Abstract
Irritable bowel syndrome (IBS) is a disabling functional gastrointestinal disorder, which serves as a model for abdominal pain syndromes. An association between intimate partner violence and IBS has been shown among Caucasian women in the industrialized world. To determine whether this relationship transcends cultural boundaries, we conducted a population-based, cross-sectional survey in Nicaragua, using the innovative Health and Demographic Surveillance System in the León province. Women who had experienced physical intimate partner violence had significantly increased risk of IBS (OR 2.08, 95% CI, 1.35, 3.21), as did those who had experienced sexual intimate partner violence (OR 2.85, 95% CI 1.45, 5.59). These findings argue for intimate partner violence screening among Latina women with IBS.
Keywords: violence, abuse, irritable bowel syndrome
INTRODUCTION
Intimate partner violence is associated with long-term health problems, beyond the immediate physical trauma. Individuals who have experienced intimate partner violence have higher rates of depression, post-traumatic stress disorder, chronic pelvic pain, migraine syndromes, low birth weight deliveries, sexually transmitted infections, HIV/AIDS, and even common colds and influenza (Lesserman, Drossman, & Hu, 1998; Pico-Alfonso et al., 2006; Valladares, Ellsberg, Peña, Högberg, & Persson, 2002; Silverman, Decker, Saggurti, Balaiah, & Raj, 2008; Letourneau, Holmes, & Chasedunn-Roark, 1999; Coker, Smith, Bethea, King, & McKeown, 2000; Talley, Helgeson, Zinsmeister, & Melton, 1994). Self-reported gastrointestinal symptoms are also more prevalent among those who have experienced intimate partner violence, including symptoms of irritable bowel syndrome (IBS) and dyspepsia (Talley, Fett, & Zinmeister, 1995).
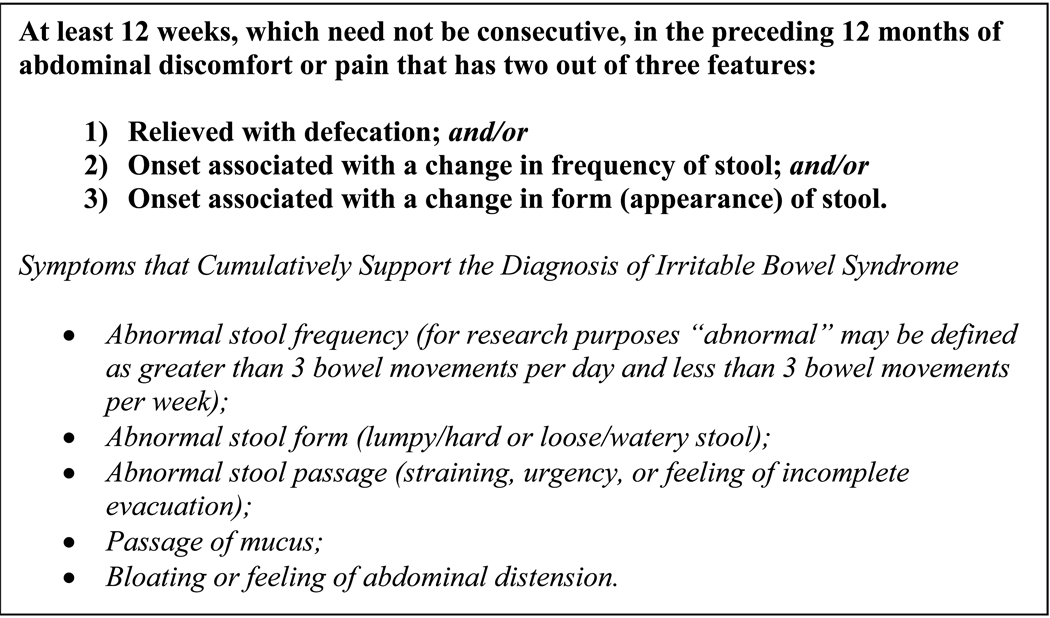
IBS is one of the most common gastrointestinal disorders with a global prevalence ranging between 4% and 24% (Kang, 2005). There are no known population-based studies of IBS prevalence in Latin America or among Latinos in the US. IBS is a non-inflammatory disease of the gastrointestinal tract within the family of functional gastrointestinal disorders, characterized by recurrent abdominal pain or discomfort associated with altered bowel function (constipation, diarrhea, or constipation alternating with diarrhea) (See Figure 1). IBS can be debilitating, resulting in a lower quality of life, lower work productivity, and psychological distress (ten Berg, Goettsch, van den Boom, Smout, & Herings, 2006; Luscombe, 2000; Maxion-Bergemann, Thielecke, Abel, & Bergemann, 2006). In addition, IBS often leads to increased health care utilization, including diagnostic procedures, medications, and surgery (Lesserman & Drossman, 2007). For example, in the U.S., IBS accounts for over 2.1 million outpatient visits annually (Shaheen, Hansen, & Morgan, 2006).
Figure 1.
Diagnostic Criteria* for IBS
*In the absence of structural or metabolic abnormalities to explain the symptoms.
Reprinted with permission from the Rome Foundation (Thompson et al., 2000, p.360).
IBS serves as a model for the abdominal pain syndromes. In the evolving biopsychosocial model, complex gene-environment interactions are responsible for the development and maintenance of IBS. These involve the “Brain-Gut Axis”, the interplay between the gastrointestinal mucosa, the enteric nervous system, and the central nervous system. Both physiologic factors (motility, sensation, bacterial flora) and psychosocial factors (psychological state, stressors, coping mechanisms, social support) modulate these interactions (Kanazawa et al., 2008; Drossman, 2006). Various forms of trauma stimulate the hypothalamic-pituitary-adrenal axis (Inslicht et al., 2006); this dysregulated axis and the enteric nervous system are thought to be involved in the pathogenesis and maintenance of IBS and related functional gastrointestinal disorders (Dinan et al, 2006; Heitkemper et al, 1996; Fukudo, 2007).
Intimate partner violence has been proposed as an important etiologic factor within the IBS biopsychosocial model. Over one half of patients being treated for functional bowel disorders in specialty clinics report intimate partner violence (Drossman et al., 1990); these patients carry a poorer prognosis for their functional bowel disease (Drossman et al., 1990; Walker, Gelfand, Gelfand, & Katon, 1995). Prior studies that have examined intimate partner violence as a risk factor for IBS have focused on Caucasian subjects in the industrialized world. There are no studies of this association in other racial or ethnic groups, or in the developing world. It is unclear if the meaning and impact that violence has on an individual is culturally-determined or universal.
We examined the relation between intimate partner violence and IBS in a population of Central American women, using a population-based study design. The University of Nicaragua, León has performed pioneering work defining the prevalence of intimate partner violence in Nicaragua, which in turn facilitated national legislation (Ellsberg, Peña, Herrera, Liljestrand, & Winkvist, 1999).
Studying the relationship between IBS and intimate partner violence in a non-Caucasian, non-industrialized population provides information on whether this relationship transcends cultural boundaries. Also, as 72% of the 45.4 million U.S. Latinos have their origins in Mesoamerica, (Mexico and Central America), these findings may have implications for the U.S Latina population (Pew Hispanic Center, 2007).
METHODS
Study Design
We conducted a cross-sectional study in León, Nicaragua, using a random representative sample from the established Health and Demographic Surveillance Site-León (HDSS-León) (Peña, Pérez, Meléndez, Källestål, & Persson, 2008). HDSS-León, established in 1993, includes 11, 000 households, 24% of the León province’s estimated population of 176,915. This is the only member in Latin America of the INDEPTH network, an international network of surveillance systems in developing nations (INDEPTH demographic network, 2009). Approximately 95% of the region’s population is of Hispanic mestizo origin. The population distribution is relatively young, with a median age of 26 years.
All consenting adult residents of León municipality within the surveillance system over age 18 were considered for inclusion. The target enrollment was one thousand women, with random sampling to represent the HDSS-León population distribution. Exclusion criteria included having a history of gastrointestinal disease (e.g., inflammatory bowel disease, gastrointestinal cancer), major abdominal surgery, hospitalization within the past 3 months, or significant comorbidities. Interviews were conducted privately in participants’ homes using trained female interviewers.
Rome II Modular Questionnaire
The Rome II Modular Questionnaire for the functional gastrointestinal disorders, based on Rome II diagnostic criteria, was used for IBS case identification (Thompson et al., 2000, p. 673–4). The Rome II questionnaire was the standard international study instrument during the study period. It was created through international consensus (Drossman, 1999) and has been validated in several studies (Kwan, et al. 2003; Caplan, Walker, & Rasquin, 2005). Case status was confirmed by physicians, who were blinded to the survey results.
The Conflict Tactics Scales
Physical and sexual intimate partner violence and childhood sexual abuse were assessed using the physical aggression scale of the Conflict Tactics Scales (Straus, 1979). This scale has been used extensively in the past, including in this population (Ellsberg, et al, 1999b) and is considered to have construct validity and reliability in the evaluation of violence (Barling, O’Leary, Jouriles, Vivian, & MacEwen, 1987; Smith, 1994). The Universidad Nacional Autónoma de Nicaragua, León study team has extensive experience with the evaluation of intimate partner violence and related study instruments (Valladares, Peña, Persson, & Högberg, 2005; Ellsberg, Caldera, Herrera, Winkvist, & Kullgren, 1999).
A respondent was considered to have experienced physical intimate partner violence if she had been slapped, punched, kicked, pushed, cornered, strangled, burned, or threatened with a pistol or knife by a current or past intimate partner. A respondent was considered to have experienced sexual intimate partner violence if a current or past intimate partner coerced or forced her to perform a sexual act against her will, to engage in a sexual act out of fear, or to engage in a sexual act she found humiliating or that she was injured by, whether or not the act was completed. A respondent was considered to have experienced childhood sexual abuse if any of the above sexual activities occurred before the age of 12.
Sociodemographic Variables
Socioeconomic status was assessed by a validated poverty index, the Unsatisfied Basic Need Assessment (Renzi & Agurto 1993). The Unsatisfied Basic Need Assessment is a scale from 0 to 4 that is based on four indicators: household condition, water and sanitation services, school enrollment, and number of dependents in the household. This scale has been adapted to specific conditions in Nicaragua and has been used in prior studies (Peña, Wall & Persson, 2000; Zelaya et al., 1996). A score of 0 or 1 implies non-poverty by Nicaraguan standards, with basic needs being met, while 4 suggests severe poverty. Additional demographic information included respondent’s age, marital status, educational attainment, and religion. In analysis, marital status was dichotomized to “in a relationship” or “not in a relationship” and religion was dichotomized to “identifies a religion” or “does not identify a religion”.
Data Analysis
We calculated crude and adjusted ORs for the odds of IBS using STATA version 9 statistical software (College Station, TX). Three models were created to assess the association between IBS and the three main factors of interest: physical intimate partner violence, sexual intimate partner violence, or childhood sexual abuse. We adjusted for age, socioeconomic status (poverty index), and relationship status. The proportion of IBS that could be attributed to either physical or sexual intimate partner violence (assuming a causal relationship) was calculated using the formula for population-attributable risk proportion: [(OR-1)/(OR)]fe, where fe is the proportion of cases exposed to intimate partner violence. Quality control measures included double data entry, interviewer observation (10%), and the random reviews of questionnaire data quality (10%). The current study was approved by the institutional review boards of the University of North Carolina, Chapel Hill and the Universidad Nacional Autónoma de Nicaragua, León. Permissions were obtained from the Rome Foundation for the use of the Rome II Modular Questionnaire.
RESULTS
Nearly one thousand women (n=962) were enrolled in the current investigation, with complete data available on 960 participants. There were 151 cases of IBS (15.7%) identified. The women ranged in age from 18 to 65, with a mean age of 37 (Table 1). Over half (56.1%) were either married or in a stable relationship and 92.1% identified with a religion. Two-thirds (66.4%) reported having their basic needs met (poverty index 0 or 1), and 60.2% had attained schooling beyond the elementary level. The study participation refusal rate was 2%.
Table 1.
Characteristics of the Sample
| Among all women n=962 |
Among women with IBS n=151 |
Among women without IBS n=811 |
p-value for difference between women with and without IBS |
|
|---|---|---|---|---|
| Characteristic | % or mean (n or sd) | % or mean (n or sd) | % or mean (n or sd) | |
| Age (years) | 37 (sd +/−13) | 38 (sd +/− 13) | 37 (sd +/− 13) | 0.525 |
| Relationship status: in a relationship |
56.1% (540) | 59.6% (90) | 55.5% (450) | 0.876 |
| Identifies a religion | 92.1% (886) | 94.0% (142) | 91.7% (744) | 0.926 |
| Poverty index | ||||
| Basic needs met (0,1) | 66.4% (639) | 68.9% (104) | 66.0% (535) | 0.771 |
| Moderate poverty (2,3) | 29.9% (288) | 28.5% (43) | 30.2% (245) | |
| Severe poverty (4) | 3.6% (35) | 2.6% (4) | 3.8% (31) | |
| Education | ||||
| 6th grade or less | 39.8% (383) | 34.4% (52) | 40.8% (331) | 0.220 |
| 7th through 12th grade | 41.5% (399) | 47.7% (72) | 40.3% (327) | |
| Beyond 12th grade | 18.7% (180) | 17.9% (27) | 18.9% (153) | |
| Irritable bowel syndrome | 15.7% (151) | 100.0% (151) | 0.0% (0) | N/A |
IBS= Irritable bowel syndrome, sd= Standard deviation, N/A= Not applicable
Overall, all forms of intimate partner violence were common (Table 2): 14.8% of the women reported having experienced physical violence, 4.4% reported sexual violence, and 7.5% reported childhood sexual abuse. One fifth of women (19.4%) reported at least one form of violence. Nearly all of the women (90.5%) who reported sexual intimate partner violence also reported physical intimate partner violence.
Table 2.
Prevalence of Violence Among Women With and Without Irritable Bowel Syndrome
| Among all women n=962 |
Among women with IBS n=151 |
Among women without IBS n=811 |
p-value for difference between women with and without IBS |
|
|---|---|---|---|---|
| Type of Violence | %(n) | %(n) | %(n) | %(n) |
| Physical intimate partner violence | 14.8% (142) | 23.8% (36) | 13.1% (106) | 0.001 |
| Sexual intimate partner violence | 4.4% (42) | 9.3% (14) | 3.5% (28) | 0.001 |
| Sexual abuse prior to age 12 | 7.5% (72) | 11.3% (17) | 6.8% (55) | 0.056 |
| Any of above types of violence | 19.4% (186) | 31.1% (47) | 17.2% (139) | <0.001 |
IBS=irritable bowel syndrome
Women who reported physical intimate partner violence and childhood sexual abuse were more likely to be living in poverty. There were no statistically significant differences in age, religion, or educational attainment between women with and without physical intimate partner violence. There were no statistically significant differences in age, relationship status, poverty index, religion, or educational attainment between women with and without IBS.
Relationship Between Intimate Partner Violence and IBS
A strong relationship was observed between IBS and prior exposure to violence, which was relatively consistent across the types of violence. A significantly higher percentage of women with IBS (23.8%) had experienced physical intimate partner violence, versus women without IBS (13.1%, p=0.001) (Table 2). In parallel, 9.3% of women with IBS versus 3.5% of women without IBS had experienced sexual intimate partner violence (p=0.001). Finally, 11.3% of women with IBS vs. 6.8% of women without IBS had experienced childhood sexual abuse (p=0.056). In all, 31.1% of women with IBS had experienced either intimate partner violence or childhood sexual abuse. Those who had experienced physical intimate partner violence had 2.08 (95% CI: 1.35, 3.21) times the odds of IBS after adjusting for sociodemographic factors: age, poverty index, and marital status (Table 3). Those who had experienced sexual intimate partner violence had 2.85 (95% CI: 1.45, 5.59) times the odds of IBS, after adjustment. Those who experienced childhood sexual abuse had 1.82 (95% CI 1.02, 3.25) times the odds of IBS after adjustment.
Table 3.
Relationship Between Violence and Irritable Bowel Syndrome
| Risk Factor | Unadjusted OR (95% CI) | Adjusted OR* (95% CI) |
|---|---|---|
| Physical intimate partner violence | 2.08 (1.36, 3.18) | 2.08 (1.35, 3.21) |
| Sexual intimate partner violence | 2.85 (1.46, 5.55) | 2.85 (1.45, 5.59) |
| Sexual abuse prior to age 12 | 1.74 (0.98, 3.09) | 1.82 (1.02, 3.25) |
| Any of above types of violence | 2.18 (1.47, 3.22) | 2.22 (1.50, 3.32) |
Adjusted by age, poverty index, and marital status
The population-attributable risk proportion of IBS that could be attributed to intimate partner violence was 15.6%; which increases to 17.1% if childhood sexual abuse is also included.
DISCUSSION
Our population-based study suggests that intimate partner violence is associated with irritable bowel syndrome in this Central America population. This is the first study of this relationship among Latinas and in a developing country, where perceptions and manifestations of violence and disease may be different than in a Caucasian population in the industrialized world. Our findings are consistent with other studies of this association among Caucasians in both the United States and Australia (Talley et al., 1994; Talley, Boyce, & Jones, 1998).
In all, 31.1% of women with IBS had experienced either intimate partner or childhood sexual violence. We found that the odds of physical intimate partner violence among women with IBS was about twice that of women without IBS. Sexual intimate partner violence, which may be considered one of the more significant exposures to intimate partner violence, had a stronger relationship, nearly a factor of three. Assuming a causal relationship of this association, 15.6% of IBS among the women in our sample could be attributed to intimate partner violence.
Our findings also support the reality of adult chronic health and pain syndromes resulting from childhood sexual abuse. The relationship between IBS and childhood sexual abuse was statistically significant, although of weaker magnitude. This may reflect a true weaker association or a reporting bias: participants may have been more reluctant to reveal a history of childhood sexual abuse, which is often perpetrated by someone in the child’s close social environment. The association between IBS and childhood sexual abuse is consistent with prior research, suggesting that childhood abuse is associated with various chronic health problems in adulthood, including depression, sexually transmitted diseases, alcoholism, and tobacco abuse (Dube, Felitti Dong, Giles, & Anda, 2003).
As intimate partner violence is prevalent among women of all racial and ethnic groups (Bangdiwala et al., 2004; McFarlane, Groff, O’Brien, & Watson, 2005; Field & Caetano, 2004), a universal association between intimate partner violence and IBS may have broad implications, especially when IBS is considered a model for abdominal pain syndromes. Future studies among other racial and ethnic groups are warranted to confirm these observations.
Our study, using a population-based sample in Nicaragua, more specifically investigated the relationship between intimate partner violence and IPV among Latinas. Latino ethnicity is by no means a homogeneous category, as Latinos originate from over 20 countries, each with a distinct culture. In addition, Latinos in the U.S. have varying degrees of acculturation into the mainstream culture. However, Latinos do share much in common, including a common language, a shared history of colonization, and core cultural values, such as dependence on the extended family versus the individual (familismo) and the importance of personal relationships (personalismo) (Bernal, & Domenech Rodríguez, 2009, Bernal, Cuma-Aviles, & Saez-Santiago, 2006). Furthermore, 95% of the study’s participants were of mestizo race, which is predominant in Mesoamerica. Although it was hypothesized that these complex cultural and racial factors may influence the individual’s response to intimate partner violence, our findings showed a strikingly similar relationship between intimate partner violence and IBS as in Caucasian women in the industrialized world.
The findings further support our current understanding of the pathophysiology of IBS, which encompasses a biopsychosocial disease etiology model (Drossman, 2006). Although the exact mechanism for the relationship between intimate partner violence and IBS is unclear, investigators highlight the link between violence-related stress and neuroendocrine signaling (Leserman, et al., 2007; Ellsberg, et al., 1999a; Austin & Leader, 2000). Episodes of intimate partner violence stimulate the hypothalmamic pituitary adrenal access, which in turn is thought to be involved with the pathogenesis and maintenance of IBS. (Dinan et al, 2006; Heitkemper et al,1996; Fukudo, 2007).
A lower prevalence of lifetime intimate partner violence was found in this sample (20%) as compared with a prior cohort study carried out with pregnant women in the same setting, which reported a 54% lifetime prevalence of intimate partner violence (Valladares et al., 2005). Despite our use of an international validated scale, and that our interviewers had previous experience with the assessment of intimate partner violence, the main focus of the study was not intimate partner violence but gastrointestinal disorders. It has been previously shown that studies primarily designed for other purposes and not focused solely on violence are more likely to underestimate the prevalence of intimate partner violence (Ellsberg, Heise, Peña, Agurto, & Winkvist, 2001).
Although using a population-based sample allows us to effectively examine this relationship in a community setting, it may limit our ability to generalize our findings to other groups of Latinas, both in their native countries and as immigrants to the US. As discussed above, we recognize that there may be some differences in this relationship related to country-of-origin.
The study’s findings may have both clinical and public health implications. First, the findings provide support for screening patients, with a diagnosis of IBS for intimate partner violence. Positive screening would prompt counseling and appropriate referral. From a public health standpoint, the findings support the ongoing intimate partner violence prevention efforts in Nicaragua and Mesoamerica. Also, while there may be differences between the sampled Nicaraguan population and the U.S. Latina population, these results may be generalizable to recent immigrant populations from Mesoamerica in the U.S. Efforts for prevention of intimate partner violence at the population level should be considered in an effort to prevent adverse health outcomes, including gastrointestinal diseases.
CONCLUSIONS
This is the first study to show an association between intimate partner violence and IBS in the developing world, and in a non-Caucasian population. Future studies in other populations may confirm the strength of this relationship. Our findings support screening for intimate partner violence among women with IBS in this population, as well as continued efforts to prevent intimate partner violence in Central America.
ACKNOWLEDGEMENTS
We would like to acknowledge Magdaly Torres, Jacobo Morales, Wilton Pérez and the staff of the Centro de Investigación en Demografia y Salud (CIDS) for their contributions to this study.
This study was supported by a grant from the Rome Foundation, the Centro de Investigación en Demografia y Salud (CIDS, Center for Epidemiology and Health) of the University of Nicaragua, León, as a member of the INDEPTH Network, the UNC Center for Gastrointestinal Biology and Disease (P30 DK034987), and the UNC Center for Functional GI & Motility Disorders (R24 DK067674). Dr. Becker-Dreps was supported by a National Research Service Award from the Health Resources and Services Administration (5-T32 HP14001-19).
Contributor Information
Sylvia Becker-Dreps, Department of Family Medicine, University of North Carolina at Chapel Hill, 590 Manning Drive, CB #7595, Chapel Hill, NC 27599-7595, tel (919) 966-3711, fax (919) 966-6125, sbd@unc.edu.
Douglas Morgan, Division of Gastroenterology, Department of Medicine, University of North Carolina at Chapel Hill, 4143 Bioinformatics Building, CB#7080, Chapel Hill, NC 27599-7080, pager (919) 216-4783, douglas_morgan@med.unc.edu.
Rodolfo Peña, Dean, School of Medicine, University of Nicaragua-León, León, Nicaragua, tel 505-5-311-4675, rodolfo.pena@epiph.umu.se.
Loreto Cortes, Center for Epidemiology and Health, University of Nicaragua-León,, Centro de Investigación en Demografía y Salud, Universidad Nacional Autónoma de Nicaragua-León, Esquina de los Bancos, 2 ½ Cuadras al Oeste, León, Nicaragua, América Central, Phone and fax: +505-5-311-0368, locortes2003@yahoo.es.
Christopher F. Martin, Division of Gastroenterology, Department of Medicine, University of North Carolina at Chapel Hill, 4143 Bioinformatics Building, CB#7080, Chapel Hill, NC 27599-7080, tel (919) 966-9340, cmartin@med.unc.edu.
Eliette Valladares, Center for Epidemiology and Health, and Department of Obstetrics and Gynecology, University of Nicaragua-León, Centro de Investigación en Demografía y Salud, Universidad Nacional Autónoma de Nicaragua-León, Esquina de los Bancos, 2 ½ Cuadras al Oeste, León, Nicaragua, América Central, Phone and fax: +505-5-311-0368, eliette.valladares@epiph.umu.se.
REFERENCES
- Austin MP, Leader L. Maternal stress and obstetric and infant outcomes: Epidemiological findings and neuroendocrine mechanisms. Australian & New Zealand Journal of Obstetrics & Gynaecology. 2000;40(3):331–337. doi: 10.1111/j.1479-828x.2000.tb03344.x. [DOI] [PubMed] [Google Scholar]
- Bangdiwala SI, Ramiro L, Sadowski LS, Bordin IA, Hunter W, Shankar V. Intimate partner violence and the role of socioeconomic indicators in WorldSAFE communities in Chile, Egypt, India and the Philippines. Injury Control and Safety Promotion. 2004;11(2):101–109. doi: 10.1080/15660970412331292324. [DOI] [PubMed] [Google Scholar]
- Barling J, O’Leary D, Jouriles EN, Vivian D, MacEwen KE. Factor similarity of the Conflict Tactics Scales across samples, spouses, and sites: issues and implications. Journal of Family Violence. 1987;2:37–54. [Google Scholar]
- Bernal G, Cumba-Avilés E, Sáez-Santiago E. Cultural and relational processes in depressed Latino adolescents. In: Beach SRH, Wamboldt MZ, Kaslow NJ, Heyman RE, First MB, editors. Relational processes and DSM-V: Neuroscience, assessment, prevention, and treatment. Washington, DC: American Psychiatric Association; 2006. pp. 211–224. [Google Scholar]
- Bernal G, Domenech Rodríguez MM. Advances in Latino family research: cultural adaptations of evidence-based interventions. Family Process. 2009;48(2):169–178. doi: 10.1111/j.1545-5300.2009.01275.x. [DOI] [PubMed] [Google Scholar]
- Caplan A, Walker L, Rasquin A. Validation of the pediatric Rome II criteria for functional gastrointestinal disorders using the questionnaire on pediatric gastrointestinal symptoms. Journal of Pediatric Gastroenterology and Nutrition. 2005;41(3):305–316. doi: 10.1097/01.mpg.0000172749.71726.13. [DOI] [PubMed] [Google Scholar]
- Coker AL, Smith PH, Bethea L, King MR, McKeown RE. Physical health consequences of physical and psychological intimate partner violence. Archives of Family Medicine. 2000;9:451–457. doi: 10.1001/archfami.9.5.451. [DOI] [PubMed] [Google Scholar]
- Dinan TG, Quigley EM, Ahmed SM, Scully P, O’Brien S, O’Mahony L, O’Mahony S, Shanahan F, Keeling PW. Hypothalamic-pituitary-gut axis dysregulation in irritable bowel syndrome: plasma cytokines as a potential biomarker? Gastroenterology. 2006;130(2):304–311. doi: 10.1053/j.gastro.2005.11.033. [DOI] [PubMed] [Google Scholar]
- Drossman DA. The functional gastroenterology disorders and the Rome III process. Gastroenterology. 2006;130(5):1377–1390. doi: 10.1053/j.gastro.2006.03.008. [DOI] [PubMed] [Google Scholar]
- Drossman DA. The functional gastrointestinal disorders and the Rome II process. Gut. 1999;45 Suppl. 2:i1–ii5. doi: 10.1136/gut.45.2008.ii1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drossman DA, Corazziari E, Talley NJ, Thompson G, Whitehead W, editors. Rome II, The Functional Gastrointestinal Disorders. McLean, VA: Degnon Associates, Inc; 2000. [Google Scholar]
- Drossman DA, Leserman J, Nachman G, Li Z, Gluck H, Toomey TC. Sexual and physical abuse in women with functional or organic gastrointestinal disorders. Annals of Internal Medicine. 1990;113:828–833. doi: 10.7326/0003-4819-113-11-828. [DOI] [PubMed] [Google Scholar]
- Dube SR, Felitti VJ, Dong M, Giles WH, Anda RF. The impact of adverse childhood experiences on health problems: evidence from four birth cohorts dating back to 1900. Preventive Medicine. 2003;37(3):268–277. doi: 10.1016/s0091-7435(03)00123-3. [DOI] [PubMed] [Google Scholar]
- Ellsberg M, Heise L, Peña R, Agurto S, Winkvist A. Researching domestic violence against women: methodological and ethical considereations. Studies in Family Planning. 2001;1:1–16. doi: 10.1111/j.1728-4465.2001.00001.x. [DOI] [PubMed] [Google Scholar]
- Ellsberg M, Caldera T, Herrera A, Winkvist A, Kullgren G. Domestic violence and emotional distress among Nicaraguan women: results from a population-based study. American psychologist. 1999a;54(1):30–36. [Google Scholar]
- Ellsberg MC, Peña R, Herrera A, Liljestrand J, Winkvist A. Wife abuse among women of childbearing age in Nicaragua. American Journal of Public Health. 1999b;89(2):241–244. doi: 10.2105/ajph.89.2.241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Field CA, Caetano R. Ethnic differences in intimate partner violence in the U.S. general population: the role of alcohol use and socioeconomic status. Trauma, Violence, & Abuse. 2004;5(4):303–317. doi: 10.1177/1524838004269488. [DOI] [PubMed] [Google Scholar]
- Fukudo S. Role of corticotropin-releasing hormone in irritable bowel syndrome and intestinal inflammation. Journal of Gastroenterology. 2007;42 Suppl. 17:48–51. doi: 10.1007/s00535-006-1942-7. [DOI] [PubMed] [Google Scholar]
- Heitkemper M, Jarrett M, Levy RL, Cain KC, Burr RL, Feld A, Barney P, Weisman P. Increased urine catecholamines and cortisol in women with irritable bowel syndrome. American Journal of Gastroenterology. 1996;91(5):906–913. [PubMed] [Google Scholar]
- Indepth demographic network. Indepth demographic network surveillance site in Central America. 2009 Retrieved November 16, 2009, from http://www.indepth-network.org/index.php?option=com_content&task=view&id=861&Itemid=
- Inslicht SS, Marmar CR, Neylan TC, Metzler TJ, Hart SL, Otte C, McCaslin SE, Larkin GL, Hyman KB, Baum A. Increased cortisol in women with intimate partner violence-related posttraumatic stress disorder. Psychoneuroendocrinology. 2006;31(7):825–838. doi: 10.1016/j.psyneuen.2006.03.007. [DOI] [PubMed] [Google Scholar]
- Kang JY. Systematic review: the influence of geography and ethnicity in irritable bowel syndrome. Alimentary Pharmacology & Therapeutics. 2005;21(6):663–676. doi: 10.1111/j.1365-2036.2005.02396.x. [DOI] [PubMed] [Google Scholar]
- Kanazawa M, Palsson OS, Thiwan SI, Turner MJ, van Tilburg MA, Gangarosa LM, Chitkara DK, Fukudo S, Drossman DA, Whitehead WE. Contributions of Pain Sensitivity and Colonic Motility to IBS Symptom Severity and Predominant Bowel Habits. American Journal of Gastroenterology. 2008;103(10):2550–2561. doi: 10.1111/j.1572-0241.2008.02066.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kwan AC, Bao TN, Chakkaphak S, Chang FY, Ke MY, Law NM, Leelakusolvong S, Luo JY, Manan C, Park HJ, Piyaniran W, Qureshi A, Long T, Xu GM, Xu L, Yuen H. Validation of Rome II criteria for functional gastrointestinal disorders by factor analysis of symptoms in Asian patient sample. Journal of Gastroenterology and Hepatology. 2003;18(7):796–802. doi: 10.1046/j.1440-1746.2003.03081.x. [DOI] [PubMed] [Google Scholar]
- Leserman J, Drossman DA. Relationship of abuse history to functional gastrointestinal disorders and symptoms: some possible mediating mechanisms. Trauma, Violence, & Abuse. 2007;8(3):331–343. doi: 10.1177/1524838007303240. [DOI] [PubMed] [Google Scholar]
- Leserman J, Li D, Drossman DA, Hu YJB. Selected symptoms associated with sexual and physical abuse among female patients with gastrointestinal disorders: the impact on subsequent health care visits. Psychological Medicine. 1998;28(2):417–425. doi: 10.1017/s0033291797006508. [DOI] [PubMed] [Google Scholar]
- Letourneau EJ, Holmes M, Chasedunn-Roark J. Gynecologic health consequences to victims of interpersonal violence. Women’s Health Issues. 1999;9(2):115–120. doi: 10.1016/s1049-3867(98)00031-0. [DOI] [PubMed] [Google Scholar]
- Luscombe FA. Health-related quality of life and associated psychosocial factors in irritable bowel syndrome: a review. Quality of Life Research. 2000;9(2):161–176. doi: 10.1023/a:1008970312068. [DOI] [PubMed] [Google Scholar]
- Maxion-Bergemann S, Thielecke F, Abel F, Bergemann R. Costs of irritable bowel syndrome in the UK and US. Pharmacoeconomics. 2006;24(1):21–37. doi: 10.2165/00019053-200624010-00002. [DOI] [PubMed] [Google Scholar]
- McFarlane JM, Groff JY, O’Brien JA, Watson K. Prevalence of partner violence against 7,443 African American, White, and Hispanic women receiving care at urban public primary care clinics. Public Health Nursing. 2005;22(2):98–107. doi: 10.1111/j.0737-1209.2005.220203.x. [DOI] [PubMed] [Google Scholar]; Padilla A. Hispanic psychology: Critical issues in theory and research. Thousand Oaks, CA: Sage; 1995. [Google Scholar]
- Peña R, Pérez W, Meléndez M, Källestål C, Persson LA. The Nicaraguan Health and Demographic Surveillance Site, HDSS-Leon: a platform for public health research. Scandinavian Journal of Public Health. 2008;36(3):318–325. doi: 10.1177/1403494807085357. [DOI] [PubMed] [Google Scholar]
- Peña R, Wall S, Persson LA. The effect of poverty, social inequity, and maternal education on infant mortality in Nicaragua, 1988–1993. American Journal of Public Health. 2000;90(1):64–69. doi: 10.2105/ajph.90.1.64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pew Hispanic Center. Statistical Portrait of Hispanics in the United States, 2007, Detailed Hispanic Origin: 2007. 2007 Retrieved November 16, 2009, from http://pewhispanic.org/files/factsheets/hispanics2007/Table-5.pdf.
- Pico-Alfonso MA, Garcia-Linares MI, Celda-Navarro N, Blasco-Ros C, Echeburúa E, Martinez MJ. The impact of physical, psychological, and sexual intimate male partner violence on women's mental health: depressive symptoms, posttraumatic stress disorder, state anxiety, and suicide. Women’s Health (Larchmt) 2006;15(5):599–611. doi: 10.1089/jwh.2006.15.599. [DOI] [PubMed] [Google Scholar]
- Renzi MR, Agurto S. Economic and social situation of Leon, Managua, and Granada. Managua, Nicaragua. International Foundation for Global Economic Development (FIDEG); 1993. [Google Scholar]
- Shaheen NJ, Hansen RA, Morgan DR, Gangarosa LM, Ringel Y, Thiny MT, Russo MW, Sandler RS. The burden of gastrointestinal and liver diseases, 2006. American Journal of Gastroenterology. 2006;101(9):2128–2138. doi: 10.1111/j.1572-0241.2006.00723.x. [DOI] [PubMed] [Google Scholar]
- Silverman JG, Decker MR, Saggurti N, Balaiah D, Raj A. Intimate partner violence and HIV infection among married Indian women. Journal of the American Medical Association. 2008;300(6):703–710. doi: 10.1001/jama.300.6.703. [DOI] [PubMed] [Google Scholar]
- Smith MD. Enhancing the quality of survey data on violence against women: a feminist approach. Gender & Society. 1994;8(1):109–127. [Google Scholar]
- Straus MA. Measuring intrafamily conflict and violence. The Conflict Tactics (CT) Scales. Journal of Marriage and Family. 1979;41:75–88. [Google Scholar]
- Talley NJ, Boyce PM, Jones M. Is the association between irritable bowel syndrome and abuse explained by neuroticism? A population based study. Gut. 1998;42(1):47–53. doi: 10.1136/gut.42.1.47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Talley NJ, Fett SF, Zinmeister AR. Self-reported abuse and gastrointestinal disease in outpatients: association with irritable bowel-type symptoms. American Journal of Gastroenterology. 1995;90(3):366–371. [PubMed] [Google Scholar]
- Talley NJ, Helgeson SL, Zinsmeister AR, Melton LJ., III Gastrointestinal tract symptoms and self reported abuse: a population-based study. Gastroenterology. 1994;107:1040–1049. doi: 10.1016/0016-5085(94)90228-3. [DOI] [PubMed] [Google Scholar]
- ten Berg MJ, Goettsch WG, van den Boom G, Smout AJ, Herings RM. Quality of life of patients with irritable bowel syndrome is low compared to others with chronic diseases. European Journal of Gastroenterology and Hepatology. 2006;18(5):475–481. doi: 10.1097/00042737-200605000-00004. [DOI] [PubMed] [Google Scholar]
- Thompson WG, Longstreth GF, Drossman DA, Heaton KW, Irvine EJ, Mueller-Lissner SA. Functional Bowel Disorders and Functional Abdominal Pain. In: Drossman DA, Talley NJ, Thompson WG, Whitehead WE, Corazziari E, editors. Rome II: Functional Gastrointestinal Disorders: Diagnosis, Pathophysiology, and Treatment. McLean, VA: Degnon Associates, Inc; 2000. [Google Scholar]
- Valladares E, Ellsberg M, Peña R, Högberg U, Persson LA. Physical partner abuse during pregnancy: a risk factor for low birth weight in Nicaragua. Obstetrics and Gynecology. 2002;100(4):700–705. doi: 10.1016/s0029-7844(02)02093-8. [DOI] [PubMed] [Google Scholar]
- Valladares E, Peña R, Persson LA, Högberg U. Violence against women: prevalence and characteristics: A population-based study in Nicaragua. British Journal of Obstetrics and Gynaecology. 2005;112:1243–1248. doi: 10.1111/j.1471-0528.2005.00621.x. [DOI] [PubMed] [Google Scholar]
- Walker EA, Gelfand AN, Gelfand MD, Katon WJ. Psychiatric diagnoses, sexual and physical victimization, and disability in patients with irritable bowel syndrome or inflammatory bowel disease. Psychological Medicine. 1995;25(6):1259–1267. doi: 10.1017/s0033291700033225. [DOI] [PubMed] [Google Scholar]
- Zelaya E, Peña R, Garcia J, Berglund S, Persson LA, Liljestrand J. Contraceptive patterns among women and men in Leon, Nicaragua. Contraception. 1996;54(9):359–365. doi: 10.1016/s0010-7824(96)00203-x. [DOI] [PubMed] [Google Scholar]