Abstract
We identified a novel human polyomavirus from a kidney transplant patient under immunosuppressive treatment, by use of a generic PCR. The genome of the virus was completely amplified and sequenced. In phylogenetic analyses, it appeared as the closest relative to the African green monkey-derived lymphotropic polyomavirus (LPV). Further investigation of clinical samples from immunocompromised patients with specific nested PCR revealed additional positive samples, indicating that the virus naturally infects humans. The virus was tentatively named human polyomavirus 9 (HPyV9). The previously observed seroreactivity to LPV in human populations might find a partial explanation in the circulation of HPyV9.
Humans are known to be infected with a minimum of eight distinct polyomaviruses (PyVs): BK PyV (BKV) (7), JC PyV (JCV) (13), KI PyV (KIV) (1), WU PyV (WUV) (8), Merkel cell PyV (MCPyV) (5), HPyV6 and HPyV7 (14), and trichodysplasia spinulosa-associated PyV (TSV) (16). These members of the Polyomaviridae family are small DNA viruses which generally infect individuals in a persistent manner (from their early childhood on) but asymptomatically. However, PyV reactivation has been associated with pathological conditions in immunocompromised individuals; JCV has been associated with progressive multifocal leukoencephalopathy (LEP), BKV has been associated with nephropathy and cystitis (both reviewed in reference 11), MCPyV has been associated with Merkel cell carcinoma (MCC), a rare but aggressive human tumor of the skin (5), and TSV has been associated with the eponymous pathology (16). Given the growing disease burden entailed by acquired immunodeficiencies (mostly medically induced in industrialized countries, as well as a side effect of the spread of HIV-1 infections), human PyVs are now increasingly considered emerging opportunistic pathogens. Gaining more insight into their diversity, prevalence, and etiopathogenesis is therefore essential.
Given the accelerated rate of human PyV discovery over the last few years, it appears very likely that further, still-unknown PyVs are actually circulating in human populations. In support of this notion, seroepidemiological studies have revealed that up to 30% of human sera had strong reactions to antigens derived from a PyV initially identified in African green monkeys (Chlorocebus aethiops), the lymphotropic polyomavirus (LPV, or African green monkey PyV [AGMPyV]) (3, 9, 15, 17, 18), a fact which could not be explained by cross-reactivity to already known human PyVs (17). In addition, we recently identified more than 20 novel PyVs in a number of nonhuman primates (NHP), including apes (12; N. Scuda, F. Leendertz, and B. Ehlers, unpublished data). These new PyVs span nearly the entire known diversity of mammalian PyVs, which suggests that primates as a whole, including humans, are infected with a plethora of PyVs.
To further test this hypothesis, we screened DNA extracts from 597 clinical samples for the presence of PyVs. The majority of the samples were from immunocompromised transplant recipients, LEP patients, and HIV-positive patients (serum, plasma, urine, or whole blood) and originally had been collected for BKV and herpesvirus diagnostics at three German university hospitals (Table 1). In addition, cerebrospinal fluid (CSF) samples from LEP patients, bronchoalveolar lavage (BAL) fluid from patients with pneumonia, and fecal samples from children with diarrhea were tested (Table 1). A generic PCR assay using degenerate and deoxyinosine-substituted primers was used as described previously (12). The primers had been designed to target conserved regions in the VP1 genes of the known PyVs (except the highly divergent PyV group represented by KIV, WUV, HPyV6, and HPyV7). From 84/597 samples, VP1 sequences could be determined which unambiguously pointed at known human PyVs, as shown by sequencing and BLAST analysis (2) of GenBank (BKV [n = 56], JCV [n = 18], MCPyV [n = 8], and TSV [n = 2]) (Table 1). These PyV sequences were amplified from plasma (12/176), urine (71/179), and BAL fluid (1/21) samples. CSF (n = 74), whole blood (n = 21), serum (n = 87), and fecal (n = 38) samples remained negative (Table 1).
Table 1.
Analysis of selected human samples for polyomaviruses and HPyV9 with PCR
| Sample type | Source(s) | No. of samples tested | PyV detected (no. of samples) by generic PCRc | No. of samples HPyV9 positive by specific PCRc | HPyV9 genome amplified |
|---|---|---|---|---|---|
| Plasma | Kidney transplant recipientsa | 76 | BKV (5), MCPyV (1) | 1 | + |
| Patients with HIVb | 50 | MCPyV (1) | — | ||
| Immunocompromised adultsd | 25 | BKV (3) | — | ||
| Immunocompromised pediatric patientsd | 25 | BKV (2) | — | ||
| Serum | Patients with leukoencephalopathye | 47 | — | 1 | — |
| Kidney transplant recipientsa | 41 | HPyV9 (1) | 1 | + | |
| Urine | Kidney transplant recipientsa,f | 38 | BKV (6), MCPyV (1) | 1g | − |
| Immunocompromised patients with cancera | 26 | BKV (6), JCV (4), TSV (1) | — | ||
| Stem cell transplant recipientsa | 14 | BKV (6) | — | ||
| Patients with multiple sclerosish | 9 | JCV (2) | — | ||
| Othera | 92 | BKV (28), JCV (12), MCPyV (4), TSV (1) | — | ||
| Whole blood | Transplant recipientse | 20 | — | — | |
| Acute myeloid leukemia patient | 1 | — | 1 | — | |
| Bronchoalveolar lavage fluid | Patients with pneumoniae | 21 | MCPyV (1) | — | |
| Feces | Pediatric patients with gastroenteritis | 38 | — | — | |
| Cerebrospinal fluid | Patients with leukoencephalopathyi | 36 | — | — | |
| Othere | 38 | — | — |
Samples collected for BKV infection diagnosis.
Plasma with active cytomegalovirus infection.
—, PCR negative.
Samples collected for cytomegalovirus infection diagnosis.
Samples collected for herpesvirus infection diagnosis.
25 to 100 μl eluate from 10 to 30 ml urine (n = 27) or from 0.2 ml urine (n = 11).
From a patient with a double infection (MCPyV plus HPyV9).
From patients under natalizumab (Tysabri) therapy.
Samples collected for JCV infection diagnosis.
Most importantly, an unknown PyV sequence was amplified from the serum of a kidney transplant patient under immunosuppressive treatment. In a BLAST analysis, it revealed the closest similarity to the VP1 gene of LPV (pairwise nucleic acid identity, 83%). To obtain additional sequence information for the novel PyV, a 950-bp genome fragment spanning parts of the VP3 and VP1 genes was amplified. For this purpose, two degenerate sense primers derived from the VP3 sequence of LPV and two specific antisense primers deduced from the novel VP1 sequence were used in a nested PCR. Based on the resulting sequence, primers were designed tail to tail for the amplification and sequencing of the remaining part of the genome and used in nested long-distance PCR (LD-PCR) (all primer sequences and PCR conditions are shown in Tables S1 and S2 in the supplemental material). A final circular genome of 5,026 bp was obtained and confirmed to be more similar to the LPV genome (pairwise nucleic acid identity, 76%) than to those of other PyVs (<60%). Since eight human PyVs are presently known, the virus from which the genome originated was tentatively named human polyomavirus 9 (HPyV9).
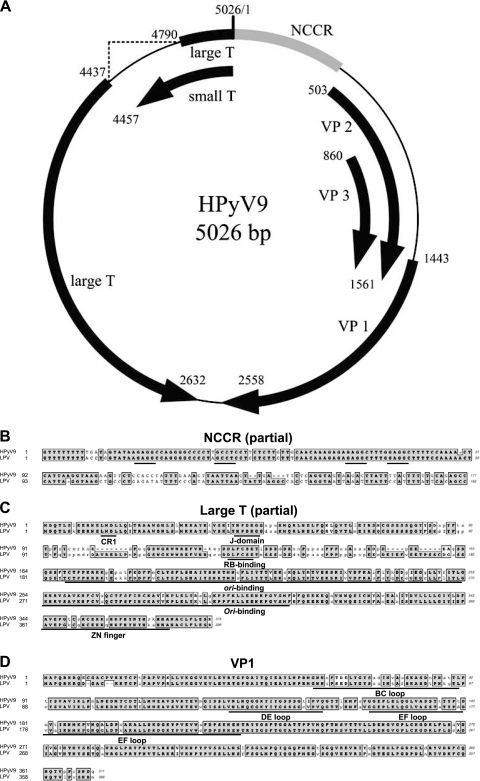
Examination of putative open reading frames (ORFs) showed that the genome of HPyV9 had a typical PyV structure, with an early region encoding regulatory proteins (small T and large T antigens) and a late region coding for structural proteins (VP1, VP2, and VP3), separated by a noncoding control region (NCCR) (Fig. 1A). HPyV9 lacked any ORF encoding an agnoprotein. The ORF locations on the viral genome and their similarities to LPV and other human PyVs are listed in Table S3 in the supplemental material. Over the entire genome length, HPyV9 and LPV had a high similarity (see Fig. S4 in the supplemental material), and the similar regions included functionally important sites in the NCCR and sequences encoding functionally important sites in the large T and VP1 proteins (Fig. 1B to D, respectively).
Fig. 1.
Genome map of HPyV9 and comparison of encoded proteins with those of LPV. (A) Genome organization of HPyV9. Putative coding regions for VP1 to VP3, small T antigen, and large T antigen are marked by arrows. (B) Part of the noncoding control region (NCCR) of HPyV9 was aligned with that of LPV using ClustalW (as implemented in MacVector 10.6). Conserved regions are outlined and shaded. T antigen binding elements (GAGGC or the complement GCCTC) are underlined. (C) Comparison of HPyV9 and LPV large T proteins. The CR1, J, RB-binding, ori-binding, and Zn finger domains are underlined. (D) Comparison of VP1 proteins. VP1 loops are underlined. For panels C and D, identical amino acids (in bold type) are outlined and shaded, similarities (in bold type) are outlined only, and mismatches are in normal, lowercase type.
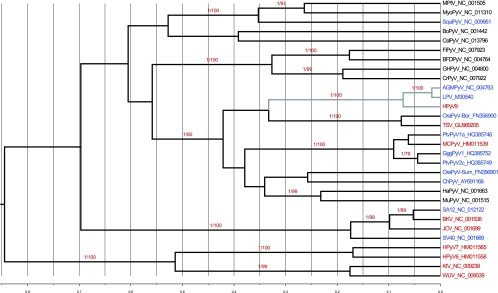
Phylogenetic analyses were performed using a concatenated data set of VP1, VP2, and large T sequences, including those of HPyV9 as well as a representative collection of published PyVs (see Table S5 in the supplemental material). Preparation of the data set and downstream analyses, including maximum likelihood (ML) and Bayesian tree reconstructions, was conducted as described previously (12). The resulting tree evidenced the close relationship of HPyV9 and LPV, which formed a highly supported monophyletic group (bootstrap [Bp] and posterior probability [pp] values were 100 and 1, respectively) (Fig. 2).
Fig. 2.
Bayesian chronogram deduced from the analysis of a 687-amino-acid alignment of concatenated VP1, VP2, and large T antigen sequences. PyVs identified from human hosts are in red and those from nonhuman primates are in blue. The clade formed by HPyV9 and LPV is highlighted with a gray line. Statistical support for a branch is given where the Bp value is ≥70 and the pp value is ≥0.95. Bp values are shown after the slash, and pp values are shown before the slash (pp/Bp). The scale axis is in amino acid substitutions per site. This chronogram was rooted by using a relaxed clock. A maximum likelihood analysis of the same data set concluded to a similar topology and is thus not shown here. For the full virus names represented here by abbreviations, see Table S5 in the supplemental material.
To determine whether individuals other than the index case were infected with HPyV9, all 597 samples were rescreened with an HPyV9-specific nested PCR using primers deduced from the VP1 sequence (see Tables S1 and S2 in the supplemental material). In four additional samples (serum, plasma, whole blood, and urine), VP1 sequences from HPyV9 were detected (100% nucleic acid sequence identity to the index VP1 sequence). All CSF and BAL fluid samples were negative (Table 1). In attempting to amplify complete genomes sequences from these samples, we preamplified PyV genomes by using the Templiphi 100 rolling circle amplification kit according to the instructions of the manufacturer (GE Healthcare, Germany) prior to performing the VP3/VP1 PCR and the LD-PCR. By this approach, another complete HPyV9 genome could be amplified (from the plasma sample of a renal transplant patient; data not shown). It revealed 100% nucleic acid identity to the index genome. These findings qualify HPyV9 as a human virus, although one with a low prevalence in the selected samples (as revealed by DNA-based assays). Further studies are required in order to identify the sites of HPyV9 replication and persistence as well as to determine HPyV9 pathogenicity in immunocompetent and immunocompromised individuals.
Notably, HPyV9 exhibited very close sequence relatedness to LPV, a fact that deserves closer attention. Seroepidemiological studies have indeed revealed that up to 30% of adult human sera contain antibodies against LPV (3, 9, 15). Viscidi et al. studied the serological cross-reactivity between BKV, JCV, simian virus 40 (SV40), and LPV capsids by using enzyme immunoassays (EIAs) based on virus-like particles. Their data indicated that LPV-reactive antibodies found in human sera could not be attributed to cross-reacting anti-BKV or anti-JCV antibodies (17). Based on competition assays, Kean et al. could exclude serological cross-reactivity between VP1 proteins of LPV and MCPyV (9). Taken together, these results pointed at LPV having a serologically related human counterpart.
Capsid protein VP1 is the major structural component of polyomavirus particles. It contains antigenic determinants and is involved in the interaction of PyVs with host cells through its outfacing loops. Therefore, the similarity between the HPyV9 and LPV VP1 proteins, even in the highly variable loop regions (Fig. 1D), is remarkable, and serological cross-reactivity appears a reasonable possibility. This hypothesis is supported by the observation of cross-reactivity between VP1 capsomers of JCV/BKV and SV40 (9), despite the fact that SV40 VP1 is more distantly related to the JCV/BKV VP1 (pairwise amino acid sequence identities, 75% and 81%, respectively) than HPyV9 is to LPV (87%). Against this line of argumentation stand two observations. First, WUV and KIV VP1 capsomers show no evidence of cross-reactivity, while their VP1 amino acid sequences are approximately as distant from each other as those of JCV/BKV are from that of SV40 (9). Then, it was also shown that antibodies raised against a given strain of BKV could occasionally discriminate subgroups in neutralization assays (10), while the maximum VP1 genetic distance within BKV is largely outscored by the genetic distance between LPV/AGMPyV VP1 and HPyV9 VP1 (see Fig. S6 in the supplemental material). All in all, these contrasted results prevent any firm prediction of cross-reactivity that would be solely based on genetic make-up. However, we propose that HPyV9 could at least be considered one good candidate for the frequent LPV-like serological reactivity observed in human populations while acknowledging that other PyVs might be involved as well. Another good candidate PyV could be LPV itself, as short DNA fragments of LPV were recently detected in CSF and blood of AIDS patients as well as in blood of healthy subjects (4). Other authors analyzed patients suffering from progressive multifocal leukoencephalopathy and did not detect LPV while using specific primers (6). Our data do not provide evidence of LPV infection in immunocompromised patients, either. If the prevalences of both HPyV9 and LPV infections in human populations can be confirmed to be at low levels, the existence of other antigenically related yet unknown human PyVs must be postulated. Further investigation of this question, notably involving differential serological testing of HPyV9 and LPV, should clarify this issue.
Nucleotide sequence accession number.
The genome sequence of HPyV9 was deposited in GenBank under accession number HQ696595.
Supplementary Material
Acknowledgments
We are grateful for the excellent technical assistance from Sonja Liebmann, Cornelia Walter, and Nezlisah Yasmum as well as for helpful discussions with Fabian H. Leendertz. The supply of clinical samples by Marina Höhne, Sebastian Voigt, Ioannis Anagnostopoulos, Ulrike Blume-Peytavi, and Mona Embarek is kindly acknowledged.
Footnotes
Supplemental material for this article may be found at http://jvi.asm.org/.
Published ahead of print on 9 February 2011.
REFERENCES
- 1. Allander T., et al. 2007. Identification of a third human polyomavirus. J. Virol. 81:4130–4136 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Altschul S. F., Gish W., Miller W., Myers E. W., Lipman D. J. 1990. Basic local alignment search tool. J. Mol. Biol. 215:403–410 [DOI] [PubMed] [Google Scholar]
- 3. Brade L., Mueller-Lantzsch N., zur Hausen H. 1981. B-lymphotropic papovavirus and possibility of infections in humans. J. Med. Virol. 6:301–308 [DOI] [PubMed] [Google Scholar]
- 4. Delbue S., et al. 2008. First identification and molecular characterization of lymphotropic polyomavirus in peripheral blood from patients with leukoencephalopathies. J. Clin. Microbiol. 46:2461–2462 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Feng H., Shuda M., Chang Y., Moore P. S. 2008. Clonal integration of a polyomavirus in human Merkel cell carcinoma. Science 319:1096–1100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Focosi D., et al. 2009. Polyomaviruses other than JCV are not detected in progressive multifocal leukoencephalopathy. J. Clin. Virol. 45:161–162 [DOI] [PubMed] [Google Scholar]
- 7. Gardner S. D., Field A. M., Coleman D. V., Hulme B. 1971. New human papovavirus (B.K.) isolated from urine after renal transplantation. Lancet i:1253–1257 [DOI] [PubMed] [Google Scholar]
- 8. Gaynor A. M., et al. 2007. Identification of a novel polyomavirus from patients with acute respiratory tract infections. PLoS Pathog. 3:e64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Kean J. M., Rao S., Wang M., Garcea R. L. 2009. Seroepidemiology of human polyomaviruses. PLoS Pathog. 5:e1000363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Knowles W. A., Gibson P. E., Gardner S. D. 1989. Serological typing scheme for BK-like isolates of human polyomavirus. J. Med. Virol. 28:118–123 [DOI] [PubMed] [Google Scholar]
- 11. Krumbholz A., Bininda-Emonds O. R., Wutzler P., Zell R. 2009. Phylogenetics, evolution, and medical importance of polyomaviruses. Infect. Genet. Evol. 9:784–799 [DOI] [PubMed] [Google Scholar]
- 12. Leendertz F. H., et al. 2011. African great apes are naturally infected with polyomaviruses closely related to Merkel cell polyomavirus. J. Virol. 85:916–924 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Padgett B. L., Walker D. L., ZuRhein G. M., Eckroade R. J., Dessel B. H. 1971. Cultivation of papova-like virus from human brain with progressive multifocal leucoencephalopathy. Lancet i:1257–1260 [DOI] [PubMed] [Google Scholar]
- 14. Schowalter R. M., Pastrana D. V., Pumphrey K. A., Moyer A. L., Buck C. B. 2010. Merkel cell polyomavirus and two previously unknown polyomaviruses are chronically shed from human skin. Cell Host Microbe 7:509–515 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Takemoto K. K., Segawa K. 1983. A new monkey lymphotropic papovavirus: characterization of the virus and evidence of a related virus in humans. Prog. Clin. Biol. Res. 105:87–96 [PubMed] [Google Scholar]
- 16. van der Meijden E., et al. 2010. Discovery of a new human polyomavirus associated with trichodysplasia spinulosa in an immunocompromized patient. PLoS Pathog. 6:e1001024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Viscidi R. P., Clayman B. 2006. Serological cross reactivity between polyomavirus capsids. Adv. Exp. Med. Biol. 577:73–84 [DOI] [PubMed] [Google Scholar]
- 18. zur Hausen H., Gissmann L. 1979. Lymphotropic papovaviruses isolated from African green monkey and human cells. Med. Microbiol. Immunol. 167:137–153 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.