Abstract
Mumps virus (MuV) is highly neurotropic and was the leading cause of aseptic meningitis in the Western Hemisphere prior to widespread use of live attenuated MuV vaccines. Due to the absence of markers of virus neuroattenuation and neurovirulence, ensuring mumps vaccine safety has proven problematic, as demonstrated by the occurrence of aseptic meningitis in recipients of certain vaccine strains. Here we examined the genetic basis of MuV neuroattenuation and neurovirulence by generating a series of recombinant viruses consisting of combinations of genes derived from a cDNA clone of the neurovirulent wild-type 88-1961 strain (r88) and from a cDNA clone of the highly attenuated Jeryl Lynn vaccine strain (rJL). Testing of these viruses in rats demonstrated the ability of several individual rJL genes and gene combinations to significantly neuroattenuate r88, with the greatest effect imparted by the rJL nucleoprotein/matrix protein combination. Interestingly, no tested combination of r88 genes, including the nucleoprotein/matrix protein combination, was able to convert rJL into a highly neurovirulent virus, highlighting mechanistic differences between processes involved in neuroattenuation and neurovirulence.
INTRODUCTION
Mumps virus (MuV) is a paramyxovirus belonging to the Rubulavirus genus. The nonsegmented negative-sense genome of 15,384 nucleotides contains the following seven transcription units: the nucleoprotein (N), the V/phosphoprotein (V/P/I), the matrix protein (M), the fusion protein (F), the small hydrophobic protein (SH), the hemagglutinin-neuraminidase protein (HN), and the large protein (L) genes. Each gene encodes a single protein, with the exception of the V/P/I gene (conventionally referred to as the P gene), which gives rise to additional mRNA species as a result of the cotranscriptional insertion of nontemplated G nucleotides between positions 461 and 466, the so-called editing site. Faithful transcription of the gene produces the V protein, whereas insertion of two G residues within the editing site produces an mRNA encoding the P protein, and insertion of four G residues produces an mRNA encoding the I protein, analogous to the W protein identified in other paramyxoviruses (9, 20, 28). The roles of the viral proteins in the life cycle of paramyxoviruses have been well described in the literature (9, 12, 20). Briefly, the N protein encapsidates the nascent viral RNA as it is being synthesized, forming a ribonucleoprotein (RNP) complex, which serves as the substrate for the viral RNA-dependent RNA polymerase (RdRp), formed by the P and L proteins. The HN glycoprotein mediates attachment of the virus to its cellular receptor (sialic acid) and, together with the F glycoprotein, mediates fusion of the virion membrane with the target cell membrane. Based on studies of related paramyxoviruses, the M protein is involved in assembling the RNP at the plasma membrane in regions containing the HN and F glycoproteins, presumably via interacting with the carboxy-terminal tail portion of the RNP-associated N protein and the cytoplasmic tails of the glycoproteins (11, 16, 38). The SH protein itself is not required for virus replication but is believed to serve luxury functions, such as exhibiting antiapoptotic activity (43, 47). The V protein is a nonstructural protein that interferes both with induction of beta interferon (IFN-β) (3) and with the interferon-mediated antiviral responses (18, 19). The role of the I protein in the life cycle of the virus is not known but, like the V protein, may be involved in inhibition of the IFN-mediated antiviral pathway (39).
MuV causes an acute communicable respiratory viral infection transmitted by oropharyngeal secretions. Approximately one-third to one-half of infections are asymptomatic or result in nonspecific respiratory symptoms. Specific symptoms are the result of viremia, which most likely occurs following virus spread from primary sites of replication in tissues of the upper respiratory tract to local lymph nodes, although the pathogenesis of mumps following natural infection has not been specifically demonstrated. Parotitis is the hallmark of mumps infection; however, the virus frequently invades the central nervous system (CNS), leading to aseptic meningitis, encephalitis, and other neurological complications (5, 9). Due to the neurovirulent nature of wild-type MuV, national regulatory authorities require preclinical neurovirulence safety testing of candidate live, attenuated MuV vaccines. Such testing is typically performed in intracerebrally inoculated monkeys, although this assay appears to not reliably discern sufficiently from insufficiently attenuated strains (1, 33). Thus, it is perhaps not surprising that many MuV vaccines have caused aseptic meningitis in vaccinees despite presumably passing monkey neurovirulence safety testing (4, 29). In order to overcome the current difficulties in preclinical neurovirulence assessment of new mumps vaccine candidates, more reliable and predictive animal models are being evaluated, including a newborn rat model, developed in our laboratory, in which the severity of MuV-induced hydrocephalus following intracerebral inoculation appears to correlate with the human neurovirulence potential of the virus (30, 32). Here, using this model, we investigated molecular determinants of MuV neurovirulence and neuroattenuation by testing a series of chimeric recombinant viruses composed of various combinations of genes derived from a cDNA clone of the neurovirulent 88-1961 (r88) MuV strain and from a cDNA clone of the highly neuroattenuated Jeryl Lynn (rJL) vaccine virus-derived strain.
MATERIALS AND METHODS
Cell lines.
Vero (monkey kidney) cells were grown in Dulbecco's modified Eagle's medium (DMEM; Quality Biological, Inc., Gaithersburg, MD) supplemented with 10% (vol/vol) fetal bovine serum (FBS; Quality Biological, Inc., Gaithersburg, MD). BHK BSRT7/5 cells (7), kindly provided by Ulla Buchholz (Bethesda, MD), were maintained in DMEM supplemented with 10% (vol/vol) FBS and 1 mg/ml Geneticin at every other passage (Invitrogen, Carlsbad, CA).
RT-PCR, PCR, and sequencing.
All reverse transcription (RT) reactions were carried out using the SuperScript II reverse transcriptase kit (Invitrogen). Overlapping PCR fragments, used for overlap extension PCR (15), were produced using Taq DNA polymerase (Promega, Madison, WI). All other PCR amplifications were carried out using Expand high-fidelity polymerase (Roche Biochemicals, Burlington, NC). Sequencing was done using an ABI 3100 and an ABI 3730xl automated capillary DNA sequencer (Applied Biosystems, Carlsbad, CA) by the Center for Biologics Evaluation and Research (FDA, CBER, Bethesda, MD) core facility or by Macrogen USA Corp. (Rockville, MD). Sequence data were analyzed with the Chromas (Technelysium, Tewantin, Australia) and Jellyfish (LabVelocity, Los Angeles, CA) software packages.
Construction of plasmids.
Construction of expression plasmids pMuVNP, pMuVP, and pMuVL (kindly provided by D. Clarke, Wyeth-Lederle Vaccines, Pearl River, NY) carrying the rJL N, P, and L genes, respectively, expression plasmids p-N, p-P, and p-L carrying the r88 N, P, and L genes, respectively, full-length cDNA clone pMuV(MPBS) carrying the “JL5” major component of the attenuated rJL vaccine, and full-length cDNA clone p88-1961A271 encoding the neurovirulent r88 wild-type MuV strain are described elsewhere (10, 21, 23, 24). Plasmids pMuV(MPBS) and p88-1961A271 were renamed pJL and p88A271, respectively, in the present study for ease of readability. Plasmid pJL contains artificially introduced restriction sites (MluI, PmeI, BmgBI, SgfI) in the untranslated regions (UTRs) flanking the M, F, SH, and HN genes, respectively, as well as a naturally occurring NheI site in the terminal coding region of the HN gene (21) (Fig. 1). It was anticipated that in vivo comparisons of virus rescued from pJL with virus rescued from p88A271 could be complicated by the presence of these restriction sites in one virus but not the other. To address this, a modified version of p88A271 was generated to include all of the aforementioned restriction sites in pJL and was termed p88mod. However, unlike pJL, introduction of the NheI site into p88mod (by changing A8342 to G) results in a predicted coding change in the HN protein (T578A). To control for a possible effect of this coding change, p88mod was altered by site-directed mutagenesis to restore this site to its native sequence. This plasmid was termed p88modΔNhe. A detailed description of the generation of p88mod and p88modΔNhe is available from us upon request.
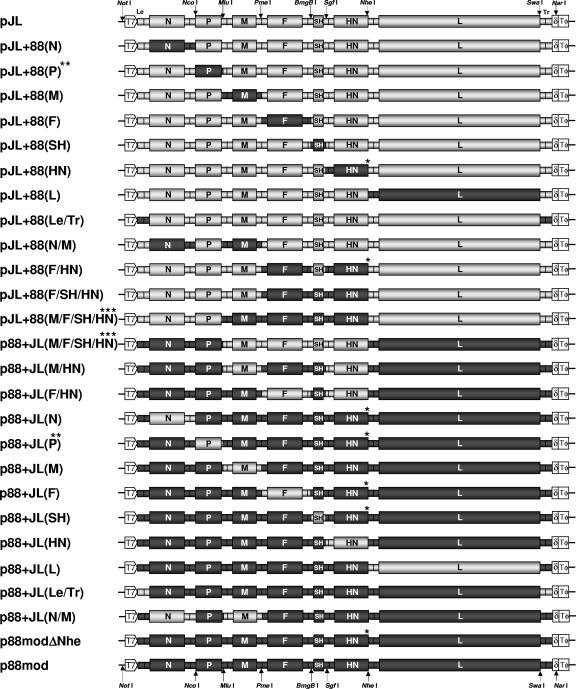
Fig. 1.
Overview of the genome structure of chimeric viruses. All chimeric cDNA constructs as well as plasmids p88mod and p88modΔNhe were generated by replacing rJL-specific sequences from plasmid pJL (carrying the antigenome of the major component of the rJL vaccine strain) with those of MuV strain r88. All boxed elements shown in gray or black denote rJL- or r88-derived sequences, respectively. The locations of several restriction sites used for generation of the different constructs are indicated. Note that the NheI site is authentic in the ORF of the rJL HN gene but is not present in that of r88. The NheI site was introduced for cloning purposes in the r88 HN gene and is present in all constructs shown except for those that are marked with a single asterisk. Note that all other restriction sites indicated on the top and bottom of the cartoon are present in all constructs depicted. In all cDNA clones, the antigenome is flanked by a 5′ T7 RNA polymerase promoter and at the 3′ end by the hepatitis delta ribozyme (δ) and the T7 RNA polymerase terminator (TΦ). ORFs are indicated by large boxes. The smaller boxes between ORFs delineate untranslated regions that contain the gene end and gene start signals. The vertical black lines within these smaller boxes indicate the intergenic region. The Le and Tr regions are indicated. Note that the size of the individual genomic elements is for illustration purposes only and may not be to correct scale. Plasmid pJL is identical to pMuV(MPBS) (21). **, note that for reasons of simplicity, the V/P/I gene is referred to here as the P gene, as has been the convention in the past; ***, alternative names are used for pJL+88(M/F/SH/HN) shown in Fig. 2 [p88+JL(Le/N/P/L/Tr)] and for p88+JL(M/F/SH/HN) shown in Fig. 3 [pJL+88(Le/N/P/L/Tr)]. See Materials and Methods for further details.
Sequences from p88A271, p88mod, p88modΔNhe, and pJL were used to construct chimeric full-length cDNA plasmids containing various combinations of rJL-derived and r88-derived gene sequences. It should be noted that the term “gene” is being used here to denote the entire open reading frame (ORF) of the gene of interest as well as the partial flanking UTRs but not the entire flanking UTRs. This is a consequence of the cloning strategy which employs use of restriction sites located within the UTRs. Thus, in some cases, parts of the UTRs were still derived from the heterologous virus strain. A detailed description of the generation of all chimeric plasmids, including primer sequences, is available from us upon request. The basic strategy involved amplifying the respective genes and gene segments by PCR and/or overlap extension PCR and subcloning these PCR products into pCR2.1-TOPO (Invitrogen). All cloning steps were verified by sequencing of the foreign gene(s), including sites of ligation, in all chimeric viruses. In comparison to the JL5 sequence (GenBank accession no. AF338106), except for the intentionally introduced genetic tags by Clarke et al. (10) at U6081→ C (F gene; silent mutation), A8502→G (K22R; L protein), A11731 →G (L gene; silent mutation), and the restriction sites introduced by Lemon et al. (21), the following mutations were identified in pJL: G214→ U (E23D; N protein); A6028→G (I495V; F glycoprotein); C8459→U (L8F; L protein); and U11632→G (L gene, silent mutation). In comparison to the sequence of MuV 88-1961 (GenBank accession no. AF467767), except for the intentionally introduced tag by Malik et al. at U14161→C (L gene, silent mutation), the 88-1961 cDNA clone p88A271 (23) that was used as the template for generation of the various chimeric cDNA constructs displayed a mutation in the 3′ leader (Le) sequence at G26→A and in the 5′UTR of the N gene at G70→U.
Constructs with a predominant Jeryl Lynn background are identified with the prefix “pJL,” and those with a predominant 88-1961 background are identified with the prefix “p88.” The virus from which the replaced gene was derived is identified after the prefix, and the gene is in parentheses. When referring to the V/P/I gene, for reasons of simplicity, the more conventional abbreviation “P” is used. Thus, p88+JL(P) carries a recombinant virus that encodes not only the rJL P protein but also the rJL V and I proteins as well.
Rescue of recombinant viruses from cDNA.
For all virus rescues, BHK BSRT7/5 cells were grown to 95% confluence in 6-well dishes in the presence of 1 mg/ml Geneticin and a total volume of 2 ml DMEM-9% (vol/vol) FCS. Medium was replaced with 2 ml of fresh medium lacking Geneticin at least 2 h before transfection. For the rescue of all viruses containing the rJL N, P, and L genes, cells were transfected with a mixture containing 300 ng of pMuVNP, 50 ng of pMuVP, 200 ng of pMuVL, and 6.95 μg of the corresponding cDNA full-length constructs. For the rescue of all viruses containing the r88 N, P, and L genes, cells were transfected with a mixture containing 225 ng, 37 ng, and 172 ng, respectively, of the plasmids encoding the r88 N, P, and L proteins, respectively, and 6.95 μg of the corresponding cDNA full-length constructs. For the rescue of chimeric viruses that carried a heterologous set of N, P, and L genes, cells were transfected with the appropriate corresponding set of plasmids carrying the N, P, and L genes. The amounts of the respective plasmids were the same as those indicated above. For all transfections, DNA was mixed with 30 μl of Lipofectamine 2000 (Invitrogen) in a total volume of 530 μl of Opti-MEM I medium (Invitrogen) as the diluent. Cells were transferred to a 25-cm2 flask 48 h posttransfection (hpt), and depending on the number of syncytia present, cells were further transferred into four to six 6-well dishes or a 75-cm2 flask 48 to 72 h later. Supernatants were collected and (in case of 6-well dishes) pooled 6 to 11 days posttransfection (dpt). Confluent monolayers of Vero cells in 75-cm2 flasks were infected with 5 ml of supernatants from BHK BSRT7/5 cells and incubated in a total volume of 20 ml medium for 3 to 6 days. Supernatants were clarified by centrifugation at 1,200 rpm for 5 min, and aliquots were stored at −70°C. Virus titer was determined by plaque assay (35) and is expressed by the number of PFU. As a quality control measure, recombinant chimeric viruses were typically rescued twice from each full-length cDNA clone, identified by the suffixes 1 and 2. For example, rJL+88(HN)-1 is a virus rescued from a cDNA clone [pJL+88(HN)] expressing the full-length rJL virus but containing the HN gene from r88. Virus rJL+88(HN)-2 is a repeat rescue from this same cDNA. In the case of p88+JL(SH), a third rescue was carried out. Each rescue was tested independently in vitro for replication kinetics and in vivo for neurovirulence assessment. All rescued viruses were partially or fully sequenced.
Nucleotide sequencing of the cDNA-derived chimeric viruses.
RNA from virus supernatants clarified by centrifugation was extracted with the QIAamp MinElute virus spin kit (Qiagen, Valencia, CA), as recommended by the manufacturer. Samples were incubated with DNase (2 units per 50 μl RNA eluate) for 10 min at 37°C, followed by heat inactivation in the presence of 3.5 mM EDTA for 10 min at 75°C. RNA was subjected to RT-PCR using up to 15 different primer pairs that produced partially overlapping amplicons ranging in size from 629 to 1,884 bp. To verify the RT dependence of RT-PCRs, parallel RT reactions were carried out, omitting the reverse transcriptase enzyme. All PCR fragments were completely sequenced, and nucleotide heterogeneities were confirmed either by sequencing both strands of the PCR products or by a second PCR or a second independent RT-PCR. The nucleotides composing a heterogeneous site were designated either equivalent or major/minor based on chromatogram peaks. Sequence information for all primers used for RT-PCR and for sequencing can be obtained from us upon request.
In vitro multicycle growth kinetics.
To study kinetics of virus growth in vitro, Vero cells were seeded onto 6-well plates and grown until confluence. Cells (2 × 106 to 3 × 106 per well) were infected at a multiplicity of infection (MOI) of 0.05 in a total volume of 500 μl DMEM-FBS. Each virus was tested in duplicate wells. Following incubation for 1 h at 37°C on a rocking platform, supernatants were removed, cells were washed twice with phosphate-buffered saline (PBS), and 2 ml of medium each was added. For each time point, 10% of the cell culture supernatant was removed and stored at −70°C until determination of virus titers. The removed volumes of medium were replaced with equal volumes of medium. This procedure was repeated every 24 h for a period of 6 days. Samples were additionally taken at 36 h postinfection (hpi).
Growth kinetics in rat brain.
Litters of Lewis rats (Harlan, Indianapolis, IN) were inoculated intracerebrally within 16 h postpartum with 20 μl of Eagle's minimum essential medium (EMEM) containing 100 PFU of virus. On days 1, 2, 3, 4, 6, and 8 postinfection (p.i.), the brains from 2 to 8 rats (4 to 6 rats for days 1, 2, and 4; 4 to 8 for day 3; 3 to 5 for day 6; and 2 to 4 for day 8) from each virus group were removed aseptically. Brains were homogenized into a 20% (wt/vol) suspension in DMEM with 2% (vol/vol) FBS by Dounce homogenization, followed by three brief pulses (10 s each) of ultrasonic treatment. Homogenates were clarified by centrifugation at 2,000 × g at 4°C for 10 min and stored at −70°C until examination by plaque assay (35) for virus content per gram of brain.
Neurovirulence phenotype determination.
The neurovirulence phenotype of the rescued viruses was assessed by measuring the extent of MuV-induced hydrocephalus, the major neuropathological outcome of MuV infection in rats, as previously described (32). Briefly, for each virus rescued, 2 to 7 litters of Lewis rats were inoculated intracerebrally with 20 μl of EMEM containing 100 PFU of virus. The back-titers of the remaining inocula were determined by plaque assay (35) to control for accuracy of the prepared dilutions. On day 30 postinoculation, rats were humanely sacrificed by CO2 asphyxiation by following the NIH Guidelines for the Care and Use of Laboratory Animals. Brains were removed, divided sagittally, and fixed in 10% neutral buffered formalin at 4°C for 4 to 5 days, followed by paraffin embedding. One 8- to 10-μm-thick sagittal section was selected at a standard distance from either side of the anatomical midline, and both were stained with hematoxylin and eosin (H&E). The neurovirulence score, which is a measure of the severity of MuV-induced hydrocephalus, was determined by calculating the ratio between the cross-sectional area of the brain (excluding the cerebellum) and the cross-sectional area of the lateral ventricle (which is enlarged following infection with neurovirulent MuV) on each tissue section using Image Pro Plus image analysis software (Media Cybernetics, Silver Spring, MD). The mean ratio (given in percent) of these two measurements on each of the two tissue sections per rat brain is the neurovirulence score for that particular brain. The neurovirulence score for a given virus variant is determined by the mean neurovirulence score for all brains within a treatment group. Statistical analyses were done using SigmaPlot 11 (Systat Software, Inc., San Jose, CA) software. All comparisons used the t test or, if the normality test (Shapiro-Wilk) failed, the Mann-Whitney rank sum test (α = 0.05).
RESULTS
Generation of chimeric viruses.
To identify gene-specific contributions to neuroattenuation and neurovirulence, genetic material from the rJL MuV strain (fully neuroattenuated) and from the r88 MuV strain (highly neurovirulent) were used to construct a series of chimeric recombinant viruses consisting of rJL-derived genes in an r88 background and of r88-derived genes in an rJL background (Fig. 1). As a control measure to monitor for the possibility of an effect on neuroattenuation and neurovirulence by random mutations arising during virus rescue and expansion, all recombinant chimeric virus stocks [with the exception of r88+JL(M/HN)] were rescued twice and independently tested in vivo for consistency (discussed later).
Viruses rescued from p88A271 (an authentic neurovirulent full-length clone of clinical isolate 88-1961[23]), p88mod (identical to p88A271 but containing the artificially introduced restriction sites MluI, PmeI, BmgBI, and SgfI in the UTRs flanking the M, F, SH, and HN genes, respectively, and NheI in the carboxy-terminal coding region of the HN gene), and p88modΔNhe (identical to p88mod but with the NheI site restored to its native sequence) were of similarly high neurovirulence in rats (Fig. 2), demonstrating a lack of a significant effect of these restriction sites on virus neurovirulence phenotype. In contrast to these high neurovirulence scores, virus rescued from pJL was highly neuroattenuated, consistent with previously determined rat neurovirulence scores obtained for the Jeryl Lynn vaccine virus (31, 32) (Fig. 2).
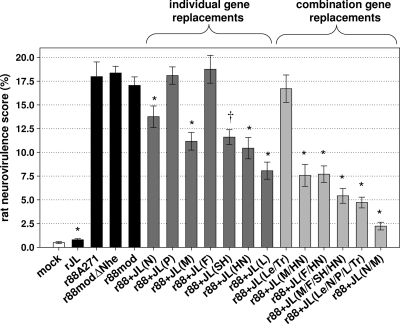
Fig. 2.
Severity of hydrocephalus in rats inoculated with r88-derived viruses. All bars represent the mean values of neurovirulence scores from two independent rescues each except for viruses r88+JL(M/HN), r88mod, and r88A271, for which only one rescued virus was evaluated (the latter virus has been tested extensively in our laboratory for other studies [23, 25] and consistently results in very high neurovirulence scores, similar to the one determined here), and r88+JL(SH), for which three rescued viruses were tested. Error bars indicate standard errors of the means (SEM). Asterisks denote statistically significant differences (i.e., P values of less than 0.05) between the indicated virus and reference viruses r88A271, r88modΔNhe, and r88mod. †, due to the differences in individual neurovirulence scores of the r88+JL(SH) viruses (Table 1), no statistics were applied to the mean value. Mock infections were done using virus diluent. Note that virus r88+JL(Le/N/P/L/Tr) is identical to virus rJL+88(M/F/SH/HN) depicted in Fig. 1. Refer to Fig. 1 for further details on the viruses tested.
Gene-specific effects on neuroattenuation.
To identify genetic determinants of MuV neuroattenuation, genes of r88 were substituted individually and in combination with corresponding genes of rJL. Results are summarized in Fig. 2. Individual replacement of the P and F genes had no effect on neurovirulence phenotype, nor did replacement of the leader (Le) and trailer (Tr) transcriptional control regions (consisting of the noncoding 145 and 161 nucleotides at the 3′ and 5′ ends of the genome, respectively, that encompass the genomic ends, the Le and Tr regions, and the upstream N-UTR and downstream L-UTR, respectively). All other individual gene replacements reduced r88 neurovirulence by 25% to 50%. With the exception of virus rescued from cDNA plasmids p88+JL(P) and p88+JL(SH), the neurovirulence scores of repeat rescues from the same plasmid were consistent (Table 1), suggesting that any random mutations that may have arisen during the production of these virus stocks were unlikely to have been responsible for the observed neurovirulence phenotype. While the neurovirulence levels of the two viruses rescued from p88+JL(P) were significantly different from one another (21.3% versus 15.2%) (Table 1), relative to that of the parental virus, neither virus was attenuated, suggesting that the rJL V, P, and I proteins are not involved in the neuroattenuation of r88. With regard to plasmid p88+JL(SH), the neurovirulence score of the first rescue [r88+JL(SH)-1] was significantly lower than that of the second rescue [r88+JL(SH)-2] (9.6% versus 17.0%) (Table 1). We therefore performed a third rescue from p88+JL(SH), which yielded a neurovirulence score identical to that of the first rescue (9.6%) (Table 1). As will be discussed later, although it is not clear if the rJL SH gene itself is responsible for the reduced neurovirulence observed with two of the three rescued viruses, it is clear that neither the SH gene nor any of the other individual genes tested are capable of conferring complete neuroattenuation.
Table 1.
Comparison of rat neurovirulence scores and peak virus titers in Vero cells of individual rescued virusese
| Virus | Rescue | RNV score (mean ± SEM) | P valued | Maximum titer in Vero cells (no. of PFU/ml, log10) |
|---|---|---|---|---|
| rJL | 1 | 0.84 ± 0.15 | 0.21 | 6.32 |
| 2 | 0.52 ± 0.1a | 6.19 | ||
| rJL+88(N) | 1 | 2.24 ± 0.8 | 0.32 | 6.82 |
| 2 | 1.23 ± 0.17 | 6.03 | ||
| rJL+88(P) | 1 | 1.78 ± 0.47 | 0.26 | 7.04 |
| 2 | 1.12 ± 0.23 | 7.05 | ||
| rJL+88(M) | 1 | 2.32 ± 0.81 | 0.89 | 6.82 |
| 2 | 1.13 ± 0.31 | 6.62 | ||
| rJL+88(F) | 1 | 1.3 ± 0.16 | 0.2 | 7.31 |
| 2 | 0.98 ± 0.17 | 7.35 | ||
| rJL+88(SH) | 1 | 0.77 ± 0.23 | 0.49 | 6.57 |
| 2 | 0.72 ± 0.15 | 6.38 | ||
| rJL+88(HN) | 1 | 2.71 ± 0.76 | 0.001 | 5.57 |
| 2 | 0.9 ± 0.2 | 5.44 | ||
| rJL+88(L) | 1 | 0.89 ± 0.1 | 0.47 | 7.41 |
| 2 | 0.83 ± 0.13 | 7.5 | ||
| rJL+88(Le/Tr) | 1 | 0.73 ± 0.1 | 0.87 | 6.52 |
| 2 | 0.8 ± 0.16 | 6.48 | ||
| rJL+88(N/M) | 1 | 2.98 ± 0.81 | 0.31 | 7.0 |
| 2 | 2.22 ± 0.66 | 6.89 | ||
| rJL+88(F/HN) | 1 | 2.03 ± 0.27 | 0.12 | 7.16 |
| 2 | 3.89 ± 0.89 | 7.17 | ||
| rJL+88(F/SH/HN) | 1 | 2.61 ± 0.65 | 0.07 | 7.12 |
| 2 | 1.36 ± 0.56 | 7.14 | ||
| rJL+88(M/F/SH/HN)c | 1 | 4.13 ± 0.9 | 0.69 | 7.63 |
| 2 | 4.94 ± 0.71 | 7.68 | ||
| r88+JL(M/F/SH/HN)c | 1 | 3.55 ± 1.65 | 0.09 | 7.25 |
| 2 | 5.89 ± 0.88 | 6.2 | ||
| r88+JL(F/HN) | 1 | 9.96 ± 1.93 | 0.19 | 7.17 |
| 2 | 6.81 ± 0.92 | 7.3 | ||
| r88+JL(M/HN)b | 1 | 7.58 ± 1.16 | NA | 7.32 |
| r88+JL(N) | 1 | 13.14 ± 1.37 | 0.32 | 7.99 |
| 2 | 14.42 ± 1.83 | 8.14 | ||
| r88+JL(P) | 1 | 15.23 ± 1.06 | <0.001 | 7.23 |
| 2 | 21.33 ± 1.24 | 8.98 | ||
| r88+JL(M) | 1 | 11.59 ± 1.15 | 0.53 | 7.29 |
| 2 | 10.3 ± 1.61 | 7.51 | ||
| r88+JL(F) | 1 | 20.88 ± 1.84 | 0.056 | 5.66 |
| 2 | 15.45 ± 2.27 | 6.22 | ||
| 1 | 9.55 ± 0.97 | <0.001 | 7.94 | |
| r88+JL(SH) | 2 | 16.97 ± 1.7 | 0.001 | 8.01 |
| 3 | 9.55 ± 1.11 | 8.37 | ||
| r88+JL(HN) | 1 | 11.49 ± 1.47 | 0.24 | 7.41 |
| 2 | 8.74 ± 1.7 | 7.8 | ||
| r88+JL(L) | 1 | 6.64 ± 1.17 | 0.15 | 7.61 |
| 2 | 9.37 ± 1.5 | 7.51 | ||
| r88+JL(Le/Tr) | 1 | 17.25 ± 2 | 0.42 | 8.07 |
| 2 | 15.7 ± 1.88 | 7.29 | ||
| r88+JL(N/M) | 1 | 1.88 ± 0.66 | 0.24 | 7.42 |
| 2 | 2.48 ± 0.52 | 7.22 | ||
| r88modb | 1 | 17.06 ± 0.89 | NA | 7.81 |
| r88modΔNhe | 1 | 18.31 ± 0.81 | 0.86 | 8.35 |
| 2 | 18.66 ± 1.38a | ND | ||
| r88A271b | 1 | 17.98 ± 1.54 | NA | 8.29 |
Only 1 litter was analyzed.
Only 1 rescue was performed.
Alternative names are used for rJL+88(M/F/SH/HN) shown in Fig. 2 [r88+JL(Le/N/P/L/Tr)] and for r88+JL(M/F/SH/HN) shown in Fig. 3 [rJL+88(Le/N/P/L/Tr)].
P values highlighted in boldface indicate statistical significant differences in RNV scores between repeat rescues (P < 0.05).
RNV, rat neurovirulence; NA, not applicable; ND, no done.
As it was not practical to construct p88-based plasmids carrying all possible combinations of rJL-derived genes, we separately evaluated combinations of envelope-associated (M, F, SH, HN) and replication complex-associated (Le, N, P, L, Tr) genes (Fig. 1). Not surprisingly, relative to individual gene replacements, combined gene replacements led to more substantial neuroattenuation; however, not even extensive gene replacement could fully neuroattenuate r88 (Fig. 2). The greatest effect was achieved with virus rescued from plasmid p88+JL(M/F/SH/HN) expressing all envelope-associated genes and from plasmid p88+JL(Le/N/P/L/Tr) expressing all replication complex-associated genes, both of which reducing r88 neurovirulence by approximately 70%.
Our results demonstrating that no combination of JL envelope-associated or replication complex-associated genes was capable of fully neuroattenuating r88 implicated the requirement of a combination of envelope- and replication complex-associated genes for full neuroattenuation. To test this hypothesis, a plasmid carrying the rJL N and M genes in an r88 background was constructed, and rescued virus was analyzed in vivo. Compared to its parental r88 virus, this chimeric virus was nearly completely neuroattenuated (17.1% versus 2.2%) (Fig. 2).
Gene-specific effects on neurovirulence induction.
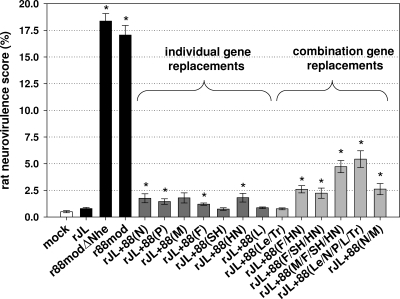
Up to this point, we have demonstrated the ability of several rJL genes, individually and in combination, to confer various degrees of neuroattenuation to r88. This raised the question as to whether these genes could convert the highly neuroattenuated rJL virus into a neurovirulent virus. We therefore produced chimeric full-length cDNA plasmids consisting of r88-derived genes in an rJL background and investigated the neurovirulence phenotype of viruses rescued from these plasmids. Results are presented in Fig. 3. While certain r88-derived genes and gene combinations were capable of increasing the neurovirulence of rJL, the effect was only minor, particularly compared to the neurovirulence scores of the r88 viruses. The greatest effect was achieved with virus rescued from plasmids carrying all r88 envelope-associated genes [pJL+88(M/F/SH/HN)] or all r88 replication complex-associated genes [pJL+88(Le/N/P/L/Tr)], in both cases increasing the neurovirulence score to approximately 5%. Although this is substantially higher than the 0.8% score for rJL, these viruses remained substantially neuroattenuated. Surprisingly, the N/M gene combination, which was highly effective in altering the neurovirulence phenotype of r88, had very little effect on the neurovirulence phenotype of rJL. As with the r88-based viruses, the neurovirulence scores of repeat rescues from the same JL-based plasmids were consistent, with the exception of the two viruses rescued from cDNA plasmid pJL+88(HN) (Table 1). Even though the greater of the two scores [rJL+88(HN)-1; 2.7%] was statistically higher than that observed for rJL (0.8%), this increase in neurovirulence is minor compared to the neurovirulence scores of the recombinant r88 viruses (Fig. 3).
Fig. 3.
Severity of hydrocephalus in rats inoculated with rJL-derived viruses. All bars represent the mean values of neurovirulence scores from each of two independent rescues, except for virus r88mod, for which only one rescued virus was evaluated. Error bars indicate SEM. Asterisks denote statistically significant differences between the indicated virus and reference virus rJL (i.e., P values of less than 0.05). Mock infections were done using virus diluent. Note that virus rJL+88(Le/N/P/L/Tr) is identical to virus r88+JL(M/F/SH/HN) depicted in Fig. 1. Refer to Fig. 1 for further details on viruses tested.
Sequence analysis of recombinant viruses.
In order to verify the integrity of the rescued chimeric viruses, the replaced genomic regions of all rescued viruses were sequenced (Table 2). In addition, some chimeric viruses were sequenced entirely. Moreover, to evaluate the rate of mutations that occurs in parental unaltered rescued viruses, viruses rJL-1, r88modΔNhe-1, r88modΔNhe-2, and r88A271 were fully sequenced as well. Genomic positions that exhibited nucleotide heterogeneity were identified in the chromatograms of several viruses. Many of the detected sites of heterogeneity were in the form of silent mutations or occurred in noncoding regions and thus were unlikely to have affected the neurovirulence phenotype of the virus. In the majority of cases where coding changes were detected, the subpopulation with the wild-type nucleotide was predominant, and no effect on neurovirulence phenotype was apparent, given that the second rescued viruses from each of the plasmids (which lacked these mutations) exhibited similar neurovirulence scores (Table 1). The two exceptions were viruses rescued from p88+JL(SH) and from p88+JL(P). As will be discussed later, it is unclear what role each of the identified mutations may have had on the neurovirulence phenotype of the viruses rescued from these plasmids.
Table 2.
Nucleotide changes identified in rescued viruses
| Virus | Genomic region(s) sequenced (nt)a | Mutation detected in virus stockb | Amino acid changec |
|---|---|---|---|
| rJL-1 | 24–15362 | A14269 > G | L1944 (L); silent mut. |
| A14399 > G | N1988D (L) | ||
| rJL+88(N)-1 | 71–1921 | ||
| rJL+88(N)-2 | 71–1921 | ||
| rJL+88(P)-1 | 1860–3850 | ||
| rJL+88(P)-2 | 1860–3850 | ||
| rJL+88(M)-1 | 2871–5135 | ||
| rJL+88(M)-2 | 2910–5135 | U2928 > G | L317V (P) |
| rJL+88(F)-1 | 4111–6450 | ||
| rJL+88(F)-2 | 4111–6581 | C4361 > U | F367 (M); silent mut. |
| C5412 > U | F289 (F); silent mut. | ||
| rJL+88(SH)-1 | 6061–6551 | ||
| rJL+88(SH)-2 | 6031–6551 | ||
| rJL+88(HN)-1 | 6031–9100 | ||
| rJL+88(HN)-2 | 6031–9080 | ||
| rJL+88(L)-1 | 8121–15362 | U14355→G | F1973L (L) |
| rJL+88(L)-2 | 8121–15362 | ||
| rJL+88(F/HN)-1 | 4135–9061 | ||
| rJL+88(F/HN)-2 | 4168–9032 | ||
| rJL+88(Le/Tr)-1 | 23–411; 14762–15362 | ||
| rJL+88(Le/Tr)-2 | 23–411; 14756–15362 | ||
| rJL+88(N/M)-1 | 100–1941; 2910–5143 | ||
| rJL+88(N/M)-2 | 93–1941; 2982–5105 | ||
| rJL+88(F/SH/HN)-1 | 4105–8524 | ||
| rJL+88(F/SH/HN)-2 | 4108–9058 | ||
| rJL+88(M/F/SH/HN)-1 | 2980–9033 | ||
| rJL+88(M/F/SH/HN)-2 | 2983–8960 | ||
| r88+JL(N)-1 | 81–1971 | ||
| r88+JL(N)-2 | 80–1971 | ||
| r88+JL(P)-1 | 24–15363 | A6501 > U | NA (3′UTR of SH gene) |
| r88+JL(P)-2 | 24–15363 | ||
| r88+JL(M)-1 | 2980–5121 | ||
| r88+JL(M)-2 | 2981–5107 | ||
| r88+JL(F)-1 | 4107–6565 | ||
| r88+JL(F)-2 | 4110–6560 | ||
| r88+JL(SH)-1 | 69–15364 | U10811 < C | S792P (L) |
| G11542 < A | M1035I (L) | ||
| A2710 > G | Q244R (P) | ||
| r88+JL(SH)-2 | 71–15362 | A10501 > C | T688 (L); silent mut. |
| C12546 > A | T1370K (L) | ||
| r88+JL(SH)-3 | 24–15362 | G11669 < U | R1078I (L) |
| r88+JL(HN)-1 | 6041–9032 | ||
| r88+JL(HN)-2 | 6489–9041 | ||
| A11621 > G | M1062V (L) | ||
| r88+JL(L)-1 | 8001–15362 | G12590 = A | E1385K (L) |
| r88+JL(L)-2 | 8001–15362 | G12590 > A | E1385K (L) |
| r88+JL(F/HN)-1 | 4112–9031 | ||
| r88+JL(F/HN)-2 | 4111–9030 | A4431 = C | NA (5′UTR of M gene) |
| r88+JL(M/HN) | 2981–5116; 6485–9031 | ||
| r88+JL(Le/Tr)-1 | 22–391; 14731–15360 | ||
| r88+JL(Le/Tr)-2 | 22–391; 14731–15360 | A14755 < G | I2106M (L) |
| r88+JL(M/F/SH/HN)-1 | 2981–9031 | ||
| r88+JL(M/F/SH/HN)-2 | 2990–9000 | ||
| G2823 > A | G282R (P) | ||
| Nt insertion after A4481 of an additional A in poly(A) stretch (6 A's) in M gene intragenic stop signal: 6A > 7A | NA (noncoding region) | ||
| G11542 > U | M1035I (L) | ||
| C14919 = U | T2161I (L) | ||
| r88+JL(N/M)-1 | 24–15362 | ||
| G1317 > A | R391K (N) | ||
| r88+JL(N/M)-2 | 24–15362 | C7950 < U | S446F (HN) |
| r88modΔNhe-1 | 24–15362 | Nt insertion after A6210 of an additional A in poly(A) stretch (7 A's) in F gene intragenic stop signal: 7A = 8A | NA (noncoding region) |
| U6247→A | NA (5′UTR of SH gene) | ||
| G6251→C | NA (5′UTR of SH gene) | ||
| U7652 = A | Y347N (HN) | ||
| r88modΔNhe-2 | 24–15362 | C9749→U | H438Y (L) |
| r88A271 | 24–15362 | G14183 > U | V1916L (L) |
The genomic regions sequenced each involved the gene that was replaced in the respective chimeric virus. nt, nucleotides.
→, nucleotide change; >/</=, nucleotide heterogeneity with the wild-type nucleotide on the left side representing either the major (>), the minor (<), or an equal (=) fraction in the virus preparation compared to that of the mutant nucleotide. Scoring of a nucleotide to represent a major, minor, or equal fraction in the virus pool is based on the evaluation of the pattern of double peaks (indicative of nucleotide heterogeneity) in the chromatogram. Changes that involve amino acid replacements are highlighted in boldface.
Predicted amino acid heterogeneity. The affected protein is given in parentheses. mut., mutation; NA, not applicable.
Rarely were complete mutations identified. Of the 52 viruses sequenced, 11 fully (excluding the 3′- and 5′-end termini) and 41 partially, only four mutations in total were identified for which the parental nucleotide no longer was detectable, one in rJL+88(L)-1, two in r88modΔNhe-1, and one in r88modΔNhe-2 (Table 2). Of these, only two led to amino acid changes, and neither appeared to affect neurovirulence based on the observation that the second rescued viruses from each of the plasmids (which lacked these mutations) exhibited similar neurovirulence scores (Table 1).
Among all the viruses with genomic sites of nucleotide heterogeneity, there was only one instance in which an identical mutation was present in two independently rescued viruses from the same cDNA plasmid. In both r88+JL(L)-1 and r88+JL(L)-2, nucleotide heterogeneity was apparent at position 12590, predicted to result in amino acid change E1385K in the L protein (Table 2). Both of these viruses were significantly neuroattenuated compared to parental virus r88mod, raising the possibility that the observed attenuation was mediated by the mutation and not by the rJL L gene per se. To investigate whether the virus subpopulation with K1385 was responsible for the reduced neurovirulence phenotype, brains from three rats inoculated with r88+JL(L)-2 were harvested and homogenized at 3 days postinfection (day of peak virus production), and viral RNA was analyzed by RT-PCR. For all three brains analyzed, only native G12590 (E1385) could be identified in the PCR products, suggesting that the K1385 mutation does not play a role in the observed partial neuroattenuation.
Overall, whole-genome analysis of seven chimeric viruses revealed between 0 and 4 sites of nucleotide heterogeneity, which is in very good agreement with the frequency of mutations (two to four per genome) found for nonchimeric recombinant viruses rJL-1, r88modΔNhe-1, r88modΔNhe-2, and r88A271 (Table 2).
Rat neurovirulence scores correlate with in vivo virus replication potential.
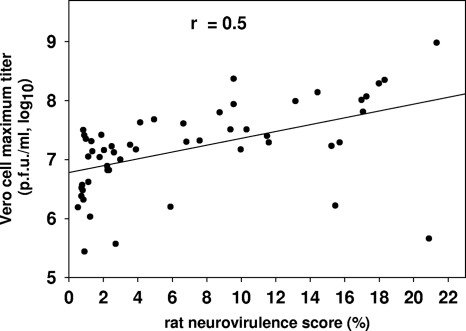
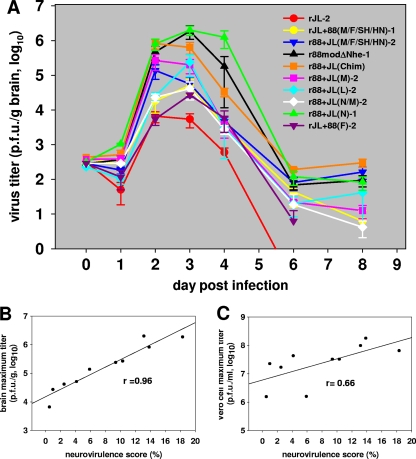
Peak viral titers for all recombinant viruses were determined by multicycle growth kinetics in Vero cells. Whereas we observed intervirus differences and some few differences between repeat rescues, all viruses were found to replicate efficiently (Table 1). Notably, all viruses that contained the rJL F gene exhibited a hyperfusogenic phenotype [with the exception of rJL+88(P)], compared to viruses containing the r88 F gene (data not shown). This led to a rapid onset of cytopathic effects around 48 h postinfection. The peak virus titers of rJL F-expressing viruses ranged from 2.5 × 105 PFU/ml to 3.2 × 107 PFU/ml. In contrast, those of the r88 F-expressing viruses ranged from 1.3 × 107 PFU/ml to 9.6 × 108 PFU/ml. There was no consistent relationship between fusogenicity in vitro and neurovirulence nor between in vitro virus growth potential and neurovirulence (Fig. 4). While we did observe a trend between maximal in vitro virus titers and neurovirulent potential, the correlation was poor (r = 0.5) (Fig. 4). In contrast, in vivo, a good correlation was observed between maximal viral titers and neurovirulence scores (r = 0.96) (Fig. 5b). This contrasts with results from plotting the neurovirulence scores of all viruses analyzed in Fig. 5a against the respective maximal virus titers measured in Vero cells (r = 0.66) (Fig. 5c), consistent with the result of the regression analysis of Vero cell titers for all rescued viruses (Fig. 4). These analyses suggest that brain maximal titers, but not maximal titers in Vero cells, are a correlate of neurovirulence.
Fig. 4.
Correlation between peak virus titers in Vero cells and neurovirulence scores of all rescued viruses. Regression analysis showing a poor correlation between peak virus titers in the Vero cells of 53 rescued viruses and their corresponding neurovirulence scores.
Fig. 5.
Analysis of virus growth kinetics in rat brain and relationship to neurovirulence scores. (A) Newborn rats were inoculated intracerebrally with the indicated viruses, and brains were harvested at indicated time points for determination of virus titers. Note that for rJL+88(F)-2 no rats were analyzed at day 8 p.i. and that virus r88+JL(Chim) represents an r88/rJL chimeric virus that was constructed for a separate as-yet-unpublished study. Error bars represent SEM. (B) Regression analysis showing a good correlation between maximal virus growth in rat brain and neurovirulence scores. (C) Regression analysis showing a poor correlation between maximal virus growth in vitro (Vero cells) and neurovirulence scores.
DISCUSSION
The goal of this study was to identify gene-specific determinants of MuV neuroattenuation and neurovirulence by constructing a series of recombinant full-length cDNA clones consisting of various combinations of genes derived from a highly neurovirulent wild-type MuV strain (88-1961 [r88]) and a highly neuroattenuated MuV vaccine strain (Jeryl Lynn [rJL]). Viruses rescued from these clones were then tested for neurovirulence in rats. The strategy for identifying gene-specific determinants of MuV neuroattenuation involved the construction of a cDNA clone of r88 in which r88 genes were replaced individually and in combination with corresponding genes from rJL. Exchange of the r88 F or P genes or the genomic 3′ and 5′ ends with the corresponding rJL-derived sequences had no neuroattenuating effect. In contrast, various degrees of neuroattenuation were achieved with all other individual gene replacement regimens (N, M, SH, HN, and L), ranging from an approximate 25% reduction in neurovirulence associated with N gene replacement to an approximate 50% reduction in neurovirulence associated with L gene replacement. The fact that individual rJL-derived genes were incapable of fully neuroattenuating r88 indicated that neuroattenuation of mumps virus is a multigenic trait. As expected, greater reductions in r88 neurovirulence were achieved with multiple gene replacements, ranging from an approximate 60% reduction in neurovirulence associated with the M/HN or F/HN gene combination to an approximate 90% reduction in neurovirulence associated with the N/M gene combination, a reduction far exceeding more extensive gene replacement combinations, including the full complement of envelope-associated genes (M/F/SH/HN) or all replication complex-associated genes (Le/N/P/L/Tr). Interestingly, the degree of neuroattenuation imparted by the N/M gene combination was substantially greater than an additive effect of the two genes alone (25% and 40%, respectively), suggesting a role of an N/M interaction in virus virulence. Given that the paramyxovirus M protein physically interacts with the N protein to facilitate virus assembly via associating the RNP with areas of the host cell membrane containing the viral glycoproteins (2, 22, 26, 37, 38, 44), it is noteworthy that in comparison to parental r88, the N/M gene combination chimeric virus grew to 100-fold-lower titers in vivo. Whether efficient viral assembly or budding is impaired in r88 viruses expressing the rJL N and/or M genes requires further investigation. Notably, we cannot exclude the possibility that other combinations of replication complex- and envelope-associated genes not tested here would lead to nearly complete attenuation of the r88 virus as well, but the creation and in vitro/in vivo characterization of chimeric recombinant viruses representative of the absolute number of all possible combinations of rJL-derived and r88-derived genes was not practical.
Interestingly, neither the N/M gene combination nor most other genes that substantially affected r88 neurovirulence were capable of conferring neurovirulence to the rJL strain. This highlights what must be significant differences in the process of neuroattenuation versus neurovirulence induction, which has also been suggested in studies of rabies virus by Yamada et al. (48). They demonstrated that the glycoprotein (G) gene from a neurovirulent strain was capable of converting an attenuated virus into a neurovirulent virus, yet the converse situation, i.e., replacement of the G gene of the neurovirulent virus with that from the attenuated virus, did not neuroattenuate the neurovirulent virus (48). That none of the many r88 genes and gene combinations tested in this study converted the rJL strain into a fully neurovirulent virus contrasts with data from a study by Lemon et al., who reported conversion of the attenuated rJL virus to a highly neurovirulent phenotype upon combined replacement of the F and HN genes (a combination tested in our study) with those of the wild-type rodent brain-adapted Kilham MuV strain (21). The bulk of the effect was imparted by the F gene, a gene that had no effect on the phenotype of either r88 or rJL in our hands. Thus, it appears that genetic determinants of MuV neurovirulence are not universal but rather are strain specific, as has been reported with rabies virus (40, 48).
A caveat to interpretation of results from this study is the possible influence on virus phenotype by random mutations that arise in the course of rescuing virus from cDNA and subsequent expansion in vitro to generate a working virus stock. Notably, this is a concern for all studies involving generation of RNA virus stocks and is a consequence of the inherent low fidelity of RNA-dependent RNA polymerases (RdRp) (6, 14, 36). The average mutation rate per genome per round of replication for RNA viruses has been estimated to be approximately 0.76 (13). A careful examination of the chromatograms generated in our study revealed an average of two mutations (mostly in the form of nucleotide heterogeneity) in each virus stock, indicating the presence of variant virus subpopulations. The use of more sensitive technologies, such as massively parallel sequencing, would likely reveal many more sites of heterogeneity, reflective of the evolution of the cloned virus after numerous rounds of replication. It is well documented that different virus populations within a quasispecies can impact virus phenotype (8, 34, 35, 45, 46). Although many of the mutations identified in our study were coding changes, in nearly all cases, the wild-type nucleotide was predominant, perhaps limiting any effect of these particular mutations on the measured neurovirulence of the virus. Dissection of the effect on virus phenotype by any specific mutation is complicated by the intrinsic high error rate of the viral RdRp. If one were to construct a new plasmid encoding any of the mutations of interest for further study, upon virus rescue and expansion, de novo mutations would likely arise elsewhere in the genome, making it impossible to discern effects imparted by the engineered mutation versus those imparted by new mutations arising at different sites. In this study, we attempted to address the possibility of randomly arising mutations influencing virus phenotype by performing at least two independent virus rescues from each cDNA plasmid and to demonstrate phenotypic similarity between the two. This assumes that identical mutations do not occur upon rerescue. Indeed, of all the rescued virus pairs sequenced, we found only one instance of an identical mutation [G12590A in r88+JL(L)-1 and r88+JL(L)-2] (Table 2), which most likely did not affect neurovirulence, given that the variant with the mutation was selected against within the first 3 days of replication in rat brain.
With few exceptions, repeat rescues of viruses behaved similarly in vivo. Significant intrapair differences in neurovirulence scores were seen only with viruses rescued from plasmids p88+JL(P), pJL+88(HN), and p88+JL(SH). Viruses rescued from p88+JL(P) and pJL+88(HN) ultimately did not appear to be of consequence, given that both viruses rescued from the former were highly neurovirulent, removing any argument supporting the independent involvement of the rJL P, V, and I proteins in significant attenuation, and for the latter, both viruses were highly attenuated, removing any argument supporting the r88 HN protein as a significant independent virulence factor.
The case is not as clear for the multiple rescues made from p88+JL(SH), which demonstrated much greater differences. Sequencing of these viruses revealed a total of two heterogeneous sites in r88+JL(SH)-1, both leading to coding changes in the L protein (S792P and M1035I), and a single heterogeneous site in r88+JL(SH)-3, also leading to a coding change in the L protein (R1078I). In all cases, the mutant nucleotide dominated over the wild-type nucleotide, and all were located within conserved domains, based on analogy to other paramyxoviruses and rhabdoviruses (41). Thus, rather than the rJL SH gene being responsible for the observed attenuation, it is quite possible that the mutations arising in the L gene during virus rescue were responsible. While two heterogeneous sites were also identified in the nonattenuated r88+JL(SH)-2 virus (one leading to a coding change in the L protein [T1370K] and the other to a coding change in the P protein [Q244R]), in both cases, the wild-type nucleotide dominated, thus the consensus sequences of the L and P genes in r88+JL(SH)-2 were identical to that of the parental r88 virus (r88modΔNhe). Notably, several nucleotide heterogeneities also were identified in viruses rescued from the r88 cDNA clone containing the rJL N/M gene combination. It is important to note that these as well as the mutations identified in the other chimeric viruses most likely are of a random nature, rather than of a compensatory nature, given that we also identified similar frequencies of mutations in several parental nonchimeric viruses.
Intriguingly, in two viruses, a single nucleotide insertion was identified in poly(A) intragenic stop signals, one at the end of the M gene [r88+JL(N/M)-1] and one at the end of the F gene (r88modΔNhe-1). This phenomenon is most likely due to the stuttering of the RdRp at homopolymeric tracts and has been reported previously (6, 36). Addition of a nucleotide to the mumps virus genome would violate the “rule of six,” thought to be a requirement for efficient replication of those paramyxoviruses that edit their P gene (17). However, the stringency of the rule of six has not been specifically examined for mumps virus, and in studies of related rubulaviruses, the stringency of this rule does not appear to be absolute (27, 42). Whether or not the two viruses in question here have compensatory deletions elsewhere, such as at the genomic ends, was not investigated due to expected complications in interpretation of results obtained from 3′ and 5′ rapid amplification of cDNA ends (RACE) results (35). In any case, since both r88+JL(N/M)-1 and r88+JL(N/M)-2 replicated with the same efficiency and displayed similar neurovirulence scores, and since the neurovirulence score or r88modΔNhe-1 was almost identical to that of r88modΔNhe-2, the nucleotide insertions likely did not have any impact on neurovirulence.
A second limitation to interpreting the data from this study involves the cloning strategy employed, which involved the use of restriction enzyme sites located within the UTRs between ORFs, resulting in the generation of chimeric viruses composed not only of the foreign inserted ORF but also of portions of the flanking UTRs. This is an approach used by many, but the implications are often not considered. Therefore, we cannot rule out the possibility that the apparent gene-specific effects on virus phenotype were in part due to the effects of the UTRs that display sequence differences between rJL and r88. Western blot analyses of select constructs failed to identify an effect of changes in the UTRs on protein expression levels, but this needs to be explored further, including an assessment of mRNA levels by Northern blotting, which will be the focus of future studies. Notably, for technical reasons, this limitation is difficult to circumvent, requiring extensive correction in each clone by site-directed mutagenesis. Nonetheless, this deserves exploration.
Although the pathological mechanism underlying MuV neurovirulence is not well understood, in the rat model, we have previously demonstrated that the r88 virus grows to significantly higher titers in brain tissue than the rJL virus and that the severity of hydrocephalus appeared to be associated with the extent of virus infection of the ventricular ependymal cells and the ability to spread deeper into the brain parenchyma (31). Nevertheless, it was unclear whether a strict correlation exists between maximum brain virus titers and neurovirulence scores. The recombinant viruses generated for this study provided a unique opportunity to investigate the relationship between virus replication potential and neurovirulence. In vitro, we observed a poor correlation between virus growth kinetics and neurovirulence scores. Of note, all viruses that expressed the rJL F gene in general exhibited a higher fusogenicity in Vero cells than those expressing the r88 F gene. This caused lysis of fused cells and likely prevented the virus from further replication to reach higher peak titers. However, omission of all rJL F-expressing viruses in the regression analysis (Fig. 4) led to an increase in the regression coefficient from 0.5 to 0.7 only (data not shown), indicating that fusogenicity is not a major determinant of virus titer and neurovirulence. Rather, replication complex-associated proteins, as expected, appear to be major determinants of peak virus titers in Vero cells. Nevertheless, the fact that we found a very good correlation between virus growth in the brain and neurovirulence might be due in part to the possibility that viruses expressing the rJL F gene might be unable to cause fusion of infected brain cells. These in vivo replication data are consistent with previous findings suggesting that the relative neurovirulence of MuV is associated with the extent of infection of ventricular ependymal cells (the primary targets of the virus in rats inoculated intracerebrally) and virus spread from these sites into the subventricular parenchyma (31). Notably, we did not examine virus growth in other rat tissues; thus, it is quite possible that a similar pattern of virus replication observed in the brain might also be apparent in extraneural tissues.
Results from this study demonstrating multiple virus proteins acting independently and in combination to affect the ability of virus to replicate in rat brain highlight the vast array of possible mechanisms of neuroattenuation. These results highlight the complexity of MuV neurovirulence and neuroattenuation and likely apply to other related viruses. From an applied perspective, further research in this area may provide a basis for the rationale design of new live attenuated vaccines, particularly for MuV, given the apparent difficulty in adequately neuroattenuating this virus, as indicated by the occurrence of aseptic meningitis in recipients of nearly all mumps vaccine strains, with the exception of vaccines derived from the rJL strain (29).
ACKNOWLEDGMENTS
Salary support for C.X.Z., L.N., and K.W. was provided by the Oak Ridge Institute for Science and Education through an interagency agreement between the U.S. Department of Energy and the U.S. Food and Drug Administration.
We thank U. Buchholz (NIH, Bethesda, MD) for providing the BHK BSR-T7/5 cells and D. Clarke (Wyeth, Pearl River, NY) for providing the JL helper plasmids. We are grateful to Hana Golding and Dmitriy Volokhov (FDA/CBER) for critical reading of the manuscript.
Footnotes
Published ahead of print on 4 May 2011.
REFERENCES
- 1. Afzal M. A., et al. 1999. Evaluation of the neurovirulence test for mumps vaccines. Biologicals 27:43–49 [DOI] [PubMed] [Google Scholar]
- 2. Ali A., Nayak D. P. 2000. Assembly of Sendai virus: M protein interacts with F and HN proteins and with the cytoplasmic tail and transmembrane domain of F protein. Virology 276:289–303 [DOI] [PubMed] [Google Scholar]
- 3. Andrejeva J., et al. 2004. The V proteins of paramyxoviruses bind the IFN-inducible RNA helicase, mda-5, and inhibit its activation of the IFN-beta promoter. Proc. Natl. Acad. Sci. U. S. A. 101:17264–17269 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Balraj V., Miller E. 1995. Complications of mumps vaccines. Rev. Med. Virol. 5:219–227 [Google Scholar]
- 5. Bang H. O., Bang J. 1943. Involvement of the central nervous system in mumps. Acta Med. Scand. 113:487–505 [Google Scholar]
- 6. Biacchesi S., Murphy B. R., Collins P. L., Buchholz U. J. 2007. Frequent frameshift and point mutations in the SH gene of human metapneumovirus passaged in vitro. J. Virol. 81:6057–6067 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Buchholz U. J., Finke S., Conzelmann K. K. 1999. Generation of bovine respiratory syncytial virus (BRSV) from cDNA: BRSV NS2 is not essential for virus replication in tissue culture, and the human RSV leader region acts as a functional BRSV genome promoter. J. Virol. 73:251–259 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Buesa-Gomez J., Teng M. N., Oldstone C. E., Oldstone M. B., de la Torre C. J. 1996. Variants able to cause growth hormone deficiency syndrome are present within the disease-nil WE strain of lymphocytic choriomeningitis virus. J. Virol. 70:8988–8992 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Carbone K. M., Rubin S. 2007. Mumps virus, p. 1527–1542 In Knipe D. M., Howley P. M.(ed.), Fields virology , 5th ed. Wolters Kluwer, Lippinocott Williams & Wilkins, Philadelphia, PA [Google Scholar]
- 10. Clarke D. K., Sidhu M. S., Johnson J. E., Udem S. A. 2000. Rescue of mumps virus from cDNA. J. Virol. 74:4831–4838 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Coronel E. C., Takimoto T., Murti K. G., Varich N., Portner A. 2001. Nucleocapsid incorporation into parainfluenza virus is regulated by specific interaction with matrix protein. J. Virol. 75:1117–1123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Curran J., Kolakofsky D. 1999. Replication of paramyxoviruses. Adv. Virus Res. 54:403–422 [DOI] [PubMed] [Google Scholar]
- 13. Drake J. W., Holland J. J. 1999. Mutation rates among RNA viruses. Proc. Natl. Acad. Sci. U. S. A. 96:13910–13913 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Holland J., et al. 1982. Rapid evolution of RNA Genomes. Science 215:1577–1585 [DOI] [PubMed] [Google Scholar]
- 15. Horton R. M. 1995. PCR-mediated recombination and mutagenesis. SOEing together tailor-made genes. Mol. Biotechnol. 3:93–99 [DOI] [PubMed] [Google Scholar]
- 16. Iwasaki M., et al. 2009. The matrix protein of measles virus regulates viral RNA synthesis and assembly by interacting with the nucleocapsid protein. J. Virol. 83:10374–10383 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Kolakofsky D., Roux L., Garcin D., Ruigrok R. W. H. 2005. Paramyxovirus mRNA editing, the ‘rule of six’ and error catastrophe: a hypothesis. J. Gen. Virol. 86:1869–1877 [DOI] [PubMed] [Google Scholar]
- 18. Kubota T., Yokosawa N., Yokota S., Fujii N. 2001. C terminal CYS-RICH region of mumps virus structural V protein correlates with block of interferon alpha and gamma signal transduction pathway through decrease of STAT 1-alpha. Biochem. Biophys. Res. Commun. 283:255–259 [DOI] [PubMed] [Google Scholar]
- 19. Kubota T., et al. 2005. Mumps virus V protein antagonizes interferon without the complete degradation of STAT1. J. Virol. 79:4451–4459 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Lamb R. A., Parks G. D. 2007. Paramyxoviridae: the viruses and their replication, p. 1449–1496 In Knipe D. M., Howley P. M.(ed.), Fields virology , 5th ed. Wolters Kluwer, Lippincott Williams and Wilkins, Philadelphia, PA [Google Scholar]
- 21. Lemon K., Rima B. K., McQuaid S., Allen I. V., Duprex W. P. 2007. The F gene of rodent brain-adapted mumps virus is a major determinant of neurovirulence. J. Virol. 81:8293–8302 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Li M., et al. 2009. Mumps virus matrix, fusion, and nucleocapsid proteins cooperate for efficient production of virus-like particles. J. Virol. 83:7261–7272 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Malik T. H., et al. 2007. A single nucleotide change in the mumps virus F gene affects virus fusogenicity in vitro and virulence in vivo. J. Neurovirol. 13:513–521 [DOI] [PubMed] [Google Scholar]
- 24. Malik T. H., et al. 2007. Functional consequences of attenuating mutations in the haemagglutinin neuraminidase, fusion and polymerase proteins of a wild-type mumps virus strain. J. Gen. Virol. 88:2533–2541 [DOI] [PubMed] [Google Scholar]
- 25. Malik T. H., Wolbert C., Nerret L., Sauder C., Rubin S. 2009. Single amino acid changes in the mumps virus haemagglutinin-neuraminidase and polymerase proteins are associated with neuroattenuation. J. Gen. Virol. 90:1741–1747 [DOI] [PubMed] [Google Scholar]
- 26. Matsumoto T. 1982. Assembly of paramyxoviruses. Microbiol. Immunol. 26:285–320 [DOI] [PubMed] [Google Scholar]
- 27. Murphy S. K., Parks G. D. 1997. Genome nucleotide lengths that are divisible by six are not essential but enhance replication of defective interfering RNAs of the paramyxovirus simian virus 5. Virology 232:145–157 [DOI] [PubMed] [Google Scholar]
- 28. Paterson R. G., Lamb R. A. 1990. RNA editing by G-nucleotide insertion in mumps virus P-gene mRNA transcripts. J. Virol. 64:4137–4145 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Plotkin S. A., Rubin S. A. 2008. Mumps vaccine, p. 435–465 In Plotkin S. A., Orenstein W. A., Offit P. A.(ed.), Vaccines , 5th ed. Saunders Elsevier, Philadelphia, PA [Google Scholar]
- 30. Rubin S. A., et al. 2005. The rat-based neurovirulence safety test for the assessment of mumps virus neurovirulence in humans: an international collaborative study. J. Infect. Dis. 191:1123–1128 [DOI] [PubMed] [Google Scholar]
- 31. Rubin S. A., et al. 2003. Changes in mumps virus gene sequence associated with variability in neurovirulent phenotype. J. Virol. 77:11616–11624 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Rubin S. A., et al. 2000. Evaluation of a neonatal rat model for prediction of mumps virus neurovirulence in humans. J. Virol. 74:5382–5384 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Rubin S. A., et al. 1999. The mumps virus neurovirulence safety test in rhesus monkeys: a comparison of mumps virus strains. J. Infect. Dis. 180:521–525 [DOI] [PubMed] [Google Scholar]
- 34. Sanz-Ramos M., Diaz-San S. F., Escarmis C., Domingo E., Sevilla N. 2008. Hidden virulence determinants in a viral quasispecies in vivo. J. Virol. 82:10465–10476 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Sauder C. J., et al. 2006. Changes in mumps virus neurovirulence phenotype associated with quasispecies heterogeneity. Virology 350:48–57 [DOI] [PubMed] [Google Scholar]
- 36. Sauder C. J., et al. 2009. Presence of lysine at aa 335 of the hemagglutinin-neuraminidase protein of mumps virus vaccine strain Urabe AM9 is not a requirement for neurovirulence. Vaccine 27:5822–5829 [DOI] [PubMed] [Google Scholar]
- 37. Schmitt A. P., Lamb R. A. 2004. Escaping from the cell: assembly and budding of negative-strand RNA viruses, p. 145–196 In Kawaoka Y.(ed.), Biology of negative strand RNA viruses: the power of reverse genetics , 1st ed., vol. 283 Springer-Verlag, Heidelberg, Germany: [DOI] [PubMed] [Google Scholar]
- 38. Schmitt P. T., Ray G., Schmitt A. P. 2010. The C-terminal end of PIV5 NP protein is important for virus-like particle production and M-NP protein interaction. J. Virol. 84:12810–12823 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Shaw M. L., Cardenas W. B., Zamarin D., Palese P., Basler C. F. 2005. Nuclear localization of the Nipah virus W protein allows for inhibition of both virus-and toll-like receptor 3-triggered signaling pathways. J. Virol. 79:6078–6088 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Shimizu K., et al. 2007. Involvement of nucleoprotein, phosphoprotein, and matrix protein genes of rabies virus in virulence for adult mice. Virus Res. 123:154–160 [DOI] [PubMed] [Google Scholar]
- 41. Sidhu M. S., Menonna J. P., Cook S. D., Dowling P. C., Udem S. A. 1993. Canine distemper virus L gene: sequence and comparison with related viruses. Virology 193:50–65 [DOI] [PubMed] [Google Scholar]
- 42. Skiadopoulos M. H., et al. 2003. The genome length of human parainfluenza virus type 2 follows the rule of six, and recombinant viruses recovered from non-polyhexameric-length antigenomic cDNAs contain a biased distribution of correcting mutations. J. Virol. 77:270–279 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Takeuchi K., Tanabayashi K., Hishiyama M., Yamada A. 1996. The mumps virus SH protein is a membrane protein and not essential for virus growth. Virology 225:156–162 [DOI] [PubMed] [Google Scholar]
- 44. Takimoto T., Portner A. 2004. Molecular mechanism of paramyxovirus budding. Virus Res. 106:133–145 [DOI] [PubMed] [Google Scholar]
- 45. Teng M. N., Oldstone M. B., de la Torre C. J. 1996. Suppression of lymphocytic choriomeningitis virus—induced growth hormone deficiency syndrome by disease-negative virus variants. Virology 223:113–119 [DOI] [PubMed] [Google Scholar]
- 46. Vignuzzi M., Stone J. K., Arnold J. J., Cameron C. E., Andino R. 2006. Quasispecies diversity determines pathogenesis through cooperative interactions in a viral population. Nature 439:344–348 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Wilson R. L., et al. 2006. Function of small hydrophobic proteins of paramyxovirus. J. Virol. 80:1700–1709 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Yamada K., Ito N., Takayama-Ito M., Sugiyama M., Minamoto N. 2006. Multigenic relation to the attenuation of rabies virus. Microbiol. Immunol. 50:25–32 [DOI] [PubMed] [Google Scholar]