Abstract
Like the histidine-to-tyrosine substitution at position 274 in neuraminidase (NA H274Y), an asparagine-to-serine mutation at position 294 in this protein (NA N294S) confers oseltamivir resistance to highly pathogenic H5N1 influenza A viruses. However, unlike viruses with the NA H274Y mutation, the properties of viruses possessing NA N294S are not well understood. Here, we assessed the effect of the NA N294S substitution on the replication and pathogenicity of human H5N1 viruses and on the efficacy of the NA inhibitors oseltamivir and zanamivir in mouse and ferret models. Although NA N294S-possessing H5N1 viruses were attenuated in mice and ferrets compared to their oseltamivir-sensitive counterparts, one of the infected ferrets died from systemic infection, demonstrating the potential lethality in ferrets of oseltamivir-resistant H5N1 viruses with the NA N294S substitution. The efficacy of oseltamivir, but not that of zanamivir, against an NA N294S-possessing virus was substantially impaired both in ferrets and in vitro. These results demonstrate the considerable pathogenicity of NA N294S substitution-possessing H5N1 viruses and underscore the importance of monitoring the emergence of the NA N294S mutation in circulating H5N1 viruses.
INTRODUCTION
Since the first human cases in 1997 in Hong Kong (5, 29, 33), highly pathogenic H5N1 avian influenza A viruses have been circulating among avian species and have spread throughout Asia, Europe, and Africa, with sporadic transmission to humans and high mortality (http://www.who.int/csr/disease/avian_influenza/en/). Since the seasonal influenza vaccine does not elicit effective immunity against H5N1 influenza viruses, we must rely on antiviral drugs to combat these deadly viruses.
Although M2 ion channel blockers (the amino-adamantanes amantadine and rimantadine) and neuraminidase (NA) inhibitors (oseltamivir and zanamivir) are available to treat influenza patients, single amino acid substitutions at several positions in the M2 transmembrane region (1, 14, 25) and NA active site (10–12, 16, 20, 34) confer resistance to viruses against amino-adamantanes and NA inhibitors, respectively. Amino-adamantane-resistant viruses readily emerge under drug selective pressure (15, 27) and are already prevalent among the seasonal influenza viruses (2, 3, 8, 30) and the recently emerged pandemic (H1N1) 2009 viruses (6). Further, circulation of amino-adamantane-resistant H5N1 viruses in Asia was reported in 2006 (4). Accordingly, the World Health Organization recommended that countries stockpile oseltamivir for the treatment and prophylaxis of human H5N1 influenza (26).
We and others, however, isolated oseltamivir-resistant H5N1 viruses from oseltamivir-treated patients (7, 23; http://www.emro.who.int/csr/media/pdf/ai_press_22_01_07.pdf). These resistant viruses possess either a histidine-to-tyrosine substitution at position 274 (N2 numbering; H274Y) or an asparagine-to-serine substitution at position 294 (N294S) in their NAs. Although amino acid substitutions at position 116, 117, 119, 248, or 252 in NA are also thought to reduce the oseltamivir sensitivity of H5N1 viruses (17, 18, 24), the contribution of these substitutions to the clinical manifestations of H5N1 virus infection remains unknown. In contrast, the NA H274Y and N294S substitutions were detected in fatal cases, even though drug treatment was initiated early (i.e., within 48 h of onset of symptoms) (9), suggesting the potential virulence of H5N1 virus variants with these NA mutations for oseltamivir resistance. In fact, A/Vietnam/1203/04 (H5N1)-based recombinant viruses possessing either the NA H274Y or N294S substitution exhibited lethality similar to that of the wild-type virus in a mouse model (19, 22, 32).
However, in ferrets, which are considered the most suitable animal model of human influenza virus pathogenicity, we demonstrated that the replication of an NA H274Y-possessing H5N1 virus isolated from an oseltamivir-treated patient (A/Hanoi/30408/05 clone 9) was attenuated compared to that of its oseltamivir-sensitive counterpart (A/Hanoi/30408/05 clone 7) (23). Here, we assessed the impact of another oseltamivir-resistant mutation, NA N294S, on the pathogenicity of human H5N1 viruses by using mouse and ferret models.
MATERIALS AND METHODS
Viruses and cells.
Highly pathogenic H5N1 influenza virus A/Hanoi/30408/2005 oseltamivir-sensitive clone 7 (HN30408 virus), oseltamivir-resistant clone 3 possessing an asparagine-to-serine substitution at position 294 in the NA protein (HN30408-N294S virus), and oseltamivir-resistant clone 9 possessing a histidine-to-tyrosine substitution at position 274 in the NA protein (HN30408-H274Y virus) were isolated from an oseltamivir-treated influenza patient by using plaque purification in Madin-Darby canine kidney (MDCK) cells, which were maintained in Eagle's minimal essential medium supplemented with 5% newborn calf serum (see reference 23 for details). Wild-type A/Vietnam/1203/04 (H5N1; VN1203 virus) and its two oseltamivir-resistant variants, one possessing the histidine-to-tyrosine substitution at position 274 (VN1203-H274Y virus) and the other possessing the asparagine-to-serine substitution at position 294 (VN1203-N294S virus) in the NA protein, were generated by using reverse genetics (13) as described previously (19, 22) in 293T cells, which were maintained in Dulbecco's modified Eagle's medium supplemented with 10% fetal calf serum. Cells were cultured at 37°C in 5% CO2. All experiments with H5N1 viruses were performed in a biosafety level 3 containment laboratory approved for such use by the Ministry of Agriculture, Forestry, and Fisheries, Japan.
Viral genome sequencing.
Viral RNA was extracted from plaque-purified viruses by use of an RNA extraction kit (QIAamp; Qiagen) according to the manufacturer's instructions and reverse transcribed with SuperScript III reverse transcriptase (Invitrogen) and the A-U12 primer (5′-AGCAAAAGCAGG-3′), which is complementary to the 3′ end of the viral RNA. The resultant cDNA products were used to amplify the hemagglutinin (HA) and NA genes by using a standard PCR method with Pfu-ultra (Stratagene). The purified PCR products were sequenced by using standard DNA sequencing techniques.
Experimental infection of mice.
Six-week-old female BALB/c mice (Japan SLC Inc., Shizuoka, Japan) were anesthetized with sevoflurane and intranasally inoculated with 100, 101, 102, 103, 104, 105, or 106 PFU (50 μl) of virus. Mouse survival was monitored daily for 21 days.
Experimental infection of ferrets.
Three-month-old male ferrets (Marshall BioResources), which were serologically negative for human influenza viruses and H5N1 influenza virus by hemagglutination inhibition assay and which weighed 0.6 to 0.8 kg, were anesthetized with ketamine and xylazine (25 mg and 2 mg per kg of body weight, respectively) and intranasally infected with 2.5 × 105 PFU (250 μl) of virus. Three ferrets per group were administered oseltamivir phosphate (25 mg/kg) orally or zanamivir (5 mg/kg) intranasally twice daily for 5 days beginning at 2 h postinfection (p.i.). Control animals for these drug treatments received distilled water orally and phosphate-buffered saline intranasally, respectively. All infected ferrets were monitored daily for changes in body temperature and weight for 10 days. For virological analysis, nasal washes were collected.
RESULTS AND DISCUSSION
Oseltamivir-resistant H5N1 influenza A virus with the NA N294S substitution.
Previously, we found that a highly pathogenic H5N1 influenza virus, A/Hanoi/30408/2005, which was isolated from a patient treated with oseltamivir, had a mixed NA population (23). Among 10 randomly plaque-picked virus clones, 1 was oseltamivir sensitive (50% inhibitory concentration [IC50] = 0.6 nM), 3 were moderately oseltamivir resistant (IC50s = 7.1 nM to 12.5 nM), and 6 were highly oseltamivir-resistant (IC50 > 763 nM). Both the moderately and highly oseltamivir-resistant viruses possessed serine and tyrosine at positions 294 and 274 instead asparagine and histidine, respectively (23).
Effect of NA N294S substitution on pathogenicity in mice.
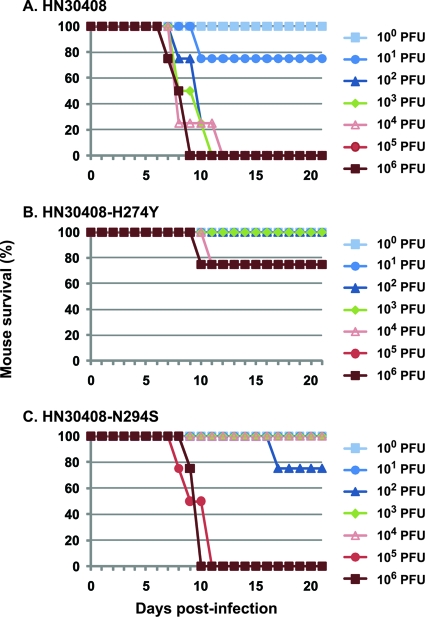
To evaluate the pathogenicity of H5N1 virus possessing the NA N294S substitution in mice, four animals were intranasally infected with NA N294S-possessing HN30408 (HN30408-N294S virus). As controls, we used the oseltamivir-sensitive (HN30408 virus) and the highly resistant (HN30408-H274Y virus) clones of HN30408. The remaining seven genes of these two control viruses were identical to those of HN30408-N294S virus. While HN30408 and HN30408-H274Y viruses showed high and limited lethality in mice, respectively, the lethality of HN30408-N294S virus in this model was moderate (Fig. 1). The 50% mouse lethal doses (MLD50s) of HN30408, HN30408-H274Y, and HN30408-N294S viruses were 20, >106, and 3.2 × 104 PFU, respectively. These results indicate that the NA N294S substitution attenuates the H5N1 virus in mice, although the degree of this attenuation is lower than that caused by the NA H274Y substitution.
Fig. 1.
Pathogenicity of oseltamivir-resistant H5N1 viruses in mice. Four mice per group were intranasally infected with 100, 101, 102, 103, 104, 105, or 106 PFU of HN30408 (A), HN30408-H274Y (B), and HN30408-N294S (C) viruses. Mouse survival was monitored daily for 21 days.
Effect of the NA N294S substitution on pathogenicity and oseltamivir-sensitivity in ferrets.
To evaluate the pathogenicity and oseltamivir sensitivity of H5N1 virus possessing the NA N294S substitution in ferrets, three animals per group were intranasally infected with either HN30408 or HN30408-N294S virus. The infected ferrets were then mock treated or treated with oseltamivir phosphate. Body temperature and weight were monitored daily for 10 days. In addition, nasal washes were collected on days 1, 3, 5, 7, and 9 p.i. to determine virus titer. During these experiments, one of the HN30408 virus-infected, mock-treated ferrets died on day 5 p.i. Viruses were recovered from the various organs of the dead ferrets (Table 1), demonstrating the high virulence of the oseltamivir-sensitive HN30408 virus.
Table 1.
Virus titers in organs of HN30408 virus-infected dead ferretsa
| Organ | Virus titer (log10 PFU/g) of HN30408-infected untreated animals used for: |
|
|---|---|---|
| Oseltamivir experiments | Zanamivir experiments | |
| Brain | 6.0 | 6.3 |
| Lung | 5.1 | 5.6 |
| Heart | 3 | 4.7 |
| Spleen | 3.6 | 2.3 |
| Liver | 5.0 | 5.6 |
| Kidney | <1 | <1 |
| Colon | <1 | <1 |
One each of the HN30408 virus-infected, mock-treated ferrets used for the oseltamivir and zanamivir treatment experiments died on days 5 and 4 postinfection, respectively. Virus recovered from the various organs of these ferrets was titrated by use of plaque assays in MDCK cells.
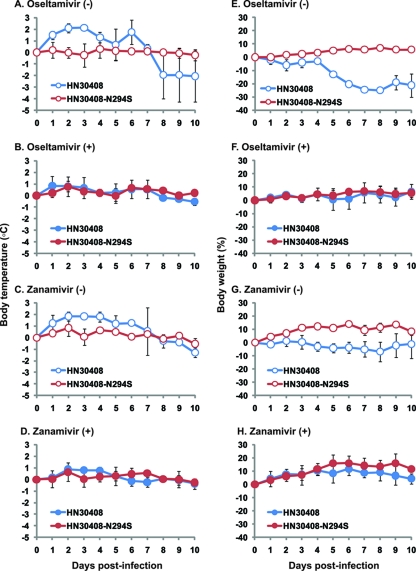
In mock-treated ferrets, the oseltamivir-sensitive HN30408 virus exhibited higher pathogenicity (e.g., substantial increase in body temperature [Fig. 2 A] and severe loss in body weight [Fig. 2E]) than the oseltamivir-resistant HN30408-N294S virus. In nasal washes, higher titers of virus were recovered from the HN30408 virus-infected ferrets than from the HN30408-N294S virus-infected ferrets from days 1 to 7; we found a statistically significant difference in titers on days 1 (P = 0.048, Student's t test), 3 (P = 0.0006), and 5 (P = 0.0048) p.i. (Fig. 3A; compare blue and red open circles). These results indicate that the NA N294S substitution attenuates HN30408 virus in the ferret model.
Fig. 2.
Pathogenicity of oseltamivir-resistant H5N1 virus in ferrets. (A to D) Body temperature of ferrets infected with oseltamivir-resistant H5N1 virus. Three ferrets per group were intranasally infected with 2.5 × 105 PFU of HN30408 or HN30408-N294S virus. Animals were mock treated (A and C) or treated with oseltamivir phosphate (25 mg/kg) orally (B) or zanamivir (5 mg/kg) intranasally (D) twice daily for 5 days beginning at 2 h postinfection. The body temperatures of infected ferrets were monitored daily for 10 days. (E to H) Body weights of ferrets infected with oseltamivir-resistant H5N1 virus. The body weights of ferrets infected with HN30408 or HN30408-N294S virus and mock treated (E and G) or treated with oseltamivir phosphate (F) or zanamivir (H) were monitored daily for 10 days. Error bars indicate standard deviations.
Fig. 3.
Virus titers in nasal washes from ferrets infected with oseltamivir-resistant H5N1 virus. Nasal washes were collected from ferrets infected with HN30408 or HN30408-N294S virus and mock treated or treated with oseltamivir phosphate (A) or zanamivir (B) on days 1, 3, 5, 7, and 9 postinfection and then subjected to plaque assays in MDCK cells. Error bars indicate standard deviations.
When ferrets were treated with oseltamivir, the pathogenicity of both viruses was marginal (Fig. 2B and F). The growth kinetics of HN30408-N294S virus were similar in mock- and oseltamivir-treated ferrets, whereas virus replication in HN30408 virus-infected ferrets was significantly impaired by oseltamivir treatment (Fig. 3A; compare blue and red filled circles). These results indicate that the NA N294S substitution substantially reduces the oseltamivir sensitivity of the H5N1 virus in ferrets.
Effect of NA N294S substitution on zanamivir sensitivity.
The in vitro assay revealed that zanamivir was effective against both HN30408 and HN30408-N294S viruses (19, 23). To assess the efficacy of zanamivir against NA N294S-possessing H5N1 virus in a ferret model, ferrets infected with either HN30408 or HN30408-N294S virus were mock treated or treated with zanamivir and analyzed as described above. Zanamivir treatment lessened the severity of the changes in body temperature (Fig. 2C and D) and weight of the HN30408 virus-infected ferrets (Fig. 2G and H), whereas no substantial differences in body temperature or weight of the HN30408-N294S virus-infected ferrets were observed due to the limited pathogenicity of HN30408-N294S virus (Fig. 2C, D, G, and H). Virological analysis revealed that zanamivir inhibited the replication of both HN30408 and HN30408-N294S viruses (Fig. 3B). These results indicate that the NA N294S substitution does not affect the zanamivir sensitivity of the H5N1 virus in ferrets. One of the HN30408 virus-infected, mock-treated ferrets died on day 4 p.i. due to systemic infection (Table 1), attesting to the high pathogenicity of the oseltamivir-sensitive HN30408 virus in ferrets.
Genetic stability of viruses possessing the NA N294S substitution.
To assess the genetic stability of H5N1 viruses with the NA N294S substitution, the NA gene of viruses isolated from nasal washes of ferrets that were infected with oseltamivir-resistant HN30408-N294S virus and subsequently mock treated or treated with oseltamivir or zanamivir was sequenced. We detected serine at position 294 in the NA of all of the samples tested, attesting to the genetic stability of viruses possessing the NA N294S substitution in ferrets.
Emergence of viruses possessing the NA N294S substitution.
To determine whether H5N1 viruses with the NA N294S mutation arise during replication under selective pressure by NA inhibitors, the NA gene of viruses isolated from nasal washes of ferrets that were infected with oseltamivir-sensitive HN30408 virus and subsequently treated with oseltamivir or zanamivir was sequenced. No NA N294S substitution was detected in any of the test samples. While all of the viruses isolated from zanamivir-treated ferrets possessed an NA gene identical to that of the inoculum, the NA H274Y mutation was detected in viruses (5/5 molecular clones) isolated from one of the three oseltamivir-treated ferrets on day 5 p.i. Further, viruses possessing an NA mutation at position 199 (asparagine to aspartic acid; N199D), which is not known to affect NA inhibitor sensitivity, together with the NA H274Y mutation, were isolated from another oseltamivir-treated ferret (3/5 molecular clones). These results suggest that the NA N294S mutation may be introduced less frequently than the NA H274Y mutation under NA inhibitor selective pressure in ferrets.
Effect of the NA N294S substitution on pathogenicity of different virus strains in ferrets.
To assess the effect of the NA N294S substitution in different genetic backgrounds of human H5N1 virus on pathogenicity in ferrets, we generated wild-type A/Vietnam/1203/04 (H5N1; VN1203 virus) and its two oseltamivir-resistant variants that possess the NA H274Y (VN1203-H274Y virus) and the N294S (VN1203-N294S virus) substitutions, respectively, by using reverse genetics. Three ferrets each were infected with these viruses as described above. One each of the animals infected with VN1203 virus and its oseltamivir-resistant variants died on days 7, 8, and 8 p.i. due to systemic infection (Table 2), indicating the potential lethality to ferrets of oseltamivir-resistant H5N1 virus possessing the NA N294S substitution. Contrary to the results with HN30408 and its oseltamivir-resistant variants (Fig. 2 and 3) (23), we found no statistically significant differences in body temperature (Fig. 4A), weight loss (Fig. 4B), or virus titers in organs (Fig. 4C) among the VN1203, VN1203-H274Y, and VN1203-N294S virus-infected animals, indicating that both VN1203-H274Y and VN1203-N294S viruses are comparable to their parental VN1203 virus in terms of ferret pathogenicity. These results suggest that the impact of the NA H274Y and N294S substitutions on the pathogenicity of human H5N1 viruses varies depending on the virus strain.
Table 2.
Virus titers in organs of VN1203 virus- and VN1203 virus variant-infected dead ferretsa
| Organ | Virus titer (log10 PFU/g) of animals infected with: |
||
|---|---|---|---|
| Wild-type VN1203 | VN1203-H274Y | VN1203-N294S | |
| Brain | 5.7 | 1.7 | 3.7 |
| Lung | 5.6 | 3.1 | 3.8 |
| Spleen | <1.7 | <1.7 | <1.7 |
| Liver | 5.2 | <1.7 | 3.9 |
| Colon | <1.7 | <1.7 | 4.1 |
One each of the wild-type VN1203-, VN1203-H274Y-, and VN1203-N294S virus-infected ferrets died on days 7, 8, and 8 postinfection, respectively. Virus recovered from the various organs of these ferrets was titrated by use of plaque assays in MDCK cells.
Fig. 4.
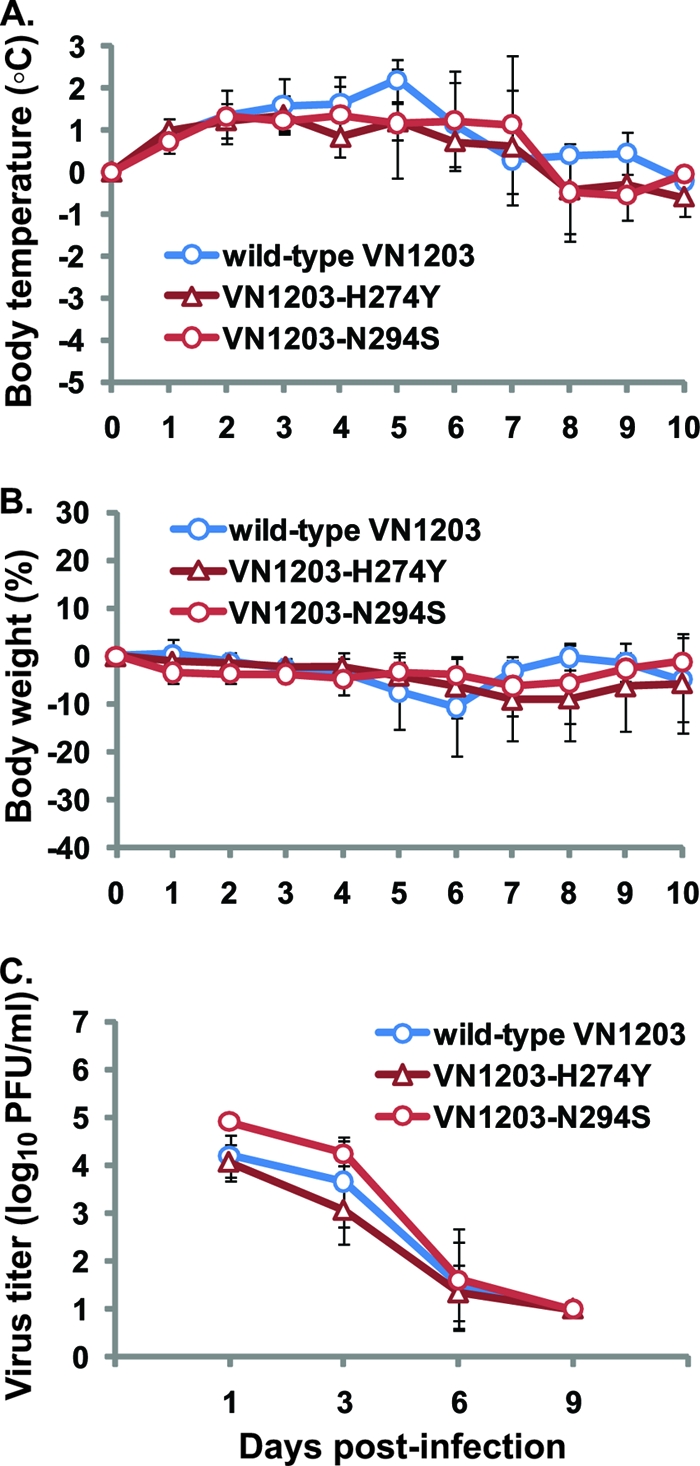
Pathogenicity of oseltamivir-resistant VN1203 viruses in ferrets. Three ferrets per group were intranasally infected with 2.5 × 105 PFU of wild-type VN1203, VN1203-H274Y, or VN1203-N294S virus. The body temperatures (A) and weights (B) of infected ferrets were monitored daily for 10 days. Nasal washes were also collected from infected ferrets on days 1, 3, 6, and 9 postinfection and subjected to plaque assays in MDCK cells (C). Error bars indicate standard deviations.
In this study, we assessed the effect of the NA N294S mutation that was found in viruses in oseltamivir-treated H5N1 influenza patients on the replication and pathogenicity of human H5N1 viruses and on the efficacy of NA inhibitors in mouse and ferret models. In the background of HN30408 virus, the NA N294S mutation substantially impaired the efficacy of oseltamivir (but not zanamivir) in ferrets (Fig. 3) and in vitro (23) and decreased the levels of virus replication and pathogenicity in mice (Fig. 1) and ferrets (Fig. 2A, C, E, and G and 3) compared to those of the oseltamivir-sensitive counterpart. In contrast, consistent with the mouse data (19, 22, 32), the ferret pathogenicity of VN1203 virus was not significantly altered by introducing the NA N294S substitution (Fig. 4). Recently, Ilyushina et al. reported that the NA N294S substitution conferred a moderate level of oseltamivir resistance and increased virus virulence in ferrets by using an A/Turkey/15/06 (H5N1)-based recombinant mutant possessing the NA N294S mutation (18). These results suggest that the effect of the NA N294S substitution on the oseltamivir sensitivity, replication, and ferret pathogenicity of human H5N1 viruses differs depending on the virus strain. Importantly, VN1203 virus possessing the NA N294S substitution was a potential killer of ferrets (Table 2), underscoring the importance of monitoring the emergence of the NA N294S substitution in circulating H5N1 viruses.
At present, several NA inhibitors are available, such as laninamivir and peramivir. Laninamivir, also known as CS-8958, is effective against oseltamivir-resistant viruses (19, 21, 31), although, like zanamivir, this inhaled drug is not appropriate for severely ill or infant patients. In contrast, peramivir is an intravenous NA inhibitor that can be given to patients who cannot be treated with inhaled drugs (28); however, some oseltamivir-resistant viruses are cross-resistant to peramivir (12). To minimize the likelihood of emergence of NA inhibitor-resistant viruses and effectively treat patients infected with such viruses, we should consider stockpiling a variety of NA inhibitors.
ACKNOWLEDGMENTS
We thank Susan Watson for editing the manuscript.
This work was supported by ERATO (Japan Science and Technology Agency), by a grant-in-aid for Specially Promoted Research from the Ministries of Education, Culture, Sports, Science, and Technology, by grants-in-aid from Health, Labor, and Welfare of Japan, by a Contract Research Fund for the Program of Founding Research Centers for Emerging and Reemerging Infectious Diseases, and by National Institute of Allergy and Infectious Diseases Public Health Service research grants.
Footnotes
Published ahead of print on 2 March 2011.
REFERENCES
- 1. Belshe R. B., Smith M. H., Hall C. B., Betts R., Hay A. J. 1988. Genetic basis of resistance to rimantadine emerging during treatment of influenza virus infection. J. Virol. 62:1508–1512 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Bright R. A., et al. 2005. Incidence of adamantane resistance among influenza A (H3N2) viruses isolated worldwide from 1994 to 2005: a cause for concern. Lancet 366:1175–1181 [DOI] [PubMed] [Google Scholar]
- 3. Bright R. A., Shay D. K., Shu B., Cox N. J., Klimov A. I. 2006. Adamantane resistance among influenza A viruses isolated early during the 2005-2006 influenza season in the United States. JAMA 295:891–894 [DOI] [PubMed] [Google Scholar]
- 4. Cheung C. L., et al. 2006. Distribution of amantadine-resistant H5N1 avian influenza variants in Asia. J. Infect. Dis. 193:1626–1629 [DOI] [PubMed] [Google Scholar]
- 5. Claas E. C., et al. 1998. Human influenza A H5N1 virus related to a highly pathogenic avian influenza virus. Lancet 351:472–477 [DOI] [PubMed] [Google Scholar]
- 6. Dawood F. S., et al. 2009. Emergence of a novel swine-origin influenza A (H1N1) virus in humans. N. Engl. J. Med. 360:2605–2615 [DOI] [PubMed] [Google Scholar]
- 7. de Jong M. D., et al. 2005. Oseltamivir resistance during treatment of influenza A (H5N1) infection. N. Engl. J. Med. 353:2667–2672 [DOI] [PubMed] [Google Scholar]
- 8. Deyde V. M., et al. 2007. Surveillance of resistance to adamantanes among influenza A(H3N2) and A(H1N1) viruses isolated worldwide. J. Infect. Dis. 196:249–257 [DOI] [PubMed] [Google Scholar]
- 9. Earhart K. C., et al. 2009. Oseltamivir resistance mutation N294S in human influenza A(H5N1) virus in Egypt. J. Infect. Public Health 2:74–80 [DOI] [PubMed] [Google Scholar]
- 10. Gubareva L. V., Kaiser L., Hayden F. G. 2000. Influenza virus neuraminidase inhibitors. Lancet 355:827–835 [DOI] [PubMed] [Google Scholar]
- 11. Gubareva L. V., Matrosovich M. N., Brenner M. K., Bethell R. C., Webster R. G. 1998. Evidence for zanamivir resistance in an immunocompromised child infected with influenza B virus. J. Infect. Dis. 178:1257–1262 [DOI] [PubMed] [Google Scholar]
- 12. Gubareva L. V., Webster R. G., Hayden F. G. 2001. Comparison of the activities of zanamivir, oseltamivir, and RWJ-270201 against clinical isolates of influenza virus and neuraminidase inhibitor-resistant variants. Antimicrob. Agents Chemother. 45:3403–3408 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Hatta M., et al. 2007. Growth of H5N1 influenza A viruses in the upper respiratory tracts of mice. PLoS Pathog. 3:1374–1379 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Hay A. J., Zambon M. C., Wolstenholme A. J., Skehel J. J., Smith M. H. 1986. Molecular basis of resistance of influenza A viruses to amantadine. J. Antimicrob. Chemother. 18(Suppl. B):19–29 [DOI] [PubMed] [Google Scholar]
- 15. Hayden F. G. 2001. Perspectives on antiviral use during pandemic influenza. Philos. Trans. R. Soc. Lond. B Biol. Sci. 356:1877–1884 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Hurt A. C., Holien J. K., Parker M., Kelso A., Barr I. G. 2009. Zanamivir-resistant influenza viruses with a novel neuraminidase mutation. J. Virol. 83:10366–10373 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Hurt A. C., et al. 2007. Susceptibility of highly pathogenic A(H5N1) avian influenza viruses to the neuraminidase inhibitors and adamantanes. Antiviral Res. 73:228–231 [DOI] [PubMed] [Google Scholar]
- 18. Ilyushina N. A., Seiler J. P., Rehg J. E., Webster R. G., Govorkova E. A. 2010. Effect of neuraminidase inhibitor-resistant mutations on pathogenicity of clade 2.2 A/Turkey/15/06 (H5N1) influenza virus in ferrets. PLoS Pathog. 6:e1000933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Kiso M., et al. 2010. Efficacy of the new neuraminidase inhibitor CS-8958 against H5N1 influenza viruses. PLoS Pathog. 6:e1000786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Kiso M., et al. 2004. Resistant influenza A viruses in children treated with oseltamivir: descriptive study. Lancet 364:759–765 [DOI] [PubMed] [Google Scholar]
- 21. Kiso M., et al. 2010. Characterization of oseltamivir-resistant 2009 H1N1 pandemic influenza A viruses. PLoS Pathog. 6:e1001079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Kiso M., et al. 2010. T-705 (favipiravir) activity against lethal H5N1 influenza A viruses. Proc. Natl. Acad. Sci. U. S. A. 107:882–887 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Le Q. M., et al. 2005. Avian flu: isolation of drug-resistant H5N1 virus. Nature 437:1108. [DOI] [PubMed] [Google Scholar]
- 24. Rameix-Welti M. A., et al. 2006. Natural variation can significantly alter the sensitivity of influenza A (H5N1) viruses to oseltamivir. Antimicrob. Agents Chemother. 50:3809–3815 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Schnell J. R., Chou J. J. 2008. Structure and mechanism of the M2 proton channel of influenza A virus. Nature 451:591–595 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Schunemann H. J., et al. 2007. WHO rapid advice guidelines for pharmacological management of sporadic human infection with avian influenza A (H5N1) virus. Lancet Infect. Dis. 7:21–31 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Shiraishi K., et al. 2003. High frequency of resistant viruses harboring different mutations in amantadine-treated children with influenza. J. Infect. Dis. 188:57–61 [DOI] [PubMed] [Google Scholar]
- 28. Sidwell R. W., Smee D. F. 2002. Peramivir (BCX-1812, RWJ-270201): potential new therapy for influenza. Expert Opin. Invest. Drugs 11:859–869 [DOI] [PubMed] [Google Scholar]
- 29. Subbarao K., et al. 1998. Characterization of an avian influenza A (H5N1) virus isolated from a child with a fatal respiratory illness. Science 279:393–396 [DOI] [PubMed] [Google Scholar]
- 30. Weinstock D. M., Zuccotti G. 2006. Adamantane resistance in influenza A. JAMA 295:934–936 [DOI] [PubMed] [Google Scholar]
- 31. Yamashita M., et al. 2009. CS-8958, a prodrug of the new neuraminidase inhibitor R-125489, shows long-acting anti-influenza virus activity. Antimicrob. Agents Chemother. 53:186–192 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Yen H. L., et al. 2007. Neuraminidase inhibitor-resistant recombinant A/Vietnam/1203/04 (H5N1) influenza viruses retain their replication efficiency and pathogenicity in vitro and in vivo. J. Virol. 81:12418–12426 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Yuen K. Y., et al. 1998. Clinical features and rapid viral diagnosis of human disease associated with avian influenza A H5N1 virus. Lancet 351:467–471 [DOI] [PubMed] [Google Scholar]
- 34. Zambon M., Hayden F. G. 2001. Position statement: global neuraminidase inhibitor susceptibility network. Antiviral Res. 49:147–156 [DOI] [PubMed] [Google Scholar]