 0.6 ml; 8.8 log10 TCID50 of VN1203 or 8.5 log10 TCID50 of UT3062 per animal). The ferrets were observed daily for symptoms of illness, and two or three animals were euthanized on days 1, 3, 6, and 14 or 16 to determine virus titers and pathological changes.
(ii) Hamsters.
For intranasal infection, virus (0.1 ml; 6.0 log10 TCID50 of VN1203 or 6.2 log10 TCID50 of UT3062) was inoculated into the nostrils of 12 5-week-old female golden Syrian hamsters (SLC Inc., Shizuoka, Japan) anesthetized with ketamine. For intragastric inoculation, a temporary percutaneous gastrostomy procedure was carried out on each hamster (total of 12 animals). A small metal probe was inserted through the esophagus into the stomach of each anesthetized animal, and the stomach was then lifted to the abdominal wall and secured to the abdomen with two sutures. Twenty-four hours after the procedure, virus-containing homogenates (0.5 ml; 7.3 log10 TCID50 of VN1203 or 7.1 log10 TCID50 of UT3062) were inoculated into the stomach by using a 1-ml syringe and a 23-gauge needle for direct percutaneous introduction. The hamsters were observed daily for symptoms, and virus titration was performed on days 1, 3, 6, and 16 (three animals per day).
Virus titration.
Virus titers in organs were determined as TCID50/gram tissue in MDCK cells.
Histopathologic analysis.
Tissues were fixed in 10% phosphate-buffered formalin, then dehydrated, embedded in paraffin, cut into sections, and stained with standard hematoxylin and eosin. One section was processed for immunohistochemical staining with antibodies to an H5 virus (VN1203).
RESULTS
Dissemination of the VN1203 and UT3062 viruses after intragastric inoculation of ferrets.
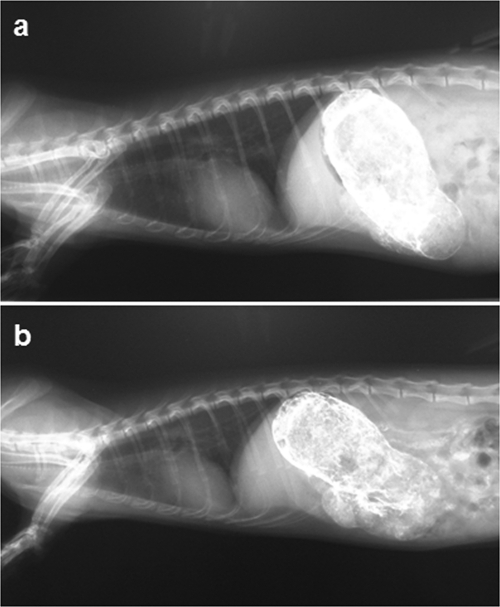
To introduce the viruses directly into the stomachs of ferrets, we used gelatin capsules. Since commercially available capsules are not sufficiently resistant to aqueous materials, we coated the inner surfaces of the capsules with petrolatum. This modification made the capsule interior resistant to water for more than 10 min, while the exterior surface remained water soluble, becoming soft in less than 4 min, and therefore dissolving in the stomach. Figure 1 shows the results of a test in which the gelatin capsules were filled with barium and then orally ingested by the ferrets (a total of 0.4 g of barium in four capsules per ferret). These capsules dissolved in the stomach, and the barium flowed through the digestive tract over a 30-min period. No ferret experienced vomiting, and the capsule contents did not leak into the respiratory organs.
Fig. 1.
Gastric delivery of gelatin capsules in ferrets. To ensure that the gelatin capsules remained intact until they reach the stomach, we coated their interiors with petrolatum (Vaseline), filled them with barium (0.4 g/capsule), and allowed the ferrets to ingest them (four capsules/animal). Lateral views 5 (a) and 30 (b) min after oral ingestion of the capsules are shown. Note that the barium (white) did not leak into the esophagus on release, but rather flowed through the digestive tract.
The pattern of infection observed after intragastric inoculation of ferrets with virus differed markedly from that following intranasal inoculation. The VN1203 virus administered intranasally was detected first in the respiratory organs and then spread to other organs, including the large intestine (Table 1). Upon intragastric administration of virus via gelatin capsules containing homogenates of virus-infected chicken embryos (a total of 0.6 ml; 8.8 log10 TCID50 of VN1203 per animal), the virus was detected in the large intestine and the mesenteric lymph nodes on day 1 postinoculation (p.i.) but was not detected in any other organ (Table 1). From day 3 p.i., the virus was detected in the respiratory organs, the tracheobronchial lymph nodes, and some organs outside the respiratory tract, such as the liver. The possibility of fecal-oral infection in these animals was excluded because no virus was detected in the organs of uninfected contact animals housed with the infected animals (data not shown).
Table 1.
Virus titers of ferret tissues infected with H5N1 viruses
| Virus | Inoculation route | Day p.i. | Virus titer(s)a (log10 TCID50/g tissue) in: |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Nasal turbinate | Trachea | Lung | TBLNb | Tonsil | Spleen | Liver | Large intestine | Mesenteric lymph node | Brain | |||
| VN1203 | Intranasal | 1 | 5.6, 7.3 | 3.1 | 5.2 | 2.2 | 4.8, 3.5 | −c | − | − | − | − |
| 3 | 5.8, 4.6 | − | 2.9 | 3.0 | 2.0, 2.0 | − | − | 1.1 | − | 1.8, 4.1 | ||
| 6 | 2.1, 2.3 | − | − | − | − | − | 2.8 | − | − | 4.1 | ||
| 16 | − | − | − | − | − | − | − | − | − | − | ||
| Intragastric | 1 | − | − | − | − | − | − | − | 4.6, 2.1 | 4.1 | − | |
| 3 | − | − | 1.9 | 2.9, 2.7 | 4.5, 3.4 | − | 4.5 | − | 4.4, 3.8 | − | ||
| 6 | 2.5 | − | − | − | − | − | 4.8 | 1.7, 1.4 | 3.1 | − | ||
| 16 | − | − | − | − | − | − | − | − | − | − | ||
| UT3062 | Intranasal | 1 | 6.4 ± 1.4 | 1.9 | 5.1 ± 0.3 | 3.9, 3.4 | 2.3 ± 0.5 | 1.1 | − | − | − | − |
| 3 | 6.3 ± 0.9 | − | 3.8 | 2.4 | 2.8 ± 0.9 | 1.1 | 5.1 | − | − | 3.9 ± 0.01 | ||
| 6 | 4.4 ± 1.8 | 1.9 | 4.8, 5.1 | 2.4 | 2.5, 1.5 | 3.8 | 4.8 ± 0.8 | 2.0 ± 1.7 | 4.6, 2.6 | 4.2 ± 1.0 | ||
| 14 | − | − | − | − | − | − | − | − | − | − | ||
| Intragastric | 1 | − | 2.9 | − | − | 3.6 | − | − | 1.5 | 3.8 | − | |
| 3 | 1.6 | − | − | − | 4.3, 4.6 | − | 3.5 | 1.7 | 2.8, 2.8 | − | ||
| 6 | 2.1 | − | − | − | 3.3 | − | 5.5, 3.1 | − | − | 3.8, 2.5 | ||
| 14 | − | − | − | − | − | − | − | − | − | − | ||
| Intranasal | 4d | 6.4 | 4.2 | 5.6 | 5.9 | 4.7 | 5.5 | 6.1 | 3.0 | 5.6 | 5.6 | |
| Intranasal | 5d | 7.4 | 4.4 | 4.8 | 5.2 | 5.0 | 6.5 | 6.6 | 3.5 | 5.1 | 5.6 | |
Virus titers are reported as means ± standard deviations (SD) (n = 3) or as individual titers if viruses were not isolated from all three animals.
TBLN, tracheobronchial lymph node.
−, not detected.
Two animals died during the observation period.
The UT3062 virus was more pathogenic than the VN1203 virus in ferrets (two deaths were associated with high-titer replication of the UT3062 virus in multiple organs, including lung) following intranasal inoculation (Table 1) (7). Thus, intranasal and intragastric inoculation revealed a difference in the susceptibilities of ferrets to this virus infection (Table 1). Nevertheless, compared to ferrets infected intranasally, ferrets inoculated via the intragastric route tended to show earlier virus detection in the intestine and mesenteric lymph nodes. On days 3 and 6 p.i., the ingested virus was detected in other organs, including the liver and brain.
Neither UT3062 nor VN1203 showed a strong predilection for growth in the lungs in the ferret model when administered directly into the stomach. Instead, pathological examination of ferrets inoculated with UT3062 directly into the stomach revealed lymph folliculitis in the digestive tract (Fig. 2 a) and mesenteric lymphadenitis as early as day 1 p.i. (Fig. 2b), demonstrating immediate viral infection in these lymphoid tissues. Moreover, infection in the tonsil was also apparent on days 1 and 3 p.i. in ferrets inoculated via the intragastric route (Fig. 2c). Thus, in ferrets, H5N1 viruses can disseminate systemically through lymphatic organs when administered via the digestive route.
Fig. 2.
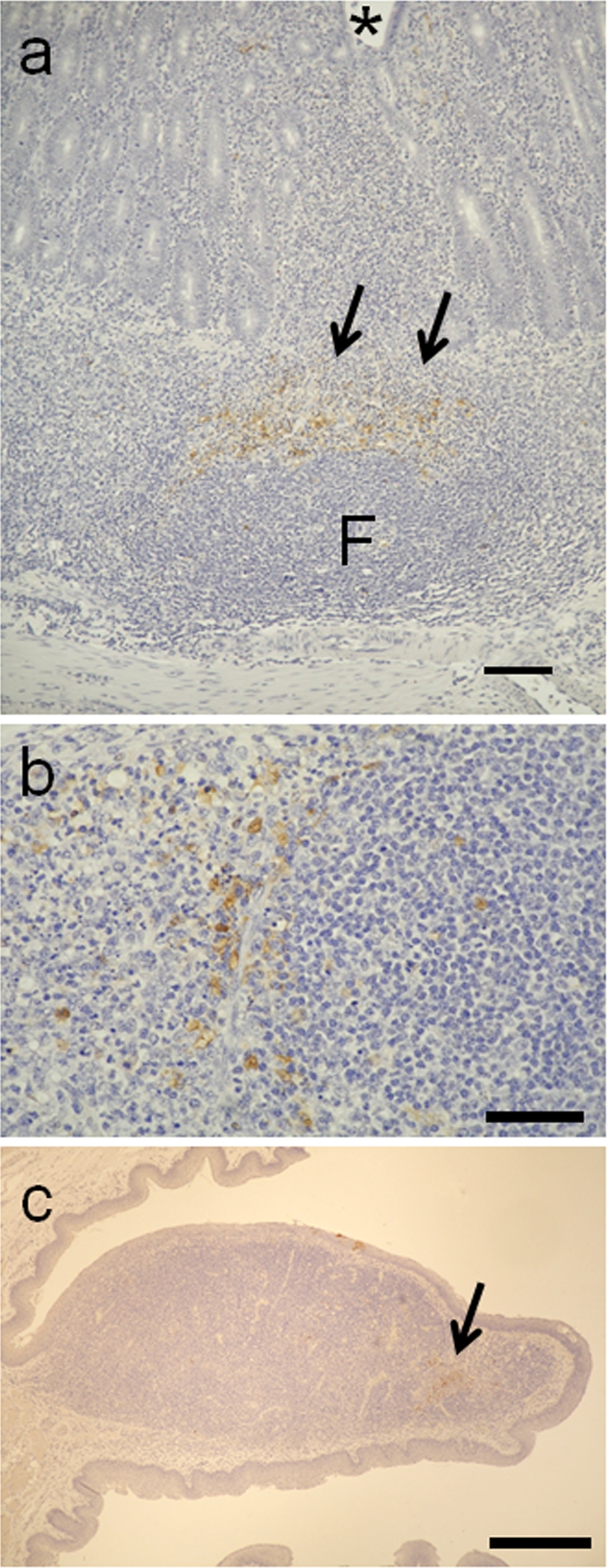
Histopathologic findings in ferrets infected with the UT3062 virus via the digestive route. (a) Folliculitis with viral antigens (arrows) in the intestinal lymph follicles (F; Peyer's patches) in a ferret on day 1 postinfection (p.i.) (bar = 500 μm). Asterisk, lumen of intestine. (b) Mesenteric lymphadenitis with viral antigens (brown pigment) on day 1 p.i. (bar = 50 μm). (c) Viral antigens detected on day 3 p.i. in the tonsilar lesions (brown pigments) of a ferret infected via the intragastric route (bar = 1 mm).
Dissemination of the VN1203 and UT3062 viruses after intragastric inoculation of hamsters.
Hamsters were also used as an animal model because of their ability to support the replication of seasonal human influenza viruses (2, 6, 20) and because the distribution pattern of their receptors is similar to that of humans. Upon intranasal inoculation, the VN1203 virus replicated to high titers in the respiratory organs by day 1 p.i. but could not be isolated from other organs, including the large intestine. By day 3 p.i., virus was recovered from tissues other than respiratory organs, albeit at relatively low levels (Table 2).
Table 2.
Virus titers of hamster tissues infected with H5N1 viruses
| Virus | Inoculation route | Day p.i. | Virus titer(s)a (log10 TCID50/g tissue) in: |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Nasal turbinate | Trachea | Lung | TBLNb | Spleen | Liver | Large intestine | Mesenteric lymph node | Brain | |||
| VN1203 | Intranasal | 1 | 8.0 ± 0.5 | 5.0 ± 1.4 | 5.3 ± 2.7 | 3.6 ± 1.0 | −c | − | − | − | − |
| 3 | 7.1 ± 1.6 | 3.9 ± 1.1 | 5.0 ± 1.5 | 4.8, 3.4 | 3.0 ± 2.1 | 4.8 | 2.8 | 4.8, 2.5 | − | ||
| 6 | 3.4 ± 1.0 | − | − | − | − | − | − | − | − | ||
| 16 | − | − | − | − | − | − | − | − | − | ||
| Intragastric | 1 | − | 2.4 | 2.8 | 4.8 | 5.5 | − | − | 7.3, 2.9 | − | |
| 3 | 5.0 ± 0.9 | − | 2.4, 1.6 | 3.9, 2.2 | − | 2.6 | − | 5.0, 1.4 | 4.8, 3.1 | ||
| 6 | 5.0, 2.9 | 3.4 | 4.3 | − | − | 3.2 | − | − | − | ||
| 16 | − | − | − | − | − | − | − | − | − | ||
| UT3062 | Intranasal | 1 | 6.1 ± 0.1 | 6.2 ± 0.3 | 4.7 ± 2.7 | 4.9 ± 0.1 | 3.4, 2.6 | 2.7 | 1.3 | 2.9 | − |
| 3 | 7.5 ± 1.2 | 6.9 ± 0.3 | 5.1 ± 0.1 | 5.9 ± 0.2 | 6.3 ± 0.7 | 6.5 ± 0.5 | 2.9 ± 0.9 | 6.7 ± 0.5 | 4.2 ± 0.4 | ||
| 4d | 7.5 ± 0.6 | 6.5 ± 0.4 | 6.1 ± 0.1 | 6.3 ± 0.1 | 7.2 ± 1.0 | 7.0 ± 0.3 | 5.5 ± 0.3 | 7.0 ± 0.5 | 4.7 ± 0.5 | ||
| Intragastric | 1 | 1.8, 1.8 | 2.4 | 1.9, 1.6 | 2.0 ± 0.2 | 2.8, 1.7 | 1.4 | − | 4.3, 1.4 | 1.3 | |
| 3 | 5.9 ± 1.5 | 5.2 ± 0.5 | 5.7 ± 1.4 | 5.7 ± 1.3 | 6.6 ± 0.5 | 6.7 ± 1.3 | 4.2 ± 0.8 | 5.7 ± 0.7 | 3.8, 4.1 | ||
| 5d | 6.1 ± 1.2 | 7.0 ± 0.6 | 5.4 ± 0.1 | 6.6 ± 0.6 | 7.0 ± 0.8 | 6.9 ± 0.4 | 4.7 ± 1.2 | 7.1 ± 0.3 | 4.6 ± 0.6 | ||
Virus titers are reported as means ± SD (n = 3) or as individual titers if viruses were not isolated from all three animals.
TBLN, tracheobronchial lymph node.
−, not detected.
None of the animals survived beyond this day p.i.
For intragastric inoculation, a temporary percutaneous gastrostomy procedure was carried out on each hamster as described in Materials and Methods. Lack of virus leakage to areas other than the stomach was demonstrated, as shown in Fig. 3, by the flow of barium following percutaneous injection into the stomach along the digestive tract over time.
Fig. 3.
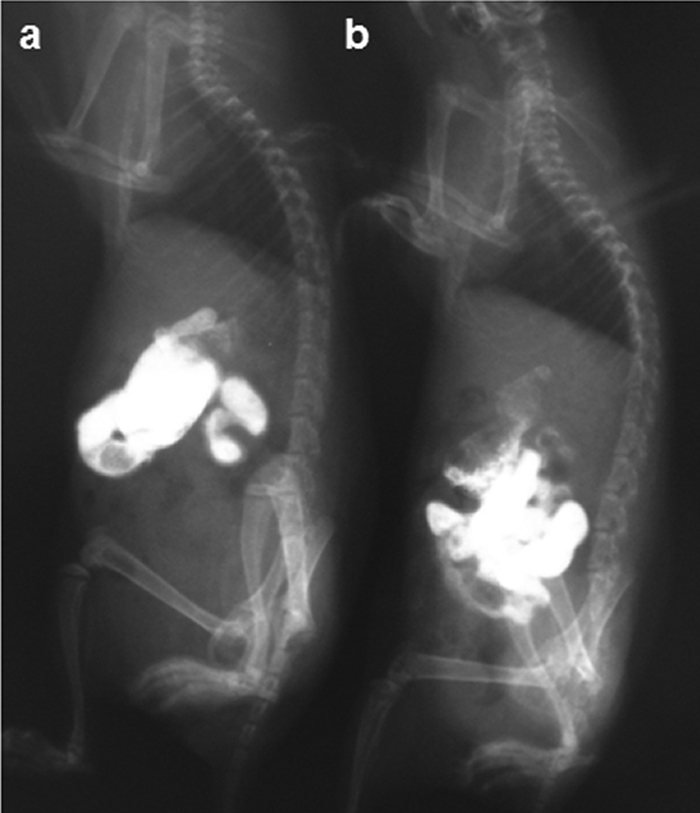
Gastric inoculation of hamsters. We performed temporary percutaneous gastrostomy, as described in the text, and injected barium (0.5 ml/animal) directly into the stomach percutaneously using a 23-guage needle and 1-ml syringe. The injected barium (white) did not leak into the abdominal space, but rather flowed through the digestive tract. (a) Five minutes after gastric inoculation of barium (lateral view). (b) Thirty minutes after gastric administration of barium (lateral view).
In contrast to results for intranasal inoculation, virus was detected in the spleen and mesenteric lymph nodes on day 1 p.i. upon intragastric inoculation. Although the infection efficiency was lower in animals intragastrically infected than in animals intranasally infected, we observed systemic viral dissemination.
In contrast to the VN1203 virus, UT3062 given intranasally infected all tissues except the brain by day 1 p.i. (Table 2), replicating to high titers by days 3 and 4 with lethal results (none of the animals survived to day 5 p.i.). Intragastric infection with UT3062 also resulted in lethal outcomes similar to those that followed intranasal inoculation. Intragastric inoculation of UT3062 led to rapidly lethal systemic infection in all hamsters tested. However, the virus titers in the respiratory organs of animals infected intragastrically were lower, in general, than those in animals infected intranasally (Table 2). We exclude the possibility of fecal-oral infection, as none of the tissues from the contact animals housed with the infected group showed evidence of virus infection.
Regardless of the inoculation route, a prominent gross finding during necropsy of the hamsters killed by the UT3062 virus infection was severe necrosis of lymphoid tissues, including Peyer's patches. However, microscopic findings in the lungs of hamsters infected intragastrically differed markedly from those for animals infected intranasally. In the intranasal group, the lung disease began as bronchopneumonia (Fig. 4 a) or bronchiolitis (Fig. 4a, inset), with inflammation (Fig. 4a, arrows) along the bronchioles (Fig. 4a, asterisks), indicating that the virus had penetrated deep into the lungs along the tracheobronchus. Hamsters inoculated by the intragastric route, however, initially developed interstitial pneumonia (Fig. 4b) and were free of bronchiolar/bronchial infection (Fig. 4b, inset), indicating the absence of virus in the bronchiolar/bronchial epithelial cells. Compared to normal alveolar tissue (Fig. 4c), the alveolar wall was thickened by inflammatory cellular infiltration (Fig. 4b). These results suggest that, in the hamster model, virus introduced intragastrically reaches the lungs via hematogenous dissemination.
Fig. 4.
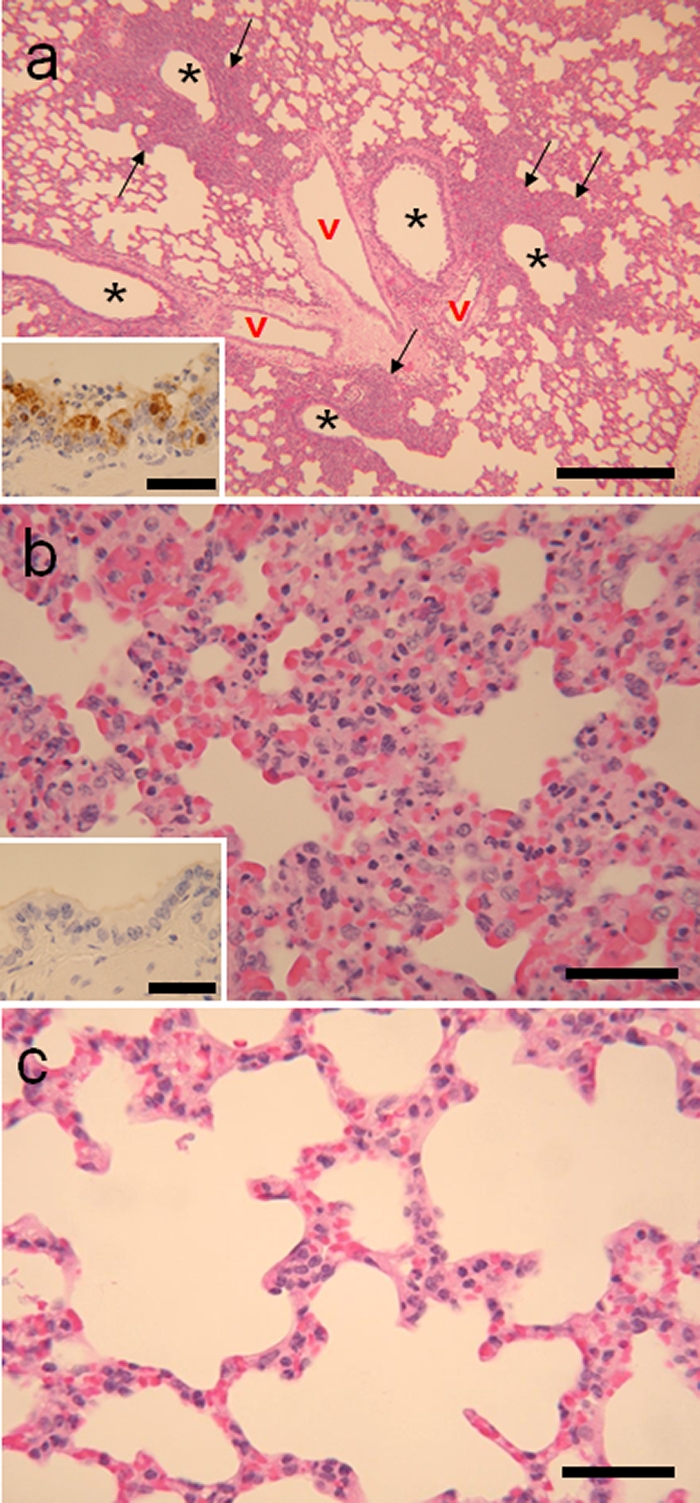
Histopathologic findings in hamsters infected with the UT3062 virus. (a) Lung specimen from an intranasally infected hamster showing bronchopneumonia (bar = 500 μm) with viral antigens (brown pigment) in bronchiolar epithelia at day 1 p.i. (inset bar = 50 μm). Asterisks, lumen of bronchus; v, blood vessels. (b) Lung specimen from hamster infected via the intragastric route showing severe interstitial pneumonia with extensive thickening of the alveolar wall on day 3 p.i. (bar = 50 μm). (Inset) Bronchiolar epithelium showed neither obvious pathological changes nor viral antigens on day 3 p.i. (bar = 50 μm). (c) Lung tissue from a control hamster showing thin alveolar walls and no inflammatory infiltrates (bar = 50 μm).
DISCUSSION
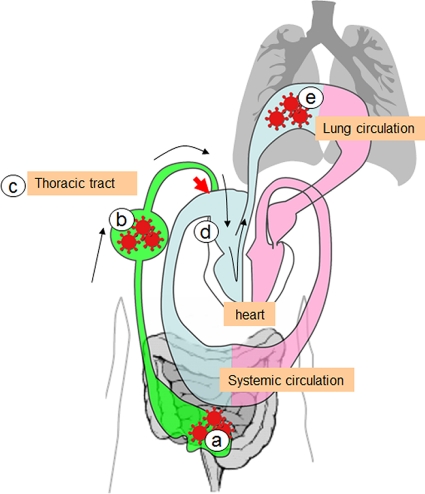
Published reports indicate that highly pathogenic H5N1 virus ingested with raw or undercooked food can establish severe infections in nonhuman mammalian hosts (5, 9, 10, 14, 16, 17). However, the dissemination routes following virus ingestion remain unclear (14). Our ferret model studies revealed that viruses inoculated directly into the stomach can establish infection, even though intragastric viral exposure is less efficient in establishing infection than intranasal viral inoculation. Interestingly, the viruses showed a greater predilection for growth in the tonsil than in the lungs after intragastric infection (Table 1). Further, microscopic examination revealed viral proliferation in the cells of these lymphoid organs (Fig. 2). Since we detected no microscopic damage in the digestive tract other than that to these lymphoid organs, we propose that, in ferrets infected through the digestive tract, H5N1 viruses can access other organs or the systemic circulation via the intestinal lymphatic system. Consistent with these results, viral dissemination through systemic organs was also observed after intragastric viral inoculation in the hamster model, regardless of the different pathogenicities of VN1203 and UT3062 against hamsters. Importantly, the lungs of hamsters infected by the intragastric route, but not the intranasal route, showed interstitial lung lesions without bronchiolar epithelial lesions on microscopic examination (Fig. 4), a result indicative of viral spread to the lungs via the hematogenous route. Thus, H5N1 virus introduced into the digestive tract can enter the bloodstream through the digestive lymphatic system. In fact, lymphocyte migration from the mesenteric lymph nodes to the systemic circulation and organs was previously demonstrated in a pig (13). This concept is also consistent with previous research on surgical shock in which the digestive lymphatic system is shown to be the major route by which factors such as H2O2 and proinflammatory cytokines reach the pulmonary blood circulation (3, 11). We, therefore, propose that, in mammals infected via the digestive tract, H5N1 viruses gain access to the lungs by circulating through the intestinal lymphatic system, as illustrated in Fig. 5. Whether or not viral trafficking via the lymphatic system requires assistance from carrier cells or lipids and protein was not addressed in this study but clearly warrants future investigation.
Fig. 5.
Illustration of how ingested viruses could reach the respiratory organs from the intestine. Pink represents arterial blood flow, blue the venous route, and green the lymphatic route. (a) Ingested food containing infectious virus (red) reaches the intestine. (b) The virus invades the lymph nodes, causing lymphadenitis. (c) Lymph fluid with virus particles flows into the thoracic duct, which connects to the venous route (red arrow). (e) The virus particles enter the venous route and, ultimately, the right side of the heart and the pulmonary circulation. When they reach the lungs, they cause pneumonia.
Our data show that H5N1 viruses inoculated into the stomach can spread to systemic organs through the digestive tract. This route generally does not apply to human infection by seasonal influenza viruses, although avirulent avian influenza virus infections usually initiate in the digestive tracts of waterfowl. Consistent with this difference in preferential replication sites, the neuraminidase of waterfowl-derived influenza A viruses tolerates a low pH environment better than that of human influenza viruses (12). Moreover, we previously showed in a ferret model that viruses isolated from birds replicate in both respiratory and intestinal organs, whereas the growth of viruses isolated from humans is mostly restricted to the respiratory organs (8). Hence, the ability of H5N1 viruses to infect ferrets and hamsters via intestinal exposure is consistent with their tolerance for a low pH environment, such as is found in the mammalian digestive tract (21).
Although H5N1 influenza A viruses can establish infection in the larynx, trachea, and lungs of humans, they grow much more efficiently in the lungs than in either of the other two sites (1). Indeed, severe and often fatal lung infection is a hallmark of highly pathogenic H5N1 viruses and may be present even when there is no evidence of pathological changes or viral antigens in the trachea (18). Our findings provide new insights into the dissemination of ingested H5N1 viruses and suggest that the consumption of contaminated meat or blood could trigger an infection by these viruses in humans.
ACKNOWLEDGMENTS
We thank Susan Watson for scientific editing.
This work was supported by Precursory Research for Embryonic Science and Technology (PRESTO), ERATO, and the Global Center of Excellence (G-COE) for Education and Research on Signal Transduction (Japan Science and Technology Agency); by a grant-in-aid for Specially Promoted Research; by a contract research fund for the Program of Founding Research Centers for Emerging and Reemerging Infectious Diseases from the Ministries of Education, Culture, Sports, Science, and Technology; by grants-in-aid from the Ministry of Health, Labor, and Welfare of Japan; and by National Institute of Allergy and Infectious Disease Public Health Service research grants.
Footnotes
Published ahead of print on 16 March 2011.
REFERENCES
- 1. Abdel-Ghafar A. N., et al. 2008. Update on avian influenza A (H5N1) virus infection in humans. N. Engl. J. Med. 358:261–273 [DOI] [PubMed] [Google Scholar]
- 2. Ali M. J., Teh C. Z., Jennings R., Potter C. W. 1982. Transmissibility of influenza viruses in hamsters. Arch. Virol. 72:187–197 [DOI] [PubMed] [Google Scholar]
- 3. Cavriani G., et al. 2005. Lymphatic system as a path underlying the spread of lung and gut injury after intestinal ischemia/reperfusion in rats. Shock 23:330–336 [DOI] [PubMed] [Google Scholar]
- 4. de Jong M. D., et al. 2006. Fatal outcome of human influenza A (H5N1) is associated with high viral load and hypercytokinemia. Nat. Med. 12:1203–1207 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Enserink M., Kaiser J. 2004. Virology. Avian flu finds new mammal hosts. Science 305:1385. [DOI] [PubMed] [Google Scholar]
- 6. Heath A. W., Maassab H. F., Odagiri T., DeBorde D. C., Potter C. W. 1986. Cold-adapted reassortants of influenza A virus: pathogenicity of A/Ann Arbor/6/60 X A/Alaska/6/77 reassortant viruses in vivo and in vitro. Arch. Virol. 91:53–60 [DOI] [PubMed] [Google Scholar]
- 7. Imai H., et al. 2010. The HA and NS genes of human H5N1 influenza A virus contribute to high virulence in ferrets. PLoS Pathog. 6:e1001106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Kawaoka Y., Bordwell E., Webster R. G. 1987. Intestinal replication of influenza A viruses in two mammalian species. Arch. Virol. 93:303–308 [DOI] [PubMed] [Google Scholar]
- 9. Keawcharoen J., et al. 2004. Avian influenza H5N1 in tigers and leopards. Emerg. Infect. Dis. 10:2189–2191 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Kuiken T., et al. 2004. Avian H5N1 influenza in cats. Science 306:241. [DOI] [PubMed] [Google Scholar]
- 11. Nakamura M., et al. 2004. Hydrogen peroxide derived from intestine through the mesenteric lymph induces lung edema after surgical stress. Shock 21:160–164 [DOI] [PubMed] [Google Scholar]
- 12. Neumann G., Kawaoka Y. 2006. Host range restriction and pathogenicity in the context of influenza pandemic. Emerg. Infect. Dis. 12:881–886 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Pabst R., Trepel F. 1979. Selective labeling of mesenteric lymph nodes: cell production and emigration of newly formed lymphocytes to other organs. Anat. Rec. 195:341–356 [DOI] [PubMed] [Google Scholar]
- 14. Rimmelzwaan G. F., et al. 2006. Influenza A virus (H5N1) infection in cats causes systemic disease with potential novel routes of virus spread within and between hosts. Am. J. Pathol. 168:176–183 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Shinya K., et al. 2006. Avian flu: influenza virus receptors in the human airway. Nature 440:435–436 [DOI] [PubMed] [Google Scholar]
- 16. Songserm T., et al. 2006. Fatal avian influenza A H5N1 in a dog. Emerg. Infect. Dis. 12:1744–1747 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Thanawongnuwech R., et al. 2005. Probable tiger-to-tiger transmission of avian influenza H5N1. Emerg. Infect. Dis. 11:699–701 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Uiprasertkul M., et al. 2005. Influenza A H5N1 replication sites in humans. Emerg. Infect. Dis. 11:1036–1041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. van Riel D., et al. 2006. H5N1 virus attachment to lower respiratory tract. Science 312:399. [DOI] [PubMed] [Google Scholar]
- 20. Wood J. M., et al. 1989. Influenza A (H1N1) vaccine efficacy in animal models is influenced by two amino acid substitutions in the hemagglutinin molecule. Virology 171:214–221 [DOI] [PubMed] [Google Scholar]
- 21. Zhou J. J., et al. 2007. Molecular characterization of the surface glycoprotein genes of an H5N1 influenza virus isolated from a human in Guangdong, China. Arch. Virol. 152:1515–1521 [DOI] [PubMed] [Google Scholar]