Abstract
Objectives
Personality factors parsimoniously capture the variation in dispositional characteristics that affect behaviours, but their value in predicting medication non-adherence is unclear. We investigated the relationship between five-factor model personality factors (Conscientiousness, Neuroticism, Agreeableness, Extraversion, and Openness) and medication non-adherence among older participants during a six-year randomized placebo-controlled trial (RCT).
Design
Observational cohort data from 771 subjects aged ≥72 years enrolled in the Ginkgo Evaluation of Memory study, a RCT of Ginkgo biloba for prevention of dementia.
Methods
Random effects logistic regression analyses examined effects of NEO Five-Factor Inventory scores on medication non-adherence, determined via pill counts every 6 months (median follow-up 6.1 years) and defined as taking <80% of prescribed pills. Analyses adjusted for covariates linked with non-adherence in prior studies.
Results
Each 5 year increment in participant age was associated with a 6.7% greater probability of non-adherence (95% confidence interval, CI [2.4, 11.0]). Neuroticism was the only personality factor associated with non-adherence: a 1 SD increase was associated with a 3.8% increase in the probability of non-adherence (95% CI [0.4, 7.2]). Lower cognitive function was also associated with non-adherence: a 1 SD decrease in mental status exam score was associated with a 3.0% increase in the probability of non-adherence (95% CI [0.2, 5.9]).
Conclusions
Neuroticism was associated with medication non-adherence over 6 years of follow-up in a large sample of older RCT participants. Personality measurement in clinical and research settings might help to identify and guide interventions for older adults at risk for medication non-adherence.
Health is profoundly influenced by personality, a relationship most established with the five-factor model (FFM) of personality (Costa & McCrae, 1997; Goldberg, 1993; Marshall, Wortman, Vickers, Kusulas, & Hervig, 1994). FFM factors – Neuroticism, Extraversion, Openness, Agreeableness, and Conscientiousness – are empirically derived clusters of dispositional tendencies that parsimoniously capture the major axes of psychological and behavioural variation in humans (Krueger, Caspi, & Moffitt, 2000; Watson & Hubbard, 1996). FFM factors have been linked with many health-related behaviours and outcomes (Bogg & Roberts, 2004; Chapman, Duberstein, & Lyness, 2007; Friedman, 2000; Roberts, Kuncel, Shiner, Caspi,&Goldberg, 2007), including medication non-adherence (Table 1).
Table 1.
Prior studies examining associations between FFM personality factors and medication non-adherence
| Study | Follow-up | Sample description | N | Mean age | Personality factors examined and findings |
||||
|---|---|---|---|---|---|---|---|---|---|
| Axelsson et al. (2009) | Cross-sectional | Population-based sample of asthmatics | 268 | 22 | Ca | N | A | E | O |
| Christensen, Moran, and Wiebe (1999) | Cross-sectional | Type I diabetics followed in endocrinology clinics | 107 | 42 | Ca | Na | |||
| Dobbels et al. (2005) | Cross-sectional | Heart, lung and liver transplant candidated | 174 | 52 | Ca | N | A | E | O |
| Penedo et al. (2003) | Cross-sectional | Community dwelling HIV + patients on highly active anti-retroviral therapy | 116 | 39 | C | N | A | E | O |
| Christensen and Smith (1995) | 8 weeks | Renal dialysis patients at an academic centre | 72 | 46 | Ca | Na | A | E | O |
| Cohen, Ross, Bagby, Farvolden, and Kenndy (2004) | 14 weeks | Depressed patients at an addiction centre | 65 | 41 | C | N | A | Ea | O |
| Ediger et al. (2007) | 1 year | Population-based sample of people with inflammatory bowel disease | 326 | NR | C | N | Aa | E | O |
| Insel et al. (2006) | 8 weeks | Community dwelling adults taking one or more daily medications | 60 | 77 | C | Na | A | E | O |
| O’Cleirigh, Ironson, Weiss, and Costa (2007) | 1 year | Community dwelling HIV + adults | 119 | 38 | Ca | ||||
| Stilley, Sereika, Muldoon, Ryan, and Dunbar-Jacob (2004) | 24 weeks | Generally healthy adults in a randomized trial of a lipid lowering drug | 158 | 46 | Ca | N | A | E | O |
Note. C, Conscientiousness; N, Neuroticism; A, agreeableness; E, Extraversion; O, Openness; HIV +, human immunodeficiency virus positive; NR, not reported.
Statistically significant association with non-adherence.
Medication non-adherence is common and associated with suboptimal health outcomes (DiMatteo, 2004; DiMatteo, Giordani, Lepper, & Croghan, 2002; Vik, Maxwell, & Hogan, 2004; Vik et al., 2006). Commonly studied correlates of non-adherence – increasing age, male gender, non-white race, lower income, depressive symptoms, obesity, smoking, cognitive impairment, disease burden, and lower social support (Briesacher, Gurwitz, & Soumerai, 2008; Gellad, Haas, & Safran, 2007; Molloy, Perkins-Porras, Strike, & Steptoe, 2008; Salas et al., 2008; Sayers, Riegel, Pawlowski, Coyne, & Samaha, 2008; Vik et al., 2004) – explain only part of the variance in adherence behaviour (Curtis et al., 2009). Disparate studies have linked non-adherence both with general psychological stress and health- and treatment-related cognitions, such as illness perceptions, self-efficacy, and perceived medication necessity and effectiveness (Chia, Schlenk, & Dunbar-Jacob, 2006). FFM factors efficiently capture much of the variance in these characteristics and thus may help unify the diffuse literature on this topic (Conard & Matthews, 2008; Costa, Somerfield, & McCrae, 1996; Sörensen, Duberstein, Chapman, Lyness, & Pinquart, 2008).
The 10 prior studies exploring associations between FFM factors and medication non-adherence had relatively small sample sizes, wide variation in participant health conditions, and yielded mixed findings (Table 1). Non-adherence has been associated with lower levels of Conscientiousness in six studies, higher levels of Neuroticism in three studies, and lower levels of Agreeableness and Extraversion in one study each (Table 1). All but one study focused on samples with mean ages in range of 20–50 years, so their applicability to older adults is unclear. All studies were either cross-sectional or longitudinal lasting 1 year or less. The lack of longer follow-up is problematic, since most medications prescribed to older adults are for chronic conditions (Machlin, Cohen, & Beauregard, 2008). Finally, prior FFM analyses failed to account for most of the aforementioned covariates commonly associated with non-adherence, so it is unclear whether FFM factors are independently associated with medication non-adherence at any age.
To address these limitations, we examined the relationship of FFM factors to medication non-adherence in a subset of participants in the six year Ginkgo Evaluation of Memory (GEM) study (DeKosky et al., 2006). Based on the literature summarized above, we hypothesized medication non-adherence would be significantly associated with lower levels of Conscientiousness (e.g., less reliability, diligence, and health consciousness; Costa & McCrae, 1997; Goldberg, 1993; Marshall et al., 1994); and higher levels of Neuroticism, since individuals who are more distress prone would be expected to experience disproportionately negative emotions in response to the minor inconvenience of daily pill taking. For the remaining FFM factors, we did not have specific hypotheses, since they exhibited little consistent relationship with non-adherence in prior studies. Our analyses adjusted for patient socio-demographic factors (age, gender, race/ethnicity, education, income), health characteristics (self-rated health, disease burden, smoking status, body mass index (BMI), depressive symptoms, cognitive functioning), and social contact – all of which have been linked with medication non-adherence in prior studies.
Methods
Details of the GEM study have been published elsewhere (DeKosky et al., 2006). The study was conducted under an investigational new drug application with the Food and Drug Administration under the auspices of the National Center for Complementary and Alternative Medicine (NCCAM) and registered at clinicaltrials.gov (see Appendix for a listing of GEM study personnel). The main finding of the GEM study was that Ginkgo biloba had no impact on the development of dementia (DeKosky et al., 2008). While eligible subjects were recruited at four sites between 2000 and 2002, for this sub-study examining the relationship between personality and non-adherence, only subjects at the University of California, Davis (UCD) site were recruited, after consenting to the additional data collection.
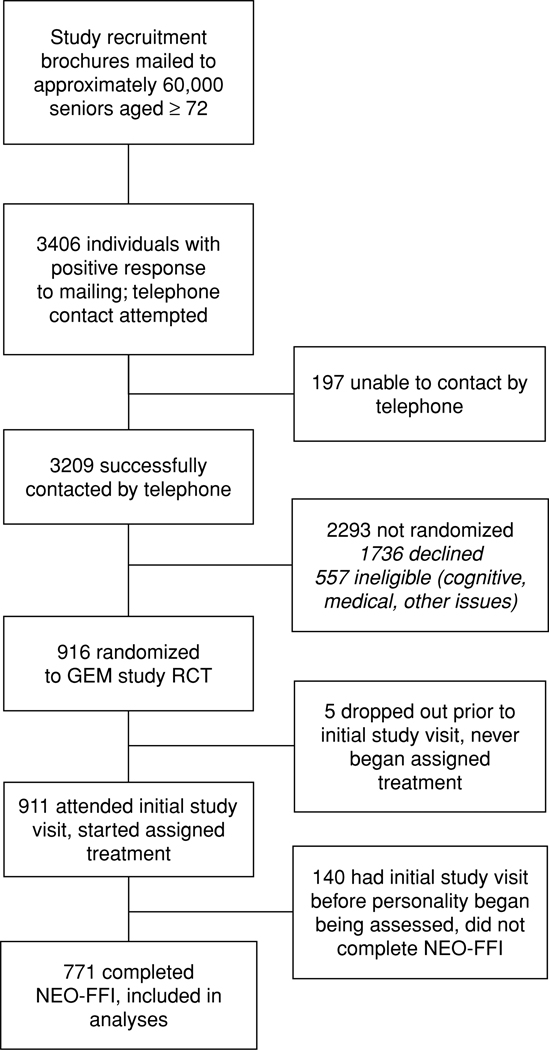
Key study enrolment criteria included: age over 72 years, availability of proxy respondent, English as usual language, and absence of significant morbidity. Details regarding the study enrolment criteria and recruitment process have been presented elsewhere (DeKosky et al., 2008; Fitzpatrick et al., 2006). Figure 1 summarizes subject recruitment and flow through the study at the UCD site. A total of 916 subjects were randomized to receive either G. biloba or identical appearing placebo at the UCD site. However, 5 (0.5%) dropped out of the study before their initial study visit, prior to beginning to take their randomly assigned treatment, and another 140 (15%) had their initial study visit before the personality measure had begun being administered. Thus, only 771 (84.2%) completed the personality inventory and are included in the current analysis. Subjects at the UCD site had characteristics similar to those at the other sites (Fitzpatrick et al., 2006). Subjects received follow-up study assessment visits, during which research measures were completed and pill counts were conducted, every 6 months until study conclusion (closeout visit October 2007–April 2008), a maximum of 7.3 years (median 6.1 years).
Figure 1.
Subject recruitment and participation. GEM, gingko evaluation of memory; RCT, randomized controlled trial; NEO-FFI, NEO five-factor inventory.
Measures
FFM personality factors
The FFM of personality, a well-validated taxonomy of personality traits, guided the present study’s approach to personality assessment (McCrae & Costa, 1997). FFM factors were measured with the NEO Five-Factor Inventory (NEO-FFI), a well-validated 60-item self-report questionnaire with 12 items measuring each of the five personality domains (range of scores for each factor, 12–60; Costa & McCrae, 1992). Examples of items assessing each factor include: ‘I try to be courteous to everyone I meet’ (Agreeableness); ‘I keep my belongings clean and neat’ (Conscientiousness); ‘I like to have a lot of people around me’ (Extraversion); ‘I often feel inferior to others’ (Neuroticism); and ‘I have a lot of intellectual curiosity’ (Openness). Response options comprise a five-point Likert scale from ‘strongly disagree’ to ‘strongly agree’. Internal consistency (Cronbach’s coefficient alpha) for the five scales ranged from .75 (Openness) to .82 (Conscientiousness) in the current study. The prior use of the NEO-FFI in gerontology and geriatric psychiatry research attests to its reliability and applicability to samples of older adults (Hooker, Monahan, Bowman, Frazier, & Shifren, 1998; Hooker, Monahan, Shifren, & Hutchinson, 1992; Schmutte & Ryff, 1997). In this sample, Cronbach’s alphas were: Neuroticism, .81; Conscientiousness, .82; Openness, .71; Extraversion, .75; and Agreeableness, .77.
Medication non-adherence
Study medication pills (G. biloba or identical-appearing placebos) were prescribed twice daily, and provided to subjects in blister packs. Non-adherence was determined by pill counts conducted by the research assistant at each six monthly study follow-up assessment visit. The per cent of total pills prescribed that had been missed since the prior study follow-up visit was recorded.
Other measures
Cognitive function was measured with the Modified Mini-Mental State Examination (3MSE; Teng & Chui, 1987). Compared with the original Mini-Mental State Exam, the 3MSE incorporates four additional test items, offers more graded scoring (0–100 instead of 0–30, with higher scores indicating better function), and is more sensitive (Teng & Chui, 1987). Depressive symptoms were measured with the 10-item Centre for Epidemiologic Studies Depression Scale (CES-D), a well-validated measure commonly used with elderly samples (Irwin, Artin, & Oxman, 1999). Scores range from 0 to 30, with higher scores indicating more depressive symptoms. Cronbach’s alpha in this sample was .75. Subjects also provided other information at baseline, including age, gender, race/ethnicity, and education (years of schooling, coded as <12 years, 12 years, 13–15 years, 16 or more years); self-rated health (excellent, very good, good, fair, poor); health conditions (hypertension, heart attack, angina, heart failure, stroke, diabetes, cancer, osteoporosis); smoking status (never, former, current); BMI in kg/m2 (categorized as <18.5, 18.5 – <25, 25 – <30, and ≥30); and self-reported number of social visits per month, either in the subject’s own home or elsewhere (0, 1, 2, 3, 4, or 5 or more).
Analyses
Data were analysed using Stata (Version 11.0, StataCorp, College Station, Texas). Key non-adherence analyses were conducted using random effects logistic regression analyses adjusting for the nesting of repeated measurements on each participant, with non-adherence versus adherence at each visit as the dependent variable. The distribution of non-adherence scores was highly skewed, precluding use of mean non-adherence scores in analyses. Thus, at each study follow-up assessment, non-adherence was defined as missing more than 20% of prescribed pills. Although this threshold is commonly employed in research (Simoni et al., 2006), it is also somewhat arbitrary, since for most medications the level of adherence required for optimal treatment effects has not been characterized (DiMatteo et al., 2002). Thus, we conducted additional analyses employing non-adherence cut points of >10%, >30%, and >40% of pills missed. These analyses revealed similar findings to the main analyses and so are not reported here, but are available from the authors upon request.
We examined a series of hierarchically nested analytic models. All models adjusted for the exogenous variables visit number and treatment assignment. Model 1 included the five FFM personality factors, standardized to a mean of zero and a standard deviation of one to facilitate interpretation. Model 2 added fixed demographic variables (age, gender, and race/ethnicity [non-Hispanic White vs. other]) unlikely to be affected by personality. Model 3 added all remaining covariates that may be influenced by personality and affect non-adherence (Gellad et al., 2007; Molloy et al., 2008; Sayers et al., 2008; Vik et al., 2004). These baseline variables were education level (<12 years schooling, 12 years, 13–15 years, and ≥16 years); median zip code income (United States Census Bureau, 2000); smoking status (ever vs. never smoker); BMI category; disease burden (sum of self-identified diagnoses, as a summary measure of morbidity, and competing medication priorities); self-rated health, dichotomized as excellent or very good versus good, fair or poor; cognitive function (3MSE); depression score (CES-D); and number of social visits per month (less than two per month vs. more). To facilitate interpretation of the results of the logistic regression analyses, associations are presented as adjusted average marginal effects (AME). The AME is the average change in probability of non-adherence associated with a unit change in the predictor. We also conducted likelihood-ratio tests to examine the significance of the cluster of variables added to each model compared with the prior model; for Model 1, the test reflects the addition of the FFM personality variables to a model including only study group and study follow-up visit.
Sensitivity analyses examined the roles of co-morbid medical conditions, considered as dichotomous variables (present vs. absent); a categorical variable for each level of self-rated health; and number of social visits per month (0, 1, 2, 3, 4, or 5 or more). Analyses also examined interactions between personality factors and the other independent variables. Finally, to examine the possible impact of study drop-out (due to diagnosis of dementia, the study end-point; death; or refusal to continue participating), a Cox proportional hazards survival analysis was conducted with time to dropping out as the survival interval, and all the above described variables as predictors.
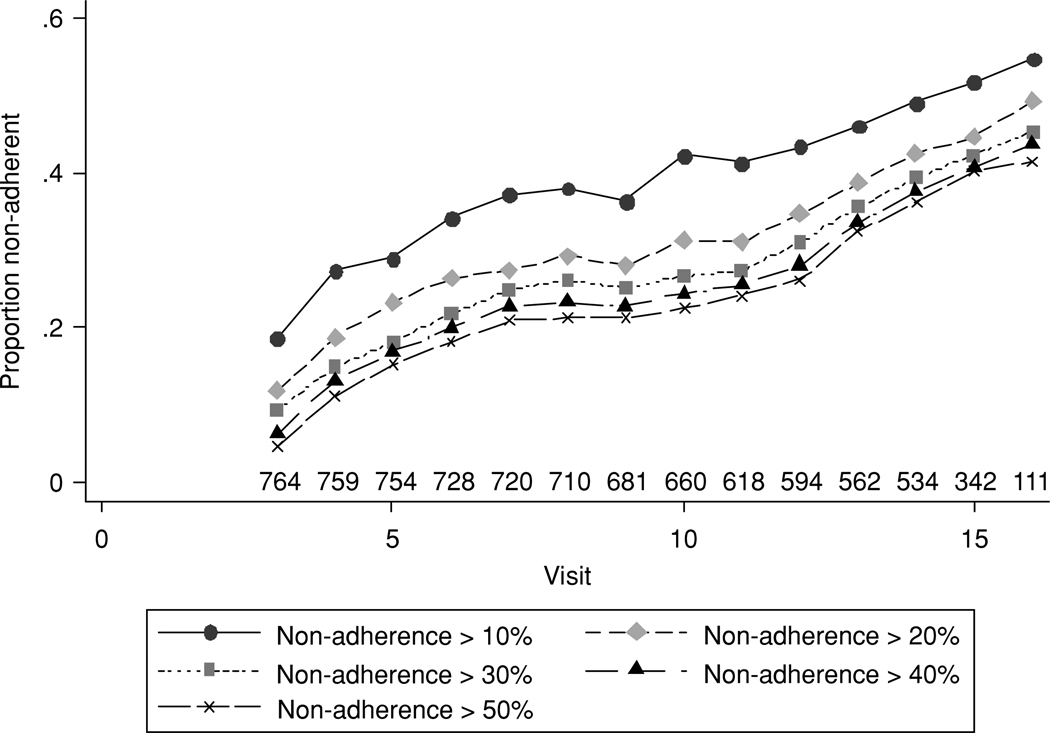
Results
Table 2 shows the characteristics of participants at baseline. The sample ranged in age from 72–91 years, and was predominantly non-Hispanic White and well educated. Overall, non-adherence (<80% of pills taken) was found at 26.5% of visits; 69.9% of participants were found to be non-adherent at one or more visits. Figure 2 shows that there was increasing medication non-adherence over time among study participants, with similar trajectories at various thresholds for defining non-adherence. Figure 2 also shows the number of participants at each visit, which declined over time, reflecting both early drop-outs and fewer possible follow-up visits for later recruits. Drop-outs were due to dementia, the study end-point (132); death (93); and refusal to continue participating (32). Cox survival analysis revealed that drop-outs were older (hazard ratio [HR] 1.12 per year, 95% confidence interval, CI [1.08, 1.16], p < .01) and had higher levels of Neuroticism (HR = 1.25 per 1 SD increase, 95% CI [1.09, 1.16], p < .01). There were no statistically significant differences between those assigned to Ginkgo or placebo on any of the variables assessed in the study.
Table 2.
Baseline characteristics of study sample
| Characteristic | Total (N = 771) |
|---|---|
| Age, years, mean (SD) | 78.6 (3.1) |
| Male (%) | 58.1 |
| Non-Hispanic White (%) | 91.8 |
| Zip code median income, $, mean (SD) | 47,622 (12,389) |
| Personality factors, mean (SD)a | |
| Neuroticism | 27.1 (6.3) |
| Conscientiousness | 44.6 (5.7) |
| Agreeableness | 46.4 (5.2) |
| Extraversion | 39.9 (5.4) |
| Openness | 41.5 (7.0) |
| Years of schooling (%) | |
| < 12 | 6.7 |
| 12 | 24.0 |
| 13–15 | 25.6 |
| ≥ 16 | 43.7 |
| Ever smoker (%) | 55.5 |
| BMI category (kg/m2) | |
| < 18.5 | 1.0 |
| 18.5–< 25 | 31.8 |
| 25–< 30 | 45.6 |
| ≥ 30 | 21.5 |
| Health conditions (%) | |
| Cardiovascularb | 25.8 |
| Diabetes | 8.0 |
| Hypertension | 54.1 |
| Cancer | 21.8 |
| Osteoporosis | 12.0 |
| Number of health conditions, mean (SD) | 1.6 (1.3) |
| Self-related health very good or excellent (%) | 51.8 |
| 3MSE score, mean (SD)c | 94.2 (4.4) |
| CES-D score, meatn (SD)d | 3.8 (3.6) |
| Social visists per month (%) | |
| 0 | 5.4 |
| 1 | 13.9 |
| 2 | 25.4 |
| 3 | 25.7 |
| 4 | 22.3 |
| ≥ 5 | 7.3 |
Note. BMI, body mass index; 3MSE, modified Mini-Mental State Examination; CES-D center for Epidemiology Studies Depression Scale.
Range of scores each factory 0–48.
Coronray heart disease, angina, stroke, transient ischemic attack, bypass surgery, or angioplasty.
Range of Scores 0–100.
Range of scores 0–30.
Figure 2.
Proportion of individuals non-adherent at each follow-up assessment, at various non-adherence thresholds.
Table 3 summarizes the results of the three random effects logistic regression analyses, showing the adjusted predictors of non-adherence as AMEs, expressed in percentages. Not shown, non-adherence increased significantly over time. In Model 1 (including only the FFM factors), the association of Neuroticism with non-adherence was significant, with a 1 SD increase in Neuroticism being associated with a 6.4% increase in non-adherence. In Model 2, which added the demographic variables, non-adherence was associated with increasing age, with a 6.7% increase in the probability of non-adherence observed for each 5 year increment in age (95% CI [2.4, 11.0]). There were no associations between non-adherence and gender or race/ethnicity, and the effect of Neuroticism was attenuated very little in this model.
Table 3.
Adjusted AME and 95% CIs of risk factors on medication non-adherencea
| Model 1 | Model 2 | Model 3 | ||||
|---|---|---|---|---|---|---|
| Variables | AME [95% CI] | p value | AME [95% CI] | p value | AME [95% CI] | p value |
| Personality factorsb | ||||||
| Neuroticism | 6.41 [3.41, 9.40] | <.01 | 5.82 [2.68, 8.97] | <.01 | 3.79 [0.39, 7.19] | .03 |
| Conscientiousness | −0.43 [−3.43, 2.57] | .78 | 0.05 [−2.92, 3.02] | .98 | −0.05 [−3.05, 2.95] | .98 |
| Agreeableness | 0.76 [−2.11, 3.63] | .61 | 0.30 [−2.72, 3.31] | .85 | 0.53 [−2.47, 3.54] | .73 |
| Extraversion | 1.37 [−1.64, 4.38] | .37 | 1.45 [−1.52, 4.42] | .34 | 2.17 [−0.87, 5.20] | .16 |
| Openness | 0.58 [−2.17, 3.34] | .68 | 0.63 [−2.12, 3.37] | .65 | 1.34 [−1.57, 4.24] | .37 |
| Age | − | − | 1.49 [0.64, 2.35] | <.01 | 1.34 [0.47, 2.21] | <.01 |
| Male | − | − | −1.41 [−7.09, 4.28] | .63 | −3.72 [−9.48, 2.04] | .21 |
| Non–Hispanic White | − | − | 2.06 [−7.55, 11.66] | .68 | 3.76 [−5.91, 13.43] | .45 |
| Years of schoolingc | ||||||
| 12 | − | − | − | − | −11.74 [−27.93, 4.45] | .16 |
| 13–15 | − | − | − | − | −4.22 [−21.53, 13.10] | .63 |
| ≥ 16 | − | − | − | − | −7.67 [−24.43, 9.08] | .37 |
| Median incomed | − | − | − | − | 0.05 [−0.16, 0.26] | .63 |
| Ever smoker | − | − | − | − | 2.48 [−3.21, 8.16] | .39 |
| BMI categorye | ||||||
| 18.5–< 25 | − | − | − | − | −25.21 [−52.08, 1.67] | .07 |
| 25–< 30 | − | − | − | − | −20.70 [−50.86, 9.46] | .18 |
| ≥ 30 | − | − | − | − | −19.78 [−51.00, 11.45] | .22 |
| Number of health conditions | − | − | − | − | −0.39 [−2.53, 1.76] | .72 |
| Self-related healthf | − | − | − | − | −9.27 [−14.28, −4.26] | <.01 |
| 3MSE | − | − | − | − | −0.68 [−1.32, −0.04] | .04 |
| CES-D | − | − | − | − | 0.78 [−0.07, 1.63] | .07 |
| < 2 social visits/month | − | − | − | − | 3.07 [−4.21, 10.35] | .41 |
Note. Model I included personality factors; Model 2 added age, gender, race/ethnicity; Model 3 added over other covariates; All analyses adjusted for follow-up visit number and study group assignment. AME, average marginal effects; CI, confidence interval; BMI, body mass index; 3 MSE, Modified Mini-Mental State Examination;
Non-adherence defined as missing > 20% of prescribed pills.
Scores for each factory were standardized (mean = 0, SD = 1)
Reference category < 12
$10,000 × Zip code median.
Reference category < 18.5 kg/m2.
Excellent or very good versus good, fair, or poor.
In Model 3, which added all remaining variables, the effect of Neuroticism was attenuated: a 1 SD increase in Neuroticism was associated with a 3.8% increase in the probability of non-adherence. Lower cognitive function was also associated with nonadherence, such that a 1 SD decrease in 3MSE score was associated with a 3.0% increase in the probability of non-adherence (95% CI [0.2, 5.9]). Lower self-rated health was also associated with non-adherence. Results of likelihood-ratio tests examining the significance of the cluster of variables added to each model compared with prior model were: Model 1, χ2(df = 5) = 19.08, p < .01; Model 2, χ2(df = 3) = 11.32, p = .01; and Model 3, χ2(df = 13) = 31.32, p < .01. There were no significant associations between non-adherence and number of health conditions, smoking, BMI, median income of residential zip code, education, or number of social visits per month.
Sensitivity analyses conducted to consider the effects of individual health conditions, using all categories of the self-reported health and social visit variables, limiting follow-up to <11 visits (which resulted in substantially less missing data) revealed consistent adjusted associations between Neuroticism and non-adherence. There were no significant interactions between any of the personality factors and the other independent variables.
Discussion
This study adds to the literature concerning the role of personality in predicting non-adherence, among older adults in particular. Confirming one of our hypotheses, we found a higher level of Neuroticism was a strong independent predictor of non-adherence in older adults enrolled in the GEM trial. A 1 SD increase in Neuroticism was associated with a fully adjusted 3.8% increase in the probability of non-adherence. This finding is consistent with research indicating that across multiple life domains, high Neuroticism is associated with a host of unfavourable behaviours and outcomes (Costa & McCrae, 1992; Roberts et al., 2007).
Of nine prior studies examining associations between Neuroticism and medication non-adherence, only one involved a sample of older adults similar to ours (Table 1). That study of community-dwelling individuals (mean age = 77; Insel, Reminger, & Hsiao, 2006) employed the six-factor model of personality, which splits Conscientiousness into two different factors (Industriousness and Methodicalness) and labels the Neuroticism factor as ‘Independence’ (Jackson, Paunonen, Fraboni, & Goffin, 1999). Mirroring our results, that study found that of the six factors, only a higher level of Independence (i.e., higher Neuroticism) was associated with non-adherence (Insel et al., 2006). However, the study had a much smaller sample size (N = 60) and much shorter follow-up period (8 weeks) than ours. It also did not adjust for known correlates of non-adherence our analyses adjusted for, including gender, race/ethnicity, income, smoking status, BMI category, disease burden, cognitive function, depressive symptoms, and social support.
Of the other eight studies exploring associations between Neuroticism and non-adherence, all involved much younger samples (Table 1), and two found high Neuroticism was associated with low adherence. While the reasons for these mixed findings remain unclear, differences among study samples in ages and other key characteristics, differences in personality measurement instruments, and other methodological issues are likely important.
We did not find support for the hypothesis that high Conscientiousness would be associated with lower medication non-adherence. This could, in part, be explained by the fact that our study enrolled relatively healthy subjects for a prevention trial involving an unproven ‘alternative’ preventative intervention. The six prior studies finding an association between Conscientiousness and non-adherence all enrolled younger and mostly less healthy participants than ours, and involved established medical approaches to treating manifest chronic conditions (Table 1). However, these prior studies were also cross-sectional, and failed to account for important correlates of non-adherence our analytic model included, which could also help to explain their different findings.
Finally, we found no significant associations between Agreeableness, Extraversion, and Openness and non-adherence. This was not surprising, since prior studies examining the role of these factors yielded little consistent evidence of such associations (Table 1).
While our study was not designed to elucidate the mechanisms underlying the association between higher levels of Neuroticism and non-adherence, several appear plausible. Regarding potential direct mechanisms, high Neuroticism individuals are more likely to experience anxiety and anger, often in response to situations and stimuli others would easily be able to cope with (Costa & McCrae, 1992). In this context, ordinary situations may become threatening, and minor frustrations may become painfully difficult. Even the relatively simple of task of taking two daily pills during a longitudinal clinical trial might trigger disproportionate frustration, leading to non-adherence. Individuals high in Neuroticism also have difficulty delaying gratification (Funder, Block, & Block, 1983). In the context of a longitudinal trial, this tendency could further contribute to non-adherence.
Neuroticism may also have indirect effects on non-adherence. Prior work suggests an association between tendency to experience psychological distress – a hallmark of high Neuroticism – and greater cognitive decline in old age (Wilson et al., 2005). Frustration and emotional rumination, to which high Neuroticism individuals are prone, can impede both immediate and long-term cognitive performance (Eysenck, 1992), and may have contributed to pill non-adherence. Thus, cognitive impairment may have at least partially mediated the relationship between Neuroticism and non-adherence. Comparison between Model 2 (which added fixed demographic variables) and Model 3 (which added cognitive function, depressive symptoms, and self-rated health) revealed some attenuation of the parameter estimate for Neuroticism. This finding is consistent with the possibility that the variables added in Model 3 may partially mediate the relationship between Neuroticism and non-adherence. Additional studies designed to permit formal mediation analyses are now required to further explore this possibility.
Our findings regarding Neuroticism and medication non-adherence have three main implications for clinicians and researchers. First, they suggest the potential utility of routinely measuring personality in both the clinical setting and in clinical research studies. Doing so in the clinical setting could help clinicians identify patients at higher than usual risk for medication non-adherence. In the clinical research setting, routine measurement of personality could aid more precise modelling of non-adherence, thereby improving the applicability of study findings to general practice. Valid, reasonably reliable, and brief (less than 5 minutes to administer) measures exist that might facilitate wider application of personality measurement (Benet-Martinez & John, 1998; Gustavsson, Jonsson, Linder, & Weinryb, 2003). Studies demonstrating the benefits of routine personality measurement in research studies and daily practice will be required before these approaches can be confidently recommended.
Second, our findings suggest the possibility of reducing medication non-adherence through interventions that address the potential mechanisms underlying the relationships between patient personality characteristics and non-adherence. For example, individuals with a high level of Neuroticism might be helped to adhere to medication if clinicians and study personnel were made aware of this personality factor standing and informed about the tendency of such individuals to become emotionally distressed or ‘dysfunctional’ in response to ostensibly innocuous stressors. Clinicians and study personnel might be trained to recognize early these signs of distress in response to taking long-term medication and related issues such as side-effects and costs, and taught to employ calming and reframing strategies with distress-prone individuals. A similar approach to identifying and training providers to work effectively with various personality profiles has been used successfully in the field of psychotherapy (Meyer & Deitsch, 1996). The potential (though as yet unproven) role of cognitive impairment in partially mediating the Neuroticism/non-adherence association (Wilson et al., 2005) suggests interventions to reduce the cognitive burden of medication taking, such as simplifying daily regimens, using pill organizing containers, and setting standing reminder alarms on wrist watches, might also help to reduce non-adherence in older adults with high levels of Neuroticism.
Beyond its potential utility in predicting and reducing medication non-adherence, increased application of personality measurement could benefit clinicians and researchers in a third important way. Currently, a large number of psychological and dispositional characteristics are studied as correlates of medication non-adherence, with little overlap in the correlates examined among studies. Since the FFM factors capture much of the inter-individual variation in these psychological characteristics, greater application of the model in non-adherence studies could go a long way towards unifying the currently diffuse literature in this field.
Strengths of our study included the longitudinal design featuring multiple follow-up assessments of adherence over a six-year period, a comprehensive multi-variable analytic model, and the use of a well-established model and measure of personality. Our study also had some limitations. Our study sample, though relatively large, was community-based and relatively healthy, so our findings may not be applicable to other groups. Subjects were also selected individuals enrolled in a prevention trial of an ‘alternative’ medication, G. biloba, which turned out to be no more effective than placebo. While the ‘negative’ results of the GEM study were fortuitous in one sense, precluding confounding effects of the study medication, our findings may not be applicable to different treatments and regimens. For example, the association between high Neuroticism and non-adherence might be weaker or even non-existent where relatively short, acute courses of medication are concerned, and/or for medications that have large and immediately noticeable beneficial effects rather than those used for prevention. Further studies examining associations between personality and non-adherence involving a wide array of patient samples, health issues, and medication types and regimens would be welcome.
Also, we used pill counts to determine medication non-adherence. While highly feasible and of proven utility, pill counts may not reflect actual pill taking, since patients may ‘pocket’ or throw away some doses, particularly prior to study data collection appointments (Berg & Arnsten, 2006). On the other hand, no gold standard measure of medication adherence or non-adherence exists (DiMatteo, 2004), and even the use of electronic pill cap monitoring has a number of practical drawbacks (Berg & Arnsten, 2006). The key point is that studies that replicate our general analytic approach while using different measures of non-adherence are now required to determine the robustness of our findings.
Finally, there were some missing participant follow-up data in the GEM study, due to death, diagnosis of dementia (the study end-point), and refusal to continue participating. We found drop-outs were older and had higher levels of Neuroticism. Missing data in randomized controlled trial (RCTs; and observational studies) do not occur at random but instead appear to be related to personality (Jerant, Chapman, Duberstein, & Franks, 2009). Personality factors, particularly Neuroticism, have been associated with death and study attrition due to worsening cognition in other studies (Roberts et al., 2007; Wilson et al., 2005). The expected net effect of these associations would be to bias our findings towards the null. Thus, we may have underestimated the strength of association between higher levels of Neuroticism and non-adherence.
In conclusion, higher levels of Neuroticism, one of the factors within the FFM of personality, appear to be associated with medication non-adherence in older adults. Wider application of brief personality measures in the clinical and clinical research settings might help to identify individuals at risk for medication non-adherence, could guide the development of effective personality-based interventions to minimize non-adherence, and could facilitate targeting of such interventions to those most in need. The scope of the problem of medication non-adherence is vast and associated with myriad detrimental health effects (DiMatteo et al., 2002). In this context, our findings suggest the public health impact of routinely measuring and accounting for patient personality in efforts to reduce medication non-adherence might be considerable.
Acknowledgements
We are indebted to Stephen Straus, MD, the late former director of NCCAM, who championed efforts to evaluate complementary and alternative therapies in rigorous scientific fashion. We gratefully acknowledge the contribution of Dr Willmar Schwabe GmbH & Co. KG, Karlsruhe, Germany, for their donation of the G. biloba tablets and identical placebos, in blister packs, for the study. We are also grateful to our volunteers, whose faithful participation in this longitudinal study made it possible.
This work was supported by the National Institute of Mental Health [T32MH073452 to P. D., K24MH072712 to P. D.]; NCCAM and the Office of Dietary Supplements [U01AT000162 to Steven DeKosky]; the National Institute on Aging, National Heart, Lung, and Blood Institute, the University of Pittsburgh Alzheimer’s Disease Research Center [P50AG05133 to Oscar Lopez]; the Roena Kulynych Center for Memory and Cognition Research; and the National Institute of Neurological Disorders and Stroke. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the NCCAM, or the National Institutes of Health.
Appendix
GEM study personnel
Project office
Richard L. Nahin, PhD, MPH, Barbara C. Sorkin, PhD, NCCAM.
Clinical centres
Michelle Carlson, PhD, Linda Fried, MD, MPH, Pat Crowley, MS, Claudia Kawas, MD, Paulo Chaves, MD, PhD, Sevil Yasar, MD, PhD, Patricia Smith, Joyce Chabot, John Hopkins University; John Robbins, MD, MHS, Katherine Gundling, MD, Sharene Theroux, CCRP, Lisa Pastore, CCRP, University of California-Davis; Lewis Kuller, MD, DrPH, Roberta Moyer, CMA, Cheryl Albig, CMA, University of Pittsburgh; Gregory Burke, MD, Steve Rapp, PhD, Dee Posey, Margie Lamb, RN, Wake Forest University School of Medicine.
Schwabe pharmaceuticals
Robert Hörr, MD, Joachim Herrmann, PhD.
Data coordinating centre
Richard A. Kronmal, PhD, Annette L. Fitzpatrick, PhD, Fumei Lin, PhD, Cam Solomon, PhD, Alice Arnold, PhD, University of Washington.
Cognitive diagnostic centre
Steven DeKosky, MD, Judith Saxton, PhD, Oscar Lopez, MD, Beth Snitz PhD, M. Ilyas Kamboh PhD, Diane Ives, MPH, Leslie Dunn, MPH, University of Pittsburgh.
Clinical coordinating centre
Curt Furberg, MD, PhD, Jeff Williamson, MD, MHS; Nancy Woolard, Kathryn Bender, PharmD, Susan Margitić, MS, Wake Forest University School of Medicine.
Central laboratory
Russell Tracy, PhD, Elaine Cornell, UVM, University of Vermont.
MRI reading centre
William Rothfus MD, Charles Lee MD, Rose Jarosz, University of Pittsburgh.
Data safety monitoring board
Richard Grimm, MD, PhD (Chair), University of Minnesota; Jonathan Berman, MD, PhD (Executive Secretary), NCCAM; Hannah Bradford, MAc, LAc, MBA, Carlo Calabrese, ND MPH, Bastyr University Research Institute; Rick Chappell, PhD, University of Wisconsin Medical School; Kathryn Connor, MD, Duke University Medical Center; Gail Geller, ScD, Johns Hopkins Medical Institute; Boris Iglewicz, PhD, Temple University; Richard S. Panush, MD, Department of Medicine Saint Barnabas Medical Center; Richard Shader, PhD, Tufts University.
References
- Axelsson M, Emilsson M, Brink E, Lundgren J, Toren K, Lotvall J. Personality, adherence, asthma control and health-related quality of life in young adult asthmatics. Respiratory Medicine. 2009;103(7):1033–1040. doi: 10.1016/j.rmed.2009.01.013. [DOI] [PubMed] [Google Scholar]
- Benet-Martinez V, John OP. Los Cinco Grandes across cultures and ethnic groups: Multitrait multimethod analyses of the Big Five in Spanish and English. Journal of Personality and Social Psychology. 1998 Jul;75(3):729–750. doi: 10.1037//0022-3514.75.3.729. [DOI] [PubMed] [Google Scholar]
- Berg KM, Arnsten JH. Practical and conceptual challenges in measuring antiretroviral adherence. Journal of Acquired Immune Deficiency Syndromes. Practical and conceptual challenges in measuring antiretroviral adherence;43 Suppl. 1:S79–S87. doi: 10.1097/01.qai.0000248337.97814.66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bogg T, Robert BW. Conscientiousness and health-related behaviors: A meta-analysis of the leading behavioral contributors to mortality. Psychological Bulletin. 2004;130((6):887–919. doi: 10.1037/0033-2909.130.6.887. [DOI] [PubMed] [Google Scholar]
- Briesache BA, Gurwitz JH, Soumerai SB. Patients at-risk for cost-related medication nonadherence: A review of the literature. Journal of General Internal Medicine. 2008;22(6):864–871. doi: 10.1007/s11606-007-0180-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chapman B, Duberstein P, Lyness JM. Personality traits, education and health-related quality of life among older adult primary care patients. Journals of Gerontology Series B: Psychological Sciences and Social Sciences. 2007;62(6):343–352. doi: 10.1093/geronb/62.6.p343. [DOI] [PubMed] [Google Scholar]
- Chia LR, Schlenk EA, QDunbar-Jacob J. Effect of personal and cultural beliefs on medication adherence in the elderly. Drugs and Aging. 2006;23(3):191–202. doi: 10.2165/00002512-200623030-00002. [DOI] [PubMed] [Google Scholar]
- Christensen AJ, Moran PJ, Wiebe JS. Assessment of irrational health beliefs: Relation to health practices and medical regimen adherence. Health Psychology. 1999;18(2):169–176. doi: 10.1037//0278-6133.18.2.169. [DOI] [PubMed] [Google Scholar]
- Christensen AJ, Smith TW. Personality and patient adherence: Correlates of the five-factor model in renal dialysis. Journal of Behavioral Medicine. 1995;18(3):305–313. doi: 10.1007/BF01857875. [DOI] [PubMed] [Google Scholar]
- Cohen NL, Ross EC, Bagby RM, Farvolden P, Kennedy SH. The 5-factor model of personality and antidepressant medication compliance. Canadian Journal of Psychiatry. 2004;49(2):106–113. doi: 10.1177/070674370404900205. [DOI] [PubMed] [Google Scholar]
- Conard MA, Matthews RA. Modeling the stress process: Personality eclipses dysfunctional cognitions and workload in predicting stress. Personality and Individual Differences. 2008;44(1):171–181. [Google Scholar]
- Costa PT, McCrae RR. Revised NEO personality inventory and NEO five factor inventory: Professional manual. Odessa, FL: Psychological Assessment; 1992. [Google Scholar]
- Costa PT, Jr, McCrae RR. Stability and change in personality assessment: The revised NEO Personality Inventory in the year 2000. Journal of Personality Assessment. 1997;68(1):94. doi: 10.1207/s15327752jpa6801_7. [DOI] [PubMed] [Google Scholar]
- Costa PT, Jr, Somerfield MR, McCrae RR. Personality and coping: A reconceptualization. In: Zeidner M, Endler NS, editors. Handbook of coping: Theory, research, applications. New York: Wiley; 1996. pp. 44–61. [Google Scholar]
- Curtis JR, Xi J, Westfall AO, Cheng H, Lyles K, Saag KG, Delzell E. Improving the prediction of medication compliance: The example of bisphosphonates for osteoporosis. Medical Care. 2009;47(3):334–341. doi: 10.1097/MLR.0b013e31818afa1c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeKosky ST, Fitzpatrick A, Ives DG, Saxton J, Williamson J, Lopez OL GEMS Investigators. The Ginkgo Evaluation of Memory (GEM) study: Design and baseline data of a randomized trial of Ginkgo biloba extract in prevention of dementia. Contemporary Clinical Trials. 2006;27(3):238–253. doi: 10.1016/j.cct.2006.02.007. [DOI] [PubMed] [Google Scholar]
- DeKosky ST, Williamson JD, Fitzpatrick AL, Kronmal RA, Ives DG, Saxton JA Ginkgo Evaluation of Memory (GEM) Study Investigators. Ginkgo biloba for prevention of dementia: A randomized controlled trial. Journal of the American Medical Association. 2008;300(19):2253–2262. doi: 10.1001/jama.2008.683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DiMatteo MR. Variations in patients’ adherence to medical recommendations: A quantitative review of 50 years of research. Medical Care. 2004;42(3):200–209. doi: 10.1097/01.mlr.0000114908.90348.f9. [DOI] [PubMed] [Google Scholar]
- DiMatteo MR, Giordani PJ, Lepper HS, Croghan TW. Patient adherence and medical treatment outcomes: A meta-analysis. Medical Care. 2002;40(9):794–811. doi: 10.1097/00005650-200209000-00009. [DOI] [PubMed] [Google Scholar]
- Dobbels F, Vanhaecke J, Desmyttere A, Dupont L, Nevens F, De Geest S. Prevalence and correlates of self-reported pretransplant nonadherence with medication in heart, liver, and lung transplant candidates. Transplantation. 2005;79(11):1588–1595. doi: 10.1097/01.tp.0000158430.06507.87. [DOI] [PubMed] [Google Scholar]
- Ediger JP, Walker JR, Graff L, Lix L, Clara I, Rawsthorne P, Bernstein CN. Predictors of medication adherence in inflammatory bowel disease. American Journal of Gastroenterology. 2007;102(7):1417–1426. doi: 10.1111/j.1572-0241.2007.01212.x. [DOI] [PubMed] [Google Scholar]
- Eysenck MW. Anxiety and performance: The processing efficiency theory. Cognition and Emotion. 1992;6(6):409–434. [Google Scholar]
- Fitzpatrick AL, Fried LP, Williamson J, Crowley P, Posey D, Kwong L GEMS Investigators. Recruitment of the elderly into a pharmacologic prevention trial: The Ginkgo Evaluation of Memory Study experience. Contemporary Clinical Trials. 2006;27(6):541–553. doi: 10.1016/j.cct.2006.06.007. [DOI] [PubMed] [Google Scholar]
- Friedman HS. Long-term relations of personality and health: Dynamisms, mechanisms, tropisms. Journal of Personality. 2000;68(6):1089–1107. doi: 10.1111/1467-6494.00127. [DOI] [PubMed] [Google Scholar]
- Funder DC, Block JH, Block J. Delay of gratification: Some longitudinal personality correlates. Journal of Personality and Social Psychology. 1983;44(6):1198–1213. [Google Scholar]
- Gellad WF, Haas JS, Safran DG. Race/ethnicity and nonadherence to prescription medications among seniors: Results of a national study. Journal of General Internal Medicine. 2007;22(11):1572–1578. doi: 10.1007/s11606-007-0385-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldberg LR. The structure of phenotypic personality traits. American Psychologist. (48) 1993;48(1):26–34. doi: 10.1037//0003-066x.48.1.26. [DOI] [PubMed] [Google Scholar]
- Gustavsson JP, Jonsson EG, Linder J, Weinryb RM. The HP5 inventory: Definition and assessment of five health-relevant personality traits from a five-factor model perspective. Personality and Individual Differences. 2003;2003(1):69–89. [Google Scholar]
- Hooker K, Monahan D, Shifren K, Hutchinson C. Mental and physical health of spouse caregivers: The role of personality. Psychology and Aging. 1992;7(3):367–375. doi: 10.1037//0882-7974.7.3.367. [DOI] [PubMed] [Google Scholar]
- Hooker K, Monahan DJ, Bowman SR, Frazier LD, Shifren K. Personality counts for a lot: Predictors of mental and physical health of spouse caregivers in two disease groups. Journals of Gerontology Series B: Psychological Sciences and Social Sciences. 1998;53(2):P73–P85. doi: 10.1093/geronb/53b.2.p73. [DOI] [PubMed] [Google Scholar]
- Insel KC, Reminger SL, Hsiao CP. The negative association of independent personality and medication adherence. Journal of Aging and Health. 2006;18(3):407–418. doi: 10.1177/0898264306286200. [DOI] [PubMed] [Google Scholar]
- Irwin M, Artin KH, Oxman MN. Screening for depression in the older adult: Criterion validity of the 10-item Center for Epidemiologic Studies Depression Scale (CES-D) Archives of Internal Medicine. 1999;159(15):1701–1704. doi: 10.1001/archinte.159.15.1701. [DOI] [PubMed] [Google Scholar]
- Jackson DN, Paunonen SV, Fraboni M, Goffin RD. A five-factor versus six-factor model of personality structure. Personality and Individual Differences. 1999;20(1):33–45. [Google Scholar]
- Jerant A, Chapman BP, Duberstein P, Franks P. Is personality a key predictor of missing study data? An analysis from a randomized controlled trial. Annals of Family Medicine. 2009;7(2):148–156. doi: 10.1370/afm.920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krueger RF, Caspi A, Moffitt TE. Epidemiological personology: The unifying role of personality in population-based research on problem behaviors. Journal of Personality. 2000;68(6):967–998. doi: 10.1111/1467-6494.00123. [DOI] [PubMed] [Google Scholar]
- Machlin S, Cohen J, Beauregard K. Health care expenses for adults with chronic conditions (AHRQ Statistical Brief #203) Rockville, MD: Agency for Healthcare Research and Quality; 2005. [Google Scholar]
- Marshall GN, Wortman CB, Vickers RR, Jr, Kusulas JW, Hervig LK. The five-factor model of personality as a framework for personality-health research. Journal of Personality and Social Psychology. 1994;67(2):278–286. doi: 10.1037//0022-3514.67.2.278. [DOI] [PubMed] [Google Scholar]
- McCrae RR, Costa PT., Jr Personality trait structure as a human universal. American Psychologist. 1997;52(5):509–516. doi: 10.1037//0003-066x.52.5.509. [DOI] [PubMed] [Google Scholar]
- Meyer RG, Deitsch SE. The clinician’s handbook: Integrated diagnostics, assessment, and intervention in adult and adolescent psychopathology. 4th ed. Needham Heights, MA: Simon & Schuster; 1996. [Google Scholar]
- Molloy GJ, Perkins-Porras L, Strike PC, Steptoe A. Social networks and partner stress as predictors of adherence tomedication, rehabilitation attendance, and quality of life following acute coronary syndrome. Health Psychology. 2008;27(1):52–58. doi: 10.1037/0278-6133.27.1.52. [DOI] [PubMed] [Google Scholar]
- O’Cleirigh C, Ironson G, Weiss A, Costa PT., Jr Conscientiousness predicts disease progression (CD4 number and viral load) in people living with HIV. Health Psychology. 2007;26(4):473–480. doi: 10.1037/0278-6133.26.4.473. [DOI] [PubMed] [Google Scholar]
- Penedo FJ, Gonzalez JS, Dahn JR, Antoni M, Malow R, Costa P, Schneiderman N. Personality, quality of life and HAART adherence among men and women living with HIV/AIDS. Journal of Psychosomatic Research. 2003;54(3):271–278. doi: 10.1016/s0022-3999(02)00482-8. [DOI] [PubMed] [Google Scholar]
- Roberts BW, Kuncel NR, Shiner R, Caspi A, Goldberg LR. The power of personality: The comparative validity of personality traits, socioeconomic status, and cognitive ability for predicting important life outcomes. Perspectives on Psychological Science. 2007;2(4):313–345. doi: 10.1111/j.1745-6916.2007.00047.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salas M, Kiefe CI, Schreiner PJ, Kim Y, Juarez L, Person SD, Dale Williams O. Obesity modifies the association of race/ethnicity with medication adherence in the CARDIA Study. Patient: Patient-Centered Outcomes Research. 2008;1(1):41–54. doi: 10.2165/01312067-200801010-00007. [DOI] [PubMed] [Google Scholar]
- Sayers SL, Riegel B, Pawlowski S, Coyne JC, Samaha FF. Social support and self-care of patients with heart failure. Annals of Behavioral Medicine. 2008;35(1):70–79. doi: 10.1007/s12160-007-9003-x. [DOI] [PubMed] [Google Scholar]
- Schmutte PS, Ryff CD. Personality and well-being: Reexamining methods and meanings. Journal of Personality and Social Psychology. 1997;73(3):549–559. doi: 10.1037//0022-3514.73.3.549. [DOI] [PubMed] [Google Scholar]
- Simoni JM, Kurth AE, Pearson CR, Pantalone DW, Merrill JO, Frick PA. Self-report measures of antiretroviral therapy adherence: A review with recommendations for HIV research and clinical management. AIDS and Behavior. 2006;10(3):227–245. doi: 10.1007/s10461-006-9078-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sörensen S, Duberstein PR, Chapman B, Lyness JM, Pinquart M. How are personality traits related to preparation for future care needs in older adults? Journal of Gerontology Series B: Psychological Sciences and Social Sciences. 2008;63(6):P328–P336. doi: 10.1093/geronb/63.6.p328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stilley CS, Sereika S, Muldoon MF, Ryan CM, Dunbar-Jacob J. Psychological and cognitive function: Predictors of adherence with cholesterol lowering treatment. Annals of Behavioral Medicine. 2004;27(2):117–124. doi: 10.1207/s15324796abm2702_6. [DOI] [PubMed] [Google Scholar]
- Teng EL, Chui HC. The Modified Mini-Mental State (3MS) examination. Journal of Clinical Psychiatry. 1987;48(8):314–318. [PubMed] [Google Scholar]
- United States Census Bureau. United States Census 2000. 2000 Retrieved from http://www.census.gov/main/www/cen2000.html.
- Vik SA, Hogan DB, Patten SB, Johnson JA, Romonko-Slack L, Maxwell CJ. Medication nonadherence and subsequent risk of hospitalisation and mortality among older adults. Drugs and Aging. 2000;23(4):345–356. doi: 10.2165/00002512-200623040-00007. [DOI] [PubMed] [Google Scholar]
- Vik SA, Maxwell CJ, Hogan DB. Measurement, correlates, and health outcomes of medication adherence among seniors. Annals of Pharmacotherapy. 2004;38(2):303–312. doi: 10.1345/aph.1D252. [DOI] [PubMed] [Google Scholar]
- Watson D, Hubbard B. Adaptational style and dispositional structure: Coping in the context of the five-factor model. Journal of Personality. 1996;64(4):737–774. [Google Scholar]
- Wilson RS, Bennett DA, Mendes de Leon CF, Bienias JL, Morris MC, Evans DA. Distress proneness and cognitive decline in a population of older persons. Psychoneuroendocrinology. 2005;30(1):11–17. doi: 10.1016/j.psyneuen.2004.04.005. [DOI] [PubMed] [Google Scholar]