Abstract
End-stage liver disease is a major cause of morbidity and mortality among ethnic minorities. In the United States, ethnic minorities comprise approximately 30% of all adult liver transplantations performed annually. Several studies have suggested that ethnic populations differ with respect to access and outcomes in the pre- and post-transplantation setting. This paper will review the existing literature on ethnic variations in the adult liver transplantation population.
Keywords: Liver transplantation, ethnicity, end-stage liver disease
End-stage liver disease (ESLD) is a major cause of morbidity and mortality among ethnic minorities.1 Ethnic variations exist in the prevalence and natural history of liver disease, access to liver transplantation, and therapeutic outcomes post–liver transplantation. These differences are inter-related and present challenges that contribute to the health disparities observed in our diverse, multiethnic population. By discussing the existing literature on ethnic variations in liver transplantation, this paper will provide a better understanding of ethnic disparities in the liver transplantation population and address clinical implications of these disparities, where applicable. Due to inconsistent classification across published studies, ethnicity and race will be used interchangeably in this paper; categories will include: white, black, Hispanic, and Asian. The term “ethnic minorities” will refer to ethnicities and races other than white.
End-Stage Liver Disease in the Ethnic Minority Population
Although there are no population-based studies focusing on the prevalence of chronic liver disease among ethnic groups, indications for liver transplantation provide useful insight into these differences. According to data from the United Network for Organ Sharing (UNOS) registry, the etiology of liver disease in transplantation recipients varies by ethnicity (Table 1). Variations in the natural history and progression of liver disease—from compensated to decompensated cirrhosis (ie, ESLD)—are well documented in the literature. Several natural history studies have consistently shown clinical hepatic decompensation to be a significant predictor of a poor survival rate and, thus, an indication for liver transplantation. Prior to the implementation of the Model for End-Stage Liver Disease (MELD), the minimum criteria for being placed on the transplantation waiting list was a Child-Pugh-Turcotte score greater than 7 (status 3) and the presence of complications related to portal hypertension, which signify a worse prognosis and higher priority for orthotopic liver transplantation (status 2B).2
Table 1.
Etiology of Liver Disease in Liver Transplantation Recipients
| White | Hispanic | Black | Asian | |
|---|---|---|---|---|
| HCV | 29% | 36% | 33% | 18% |
| HBV | 3% | 4% | 4% | 26% |
| PSC/PBC | 13% | 7% | 12% | 4% |
| Alcohol | 15% | 13% | 6% | 3% |
| HCC | 8% | 12% | 9% | 22% |
| FHF | 5% | 5% | 12% | 7% |
| Other etiologies | 27% | 23% | 24% | 20% |
- FHF
fulminant hepatic failure
- HBV
hepatitis B virus
- HCC
hepatocellular carcinoma
- HCV
hepatitis C virus
- PBC
primary biliary cirrhosis
- PSC
primary sclerosing cholangitis
Reproduced from the United Network for Organ Sharing database.
Although there are no natural history studies focusing on the incidence of hepatic decompensation among ethnic groups, a retrospective analysis of the Nationwide Inpatient Sample (NIS) provides some insight into this population.3 In this analysis, there was a significantly higher incidence of hepatic encephalopathy in Hispanic and black patients at clinical presentation compared to white patients, whereas a higher incidence of ascites was observed in white patients. The reasons for the differences in encephalopathy and ascites are unknown.
With respect to variceal bleeding, the retrospective analysis of the NIS found a lower incidence in black patients than Hispanic or white patients.3 It is unclear whether the occurrence of variceal bleeding in this study population was related to a lower prevalence of esophageal and gastric varices in black patients. An interesting finding from the HALT-C trial was the reduced frequency of portal gastropathy and esophageal varices in black patients compared to non-black patients.4,5 Furthermore, the likelihood of developing esophageal varices in this study cohort after a 4-year follow-up period was lower in black patients than non-black patients; among non-black patients, there was a higher likelihood of this development in Hispanic patients compared to white patients.6 A study conducted by Jamal and associates reported a similar finding—a lower prevalence of esophageal varices and portal gastropathy in black patients—as well as a higher in-hospital mortality rate for esophageal variceal bleeding in this ethnic group.7 Because the latter study was not designed to identify specific factors related to increased mortality in this cohort, the exact reason for the reported ethnic difference in survival is unclear.
Access to Liver Transplantation
Access to a transplantation center is a prerequisite for obtaining lifesaving organ transplantation. Therefore, referral to a transplantation center for evaluation is the initial barrier in the transplantation activation process. In a retrospective study of a single-center veterans affairs cohort, black patients were less likely to be referred for liver transplantation evaluation.8 This finding is consistent with the study conducted by Eckhoff and colleagues, which reported a referral rate for blacks that was disproportionately lower than their representation in the hospital population.9 The reason for this ethnic disparity in liver transplantation referral is not clearly understood.
In addition to lower referral rates, delayed referral has been documented in ethnic minorities with ESLD. The severity of liver disease—as measured by the MELD score—is a surrogate marker for delayed referral. Several studies have identified a significant association between ethnicity and a high MELD score at the time of transplantation listing.10,11 In a recent UNOS analysis of a study cohort of black and white patients, black patients were more likely than white patients to be listed at high MELD scores.11
Despite these findings, the impact of ethnicity, socioeconomic status, and health insurance on referral patterns for liver transplantation has not been fully understood. According to the National Healthcare Disparities Report, health insurance is the key barrier to healthcare access among black and Hispanic patients.12 In a population-based study using the NIS database, black and Hispanic patients with cirrhosis were less likely to have private insurance—but more likely to be insured by Medicaid— than white patients.3 In a large cohort of potential liver transplantation candidates, Bryce and coworkers found a strong association between insurance status and the likelihood of referral or evaluation for liver transplanta-tion.13 In this study, potential candidates with commercial or private insurance were more likely to be referred and evaluated for liver transplantation. Although this study did not provide ethnic-specific data, it provides an insight into the critical role that health insurance plays in affecting access to liver transplantation.
For patients who complete the transplantation evaluation process and are added to the UNOS waiting list, there appear to be no significant ethnic differences in wait-list outcomes.11,14 This finding contrasts with reports from the pre-MELD era.15 Recent studies in the MELD era have not found a significant ethnic difference in wait-list outcomes, as measured by mortality prior to transplantation or removal from the waiting list due to being “too sick for transplantation.” Thus, the implementation of MELD—with its emphasis on disease severity—eliminated the previously observed ethnic disparity in wait-list outcomes.
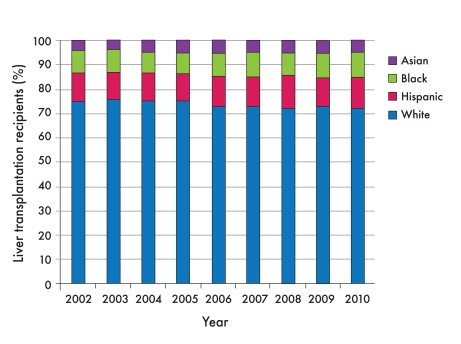
In addition, recent studies in the MELD era have shown that ethnic minorities no longer have lower transplantation rates.14 In fact, in the MELD era, there appears to be a slight increase in the percentage of black transplantation recipients (from 8.2% to 10.3%), a decrease among white patients (from 74% to 71%), and relatively stable percentages in Hispanic and Asian patients (Figure 1). Therefore, recent findings suggest that the implementation of MELD in the allocation system has led to improved access to liver transplantation among ethnic minorities; however, the impact of MELD on ethnic disparity at the transplantation activation stage remains undetermined.14,16
Figure 1.
Liver transplantation trends in the Model for End-Stage Liver Disease era (2002–2010).
Reproduced from the United Network for Organ Sharing database.
Liver Transplantation Outcomes
Several studies have reported disparities in liver transplantation outcomes for ethnic minorities with ESLD. As with other solid organ transplantations, differences in patient and graft survival rates among liver transplantation recipients have been well documented in the literature.17–19 Studies conducted before and after the implementation of MELD have consistently shown a decreased survival rate in black patients compared to other ethnic groups.20,21 The recent UNOS analysis of black, white, Hispanic, and Asian liver transplantation recipients revealed 5-year patient survival rates of 67%, 74%, 75%, and 78%, respectively, and 5-year graft survival rates of 60%, 69%, 70%, and 74%, respectively.22 Based on these findings, survival rates between Hispanic and white patients do not appear to differ, and the outcome of Asian patients is superior to all other ethnic groups. Therefore, the best survival rates are observed in Asian patients, while black patients have the worst survival rates, and Hispanic and white patients have intermediate survival rates. Due to the small number of recipients from other ethnic or racial groups (such as native Hawaiian, Pacific Islander, American Indian, or Alaskan native), these groups have not been included in most large studies. The reason for ethnic disparities in survival rates is not clearly understood. Interestingly, ethnic differences in survival rates are not observed in the pediatric liver transplantation population, possibly due to variations in underlying liver disease.23
In a retrospective analysis of the UNOS database, Roberts and associates found significant differences in survival rates based on the type of liver disease.24 In a recent study using the UNOS database, investigators conducted a comparative analysis of disease-specific survival rates among different racial and ethnic groups.21 In this study, 2-year overall survival rates (for both the patient and graft) were comparable for white, Hispanic, and black patients, except among transplantation recipients with hepatitis C virus (HCV) infection; in this group of recipients, there was a trend toward a lower survival rate among black patients. Furthermore, recurrent HCV infection was identified as the most common cause of graft failure in black patients compared to other ethnic groups.
The contributory role that response to antiviral therapy plays in the post-transplantation setting among transplantation recipients with HCV infection is unclear, as no large studies have specifically addressed the impact of ethnicity. In the pretransplantation population, it is well documented in the literature that black patients have a lower sustained virologic response (SVR) rate than other ethnic groups.25,26 However, in a small single-center study, ethnicity was not a predictor of SVR in the post-transplantation setting.27 The predictive value of the interleukin (IL)-28B polymorphism in the transplantation setting will also provide useful insight into the role of genomics in this population.
Recently, there has been growing interest in the role donor characteristics play in affecting outcomes among transplantation recipients with HCV infection. One such study implicated donor ethnicity as a significant determinant of post–liver transplantation outcomes among black transplantation recipients with HCV infection.28 This study found that black transplantation recipients with HCV infection had a worse graft survival rate with a white donor than a black donor (ie, race mismatch). Furthermore, it is noteworthy that 70% of black transplantation recipients in this large cohort study received white donor organs. If these results are validated, they may impact the current allocation scheme for liver transplantation candidates with HCV infection.
In contrast to transplantation recipients infected with HCV, recipients with hepatitis B virus (HBV) infection show no ethnic differences in overall survival rates, although white patients had a higher HBV infection recurrence rate than Asian and black patients in 1 study.29 Unfortunately, HBV outcomes in the Hispanic liver transplantation population are unknown, as Hispanic patients were not included in this study cohort. The significant improvements in post–liver transplantation outcomes observed in recipients with HBV infection are primarily related to the therapeutic advances in antiviral therapy for this infection.30 Future research evaluating the impact of direct-acting antiviral agents in transplantation recipients—as well as a better understanding of the role of genomics (eg, the IL-28B polymorphism)—is expected to result in better outcomes, particularly among black patients, who are disproportionately affected by HCV infection.31
Immunosuppressive Therapy in Ethnic Minorities
In addition to future studies directed at HCV therapeutic agents, determining the role of immunosuppressive therapies in this population is also of utmost importance. Studies focusing on pharmacokinetic parameters of commonly used immunosuppressive drugs have provided useful insights into possible mechanisms contributing to lower survival rates in the post-transplantation setting. Despite the paucity of randomized controlled trials addressing immunosuppressive drugs in ethnic minorities, several single-center studies have consistently shown lower trough levels of the currently available calcineurin inhibitors (tacrolimus and cyclosporine) in transplantation recipients of African descent. For example, among transplantation recipients receiving a specified dose of cyclosporine, the maximum concentration and area under the curve are notably lower in black patients than white patients.32,33 The pharmacokinetic study conducted by Dirks and colleagues reported a 20–50% reduction in cyclosporine bioavailability for black patients compared to other ethnic groups; as a result, higher doses are required to reach desired trough levels.34 Similar findings have been documented for transplantation recipients on tacrolimus-based regimens.35,36
Reports of ethnic variations in the ability of transplantation recipients to mount an immune response (ie, immunocompetence) add a different perspective to the challenges of immunosuppressive therapy in this population. In a single-center study, Nagashima and coworkers used in vitro immunocompetence tests to measure the effects of immunosuppressive drugs on transplantation recipients.37 Among transplantation recipients on tacrolimus-based regimens, a reduced immunosuppressive effect was observed in black patients compared to white patients. The impaired immunosuppressive effect of tacrolimus is likely related to the enhanced immune responsiveness observed in black transplantation recipients, which is thought to invariably contribute to the increased risk of allograft rejection. Furthermore, Maggard and associates reported a higher incidence of acute rejection among black liver transplantation recipients compared to patients of other ethnicities, but the exact reason for this finding was not determined.38 Despite the hypothesis that lower trough levels increase the risk of allograft rejection, several published studies show conflicting data on the correlation between trough levels of calcineurin inhibitors and episodes of allograft rejection. Nonetheless, a recent study found that, although there was no correlation with trough blood concentrations of total tacrolimus, a significant association was observed between unbound or free tacrolimus concentrations and the occurrence of allograft rejection among liver transplantation recipients.39
These observed ethnic differences in trough levels raise questions regarding the role of drug metabolizing enzymes (DMEs) in this population. As a result, there has been growing interest in the effect of genetic variations in DMEs among different ethnic groups. The DMEs predominantly involved in the metabolism of calcineurin inhibitors are the cytochrome P450 3A enzymes (CYP3A4 and CYP3A5). Variations in the DNA sequence of CYP3A4 and CYP3A5 (ie, polymorphisms) have been widely studied, particularly in relation to calcineurin inhibitors. Reports of ethnic variations in the frequency of the occurrence of CYP3A4 and CYP3A5 have resulted in renewed interest in the potential association between ethnicity and pharmacogenomics. For example, the CYP3A5 polymorphism (CYP3A5*1) occurs in 55% of blacks, 10–40% of whites, and 33% of Asians in the general population.40 Transplantation recipients with CYP3A5*1 who take tacrolimus have a higher clearance resulting in lower trough levels.41 Clinically, this translates into a 2.3-fold difference in dose requirements. Therefore, on average, recipients with CYP3A5*1 require a higher dose of tacrolimus to achieve target trough levels. If these findings are confirmed in large, randomized, controlled, prospective trials, the identification of the CYP3A5 polymorphism will be a useful pretransplantation risk stratification tool, particularly among ethnic groups in which the polymorphism occurs at a disproportionate frequency.
Summary
Heightened awareness and understanding of the ethnic variations in liver transplantation are essential for physicians involved in the care of these recipients. This paper summarizes the complex relationship between ethnicity and liver disease in the liver transplantation population and highlights the lack of prospective studies that address ethnic disparities in this field. Future research designed to identify factors that impact the transplantation activation process—as well as clinical trials aimed at improving therapeutic outcomes and, ultimately, survival rates—will be invaluable.
References
- 1.Stinson FS, Grant BF, Dufour MC. The critical dimension of ethnicity in liver cirrhosis mortality statistics. Alcohol Clin Exp Res. 2001;25:1181–1187. [PubMed] [Google Scholar]
- 2.Lucey MR, Brown KA, Everson GT, et al. Minimal criteria for placement of adults on the liver transplant waiting list: a report of a national conference organized by the American Society of Transplant Physicians and the American Association for the Study of Liver Diseases. Liver Transpl Surg. 1997;3:628–637. doi: 10.1002/lt.500030613. [DOI] [PubMed] [Google Scholar]
- 3.Nguyen GC, Segev DL, Thuluvath PJ. Racial disparities in the management of hospitalized patients with cirrhosis and complications of portal hypertension: a national study. Hepatology. 2007;45:1282–1289. doi: 10.1002/hep.21580. [DOI] [PubMed] [Google Scholar]
- 4.Sanyal AJ, Fontana RJ, Di Bisceglie AM, et al. HALT-C Trial Group. The prevalence and risk factors associated with esophageal varices in subjects with hepatitis C and advanced fibrosis. Gastrointest Endosc. 2006;64:855–864. doi: 10.1016/j.gie.2006.03.007. [DOI] [PubMed] [Google Scholar]
- 5.Fontana RJ, Sanyal AJ, Mehta S, et al. Portal hypertensive gastropathy in chronic hepatitis C patients with bridging fibrosis and compensated cirrhosis: results from the HALT-C trial. Am J Gastroenterol. 2006;101:983–992. doi: 10.1111/j.1572-0241.2006.00461.x. [DOI] [PubMed] [Google Scholar]
- 6.Fontana RJ, Sanyal AJ, Ghany MG, et al. HALT-C Trial Group. Factors that determine the development and progression of gastroesophageal varices in patients with chronic hepatitis C. Gastroenterology. 2010;138:2321–2331. doi: 10.1053/j.gastro.2010.02.058. 2331.e1–2331.e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jamal MM, Samarasena JB, Hashemzadeh M. Decreasing in-hospital mortality for oesophageal variceal hemorrhage in the USA. Eur J Gastroenterol Hepatol. 2008;20:947–955. doi: 10.1097/MEG.0b013e32830280c7. [DOI] [PubMed] [Google Scholar]
- 8.Julapalli VR, Kramer JR. El-Serag HB; American Association for the Study of Liver. Diseases, Evaluation for liver transplantation: adherence to AASLD referral guidelines in a large Veterans Affairs center. Liver Transpl. 2005;11:1370–1378. doi: 10.1002/lt.20434. [DOI] [PubMed] [Google Scholar]
- 9.Eckhoff DE, McGuire BM, Young CJ, et al. Race: a critical factor in organ donation, patient referral and selection, and orthotopic liver transplantation? Liver Transpl Surg. 1998;4:499–505. doi: 10.1002/lt.500040606. [DOI] [PubMed] [Google Scholar]
- 10.Kemmer N, Zacharias V, Kaiser TE, Neff GW. Access to liver transplantation in the MELD era: role of ethnicity and insurance. Dig Dis Sci. 2009;54:1794–1797. doi: 10.1007/s10620-008-0567-5. [DOI] [PubMed] [Google Scholar]
- 11.Moylan CA, Brady CW, Johnson JL, Smith AD, Tuttle-Newhall JE, Muir AJ. Disparities in liver transplantation before and after introduction of the MELD score. JAMA. 2008;300:2371–2378. doi: 10.1001/jama.2008.720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Agency for Healthcare Research and Quality Web site. US Department of Health and Human Services. http://www.ahrq.gov.
- 13.Bryce CL, Angus DC, Arnold RM, et al. Sociodemographic differences in early access to liver transplantation services. Am J Transplant. 2009;9:2092–2101. doi: 10.1111/j.1600-6143.2009.02737.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Volk ML, Choi H, Warren GJ, Sonnenday CJ, Marrero JA, Heisler M. Geographic variation in organ availability is responsible for disparities in liver transplantation between Hispanics and Caucasians. Am J Transplant. 2009;9:2113–2118. doi: 10.1111/j.1600-6143.2009.02744.x. [DOI] [PubMed] [Google Scholar]
- 15.Reid AE, Resnick M, Chang Y, Buerstatte N, Weissman JS. Disparity in use of orthotopic liver transplantation among blacks and whites. Liver Transpl. 2004;10:834–841. doi: 10.1002/lt.20174. [DOI] [PubMed] [Google Scholar]
- 16.Mathur AK, Schaubel DE, Gong Q, Guidinger MK, Merion RM. Racial and ethnic disparities in access to liver transplantation. Liver Transpl. 2010;16:1033–1040. doi: 10.1002/lt.22108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Luan FL, Kommareddi M, Cibrik DM, Samaniego M, Ojo AO. Influence of recipient race on the outcome of simultaneous pancreas and kidney transplantation. Am J Transplant. 2010;10:2074–2081. doi: 10.1111/j.1600-6143.2010.03211.x. [DOI] [PubMed] [Google Scholar]
- 18.Fan PY, Ashby VB, Fuller DS, et al. Access and outcomes among minority transplant patients, 1999-2008, with a focus on determinants of kidney graft survival. Am J Transplant. 2010;10((4 pt 2)):1090–1107. doi: 10.1111/j.1600-6143.2009.03009.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Allen JG, Weiss ES, Arnaoutakis GJ, et al. The impact of race on survival after heart transplantation: an analysis of more than 20,000 patients. Ann Thorac Surg. 2010;89:1956–1963; discussion 1963-1964. doi: 10.1016/j.athoracsur.2010.02.093. [DOI] [PubMed] [Google Scholar]
- 20.Nair S, Eustace J, Thuluvath PJ. Effect of race on outcome of orthotopic liver transplantation: a cohort study. Lancet. 2002;359:287–293. doi: 10.1016/S0140-6736(02)07494-9. [DOI] [PubMed] [Google Scholar]
- 21.Ananthakrishnan AN, Saeian K. Racial differences in liver transplantation outcomes in the MELD era. Am J Gastroenterol. 2008;103:901–910. doi: 10.1111/j.1572-0241.2008.01809.x. [DOI] [PubMed] [Google Scholar]
- 22.Thuluvath PJ, Guidinger MK, Fung JJ, Johnson LB, Rayhill SC, Pelletier SJ. Liver transplantation in the United States, 1999-2008. Am J Transplant. 2010;10((4 pt 2)):1003–1019. doi: 10.1111/j.1600-6143.2010.03037.x. [DOI] [PubMed] [Google Scholar]
- 23.Neff GW, Kemmer N, Kaiser T, Zacharias V, Majoras N, Safdar K. Outcomes in adult and pediatric liver transplantation among various ethnic groups. Transplant Proc. 2007;39:3204–3206. doi: 10.1016/j.transproceed.2007.09.031. [DOI] [PubMed] [Google Scholar]
- 24.Roberts MS, Angus DC, Bryce CL, Valenta Z, Weissfeld L. Survival after liver transplantation in the United States: a disease-specific analysis of the UNOS database. Liver Transpl. 2004;10:886–897. doi: 10.1002/lt.20137. [DOI] [PubMed] [Google Scholar]
- 25.Muir AJ, Bornstein JD, Killenberg PG Atlantic Coast Hepatitis Treatment Group. Peginterferon alfa-2b and ribavirin for the treatment of chronic hepatitis C in blacks and non-Hispanic whites. N Engl J Med. 2004;350:2265–2271. doi: 10.1056/NEJMoa032502. [DOI] [PubMed] [Google Scholar]
- 26.Conjeevaram HS, Fried MW, Jeffers LJ, et al. Peginterferon and ribavirin treatment in African American and Caucasian American patients with hepatitis C genotype 1. Gastroenterology. 2006;131:470–477. doi: 10.1053/j.gastro.2006.06.008. [DOI] [PubMed] [Google Scholar]
- 27.Hanouneh IA, Miller C, Aucejo F, Lopez R, Quinn MK, Zein NN. Recurrent hepatitis C after liver transplantation: on-treatment prediction of response to peginterferon/ribavirin therapy. Liver Transpl. 2008;14:53–58. doi: 10.1002/lt.21312. [DOI] [PubMed] [Google Scholar]
- 28.Pang PS, Kamal A, Glenn JS. The effect of donor race on the survival of black Americans undergoing liver transplantation for chronic hepatitis C. Liver Transpl. 2009;15:1126–1132. doi: 10.1002/lt.21835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bzowej N, Han S, Degertekin B, et al. National Institutes of Health Hepatitis B Virus Orthotopic Liver Transplantation Study Group. Liver transplantation outcomes among Caucasians, Asian Americans, and African Americans with hepatitis B. Liver Transpl. 2009;15:1010–1020. doi: 10.1002/lt.21759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kim WR, Poterucha JJ, Kremers WK, Ishitani MB, Dickson ER. Outcome of liver transplantation for hepatitis B in the United States. Liver Transpl. 2004;10:968–974. doi: 10.1002/lt.20217. [DOI] [PubMed] [Google Scholar]
- 31.Charlton MR, Thompson A, Veldt BJ, et al. Interleukin-28B polymorphisms are associated with histological recurrence and treatment response following liver transplantation in patients with hepatitis C virus infection. Hepatology. 2011;53:317–324. doi: 10.1002/hep.24074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Min DI, Lee M, Ku YM, Flanigan M. Gender-dependent racial difference in disposition of cyclosporine among healthy African American and white volunteers. Clin Pharmacol Ther. 2000;68:478–486. doi: 10.1067/mcp.2000.111255. [DOI] [PubMed] [Google Scholar]
- 33.Isaacs RB, Nock SL, Spencer CE, et al. Racial disparities in renal transplant outcomes. Am J Kidney Dis. 1999;34:706–712. doi: 10.1016/S0272-6386(99)70397-5. [DOI] [PubMed] [Google Scholar]
- 34.Dirks NL, Huth B, Yates CR, Meibohm B. Pharmacokinetics of immunosuppressants: a perspective on ethnic differences. Int J Clin Pharmacol Ther. 2004;42:701–718. doi: 10.5414/cpp42701. [DOI] [PubMed] [Google Scholar]
- 35.Andrews PA, Sen M, Chang RW. Racial variation in dosage requirements of tacrolimus. Lancet. 1996;348:1446. doi: 10.1016/S0140-6736(04)70087-2. [DOI] [PubMed] [Google Scholar]
- 36.Mancinelli LM, Frassetto L, Floren LC, et al. The pharmacokinetics and metabolic disposition of tacrolimus: a comparison across ethnic groups. Clin Pharmacol Ther. 2001;69:24–31. doi: 10.1067/mcp.2001.113183. [DOI] [PubMed] [Google Scholar]
- 37.Nagashima N, Watanabe T, Nakamura M, Shalabi A, Burdick JF. Decreased effect of immunosuppression on immunocompetence in African Americans after kidney and liver transplantation. Clin Transplant. 2001;15:111–115. doi: 10.1034/j.1399-0012.2001.150207.x. [DOI] [PubMed] [Google Scholar]
- 38.Maggard M, Goss J, Ramdev S, Swenson K, Busuttil RW. Incidence of acute rejection in African-American liver transplant recipients. Transplant Proc. 1998;30:1492–1494. doi: 10.1016/s0041-1345(98)00330-3. [DOI] [PubMed] [Google Scholar]
- 39.Zahir H, McCaughan G, Gleeson M, Nand RA, McLachlan AJ. Factors affecting variability in distribution of tacrolimus in liver transplant recipients. Br J Clin Pharmacol. 2004;57:298–309. doi: 10.1046/j.1365-2125.2003.02008.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lamba JK, Lin YS, Schuetz EG, Thummel KE. Genetic contribution to variable human CYP3A-mediated metabolism. Adv Drug Deliv Rev. 2002;54:1271–1294. doi: 10.1016/s0169-409x(02)00066-2. [DOI] [PubMed] [Google Scholar]
- 41.MacPhee IA, Fredericks S, Tai T, et al. The influence of pharmacogenetics on the time to achieve target tacrolimus concentrations after kidney transplantation. Am J Transplant. 2004;4:914–919. doi: 10.1111/j.1600-6143.2004.00435.x. [DOI] [PubMed] [Google Scholar]