Abstract
Background
Stiffness complicating TKA is a complex and multifactorial problem. We suspected internally rotated components compromised motion because of pain, patellar maltracking, a tight medial flexion gap, and limited femoral rollback on a conforming lateral tibial condyle.
Questions/purposes
We sought to determine: (1) the incidence of internal rotation of the femoral and tibial components in stiff TKAs; (2) if revision surgery that included correction of rotational positioning improved pain, ROM, and patellar tracking; and (3) if revision altered nonrotational radiographic parameters.
Methods
From a cohort of 52 patients with TKAs revised for stiffness, we performed CT scans of 34 before and 18 after revision to quantify rotational positioning of the femoral and tibial components using a previously validated scanning protocol.
Results
All 34 patients with TKAs had internal rotation of the summed values for tibial and femoral components (mean, 14.8°; range, 2.7°–33.7°) before revision for stiffness. The incidence of internal rotation was 24 of 34 femoral (mean, 3.1°; internal) and 33 of 34 tibial components (mean, 13.7° internal). Revision arthroplasty improved Knee Society function, knee, and pain scores. Mean extension improved from a contracture of 10.1° to 0.8° and flexion from 71.5° to 100°. Postrevision CT scans confirmed correction of component rotation. Nonrotational parameters were unchanged.
Conclusions
We recommend CT scanning of patients with stiff TKAs before surgical intervention to identify the presence of internally rotated components.
Level of Evidence
Level IV, therapeutic study. See Guidelines for Authors for a complete description of levels of evidence.
Introduction
Poor motion, or stiffness, occurs in 1.3% to 13.2% of TKAs [10, 11, 15, 16, 25, 40, 50] (Table 1). Whereas limited preoperative motion [37, 38], young age [36], obesity [43][40], low body mass index [36], and patella baja [35] have been identified as risk factors, knowledge of the etiology of stiffness is incomplete [9, 25, 34–36] and no definition is widely accepted [15, 25, 35, 40, 50] (Table 2).
Table 1.
Prevalence of knee stiffness after TKA
Table 2.
Published definitions of stiffness
| Study | Criteria |
|---|---|
| Kim et al. [25] | FFC > 15° or flexion < 75° |
| Parvizi et al. [35] | ROM < 90° or manipulation required |
| Gandhi et al. [15] | Flexion < 90° at 1 year |
| Yercan et al. [50] | FFC > 10° or flexion < 95° at 6 weeks |
| Scranton [40] | Flexion < 90° |
FFC = fixed flexion contracture.
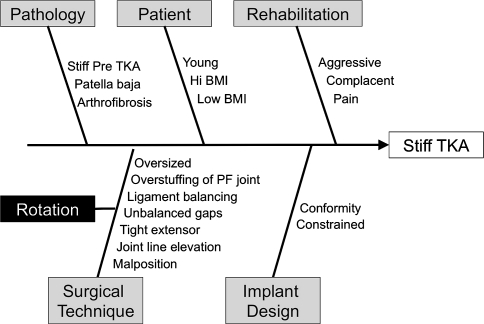
The contribution of intrinsic (eg, arthrofibrosis) versus extrinsic factors (eg, surgical technique) to stiffness is unclear. Many factors such as component sizing, patellar bone resection [24], ligament balancing, flexion-extension gap balance, extensor mechanism tension [41], joint line height, femoral component flexion position, and tibial slope influence motion [12, 25, 35, 39]. There is general agreement only that poor motion after TKA is a multifactorial problem (Fig. 1).
Fig. 1.
A fish diagram shows the multiple factors that can decrease TKA motion, either independently or additively. In a black box, on the left, is the factor Rotation that we believe may contribute to stiffness. BMI = body mass index.
Based on observations at prior revisions of stiff TKAs, we suspected that internal rotation of the tibial and femoral components, individually and summed, might alter knee kinematics in ways that limit ROM in some patients. Several mechanisms are feasible. Because internally rotated components increase patellar maltracking [28] (and more internal rotation results in more severe patellar complications) [3], we wondered if some patients, apprehensive that further flexion will result in dislocation of the patella, limit their motion. Also, the internally rotated femoral component tightens the medial flexion gap and the internally rotated tibial component has its posterolateral corner in a more anterior position. Given that posterior migration of the femoral condyle on the tibia with flexion occurs maximally in the lateral compartment, the internally rotated tibial component, especially of a conforming design, will limit rollback and flexion.
In this study, we sought to determine: (1) the incidence of internal rotation of the femoral and tibial components in stiff TKAs; (2) if revision surgery that corrected rotational positioning improved pain, ROM, and patellar tracking; and (3) if revision altered nonrotational radiographic parameters, as an alternate explanation for improvements.
Patients and Methods
We prospectively classified all 206 patients with complications of TKAs presenting to the senior author (KGV) between 1997 and 2007 as the result of: (1) infection [26, 29], (2) extensor rupture, (3) stiffness, (4) tibiofemoral instability, (5) patellar complications, (6) loosening, (7) periprosthetic fracture, (8) component breakage, and (9) a painful knee without diagnosis or a problem extrinsic to the knee. Patients in the last category did not undergo revision surgery. Stiffness was diagnosed if the patient reported unsatisfactory motion and either had a flexion contracture greater than 15° and/or flexion less than 105°. Of the 206 patients who had revision TKAs, 51 patients (52 knees) had revision surgery for stiffness. Of these patients, 34 agreed to CT scanning before revision surgery. Males were more common, patients were relatively younger, and there was a short interval before revision (Table 3). Thirty-two unsuccessful procedures were performed in 34 patients before the index revision (Table 4).
Table 3.
Patient demographics
| Parameter | Value |
|---|---|
| Gender (males/females) | 24/10 |
| Side (right/left) | 24/10 |
| Mean age at primary surgery (years) | 57.3 |
| Mean age at revision surgery (years) | 60.4 |
| Mean delay between surgeries (months) | 17.0 |
| Mean body mass index (kg/m2) | 28.3 |
Table 4.
Unsuccessful procedures before complete revision for stiffness
| Procedure | Number of patients |
|---|---|
| One manipulation under general anesthesia | 17 |
| Two manipulations under general anesthesia | 4 |
| Three manipulations under general anesthesia | 1 |
| Arthroscopic débridement | 2 |
| Open débridement | 1 |
| Polyethylene exchange (thinner polyethylene) | 3 |
| Previous partial revision for stiffness | 1 |
| Previous complete revision for stiffness | 3 |
Physical therapy and manipulation under general anesthesia were recommended in the first several months after surgery. Revision arthroplasty was not offered if the patient had arthritis of the ipsilateral hip as the cause of pain and stiffness, (in which case hip arthroplasty was recommended) or if the arthritic knee was stiff before the primary TKA. No patient was included with stiffness from a secondary cause (eg, component breakage) after an initial period of satisfactory motion. No patients with component loosening were included. Patients who underwent revision surgery were evaluated at a mean of 22 months (range, 6–52 months) after surgery.
Power analysis was performed with respect to the effect of revision knee arthroplasty on 34 stiff TKAs as measured by Knee Society scores (pain, knee, and function), with a change of 15 points established as a clinically important outcome for each [14]. This analysis concluded that sample sizes of 16, (pain), 24 (knee), and 36 (function) would be sufficient to detect differences with 80% power at the 0.05 significance level. (Version 9.1; SAS Institute, Cary, NC, USA). A second analysis of the effect of revision arthroplasty on knee flexion, with a clinically important threshold of 15°, concluded that a sample size of 31 would detect differences with 80% power at the 0.05 significance level. The final analysis was performed, with respect to the difference in 18 knees of combined tibial and femoral component rotational position on CT scans, before and after revision arthroplasty, with 10° established as clinically important. This concluded that a sample size of 21 would detect differences with 80% power at the 0.05 significance level.
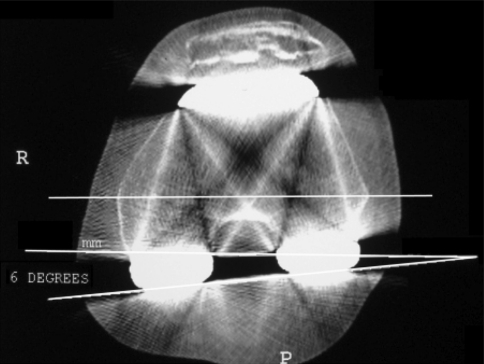
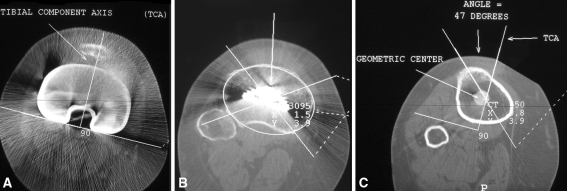
With Institutional Review Board approval, CT was recommended for all patients with TKAs considered for revision. A staff radiologist reported rotational positioning of femoral and tibial components using a previously described technique [3, 4]. CT images 1.5 mm thick were obtained at four locations: through the epicondylar axis on the femur (Fig. 2), through the tibial tubercle, through the top of the tibial plateau, and through the tibial component (Fig. 3). The protocol was modified for asymmetric (right and left) tibial components (Fig. 4).
Fig. 2.
The CT scan measurement technique for the femoral rotation angle is shown. A CT scan shows the medial and lateral epicondyles on the distal femur. The line closest to the bottom of the figure connects the posterior surfaces of the prosthetic posterior condyles, depicting the position of the component. The horizontal line in the middle of the figure connects the medial and lateral epicondyles, defining the transepicondylar axis (TEA). This line is recopied closer to the posterior condyles to facilitate measurement of the angle between the component and the TEA, in this patient 6° of internal rotation.
Fig. 3A–C.
Three cuts of the CT scan are required to define the rotational position of the tibial component relative to the extensor mechanism, specifically the tibial tubercle. (A) The most proximal cut of the CT scan passes through the component and defines the tibial component angle (TCA). (B) Immediately distal to the component a second cut is used to establish the geometric center of the proximal tibia. (C) The most distal cut is performed through the tibial tubercle. Data from the preceding two images are superimposed on this image: (1) the geometric center and (2) the TCA. One line is drawn from the apex of the tubercle to the geometric center, bearing in mind that the tibial tubercle is not in the center of the proximal tibia (the medial condyle being larger than the lateral). The angle subtended by this line and the TCA is the rotational position of the tibial component. Given the asymmetry of the tibia, angles up to 8° have been associated with normal position and good TKA function. This patient had an angle of 47°–18° = 29° pathologic internal rotation.
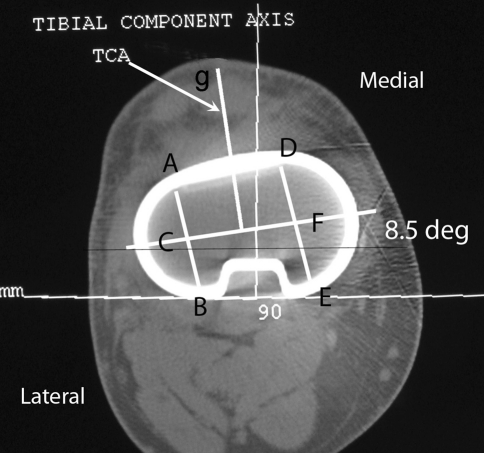
Fig. 4.
A modification of the technique to assess the rotational position of asymmetric tibial components is shown. Lines AB and DE cross the lateral and medial hemiplateau respectively. Both are bisected. A third line, CF, connects the centers of each hemiplateau and defines the flexion axis for an asymmetric component. The line at right angles to the flexion axis (indicated by the arrow and terminating at g), defines the TCA for an asymmetric component. In this case the TCA was corrected by 8.5%.
All revision procedures were performed by the senior author (KGV), with patients receiving routine antibiotic prophylaxis [30]. The surgical technique included (1) removal of the intraarticular scar, (2) rotational positioning of components according to anatomic landmarks, and (3) balancing flexion and extension gaps. The scar was managed with synovectomy, restoration of the medial and lateral parafemoral gutters, separation of the deep surface of the distal quadriceps from the anterior femur, and liberation of the patellar tendon adherent to the tibia proximal to the tubercle [42]. Gentle manipulation was performed before component removal.
The tibia was reconstructed first, with the center of the anterior tibial component rotated to the tibial tubercle, centering it behind the patellar tendon. As the femoral condyles sit in conforming tibial wells, the patella is located between the femoral condyles. This rotational position (compared with internal rotation) places the lateral tibial component farther posteriorly, to accommodate posterolateral femoral rollback.
The femoral component size was selected to decrease tightness in flexion without instability. This femoral component was rotated to the transepicondylar axis and the flexion gap stabilized with the tibial articular component. The joint line was established in flexion relative to the inferior pole of the patella. Trial component position was maintained with diaphyseal engaging, intramedullary stem extensions so that the desired distal position of the femoral component could be determined by extending the knee fully [45, 47]. Constrained implants were selected if scar release created instability.
No surgical maneuver beyond scar removal was required in 30 cases [19]. Four knees had a quadriceps split or snip [43, 45]. No patient required a tubercle osteotomy or a quadriceps turndown [42]. Femoral and tibial components were revised in all cases. A posterior-stabilized articulation was used in 16 knees, a nonlinked varus-valgus constrained device in 17 knees, and a rotating hinge prosthesis in one. A posterolateral femoral augment was used in 19 knees to increase external rotation of the femoral component, and a posteromedial augment was used in two.
Gentle motion began at 48 hours. Continuous passive motion (CPM) was recommended, but discontinued if the patient reported dissatisfaction. Frequent, gentle exercise was preferred over home CPM or supervised physical therapy sessions. Patients limited walking until swelling subsided.
Clinical data for Knee Society scores were collected by one of us (KGV) at 2 weeks, 6 weeks, 3 months, 6 months, and annually after surgery. Single-leg weightbearing AP, weightbearing lateral, Merchant patellofemoral [31], and full-length radiographs showing the hip, knee, and ankle on one view for mechanical alignment were obtained before and after revision arthroplasty. The key nonrotational variables on these studies were femorotibial angle, femoral component flexion angle [22], tibial slope [19, 22], joint line height (Fig. 5), Insall-Salvati ratio [20, 21], patellar tilt [2, 5, 6], and patellar displacement [2, 5, 6] (Fig. 6). All measurements were made by one of us (JR) who was unaware of the clinical outcome of the revision procedure. Using the identical CT scan protocol, a repeat study was requested after revision for stiffness, consistent with the Institutional Review Board-approved protocol. After revision arthroplasty for stiffness, 18 of 34 patients with prerevision CT scans agreed to second scans.
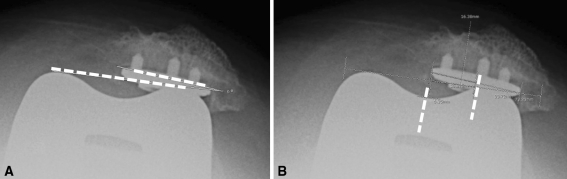
Fig. 5A–B.
The joint line was measured along the anatomic axis of the tibial shaft, viewed on a lateral radiograph. The location of the inferior pole of the patellar tendon was identified along this axis and the joint line defined as the contact of the most distal point of the femoral component. (A) The prerevision and (B) postrevision relationships of the joint line and the patella are shown.
Fig. 6A–B.
(A) Patellar tilt or angulation is defined by the angle subtended by a line across the distal femoral articulation and one along the cut surface of the patella. (B) Patellar translation is measured as the displacement of the center of the patellar component from the center of the femoral sulcus [6, 7].
We used a paired t-test to evaluate the difference in means between the prerevision and postrevision Knee Society scores. The analysis was stratified based on positive and negative difference values in which difference was the postmeasurement minus the premeasurement for CT scan angles, patellar tilt, and patellar displacement. The Shapiro-Wilk test was used to test for normality. When the Shapiro-Wilk test for normality was significant, the Wilcoxon signed rank test (nonparametric paired t-test) was used to determine if there was a difference in the median value of the preoperative and postoperative scores.
Results
All 34 patients had net combined internal rotation of the femoral and tibial components according to the prerevision CT scan protocol, averaging 14.8° (range, 2.7°–33.7°). Twenty-four of the 34 patients (70%) had modest internal rotation of the femoral component (Table 5). The largest source of internal rotation was the tibia, with 33 of the 34 patients having internal rotation, with a mean of 13.7° (range, 1° external rotation to 35° internal rotation). One patient with neutral rotation of the tibial component had 5.7° internal rotation for the femoral component.
Table 5.
CT scan measurements
| Time of measurement | Component rotation | Net femoral rotation (°) | Net tibial rotation (°) | Net combined rotation (°) | |||
|---|---|---|---|---|---|---|---|
| (p = 0.0004) | (p < 0.0001) | (p < 0.0001) | |||||
| Mean | Number of patients | Mean | Number of patients | Mean | Number of patients | ||
| Prerevision | Internal | 3.1 | 24 | 13.7 | 33 | 14.9 | 34 |
| External | 1.3 | 10 | 1.0 | 1 | 0 | ||
| Postrevision | Internal | 2.1 | 15 | 3.3 | 3 | 3.9 | 3 |
| External | 1.1 | 3 | 8.5 | 15 | 8.5 | 15 | |
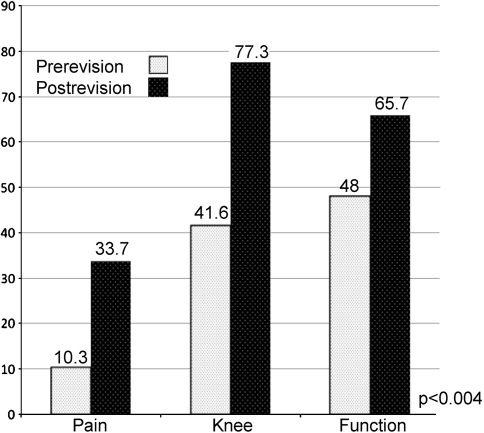
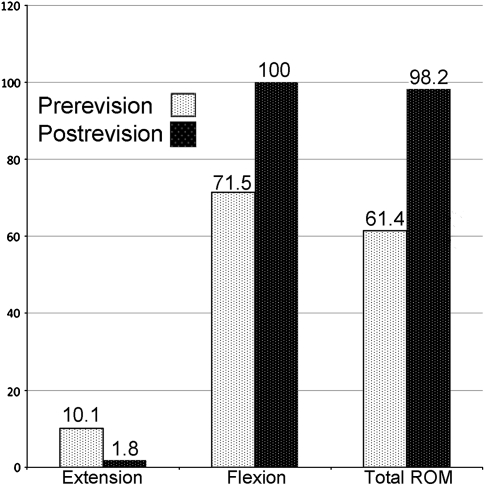
After revision, pain scores improved from 10.3 to 33.7 points, knee scores improved from 41.6 to 77.3 points, and function scores improved (p < 0.004) from 48 to 65.7 points (Fig. 7). Extension and flexion improved after revision; the total arc of motion increased (p < 0.001) from 61° to 98° (Fig. 8). Femoral and tibial component rotation was corrected (p < 0.0001) by revision (Table 5).
Fig. 7.
Prerevision and postrevision Knee Society pain, knee, and function scores are shown.
Fig. 8.
Lack of extension before revision (light stippled columns) compared with postrevision (dark stippled columns) shows a reduction in the flexion contracture. There was improved (p < 0.001) flexion and motion overall.
Nonrotational radiographic measurements, other than static images of patellar tracking, were unaffected by revision. The mean femorotibial angle (alignment) was unchanged (p = 0.119), patellar height relative to the joint line was unchanged (p = 0.266), and the Insall-Salvati ratio was unchanged (p = 0.612). Similarly, the mean femoral component flexion angle was unchanged (p = 0.035) and the tibial slope also was unchanged (p = 0.048). Patellar tracking improved after revision, as inferred from measurements of patellar tilt (p < 0.001) (Table 6) and translation (p = 0.017) (Table 7) on Merchant-view patellofemoral radiographs.
Table 6.
Patellar tilt
| Tilt opening | Prerevision | Postrevision | p Value | ||
|---|---|---|---|---|---|
| Mean tilt (°) | % of patients | Mean tilt (°) | % of patients | ||
| Medial | 3.3 | 38 | 1.6 | 23 | < 0.0001 |
| Lateral | 8.5 | 58 | 3.1 | 65 | 0.0002 |
| Neutral | 4 | ||||
Table 7.
Patellar translation
| Translation direction | Prerevision | Postrevision | p Value | ||
|---|---|---|---|---|---|
| Mean translation (°) | % of patients | Mean translation (°) | % of patients | ||
| Medial | 3.6 | 23 | 3.1 | 68 | 0.0179 |
| Lateral | 8.0 | 62 | 4.3 | 23 | < 0.0001 |
| Neutral | 15 | 9 | |||
Minor complications included five manipulations under anesthesia after revision. Two patients had a second manipulation. Patients having manipulation postrevision ultimately achieved a mean postoperative ROM of 95°, with knee and function scores of 66 and 60, respectively. Two patients had arthrotomies after the revision for release of a scar, and in one patient, the tibial polyethylene was exchanged to a thinner component. One patient had a two-stage reimplantation protocol owing to infection and ceased participation in the study after a self-inflicted gunshot wound. Two patients underwent above-knee amputations. The first sought amputation elsewhere months after revision for unremitting pain, having achieved motion from 0° to 120°. She had less than 5° combined internal rotation suggesting other factors explained her pain and stiffness. The second patient required urgent amputation for diabetic small vessel insufficiency not amenable to bypass as restoration of flexion curtailed perfusion to the foot.
Discussion
Stiffness complicating a TKA is a complex, usually multifactorial problem. We suspected internal rotation of the femoral and tibial components (known to cause maltracking [3, 20, 28, 32, 48], and anterior knee pain [2]) might contribute to stiffness [46]. Impending patellar dislocation limits knee motion, the internally rotated femoral component tightens the medial flexion gap, and an internally rotated tibial component restricts lateral femoral condylar rollback on a conforming tibia during flexion. Malrotation in stiff TKAs before revision was measured using an established CT scan protocol [2–4, 23]. We then assessed the clinical results of revision and whether malrotation had been corrected. Finally, we evaluated whether correction of nonrotational parameters might have explained the improvements.
The study was limited by numerous factors. First, a limited number of patients agreed to postrevision CT scans, to the point where the study achieved less than 80% power (21 subjects would have been necessary). However these 18 patients constitute the second largest series with revision knee arthroplasties for stiffness [25]. Second, the study depends on historical controls for normal values of rotational position [2, 3]. If we had a concurrent control group of TKAs with high function, we would have been able to perform a direct test of our method and of our ability to replicate the CT protocol [3, 4]. Nonetheless, we believe the historical controls serve the same purpose. Third is lack of consensus regarding what constitutes [7, 12, 24, 33, 39] and causes [7, 12, 24, 33, 36, 39] stiffness. We defined stiffness, by patient complaints, as either flexion contracture exceeding 15° or flexion less than 105°. Fourth, we did not confirm arthrofibrosis histologically, as was reported by Parvizi et al. [35]. Fifth, some might view complete revision as being overly aggressive compared with lysis of adhesions [17], arthroscopic resection of the posterior cruciate ligament [49], exchange of modular polyethylene [1], and partial revision. This view assumes stiffness is a result of a biologic response to the surgery, rather than some mechanical aspect in surgical technique. Further, there is substantial disagreement among some of these studies; one describes 100% success after open lysis of adhesions in 13 stiff TKAs [17], and another reports 100% failures [1]. This dichotomy might have been resolved by preoperative CT scanning. As 67% of the patients we treated already had at least one unsuccessful procedure before our consultation, and because malrotation could be quantified by CT, we selected complete revision [13, 26, 27]. Finally, it is possible we improved motion simply by lysis of adhesions or downsizing the femoral component size, effects that are difficult to isolate in these patients.
We found internal rotation in all cases when tibial and femoral values were added. The tibia was affected in 33 of 34 cases with an average of 13.7° pathologic internal rotation. Berger et al. established that the deleterious effect of tibial and femoral internal rotation on patellar tracking was exerted individually and additively [3]. Barrack et al. found with CT evaluation that patients with anterior knee pain who underwent TKAs had a higher incidence of internal rotation of the tibial component (6.2° internal rotation) as compared with a pain-free control group (0.4° external rotation) [2]. In both studies, there was more internal rotation of the tibial component than of the femoral component. Using the same CT protocol and comparing our results with those of Berger et al. [3], we found approximately 10 times the internal tibial rotation in stiff TKAs compared with TKAs with maltracking or tilting patellae, 3.3 times more internal rotation compared with subluxating TKAs, and approximately 1.5 times compared with patellae that dislocate or sustain prosthetic failure (Table 8). The mean value for internal rotation of the tibial component in our stiff TKAs was more than double that reported by Barrack et al. [2] for patients with anterior knee pain who have TKAs. In one scenario for the development of stiffness, small degrees of internal rotation result in patellar maltracking and pain, whereas large amounts make it too painful or impossible for patients to bend well. Two other studies have evaluated only the femoral components using CT [8, 44].
Table 8.
Published series employing CT scan protocol to measure tibial and femoral component rotational position
| Publication | Year of study | TKA | TKA group | Tibial | Femoral | Combined | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean (degrees) | Range (degrees) | p Value | Mean (degrees) | Range (degrees) | p Value | Mean (degrees) | Range (degrees) | p Value | ||||
| Berger et al. [3] | 1998 | 30 | 1. Lateral tracking and tilt | 1.8 IR | NS | 0.8 IR | NS | Not reported | 1–4 IR | 0.0001 | ||
| 2. Subluxation | 4 IR | NS | 1.9 IR | NS | 3–8 IR | |||||||
| 3. Early dislocation | 8.7 IR | NS | 2.4 IR | NS | ||||||||
| 4. Prosthesis breakage | 8.3 IR | 3.9 IR | 7–17 IR | |||||||||
| 20 | 5. Control | NA | NA | NA | NA | 10–1 ER | ||||||
| Barrack et al. [2] | 2001 | 14 | Anterior knee pain | 6.2 IR | 15 IR–6 ER | 0.012 | 1.5 ER | 5 IR–7 ER | NS | 4.7 IRl | 4 ER–17 IR | 0.0035 |
| 14 | Control | 0.4 ER | 8 IR–12 ER | 2.2 ER | 4 IR–9 ER | 2.6 ER | 14 ER–4 IR | |||||
| Current study | 2010 | 34 | Prerevision | 13.2 IR | 1–35 IR | 1.8 IR | 0–9 IR | 14.9 IR | 2.7 ER–37.7 IR | 0.0001 | ||
| 18 | Postrevision | 3.4 ER | 0.8 ER | 3.4 ER | ||||||||
IR = internal rotation; NA = not available; ER = external rotation; NS = nonsignificant.
Revision for stiffness, with correction of internally rotated tibial and femoral components (Table 5) improved motion and reduced pain in our patients. Incavo et al. found poor ROM in 36% of patients who underwent revision surgery specifically for clinically apparent malrotation [18]. All studies report modest improvements in motion and pain relief (Table 9). Malrotation is mentioned by Nelson et al. only in a later supplement on surgical technique [33] that referred to data from the original series of patients described by Kim et al. [25] who did not report data on rotational positioning. Kim et al. included stiffness attributed to loose components, which we believe is a distinct diagnostic entity [25].
Table 9.
Published series of revision TKAs for stiffness
| Study | Total revision TKA (excluding cases of loosening) | Mean age (minimum–maximum)(years) | CT scans | Mention rotation? | Revision - months after primary surgery/range | Followup (months) | Prerevision | Postrevision | Pain improved? | ||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Flexion (degrees) | Flexion contracture (degrees) | Flexion (degrees) | Flexion contracture (degrees) | ||||||||
| Ries & Badalamente [36] | 6 | 65 (58–75) | None | No | 20 (10–45) | 33 (24–54) | 58 | 22 | 87 | 1 | yes |
| Christensen et al. [10] | 8 | 62 (45–72) | None | No | 19 (6–48) | 37 (24–53) | 40 | 12 | 83 | 2 | yes |
| Kim et al. [25] | 38 | 69 (36–89) | None | No | 18 (9–62) | 43 (24–70) | 66 | 11 | 85 | 3 | yes |
| Haidukewych et al. [16] | 16 | 67 (44–85) | None | Yes | 24 (3–42) | 42 (24–72) | 63 | 22 | 81 | 8 | yes |
| Current study | 52 | 60 (40–80) | Yes | Yes | 27 (4–78) | 22 (6–52) | 71.5 | 10.1 | 100 | 2 | yes |
Our revisions did not alter varus-valgus alignment, joint line height, or patella baja. We observed no changes to tibial and femoral component positions as viewed on the lateral radiograph. A flexed, femoral component position is a risk factor for stiffness [35], and an increase in the AP dimension of the prearthroplasty femoral condyles by 12% increases the need for manipulation [11]. These observations are consistent with the comment that downsizing the femoral component is “integral to ROM improvements” [18]. The review, by Kim et al., of revision surgery for stiffness included a radiographic analysis with similar findings [25]. Patellar tilt and translation improved in our study after revision. Barrack et al., using the same radiographic techniques for patellar tilt and translation (in addition to CT), also showed worse tracking in patients with TKAs with anterior knee pain and internal rotational positioning of tibial and femoral components [2]. Yercan et al., studying stiff TKAs, stated that “patellar problems are a good prognostic factor for the success of revision surgery” [50], implying that motion and pain will improve if tracking, ie, rotational position, is corrected. We conclude that internal rotation of the tibial component occurs more frequently than previously believed and leads to poor motion, patellar complications, and anterior knee pain.
Footnotes
One or more of the authors (KGV) has a consultancy agreement and has received royalties from Zimmer Inc (Warsaw, IN).
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
This work was performed at the Department of Orthopaedic Surgery, University of Southern California, Los Angeles, CA, USA.
References
- 1.Babis GC, Trousdale RT, Pagnano MW, Morrey BF. Poor outcomes of isolated tibial insert exchange and arthrolysis for the management of stiffness following total knee arthroplasty. J Bone Joint Surg Am. 2001;83:1534–1536. doi: 10.2106/00004623-200110000-00012. [DOI] [PubMed] [Google Scholar]
- 2.Barrack RL, Schrader T, Bertot AJ, Wolfe MW, Myers L. Component rotation and anterior knee pain after total knee arthroplasty. Clin Orthop Relat Res. 2001;392:46–55. doi: 10.1097/00003086-200111000-00006. [DOI] [PubMed] [Google Scholar]
- 3.Berger RA, Crossett LS, Jacobs JJ, Rubash HE. Malrotation causing patellofemoral complications after total knee arthroplasty. Clin Orthop Relat Res. 1998;356:144–153. doi: 10.1097/00003086-199811000-00021. [DOI] [PubMed] [Google Scholar]
- 4.Berger RA, Rubash HE, Seel MJ, Thompson WH, Crossett LS. Determining the rotational alignment of the femoral component in total knee arthroplasty using the epicondylar axis. Clin Orthop Relat Res. 1993;286:40–47. [PubMed] [Google Scholar]
- 5.Bindelglass DF, Cohen JL, Dorr LD. Patellar tilt and subluxation in total knee arthroplasty: relationship to pain, fixation, and design. Clin Orthop Relat Res. 1993;286:103–109. [PubMed] [Google Scholar]
- 6.Bindelglass DF, Vince KG. Patellar tilt and subluxation following subvastus and parapatellar approach in total knee arthroplasty: implication for surgical technique. J Arthroplasty. 1996;11:507–511. doi: 10.1016/S0883-5403(96)80101-X. [DOI] [PubMed] [Google Scholar]
- 7.Boldt JG, Munzinger UK, Zanetti M, Hodler J. Arthrofibrosis associated with total knee arthroplasty: gray-scale and power Doppler sonographic findings. AJR Am J Roentgenol. 2004;182:337–340. doi: 10.2214/ajr.182.2.1820337. [DOI] [PubMed] [Google Scholar]
- 8.Boldt JG, Stiehl JB, Hodler J, Zanetti M, Munzinger U. Femoral component rotation and arthrofibrosis following mobile-bearing total knee arthroplasty. Int Orthop. 2006;30:420–425. doi: 10.1007/s00264-006-0085-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bong MR, Di Cesare PE. Stiffness after total knee arthroplasty. J Am Acad Orthop Surg. 2004;12:164–171. doi: 10.5435/00124635-200405000-00004. [DOI] [PubMed] [Google Scholar]
- 10.Christensen CP, Crawford JJ, Olin MD, Vail TP. Revision of the stiff total knee arthroplasty. J Arthroplasty. 2002;17:409–415. doi: 10.1054/arth.2002.32105. [DOI] [PubMed] [Google Scholar]
- 11.Daluga D, Lombardi AV, Jr, Mallory TH, Vaughn BK. Knee manipulation following total knee arthroplasty: analysis of prognostic variables. J Arthroplasty. 1991;6:119–128. doi: 10.1016/S0883-5403(11)80006-9. [DOI] [PubMed] [Google Scholar]
- 12.Dennis DA. The stiff total knee arthroplasty: causes and cures. Orthopedics. 2001;24:901–902. doi: 10.3928/0147-7447-20010901-36. [DOI] [PubMed] [Google Scholar]
- 13.Fehring TK, Odum S, Griffin WL, Mason JB. Outcome comparison of partial and full component revision TKA. Clin Orthop Relat Res. 2005;440:131–134. doi: 10.1097/01.blo.0000186560.70566.dc. [DOI] [PubMed] [Google Scholar]
- 14.Freedman KB, Bernstein J. Sample size and statistical power in clinical orthopaedic research. J Bone Joint Surg Am. 1999;81:1454–1460. doi: 10.2106/00004623-199910000-00011. [DOI] [PubMed] [Google Scholar]
- 15.Gandhi R, Beer J, Leone J, Petruccelli D, Winemaker M, Adili A. Predictive risk factors for stiff knees in total knee arthroplasty. J Arthroplasty. 2006;21:46–52. doi: 10.1016/j.arth.2005.06.004. [DOI] [PubMed] [Google Scholar]
- 16.Haidukewych GJ, Jacofsky DJ, Pagnano MW, Trousdale RT. Functional results after revision of well-fixed components for stiffness after primary total knee arthroplasty. J Arthroplasty. 2005;20:133–138. doi: 10.1016/j.arth.2004.09.057. [DOI] [PubMed] [Google Scholar]
- 17.Hutchinson JR, Parish EN, Cross MJ. Results of open arthrolysis for the treatment of stiffness after total knee replacement. J Bone Joint Surg Br. 2005;87:1357–1360. doi: 10.1302/0301-620X.87B10.16228. [DOI] [PubMed] [Google Scholar]
- 18.Incavo S, Wild J, Coughlin K, Beynnon B. Early revision for component malrotation in total knee arthroplasty. Clin Orthop Relat Res. 2007;458:131–136. doi: 10.1097/BLO.0b013e3180332d97. [DOI] [PubMed] [Google Scholar]
- 19.Insall J. A midline approach to the knee. J Bone Joint Surg Am. 1971;53:1584–1586. [PubMed] [Google Scholar]
- 20.Insall J, Goldberg V, Salvati E. Recurrent dislocation and the high-riding patella. Clin Orthop Relat Res. 1972;88:67–69. doi: 10.1097/00003086-197210000-00012. [DOI] [PubMed] [Google Scholar]
- 21.Insall J, Salvati E. Patella position in the normal knee joint. Radiology. 1971;101:101–104. doi: 10.1148/101.1.101. [DOI] [PubMed] [Google Scholar]
- 22.Insall JN, Dorr LD, Scott RD, Scott WN. Rationale of the Knee Society clinical rating system. Clin Orthop Relat Res. 1989;248:13–14. [PubMed] [Google Scholar]
- 23.Jazrawi LM, Birdzell L, Kummer FJ, Di Cesare PE. The accuracy of computed tomography for determining femoral and tibial total knee arthroplasty component rotation. J Arthroplasty. 2000;15:761–766. doi: 10.1054/arth.2000.8193. [DOI] [PubMed] [Google Scholar]
- 24.Jiang CC, Yip KM, Liu DH. Patellar thickness in total knee replacement. J Formos Med Assoc. 1994;93:417–420. [PubMed] [Google Scholar]
- 25.Kim J, Nelson CL, Lotke PA. Stiffness after total knee arthroplasty: prevalence of the complication and outcomes of revision. J Bone Joint Surg Am. 2004;86:1479–1484. doi: 10.1302/0301-620X.86B7.15255. [DOI] [PubMed] [Google Scholar]
- 26.Knutson K, Lewold S, Robertsson O, Lidgren L. The Swedish knee arthroplasty register: a nation-wide study of 30, 003 knees 1976–1992. Acta Orthop Scand. 1994;65:375–386. doi: 10.3109/17453679408995475. [DOI] [PubMed] [Google Scholar]
- 27.Mackay DC, Siddique MS. The results of revision knee arthroplasty with and without retention of secure cemented femoral components. J Bone Joint Surg Br. 2003;85:517–520. doi: 10.1302/0301-620X.85B4.13749. [DOI] [PubMed] [Google Scholar]
- 28.Malo M, Vince KG. The unstable patella after total knee arthroplasty: etiology, prevention, and management. J Am Acad Orthop Surg. 2003;11:364–371. doi: 10.5435/00124635-200309000-00009. [DOI] [PubMed] [Google Scholar]
- 29.Mason JB, Fehring TK, Odum SM, Griffin WL, Nussman DS. The value of white blood cell counts before revision total knee arthroplasty. J Arthroplasty. 2003;18:1038–1043. doi: 10.1016/S0883-5403(03)00448-0. [DOI] [PubMed] [Google Scholar]
- 30.Mauerhan DR, Nelson CL, Smith DL, Fitzgerald RH, Jr, Slama TG, Petty RW, Jones RE, Evans RP. Prophylaxis against infection in total joint arthroplasty: one day of cefuroxime compared with three days of cefazolin. J Bone Joint Surg Am. 1994;76:39–45. doi: 10.2106/00004623-199401000-00006. [DOI] [PubMed] [Google Scholar]
- 31.Merchant AC, Mercer RL, Jacobsen RH, Cool CR. Roentgenographic analysis of patellofemoral congruence. J Bone Joint Surg Am. 1974;56:1391–1396. [PubMed] [Google Scholar]
- 32.Merkow RL, Soudry M, Insall JN. Patellar dislocation following total knee replacement. J Bone Joint Surg Am. 1985;67:1321–1327. [PubMed] [Google Scholar]
- 33.Nelson CL, Kim J, Lotke PA. Stiffness after total knee arthroplasty. J Bone Joint Surg Am. 2005;87(suppl 1):264–270. doi: 10.2106/JBJS.E-00345. [DOI] [PubMed] [Google Scholar]
- 34.Nicholls DW, Dorr LD. Revision surgery for stiff total knee arthroplasty. J Arthroplasty. 1990;5(suppl):S73–77. doi: 10.1016/S0883-5403(08)80029-0. [DOI] [PubMed] [Google Scholar]
- 35.Parvizi J, Tarity TD, Steinbeck MJ, Politi RG, Joshi A, Purtill JJ, Sharkey PF. Management of stiffness following total knee arthroplasty. J Bone Joint Surg Am. 2006;88(suppl 4):175–181. doi: 10.2106/JBJS.F.00608. [DOI] [PubMed] [Google Scholar]
- 36.Ries MD, Badalamente M. Arthrofibrosis after total knee arthroplasty. Clin Orthop Relat Res. 2000;380:177–183. doi: 10.1097/00003086-200011000-00024. [DOI] [PubMed] [Google Scholar]
- 37.Ritter MA, Berend ME, Harty LD, Davis KE, Meding JB, Keating EM. Predicting range of motion after revision total knee arthroplasty: clustering and log-linear regression analyses. J Arthroplasty. 2004;19:338–343. doi: 10.1016/j.arth.2003.11.001. [DOI] [PubMed] [Google Scholar]
- 38.Ritter MA, Harty LD, Davis KE, Meding JB, Berend ME. Predicting range of motion after total knee arthroplasty: clustering, log-linear regression, and regression tree analysis. J Bone Joint Surg Am. 2003;85:1278–1285. doi: 10.2106/00004623-200307000-00014. [DOI] [PubMed] [Google Scholar]
- 39.Scott WN, Clarke HD. The stiff knee: causes and cures. Orthopedics. 2000;23:987–988. doi: 10.3928/0147-7447-20000901-31. [DOI] [PubMed] [Google Scholar]
- 40.Scranton PE., Jr Management of knee pain and stiffness after total knee arthroplasty. J Arthroplasty. 2001;16:428–435. doi: 10.1054/arth.2001.22250. [DOI] [PubMed] [Google Scholar]
- 41.Scuderi GR. The stiff total knee arthroplasty: causality and solution. J Arthroplasty. 2005;20(4 suppl 2):23–26. doi: 10.1016/j.arth.2005.03.014. [DOI] [PubMed] [Google Scholar]
- 42.Sharkey PF, Homesley HD, Shastri S, Jacoby SM, Hozack WJ, Rothman RH. Results of revision total knee arthroplasty after exposure of the knee with extensor mechanism tenolysis. J Arthroplasty. 2004;19:751–756. doi: 10.1016/j.arth.2003.12.084. [DOI] [PubMed] [Google Scholar]
- 43.Shoji H, Solomonow M, Yoshino S, D’Ambrosia R, Dabezies E. Factors affecting postoperative flexion in total knee arthroplasty. Orthopedics. 1990;13:643–649. doi: 10.3928/0147-7447-19900601-08. [DOI] [PubMed] [Google Scholar]
- 44.Suter T, Zanetti M, Schmid M, Romero J. Reproducibility of measurement of femoral component rotation after total knee arthroplasty using computer tomography. J Arthroplasty. 2006;21:744–748. doi: 10.1016/j.arth.2005.09.012. [DOI] [PubMed] [Google Scholar]
- 45.Vince K, Bedard M. Implanting the Revision Total Knee Arthroplasty. In: Lotke PA, Lonner J, editors. Master Techniques in Orthopedic Surgery: Knee Arthroplasty. 3. Baltimore, MD: Lippincott, Williams and Wilkins; 2008. pp. 203–228. [Google Scholar]
- 46.Vince K, Eissmann E. The Stiff TKA. In: Fu FH, Harner CD, Vince K, editors. Knee Surgery. Baltimore, MD: Lippincott, Williams and Wilkins; 1994. pp. 1529–1538. [Google Scholar]
- 47.Vince KG. A step-wise approach to revision TKA. Orthopedics. 2005;28:999–1001. doi: 10.3928/0147-7447-20050901-43. [DOI] [PubMed] [Google Scholar]
- 48.Vince KG, McPherson EJ. The patella in total knee arthroplasty. Orthop Clin North Am. 1992;23:675–686. [PubMed] [Google Scholar]
- 49.Williams RJ, 3rd, Westrich GH, Siegel J, Windsor RE. Arthroscopic release of the posterior cruciate ligament for stiff total knee arthroplasty. Clin Orthop Relat Res. 1996;331:185–191. doi: 10.1097/00003086-199610000-00026. [DOI] [PubMed] [Google Scholar]
- 50.Yercan HS, Sugun TS, Bussiere C, Ait Si Selmi T, Davies A, Neyret P. Stiffness after total knee arthroplasty: prevalence, management and outcomes. Knee. 2006;13:111–117. doi: 10.1016/j.knee.2005.10.001. [DOI] [PubMed] [Google Scholar]