Abstract
Background
The risk of noncontact ACL injury reportedly is increased in patients with a greater posterior tibial slope (PTS), but clinical data are inconsistent. It is unclear whether the medial and lateral PTSs have a different impact on this connection. It also is unknown whether the meniscal slope (MS) is associated with ACL injury.
Patients/methods
Using MRI, we compared the medial and lateral PTSs and MSs separately in 55 matched pairs of patients with isolated noncontact ACL injuries and a control group.
Results
Neither the PTS nor the relative difference between the medial and lateral PTSs differed between groups. In contrast, the lateral MS was greater with ACL injuries: 2.0° versus −2.7° in males with and without ACL injury and 1.7° versus −0.9 in females. Uninjured females had a greater PTS than males: 4.9° versus 3.0° in females and males medially, respectively; 5.7° versus 4.0° lateral.
Conclusions
There is no obvious link between the medial or lateral PTSs and ACL injury, and there is no obvious link between the relative difference in the medial and lateral PTSs and noncontact ACL injury. However, a greater lateral MS may indicate a greater risk of injury. The PTS can differ between the genders but the average difference is small.
Level of Evidence
Level II, prognostic study. See the Guidelines for Authors for a complete description of levels of evidence.
Introduction
The PTS of the bony tibial plateaus frequently is mentioned for its association to noncontact ACL injury [3, 18, 40, 45]. It is defined by a tangent line to the respective tibial plateau and a line perpendicular to the longitudinal axis (LA) of the tibial bone that averages 10° (± 3°) on radiographs [9, 13, 16, 19]. The measure reportedly influences knee kinematics [1, 17] and ligament function [41, 42, 44]. Dejour and Bonnin reported for every 10° increase in PTS there is an anterior tibial shift of 6 mm in a monopedal stance test [13]. An experimental PTS increase (5°–20°) resulted in anterior (2.1 mm–4.6 mm) and superior (1.6 mm–4.1 mm) translation of the tibial plateau with respect to the femoral condyles [1]. Some authors presumed that with greater translation greater ligament loading occurred and placed the ACL at greater risk with an increased PTS [13, 17, 44]. Thus, noncontact ACL injury was associated with a greater PTS, but published data are contradictory [8, 17, 35, 41, 42, 44, 46, 47]. Although there was no ACL tension increase in a biomechanical study [17], computer model data [41, 42] support a positive association between ACL tension and a greater PTS. There is incongruity between five clinical studies [8, 21, 35, 46, 47] that concluded a greater risk for noncontact ACL injury in patients with increased PTSs (Table 1). The relationship to injury either was stated only for the lateral plateau [46] or only for females [47]. Another study reported an association for the PTS in males but it was missing for the female’s lateral PTS [21]. One of these studies found no association [35]. Some of the incongruity might result from a mismatch in patient selection and how noncontact ACL injury was defined. Another reason, which we suppose is even more important, is the diversity of measurement methods. All of the referenced data were assessed using different methods. The medial and lateral PTSs in an individual are not necessarily similar, and the variability among individuals is high [19, 25, 26, 46]. The greater the variability of a parameter within a population, the broader will be the range of the observed data. With different methods used to assess an already variable parameter the natural variance is additionally intensified. When assessed on a lateral radiograph, a high-degree measurement error can exacerbate the variability [16, 26]. It remains unclear whether noncontact ACL injury is a result of a greater medial PTS, lateral PTS, or both [6, 39, 43]. Regardless of which plateau is associated with an injury risk, the menisci play a role in AP knee stability and may modify this stability when injured or resected [25, 36]. Analogous to the PTS, the MS is the angle between a tangent line between the superior meniscosynovial border of the respective meniscus and the LA [25]. The posterior meniscal horn is thicker than the anterior meniscal horn; therefore, the effect of the bony PTS could decrease with a lesser MS or, vice versa, increase with a greater MS [25, 28, 29]. We suppose that a greater MS reduces AP knee stability analogous to a resection or injury of the posterior meniscus. It is unclear whether an injury risk resulting from a greater PTS is modified by the MS. Two recent studies [20, 47] link a greater PTS to noncontact ACL injury in women, who reportedly are at a greater risk for such injury than men [18]. These data suggest gender-specific assessments of the PTS and MS would be important. We presume patients with injured ACLs have a greater PTS and MS and a greater difference in PTS between the medial and lateral plateaus when compared with the control group. The purpose of this study was to address whether the PTS and MS are associated with the risk for noncontact ACL injury. A better knowledge of these parameters with respect to the risk for injury can help to better address surgical issues including preparation and aftercare in ACL surgery. The data can help to better understand knee biomechanics and particularly the mechanisms leading to ACL injury.
Table 1.
Review of studies comparing the PTS in patients with noncontact ACL injury and a control group
| Study/(imaging method) | Mean with ± standard deviation or (range), significance level for each comparison of ACL injured and control group patients | |||||
|---|---|---|---|---|---|---|
| PTS medial | PTS lateral | |||||
| ACL injury | Control | Significance level | ACL injury | Control | Significance level | |
| Meister et al. [35] 1998 (LR) | N = 49 9.7° ± 1.8° |
N = 39 9.9 ± 2.1° |
p = 0.67 | na | na | |
| Brandon et al. [8] 2006 (LR) | N = 100 11.2 ± 3.8° |
N = 100 8.5 ± 3.0° |
p < 0.001 | na | na | |
| Stijak et al. [46] 2008 (LR + MRI) | N = 33 5.2 ± 3.6 |
N = 33 6.6 ± 3.2 |
p = 0.066 | N = 33 7.5 ± 3.4 |
N = 33 4.4 ± 2.3 |
p < 0.001 |
| Todd et al. [47] 2010 (LR) | N = 149 9.4 ± 2.7° |
N = 179 8.5 ± 2.6° |
p = 0.003 | na | na | |
| Hashemi et al. [21] 2010 (MRI) | N = 49 6° (−2–14°) |
N = 55 5° (−3–10°) |
p = 0.01 | N = 49 9° (0–12°) |
N = 55 6° (0–14°) |
p = 0.005 |
| Current study (MRI) | N = 55 4.7° ± 2.7 |
N = 55 4.1 ± 2.8 |
p = 0.257 | N = 55 5.6 ± 2.9 |
N = 55 4.9 ± 3.2 |
p = 0.292 |
LR = lateral radiograph, na = not assessed.
We asked whether (1) the medial PTS, the lateral PTS, or both, or the relative difference between the medial and lateral PTS are associated with noncontact ACL injury, (2) the MS is associated with the injury, and (3) gender plays a role in whether the PTS or MS promotes the injury.
Patients and Methods
We retrospectively reviewed the MRIs of all 55 patients (31 women, age 36 ± 12 years; 24 men, age 32 ± 9 years) with noncontact, isolated injuries of the ACL with intact menisci confirmed on MRI, seen from May 2002 until February 2007. Patients with ACL injuries were recruited when injury occurred without opponent contact. Most of the patients (66%) were injured during skiing. Twenty-six percent were injured during pivoting sports (football, handball). The others were injured during other activities (eg, dancing). All patients were weightbearing during the activity. However, most patients could not remember the exact mechanism of injury and the extent of weight which was on the leg during injury. The control group consisted of 55 patients with anterior knee pain diagnosed with patellofemoral pain syndrome (PFPS) for whom MRI was completely normal (31 women, age 37.0 ± 11 years; 24 men, 32 ± 8 years). Classification criteria for PFPS were adapted from those reported by Witvrouw et al. [50]. The groups were matched for age, gender, and site of injury. When patients from the control group had PFPS in both knees, the respective site was chosen to match the site from the injured patient. Patients with implants, fractures, and tumors were excluded from further investigation.
An a priori sample size power analysis was conducted based on the data from a prior study on the method for PTS measurement technique on MRI [23]. A sample size of 54 individuals for both groups was calculated to detect a 1.5° difference with a power of 0.94 at an α-error of 0.05. The targeted primary outcome variable was set to 1.5° because PTS differences reported in the literature range from 0.9°–3.4° [8, 46, 47]. The typical errors for interobserver and intraobserver variability related to the method used herein are 1.4° and 1.2°, respectively [23].
Although lateral radiographs are better to assess the medial PTS, they are inadequate for reliable and separate PTS and MS assessment. Therefore, we used conventional MRI scans of the knee, because they allow simple assessment of each plateau separately and provide the possibility to assess the MS reliably following a newly described method [23]. MRI scans were obtained on a 1.5 Tesla MRI scanner (Symphony, Siemens Medical Solutions, Erlangen, Germany) using the following parameters: T1, coronal plane, slice thickness: 3 mm for 170 × 138 mm, TE: 14–16 ms, TR: 450 ms; intermediate weighted sagittal plane, slice thickness: 3 mm for 180 × 143 mm, TE: 15, TR: 2700). The MRI slices were set manually by the radiologist, orthogonal to a line connecting the posterior femoral condyles.
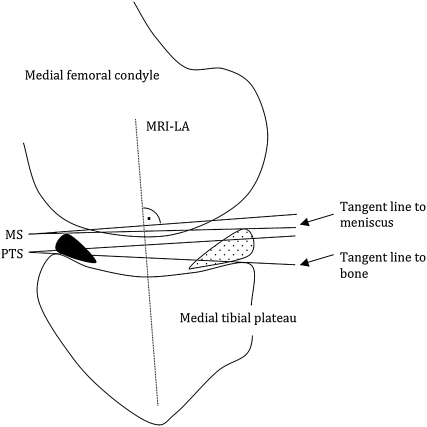
One of us (RH) made all measurements on the MRI as previously described [23]. In this previous study, the reliability of the measure was described with the typical error (TE) suggested by Hopkins [22]. That error is closely related to the limits of agreement suggested by Bland and Altman [5], accepted as a method to assess the reliability of a measurement. The advantage of the TE is its simple conversion to a variance and its self-explanatory appearance because it shows the variation in the values of repeated measurements. The intraobserver and interobserver TEs were 1.2° (confidence interval (CI), 1.2°–1.6°) and 1.4° (CI, 1.1°–1.4°), respectively [23]. All images were retrieved from our PACS system. Circles were applied digitally with computer software (Pro Vision Web 4.1.0; Cerner Corporation, Kansas City, MO, USA), which provided an infinite number of diameters and free positioning. All measurements were positioned as an overlay and remained in a fixed position on the complete image series. The MS was defined in the same manner as the PTS. A tangent to the superior edge of the meniscosynovial border of the anterior and posterior meniscus on the sagittal plane was chosen instead of the tibial plateau cortices (Fig. 1).
Fig. 1.
A diagram of the scheme for assessment of the PTS and MS on MRI is shown. The image shows the contours of a sagittal MR image at the mediolateral center of the medial plateau. A tangent line is drawn to the most superior anterior and posterior cortex edges of the medial bony plateau. Accordingly, the superior anterior and posterior meniscal borders mark the MS. The same procedure is performed for the lateral plateau. The MRI-LA is defined by the connection of two circles positioned in the proximal tibia as described previously [23].
The average PTS and MS angles are reported as mean angles with upper and lower 95% CIs. A normal distribution of data was tested graphically and confirmed using the Shapiro-Wilk W-test. An independent Student t-test was performed to test whether the PTS and MS differed between groups. Men and women were analyzed separately. A logistic regression analysis was performed to test whether ACL injury depended on the relative PTS difference between the medial and lateral PTSs. Data analysis was conducted in October 2007. We used JMP v 6.0.0 (SAS Institute, Cary, NC, USA) for our analyses and G*Power v 3.0.8 [14] (Heinrich-Heine University, Düsseldorf, Germany) for power analysis.
Results
The medial and lateral PTSs were similar (medial, p = 0.2569, lateral, p = 0.2924) in patients with isolated noncontact ACL injury and the control group (Table 2).
Table 2.
Medial and lateral PTS and MS of patients with ACL injury and the control group
| PTS and MS on MRI | Control (n = 55) | Noncontact ACL injury (n = 55) | ||
|---|---|---|---|---|
| Medial plateau | Lateral plateau | Medial plateau | Lateral plateau | |
| PTS | 4.1° (3.5°, 4.8°) | 4.9° (4.1°, 5.8°) *p = 0.0514 |
4.7° (3.9°, 5.4°) | 5.6° (4.7°, 6.4°) *p = 0.0173 |
| Men | 3.0° (1.9°, 4.2°) | 4.0° (2.7°, 5.3°) | 4.3° (3.1°, 5.5°) | 5.3° (4.2°, 6.4°) †p = 0.0872 |
| Women | 4.9° (4.0°, 5.8°) ‡p = 0.0145 |
5.7° (4.5°, 6.9°) ‡p = 0.0515 |
5.0° (4.0°, 5.7°) | 5.7° (4.6°, 6.9°) |
| MS | 0.1° (−0.7°, 0.9°) | −1.7° (−2.7°, −0.6°) *p = 0.0024 |
1.3° (0.5°, 2.1°) | 1.8° (0.8°, 2.8°) †p < 0.0001 |
| Men | −1.6° (−2.8°, −0.5°) | −2.7° (−4.2°, −1.2°) | 0.7° (−0.4, 1.9°) †p = 0.0047 |
2.0° (0.5°, 3.5°) †p < 0.0001 |
| Women | 1.4° (0.5°, 2.4°) ‡p = 0.0001 |
−0.9° (−2.4°, 0.6°) *p = 0.0030 |
1.7° (0.8°, 2.7°) | 1.7° (0.2°, 3.2°) †p = 0.0177 |
PTS = posterior tibial slope; MS = meniscal slope; the numbers in parenthesis represent the 95% confidence interval; * = significantly different from medial; ‡ = significantly different from men’ † = significantly different from control group.
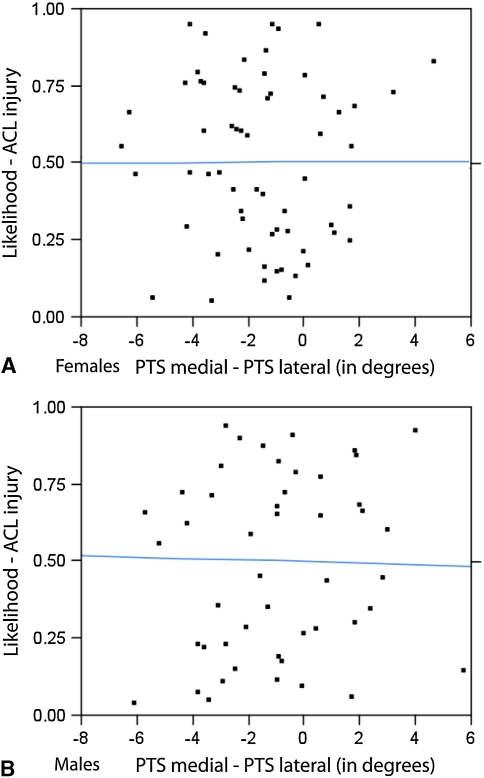
The lateral PTS was similar to the medial PTS in all groups (men with ACL injury, p = 0.08, control, p = 0.09; women with ACL injury, p = 0.11, control, p = 0.23) (Table 2). The difference between the medial and lateral PTSs ranged from −7.2° to +5.7° (mean, −0.8° ± 2.7°) in patients with ACL injury and −7.9 to +8.1° (mean, −0.8° ± 3.2°) in the control group. The relative difference between the medial and lateral PTSs was not associated with ACL injury (women, p = 0.99; men, p = 0.93) (Fig. 2).
Fig. 2A–B.
Logistic regression plots for (A) women and (B) men show the likelihood of ACL injury on the left ordinate, relative to the difference between the medial and lateral PTSs shown on the x-axis. Data points of all matched pairs of patients are plotted. The central line is the calculated logistic regression line, which remains approximately at 0.5 over the whole range of differences on the x-axis. ACL injury was not associated with the relative difference between the medial and lateral PTSs in women (p = 0.99) or in men (p = 0.93).
The lateral MS was greater (men, +4.7°; women, +2.8°; p < 0.001) in all patients with ACL injuries compared with the control group (Table 2). The differences between the medial and lateral MSs ranged from −6.1° to +6.6° (mean, −0.5° ± 3.6°) in injured patients and −5.9° to +11.2° (mean, 1.8° ± 4.1°) in the control group.
Men and women with ACL injuries had no greater medial and lateral PTSs when compared to those in the control group (medial PTS, p = 0.12; lateral PTS, p = 0.08). In contrast to men, there were only small PTS differences (less than 1.0°) between women in the injured and control groups. Women had a greater PTS and MS than men on the medial plateau in the control group (women’s medial PTS/MS, 4.9°/1.4° versus men’s, 3.0°/−1.6°, p = 0.0145/0.0001; women’s lateral PTS/MS, 5.7°/−0.9° versus men’s, 4.0°/−2.7°, p = 0.0515/0.1257) (Table 2).
Discussion
Some authors have suggested the risk for noncontact ACL injury increases with a greater PTS [4, 8, 13, 35, 46]. However, the data are conflicting, perhaps owing to high interindividual tibial plateau variability [19, 23–25, 46] and imprecise measurement methods on lateral radiographs [26]. Rotation of the tibial shaft in the xray beam may evoke an error of as much as 14° and even at the ideal true lateral position an error greater than 5° has been observed [26]. It is unclear whether the MS [25] and gender differences [47] modify the kinematic effect of the PTS and affect the risk for ACL injury. To better address whether the PTS is associated with ACL injury, it is important to separately identify the differences between the medial and lateral tibial plateaus, and to use a reproducible method. Both of these may be achieved with conventional MRI with sufficient reproducibility [23]. We asked whether (1) the medial PTS, the lateral PTS, both, or the relative difference between the medial and lateral PTSs are associated with noncontact ACL injury, (2) the MS is associated with the injury, and (3) gender plays a role in whether the PTS or MS promotes the injury.
We note limitations to our study. First, menisci are mobile when the knee performs full ROM under body weight [7, 48]. To mitigate this concern, we obtained MRI scans with patients relaxed, supine, and with the knee in extension. In this position, meniscal protrusion, which is the protrusion of any part of the meniscus beyond the tibial plateau, is presumed to be eliminated as it primarily occurs under full body weight and full ROM [7]. To further address this issue, dynamic meniscal monitoring is required, which is difficult in vivo under loading conditions. Even the imaging position for a patient standing upright in an open MR scanner does not entirely reflect normal weightbearing conditions [30, 32]. The posterior meniscal horn may be pushed posterior on the tibial plateau owing to anterior subluxation of the tibia after ACL rupture [30–32]. Therefore, a different MS can be interpreted as a result of the injury rather than a risk factor. We suppose this effect would be low because no differences in meniscotibial translation apparently occur between ACL injured and healthy knees at different flexion angles and muscle activity [49]. There was no radial expansion of the menisci observed until 1000 N axial joint compression [10]. Second, our control group consisted of patients with PFPS. We cannot exclude the possibility the pain has directly or indirectly been generated by an abnormal PTS instead of a disorder associated with PFPS. However, we could not obtain MRI scans of asymptomatic, normal knees. We do suspect the PTS/MS would have no bearing on PFPS. Third, injured patients were selected when opponent contact was not present. Most patients had a skiing injury. However, the patients were not able to exactly remember the mechanism of injury or to what extent they were weightbearing. This information is difficult to obtain in a complex environmental setting in which injury usually occurs [2, 18]. Fourth, patients were not matched for height, weight, and frequency of physical activity which placed them at risk for ACL injury. These variables may be confounding to our data. It has been postulated that an increased body mass index would result in a more extended lower extremity position with decreased knee flexion on landing [18]. However, the relative mass which is calculated from weight and height was not concluded as a risk factor in a literature review of articles from 1985 to 2008 [2].
We found that neither the medial and lateral PTSs, nor the relative difference between the medial and lateral PTSs, were different between patients with noncontact ACL injury when compared with the control group. Meister et al. [35], who studied the medial PTS on radiographs, also found no association to ACL injury. In contrast, Brandon et al. [8] and Todd et al. [47] reported injured patients to have +2.7° and +0.9° greater medial PTSs than a control group with patellofemoral pain, respectively. It is of primary importance to establish a robust tibial LA because each following measure will depend on this axis [9]. Brandon et al. [8], however, modified the standard technique described by Dejour and Bonnin [13] and used 5 cm instead of 10 cm interspace between the two points needed to determine the LA, which may have led to a greater variability. The difference reported by Todd et al. [47] is very small and we question whether 0.9° is reproducibly assessable. The interobserver and intraobserver variability for lateral radiographs were described with typical errors of 1.0° and 0.9° for the medial plateau, respectively [23]. We question whether such a small difference is relevant regarding the broad range of PTS variability reported in the literature [8, 11, 12, 20, 25, 26, 34, 35, 46, 47], particularly regarding the fact that Todd et al. found only females to have different values from the control group [47]. Although some studies relied on the use of the medial PTS, Stijak et al. [46] focused on the lateral PTS and reported only a greater lateral PTS promotes injury. However, they also found a greater medial PTS in the control group versus the injured group which contradicts the data of three other studies [8, 21, 47]. Stijak et al. [46] hypothesized that, under normal loading conditions, patients with a greater lateral PTS may have greater internal rotations of the lower leg. The resulting internal rotation stresses the ACL and may increase the injury risk [27]. Although patients with ACL injuries had no PTS difference when compared with the control group, we cannot refute the hypothesis of Stijak et al. [46], who concluded that a greater lateral PTS may put greater stress on the ACL. This is consistent with the trend for a greater lateral PTS in men with ACL injuries in our series. However, it is unclear why such a difference was not observed among women. A similar inconsistency was reported by Hashemi et al., in which the male’s medial PTS was associated with injury but not the female’s [21]. They also observed an increased medial tibial plateau depth in conjunction with an increased PTS in patients with noncontact ACL injuries and concluded an increased medial plateau depth as an important risk factor (odds ratio, 3.03), followed by the medial (odds ratio, 1.18) and lateral (odds ratio, 1.17) PTSs [21]. However, the differences between the injured patients and the control group were 1.5° for both plateaus and 0.9° for the medial plateau depth [21]. We do not share their conclusion. The reported average differences found on MRI were too small to satisfy the criteria of a relevant and evident difference with respect to the standard deviations and disparity of data reported in the literature.
We suspect some of the apparent conflict in the literature arises from imprecise measurement techniques. Some variability likely reflects the variability of the various methods used to assess the PTS. However, sufficient reproducibility and a high resolution are necessary to appropriately detect even small differences. Stijak et al. [46] used MRI to assess the medial and lateral PTSs separately, but the tibial longitudinal axis was obtained on a separate radiograph of the same knee and transferred manually on a foil to the respective MR image series. We have several concerns regarding the reproducibility reported by Hashemi et al. [20]. First, the intraobserver variability measures were conducted on only 15 subjects. They provided no information regarding the interobserver variation. The intraclass correlation coefficient between independent measures was reportedly 0.88. However, the intraclass correlation coefficient was not independently documented for each variable and it was not stated which intraclass coefficient was used [20]. The use of correlation coefficients is a sensitive subject in comparative statistics because choosing a different coefficient may result in different values for the same data set, even under the same sampling theory [37]. We suppose the “limits of agreement” suggested by Bland and Altman [5] or the “typical error” suggested by Hopkins [22] are more appropriate to display the variance of a measure. The longitudinal reference axis on the tibial bone has been described by two points approximately 4 to 5 cm apart in the middle of the sagittal orientation of the bone and the description of landmarks is insufficient. We believe [23] that 1 cm distance between these two points and imprecise definition of cortical landmarks (inner or outer cortical border) expose this axis to great variation. Also, the joint position on the MR image window was not defined. With a differently imaged length of the tibial bone the reference points vary regarding the bone. We question whether the longitudinal axis is reproducible with sufficient reliability on subsequent images.
With increasing relative difference between the medial and lateral PTSs the likelihood for ACL injury did not increase (Fig. 2). The suggestion that a greater relative difference between the medial and lateral PTSs gains rotational moment for the lower limb and stresses the ACL [27, 33] cannot be supported with our data.
In contrast to the PTS, patients with ACL injury had a greater lateral MS. Jenny et al. [25] presumed the kinematic effects of the PTS may be compromised by the menisci and stated that the MS may better reflect knee kinematics and AP stability in terms of an anatomic variable than the PTS. The menisci resist against sagittal forces and guarantee a certain stability with a function similar to the ACL [36]. As the posterior meniscal horn is thicker than the anterior, the MS is almost perpendicular to the tibial longitudinal axis and may counteract the posterior inclination of the PTS [25]. The posterior meniscal horn acts like a wedge between the posterior femoral condyle and the posterior tibial plateau [36]. When this posterior wedge is decreased relative to the anterior, the MS increases and the AP excursion of the femoral condyle may gain, in respect to the tibial plateau, and stress the ACL. We observed a greater lateral MS (+ 3.5°; p < 0.0001) in the patients with ACL injuries, which leads to the suggestion that a greater lateral MS is associated with a greater risk for noncontact ACL injury. In contrast, the pooled medial MS was not greater in the injured patients which is consistent with biomechanical data [38]. The lateral meniscus is reportedly a more important restraint to anterior tibial translation than the medial meniscus [38]. We hypothesize the lateral meniscus is a relevant variable in the injury mechanism. A decreased MS may represent a restraint to tibial AP translation whereas an increased MS may increase the injury risk. Therefore, in ACL surgery it may be beneficial to preserve particularly the lateral meniscus or to reconstruct it to improve sagittal stability and prevent the progression of osteoarthritis. However, better detection of the MS under in vivo conditions is required to better address this issue.
We found uninjured women had a greater PTS and MS than men. There is conflict with respect to the literature regarding this point. Two in vitro studies [12, 51] on 105 and 31 subjects and two radiographic studies [8, 47] found no differences for the PTS between the genders, respectively. Although Todd et al. [47] reported only women with ACL injuries, and not men with injuries, had a greater PTS (+1.6°), a direct comparison revealed the PTS to be similar between the genders. In contrast, Hashemi et al. [20] reported females to have + 2.2° greater medial and + 1.6° greater lateral PTSs than males. These data reflect our findings in which females had +1.9° and +1.7° more PTSs, respectively. We may speculate that the custom-made devices used in the in vitro studies or the lateral radiographs may have been insufficient to detect the differences seen on MRI. On radiographs only the medial PTS is sufficiently assessed [13] whereas MRI provides data for both PTS plateaus [20, 23]. Neither Hashemi et al. [21] nor we found any gender difference of any of the measured variables between the injured patients. One may ask why there is a gender difference only in the control group? Hashemi et al. suggested both genders may share the same “high-risk tibial geometry” and concluded there is an increased prevalence for an increased PTS in a female population [20, 21]. We disagree with this because we observed similar PTSs between the injured patients and the control group. When a female population has an increased prevalence for a greater PTS, as stated by Hashemi et al. [20], the difference should appear in injured patients and in control subjects. This was not the case in their [21] observation or in ours. There is no obvious reason why both studies observed a gender difference only in uninjured subjects. Their inclusion criteria were similar to those in our study but they did not state the conditions of the visit and how the subjects in the control group were recruited. Therefore, we may not exclude confounding through patients with PFPS. Although we speculate a patellofemoral disorder is unlikely to be associated with a greater PTS [50], this finding needs further study, particularly regarding the much greater incidence of PFPS in females [15].
We found no evidence that the PTS is associated with noncontact ACL injuries. In contrast, a greater lateral MS may act as an anatomic risk factor. To better address this issue, in vivo testing is needed. The average gender differences were small and may not represent a clinically relevant observation with respect to the variability and inconsistency to published data.
Acknowledgments
We thank the Department of Radiology from the University Hospital Balgrist and particularly Prof. C. Pfirrmann for continuous support and image allocation. The corresponding author thanks Eliza Kennedy for proof reading and her support in english writing.
Footnotes
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his or her institution has approved or waived approval for the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
This work was performed at the Balgrist University Hospital, University of Zurich, Zurich, Switzerland.
References
- 1.Agneskirchner JD, Hurschler C, Stukenborg-Colsman C, Imhoff AB, Lobenhoffer P. Effect of high tibial flexion osteotomy on cartilage pressure and joint kinematics: a biomechanical study in human cadaveric knees. Winner of the AGA-DonJoy Award 2004. Arch Orthop Trauma Surg. 2004;124:575–584. doi: 10.1007/s00402-004-0728-8. [DOI] [PubMed] [Google Scholar]
- 2.Alentorn-Geli E, Myer GD, Silvers HJ, Samitier G, Romero D, Lazaro-Haro C, Cugat R. Prevention of non-contact anterior cruciate ligament injuries in soccer players. Part 1: Mechanisms of injury and underlying risk factors. Knee Surg Sports Traumatol Arthrosc. 2009;17:705–729. doi: 10.1007/s00167-009-0813-1. [DOI] [PubMed] [Google Scholar]
- 3.Anderson AF, Dome DC, Gautam S, Awh MH, Rennirt GW. Correlation of anthropometric measurements, strength, anterior cruciate ligament size, and intercondylar notch characteristics to sex differences in anterior cruciate ligament tear rates. Am J Sports Med. 2001;29:58–66. doi: 10.1177/03635465010290011501. [DOI] [PubMed] [Google Scholar]
- 4.Arendt EA. Anterior cruciate ligament injuries. Curr Womens Health Rep. 2001;1:211–217. [PubMed] [Google Scholar]
- 5.Bland JM, Altman DG. Applying the right statistics: analyses of measurement studies. Ultrasound Obstet Gynecol. 2003;22:85–93. doi: 10.1002/uog.122. [DOI] [PubMed] [Google Scholar]
- 6.Boden BP, Breit I, Sheehan FT. Tibiofemoral alignment: contributing factors to noncontact anterior cruciate ligament injury. J Bone Joint Surg Am. 2009;91:2381–2389. doi: 10.2106/JBJS.H.01721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Boxheimer L, Lutz AM, Treiber K, Goepfert K, Crook DW, Marincek B, Weishaupt D. MR imaging of the knee: position related changes of the menisci in asymptomatic volunteers. Invest Radiol. 2004;39:254–263. doi: 10.1097/01.rli.0000116895.04239.84. [DOI] [PubMed] [Google Scholar]
- 8.Brandon ML, Haynes PT, Bonamo JR, Flynn MI, Barrett GR, Sherman MF. The association between posterior-inferior tibial slope and anterior cruciate ligament insufficiency. Arthroscopy. 2006;22:894–899. doi: 10.1016/j.arthro.2006.04.098. [DOI] [PubMed] [Google Scholar]
- 9.Brazier J, Migaud H, Gougeon F, Cotten A, Fontaine C, Duquennoy A. [Evaluation of methods for radiographic measurement of the tibial slope: a study of 83 healthy knees] [in French] Rev Chir Orthop Reparatrice Appar Mot. 1996;82:195–200. [PubMed] [Google Scholar]
- 10.Bylski-Austrow DI, Ciarelli MJ, Kayner DC, Matthews LS, Goldstein SA. Displacements of the menisci under joint load: an in vitro study in human knees. J Biomech. 1994;27:421–431. doi: 10.1016/0021-9290(94)90018-3. [DOI] [PubMed] [Google Scholar]
- 11.Caylor KB, Zumpano CA, Evans LM, Moore RW. Intra- and interobserver measurement variability of tibial plateau slope from lateral radiographs in dogs. J Am Anim Hosp Assoc. 2001;37:263–268. doi: 10.5326/15473317-37-3-263. [DOI] [PubMed] [Google Scholar]
- 12.Boer JJ, Blankevoort L, Kingma I, Vorster W. In vitro study of inter-individual variation in posterior slope in the knee joint. Clinical Biomech (Bristol, Avon) 2009;24:488–492. doi: 10.1016/j.clinbiomech.2009.03.008. [DOI] [PubMed] [Google Scholar]
- 13.Dejour H, Bonnin M. Tibial translation after anterior cruciate ligament rupture: two radiological tests compared. J Bone Joint Surg Br. 1994;76:745–749. [PubMed] [Google Scholar]
- 14.Faul F, Erdfelder E, Buchner A, Lang AG. Statistical power analyses using G*Power 3.1: tests for correlation and regression analyses. Behav Res Methods. 2009;41:1149–1160. doi: 10.3758/BRM.41.4.1149. [DOI] [PubMed] [Google Scholar]
- 15.Fulkerson JP, Arendt EA. Anterior knee pain in females. Clin Orthop Relat Res. 2000;372:69–73. doi: 10.1097/00003086-200003000-00009. [DOI] [PubMed] [Google Scholar]
- 16.Genin P, Weill G, Julliard R. The tibial slope: proposal for a measurement method][in French. J Radiol. 1993;74:27–33. [PubMed] [Google Scholar]
- 17.Giffin JR, Vogrin TM, Zantop T, Woo SL, Harner CD. Effects of increasing tibial slope on the biomechanics of the knee. Am J Sports Med. 2004;32:376–382. doi: 10.1177/0363546503258880. [DOI] [PubMed] [Google Scholar]
- 18.Griffin LY, Albohm MJ, Arendt EA, Bahr R, Beynnon BD, Demaio M, Dick RW, Engebretsen L, Garrett WE, Jr, Hannafin JA, Hewett TE, Huston LJ, Ireland ML, Johnson RJ, Lephart S, Mandelbaum BR, Mann BJ, Marks PH, Marshall SW, Myklebust G, Noyes FR, Powers C, Shields C, Jr, Shultz SJ, Silvers H, Slauterbeck J, Taylor DC, Teitz CC, Wojtys EM, Yu B. Understanding and preventing noncontact anterior cruciate ligament injuries: a review of the Hunt Valley II meeting, January 2005. Am J Sports Med. 2006;34:1512–1532. doi: 10.1177/0363546506286866. [DOI] [PubMed] [Google Scholar]
- 19.Grunewald J. Die Beziehungen zwischen der form und der Funktion der Tibia und Fibula des Menschen und einiger Menschenaffen. Z Orthop Chir. 1916;35:675–780. [Google Scholar]
- 20.Hashemi J, Chandrashekar N, Gill B, Beynnon BD, Slauterbeck JR, Schutt RC, Jr, Mansouri H, Dabezies E. The geometry of the tibial plateau and its influence on the biomechanics of the tibiofemoral joint. J Bone Joint Surg Am. 2008;90:2724–2734. doi: 10.2106/JBJS.G.01358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hashemi J, Chandrashekar N, Mansouri H, Gill B, Slauterbeck JR, Schutt RC, Jr, Dabezies E, Beynnon BD. Shallow medial tibial plateau and steep medial and lateral tibial slopes: new risk factors for anterior cruciate ligament injuries. Am J Sports Med. 2010;38:54–62. doi: 10.1177/0363546509349055. [DOI] [PubMed] [Google Scholar]
- 22.Hopkins WG. Measures of reliability in sports medicine and science. Sports Med. 2000;30:1–15. doi: 10.2165/00007256-200030010-00001. [DOI] [PubMed] [Google Scholar]
- 23.Hudek R, Schmutz S, Regenfelder F, Fuchs B, Koch PP. Novel measurement technique of the tibial slope on conventional MRI. Clin Orthop Relat Res. 2009;467:2066–2072. doi: 10.1007/s11999-009-0711-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Jenny JY, Boeri C, Ballonzoli L, Meyer N. [Difficulties and reproducibility of radiological measurement of the proximal tibial axis according to Levigne] [in French] Rev Chir Orthop Reparatrice Appar Mot. 2005;91:658–663. doi: 10.1016/s0035-1040(05)84470-8. [DOI] [PubMed] [Google Scholar]
- 25.Jenny JY, Rapp E, Kehr P. [Proximal tibial meniscal slope: a comparison with the bone slope] [in French] Rev Chir Orthop Reparatrice Appar Mot. 1997;84:435–438. [PubMed] [Google Scholar]
- 26.Kessler MA, Burkart A, Martinek V, Beer A, Imhoff AB. [Development of a 3-dimensional method to determine the tibial slope with multislice-CT] [in German] Z Orthop Ihre Grenzgeb. 2003;141:143–147. doi: 10.1055/s-2003-38658. [DOI] [PubMed] [Google Scholar]
- 27.Lerat JL, Moyen BL, Cladiere F, Besse JL, Abidi H. Knee instability after injury to the anterior cruciate ligament; quantification of the Lachman test. J Bone Joint Surg Br. 2000;82:42–47. doi: 10.1302/0301-620X.82B1.9740. [DOI] [PubMed] [Google Scholar]
- 28.Levy IM, Torzilli PA, Gould JD, Warren RF. The effect of lateral meniscectomy on motion of the knee. J Bone Joint Surg Am. 1989;71:401–406. [PubMed] [Google Scholar]
- 29.Levy IM, Torzilli PA, Warren RF. The effect of medial meniscectomy on anterior-posterior motion of the knee. J Bone Joint Surg Am. 1982;64:883–888. [PubMed] [Google Scholar]
- 30.Logan M, Dunstan E, Robinson J, Williams A, Gedroyc W, Freeman M. Tibiofemoral kinematics of the anterior cruciate ligament (ACL)-deficient weightbearing, living knee employing vertical access open “interventional” multiple resonance imaging. Am J Sports Med. 2004;32:720–726. doi: 10.1177/0095399703258771. [DOI] [PubMed] [Google Scholar]
- 31.Logan MC, Williams A, Lavelle J, Gedroyc W, Freeman M. Tibiofemoral kinematics following successful anterior cruciate ligament reconstruction using dynamic multiple resonance imaging. Am J Sports Med. 2004;32:984–992. doi: 10.1177/0363546503261702. [DOI] [PubMed] [Google Scholar]
- 32.Logan MC, Williams A, Lavelle J, Gedroyc W, Freeman M. What really happens during the Lachman test? A dynamic MRI analysis of tibiofemoral motion. Am J Sports Med. 2004;32:369–375. doi: 10.1177/0095399703258698. [DOI] [PubMed] [Google Scholar]
- 33.Mahfouz MR, Komistek RD, Dennis DA, Hoff WA. In vivo assessment of the kinematics in normal and anterior cruciate ligament-deficient knees. J Bone Joint Surg Am. 2004;86(suppl 2):56–61. doi: 10.2106/00004623-200412002-00009. [DOI] [PubMed] [Google Scholar]
- 34.Matsuda S, Miura H, Nagamine R, Urabe K, Ikenoue T, Okazaki K, Iwamoto Y. Posterior tibial slope in the normal and varus knee. Am J Knee Surg. 1999;12:165–168. [PubMed] [Google Scholar]
- 35.Meister K, Talley MC, Horodyski MB, Indelicato PA, Hartzel JS, Batts J. Caudal slope of the tibia and its relationship to noncontact injuries to the ACL. Am J Knee Surg. 1998;11:217–219. [PubMed] [Google Scholar]
- 36.Muhr G. [Meniscus and instability] [in German] Langenbecks Arch Chir. 1987;372:259–261. doi: 10.1007/BF01297825. [DOI] [PubMed] [Google Scholar]
- 37.Muller R, Buttner P. A critical discussion of intraclass correlation coefficients. Stat Med. 1994;13:2465–2476. doi: 10.1002/sim.4780132310. [DOI] [PubMed] [Google Scholar]
- 38.Musahl V, Citak M, O’Loughlin PF, Choi D, Bedi A, Pearle AD. The effect of medial versus lateral meniscectomy on the stability of the anterior cruciate ligament-deficient knee. Am J Sports Med. 2010;38:1591–1597. doi: 10.1177/0363546510364402. [DOI] [PubMed] [Google Scholar]
- 39.Senter C, Hame SL. Biomechanical analysis of tibial torque and knee flexion angle: implications for understanding knee injury. Sports Med. 2006;36:635–641. doi: 10.2165/00007256-200636080-00001. [DOI] [PubMed] [Google Scholar]
- 40.Shambaugh JP, Klein A, Herbert JH. Structural measures as predictors of injury basketball players. Med Sci Sports Exerc. 1991;23:522–527. [PubMed] [Google Scholar]
- 41.Shao Q, MacLeod TD, Manal K, Buchanan TS. Estimation of ligament loading and anterior tibial translation in healthy and ACL-deficient knees during gait and the influence of increasing tibial slope using EMG-driven approach. Ann Biomed Eng. 2011;39:110–121. doi: 10.1007/s10439-010-0131-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Shelburne KB, Kim HJ, Sterett WI, Pandy MG. Effect of posterior tibial slope on knee biomechanics during functional activity. J Orthop Res. 2011;29:223–231. doi: 10.1002/jor.21242. [DOI] [PubMed] [Google Scholar]
- 43.Shimokochi Y, Shultz SJ. Mechanisms of noncontact anterior cruciate ligament injury. J Athl Train. 2008;43:396–408. doi: 10.4085/1062-6050-43.4.396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Singerman R, Dean JC, Pagan HD, Goldberg VM. Decreased posterior tibial slope increases strain in the posterior cruciate ligament following total knee arthroplasty. J Arthroplasty. 1996;11:99–103. doi: 10.1016/S0883-5403(96)80167-7. [DOI] [PubMed] [Google Scholar]
- 45.Slocum B, Devine T. Cranial tibial thrust: a primary force in the canine stifle. J Am Vet Med Assoc. 1983;183:456–459. [PubMed] [Google Scholar]
- 46.Stijak L, Herzog RF, Schai P. Is there an influence of the tibial slope of the lateral condyle on the ACL lesion? A case-control study. Knee Surg Sports Traumatol Arthrosc. 2008;16:112–117. doi: 10.1007/s00167-007-0438-1. [DOI] [PubMed] [Google Scholar]
- 47.Todd MS, Lalliss S, Garcia E, DeBerardino TM, Cameron KL. The relationship between posterior tibial slope and anterior cruciate ligament injuries. Am J Sports Med. 20138:63–67. [DOI] [PubMed]
- 48.Vedi V, Williams A, Tennant SJ, Spouse E, Hunt DM, Gedroyc WM. Meniscal movement: an in-vivo study using dynamic MRI. J Bone Joint Surg Br. 1999;81:37–41. doi: 10.1302/0301-620X.81B1.8928. [DOI] [PubMed] [Google Scholar]
- 49.Eisenhart-Rothe R, Bringmann C, Siebert M, Reiser M, Englmeier KH, Eckstein F, Graichen H. Femoro-tibial and menisco-tibial translation patterns in patients with unilateral anterior cruciate ligament deficiency: a potential cause of secondary meniscal tears. J Orthop Res. 2004;22:275–282. doi: 10.1016/j.orthres.2003.08.009. [DOI] [PubMed] [Google Scholar]
- 50.Witvrouw E, Werner S, Mikkelsen C, Tiggelen D, Berghe L, Cerulli G. Clinical classification of patellofemoral pain syndrome: guidelines for non-operative treatment. Knee Surg Sports Traumatol Arthrosc. 2005;13:122–130. doi: 10.1007/s00167-004-0577-6. [DOI] [PubMed] [Google Scholar]
- 51.Yoshioka Y, Siu DW, Scudamore RA, Cooke TD. Tibial anatomy and functional axes. J Orthop Res. 1989;7:132–137. doi: 10.1002/jor.1100070118. [DOI] [PubMed] [Google Scholar]