Abstract
Traditionally, routine investigations prior to surgery are considered an important element of preanesthetic evaluation to determine the fitness for anesthesia and surgery. During past few decades this practice has been a subject of close scrutiny due to low yield and high aggregate cost. Performing routine screening tests in patients who are otherwise healthy is invariably of little value in detecting diseases and in changing the anesthetic management or outcome. Thorough history and investigation of positive answers by the clinicians, combined with physical examination of patient represents the best method for screening diseases followed by few selective tests as guided by patient's health condition, invasiveness of planned surgery and potential for blood loss. A large number of investigations which are costly to pursue often detect minor abnormalities of no clinical relevance, may be risky to patients, cause unnecessary delay or cancellation of surgery, and increase medico-legal liability. An approach of selective testing reduces cost without sacrificing safety or quality of surgical care.
Keywords: Routine laboratory investigations, routine preoperative tests, screening tests
Overview
The use of routine laboratory investigations before elective surgery is widespread. It is considered a part of pre-anesthetic evaluation to determine fitness for anesthesia and identify patients at high risk of postoperative complications. So pervasive is the thinking that surgeons, anesthetists, and even patients expect “battery of laboratory tests” prior to surgery.
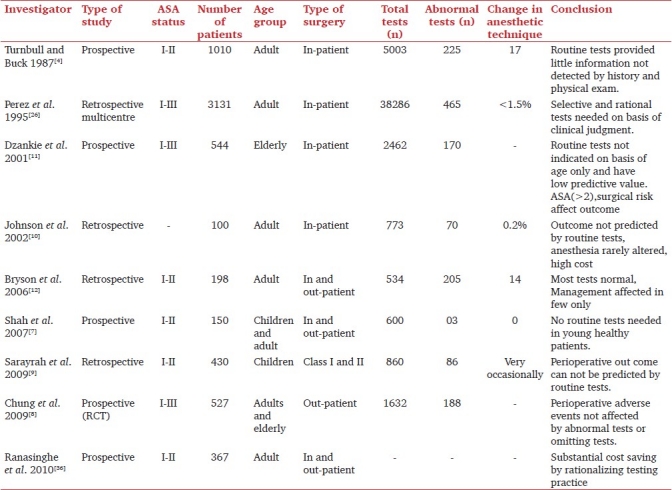
The preoperative investigations may be divided into two categories: routine or screening and indicated or diagnostic. American Society of Anesthesiologists (ASA) Task Force on Preanesthesia Evaluation (2002)[1] defined routine tests as those done in the absence of any specific clinical indication or purpose (i. e. tests intended to discover a disease or disorder in an asymptomatic patient and traditionally include a panel of blood, urine tests and X-ray chest, electrocardiogram). Indicated tests are defined as tests done for a specific clinical indication or purpose, e. g. to confirm a clinical diagnosis, to assess the severity and progress of disease, and effectiveness of therapy. The latter tests are generally well accepted as they affect perioperative care and outcome[2] However, the usefulness and cost-effectiveness of routine screening tests in the absence of any clinical indication has been questioned as the probability of finding a significant abnormality is small for laboratory tests, electrocardiogram, and chest radiography.[3–9] Our preoperative testing practice, for the most part, falls under the category of routine or category.[2] Many retrospective and prospective trials have demonstrated that the screening tests rarely uncover a disease in asymptomatic patients and abnormalities of laboratory test results very occasionally altered the perianesthetic management or outcome[4,10–12] [Table 1]. However, the cost of surgical care escalates though no safety net for medico-legal problems is offered.[3,5,10,11,13–15] This led the ASA Task Force[1] evaluation to recommend selective testing, based on clinical evaluation and risk assessment rather than the previous shotgun approach. Such an approach reduces consultations, delays, and cancellations on the day of surgery.[13] The impact of preoperative testing on health care is likely to extend beyond the simple reduction in number of tests performed.[16]
Table 1.
Data of few studies of pre-operative routine investigations
This review attempts to explore various issues of routine preoperative laboratory testing such as the background for evolution of testing, its shortcomings and value, changing trends, current guidelines and problems in dissemination, and adoption of guidelines.
Historical perspective for evolution of routine laboratory testing and challenges to practice
During 1940-1960, clinicians elicited thorough history and physical examination for preoperative assessment and only selective laboratory tests were ordered to confirm or refute clinical diagnosis.[17,18] In late 1960s, the introduction of a biochemical auto-analyzer made it easier for clinicians to obtain a large number of tests with a small addition of cost. The ease of ordering and low cost of obtaining many laboratory tests made this new method of evaluation attractive.[14] This practice evolved from the assumption that early and frequent testing could detect disease in their pre-clinical stage to allow early and less costly treatment.[17,19] This thinking was accepted as dogma and rapidly made its way into medical mindset of all health care workers such that excessive testing was equated with efficient care.[19] Many hospitals made rather arbitrary rules to perform a series of laboratory tests prior to any operative procedure[14,20] with the assumption that voluminous information would enhance the safety of surgical patients and reduce the liability for adverse events.[19] The practice continued for years without any scientific basis of the usefulness and with little consideration of cost.[5,13,17,18,20,21]
During the past three decades, this practice of routine investigations prior to surgery has been challenged by several academic publications[2,3,10,16,18,22] as it involves a sizable cost without significant benefit to millions of patients undergoing surgery. The early studies to debunk the routine preoperative screening tests were published in mid and late 1980s. In a retrospective review of charts of over 2000 elective surgical patients who underwent battery of tests including complete blood cell count, differential blood count, prothrombin time, glucose level, serum electrolytes, creatinine, platelet count, etc, Kaplan et al. (1985) demonstrated that only 96 (22%) tests revealed abnormalities. Of 96 abnormal test results, only 10 could not be determined by history and examination, of which only 4 were of actual clinical significance. Similar findings were reported in healthy adults[4,23] and in children.[9,24]
Numerous subsequent studies involving ambulatory[5,25] or inpatient surgery[10,26,27] demonstrated that the frequency of abnormal laboratory test results in asymptomatic patients was very low and 60-75% of patients would not have required any test if guided by clinical evaluation.[3,6,26,28] Even in very elderly patients, at higher risk of perioperative morbidity and mortality, ultimate benefit of routine tests prior to non-cardiac surgery seemed doubtful.[11]
Schein et al. (2002)[21] in a multicenter trial involving more than 10,000 patients of cataract surgery reported that incidence of postoperative adverse events and death was same whether preoperative routine tests were done or omitted. Similarly, studies of other ambulatory surgical patients where no preoperative investigations were done showed no adverse effects on postoperative outcome as a result of omission of tests.[8,29]
A Health Technology Assessment systematic review[30] concluded that routine screening laboratory tests produce wide range of abnormalities even in healthy patients. The clinical significance of abnormalities was uncertain and usefulness was doubtful as they rarely influenced management. There was no evidence that routine tests either improved or worsen postoperative outcome.[3]
Evidence is similarly lacking for an association for testing without indication and improvement in outcome. Routine electrocardiogram (ECG) and chest X-ray (CXR) have also shown low utility in healthy patients. The abnormal findings of CXR in asymptomatic patients ranged between 10% and 50%[30,31,32] but those which could alter anesthetic management were rare.[21,26,33] Similarly the incidence of abnormal ECG findings was very high[20,26,34] but the anesthetic management was affected in less than 5% of patients[21,26,34] The ASA Task Force[1] suggested preoperative ECG only for patients with known or suspected cardiovascular risk factors and not on the basis of age alone. Regarding chest X-ray, the Task Force did not recommend extremes of age, smoking, stable COPD, or cardiac disease as unequivocal indications of chest radiography. Tests of clotting functions in normal patients with no risk factors were incapable of predicting perioperative bleeding.[21,35]
The studies evaluating utility and cost-effectiveness of preoperative tests documented low yield and escalation of cost.[6,8,36,37] The results of cited studies and innumerable other published large trials[6,23,27] have clearly shown that performing battery of tests on a routine basis without indication produce very low abnormal findings and contributed significantly to overall health cost.[5,10]
Shortcomings of routine laboratory testing
Although the laboratory tests can help in ensuring optimal preoperative condition, routine screening tests have several shortcomings. The tests ordered in the absence of clinical indication, while frequently abnormal, fail to predict perioperative complication and seldom influence anesthetic management.[3,6,10,30,38] Nonselective testing produces many false positive, false negative, or borderline results.[14,35,39] Further evaluation or repeat test may cause unnecessary psychological and economical burden[15,20,40] and postponement of surgery.[14,18,35,41] False negative tests lead to sense of security and may result in unfavorable outcome[40] Frequently, the abnormalities detected are not pursued and the clinicians proceed with anesthesia and surgery ignoring them.[12,14] Abnormalities detected if not pursued leaves the clinicians open to more medico-legal liability than if the test was not ordered in the first place.[3,42,43]
Changing practice of preoperative testing
There are still substantial areas of uncertainty in the literature due to the lack of randomized prospective trials and relatively low incidence of post-operative adverse events.[16] But the medical,[3,4,6,21] surgical,[6,18,35,44] and anesthesia[10,11,12,26,38,45] literature is replete with reports from studies that have established that screening tests without specific indication is wasteful. Based on the available data there is general consensus that only the selective tests should be advised consistent with the clinical evaluation[17,22,45] considering patients health status, presence of medical diseases, current medication, invasiveness or risk of proposed operative procedure (minimally, moderately or highly invasive),[14] and potential for blood loss.[1,14,15,18,20,41,43] The tests should be obtained for specific clinical indication (e. g. obtain blood glucose in a known or suspected patient of diabetes or require complete blood count in surgeries where moderate or severe blood loss is expected) that may increase perioperative risk or influence management of anesthesia or surgery[10,14,15,41,43,46] and not simply because the patient is to undergo surgery. Healthy patients of ASA physical status I and II without co-existing medical condition undergoing minimally invasive outpatient surgery may require no routine investigations,[8,14,15,25,27,44] whereas those scheduled for moderately or severely invasive surgery which cause major physiological stress, few baseline tests may be done.[46] Further testing is needed only as per specific medical condition. In older patients with medical diseases, likelihood of abnormal tests is higher; therefore more liberal testing may be done. However using age as a criteria for routine tests is debated[11,34,46] and ASA physical status and risk of surgery are considered better predictors of surgical outcome in elderly patients.[11,34] There is growing evidence that physiological age with overall health condition and invasiveness of surgery rather than chronological age should determine the need of tests especially ECG.[34,47]
Value of routine tests
To determine the usefulness and interpretation of the laboratory test results, following issues need consideration.
Relevance—although some test abnormalities are clearly of concern (e. g. raised blood sugar), others may have little or no effect on perioperative anesthetic management or outcome e. g. WBC count.[19]
Normal value---usually the normal or reference range of a laboratory investigation is set arbitrarily based on 95% confidence interval. Therefore, the bete noire of the definition is that up to 5% of normal individuals may have abnormal values and vice versa.[39,41] It has been estimated that by ordering 10 independent tests in a healthy person, there are 40% chances that one of the test result will be abnormal by random chance alone.[35,39,41] Therefore, to determine its clinical relevance, the test results should be interpreted within context of clinical situation.[46]
Sensitivity, specificity of tests and prevalence of disease—the usefulness of screening a disease depends on the sensitivity and specificity of the test and the prevalence of the disease in the population. Screening tests in the asymptomatic population should only be done in patients where the potential condition is significant and of reasonable prevalence.[19,41]
Consideration of cost—a sizable amount of money can be saved by selective testing and use of a less costly test if quality of information is not compromised.[20,38]
Risk and cost versus benefit—the risks of an intervention based on results is associated with significant cost both in terms of money and potential harm[31] and also the risk may outweigh the benefit.[10,14,41] For example following a positive non-invasive test, coronary angiography and bypass surgery may be advised before a non-cardiac surgery. Although outcome may improve, morbidity associated with the procedures may be greater than any benefit.[41]
Current recommendations/guidelines
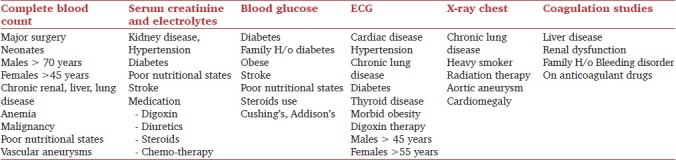
Substantial variations are found in the practice of preoperative testing and it varies markedly from one hospital to other and among clinicians of the same hospital.[47,48] In an attempt to rationalize this issue, guidelines have been systematically developed after analysis of studies, best evidence available, and consensus of expert professionals.[14,15,18,19,20,30,49] Preoperative diagnosis-based guidelines provide basic recommendations for laboratory and other tests [Table 2, based on the guidelines available in text books of anesthesia and scientific journals].[14,15,18,19,48,49] The recommendations can be accepted as such or can be modified based on local need and individual practice, to ensure highest quality of surgical care. Bryson et al. (2006)[12] noted that abnormal laboratory results were equally common in patients having ambulatory or inpatient surgery suggesting that the guidelines were over inclusive and could be further refined. Similarly, in women requiring gynecologic surgery, adherence to guidelines[49] resulted in a large number of inappropriate tests.[32] Therefore, guidelines should be periodically reviewed and re-evaluation should not be restricted to outpatients only.[12] They should be audited as warranted by evolution of medical knowledge, technology, and pattern of practice.[12,32,47]
Table 2.
Preoperative diagnosis based investigations before elective surgery
Problems in adoption of guidelines
Over the past one decade some change has occurred and the number of routine tests have decreased[23,24,29] along with cost of care both at individual[50,51] and institutional level[8,36,37] while safety of patients was not affected.[8,13,19,37,38,50] Still 30-60% tests continue to be greatly in excess of that recommended.[12,47] It is a matter of great concern that despite clear results of innumerable studies and recommendations from professional societies, after nearly 30 years, the dissemination and adoption of guidelines to routine practice is problematical.[2,16,18] The reasons why clinicians continue to order the routine tests before surgery are not clear[26] but a number of reasons have been suggested.[51] Difficulty in changing previous work pattern or behavior,[2,13,18] fear of cancellation of surgery,[51] missing some important information during evaluation,[14] and institutional requirement[18] are few. Fear of litigation is a real concern among clinicians who worry that not carrying out the tests will have to be answered in the case of an adverse event during anesthesia.[6,18,52,53] An important reason of over testing in teaching institutes is belief among junior staff that the consultants wanted them or simply by force of habit that is passed down through successive generations of junior staff.[10,50] In many hospitals and institutions the laboratory tests are ordered by the surgeons and the anesthetist are reluctant to cancel the tests ordered by surgical colleagues.[12] Any scheme that proposes to rationalize routine testing must address these issues that will otherwise act as barriers.[18]
The professionals involved in surgical care of patients include primary care physicians, internists, anaesthetists, and surgeons who should jointly try to curb on this practice. The efforts to change the old practice should include making the clinicians aware of limited value and unnecessary cost of the screening tests by providing credible data. They should also be assured that reducing or omitting the routine tests would not affect quality of care or safety of patients and would not increase the medico-legal liability. There is a strong need of continuing education of junior medical staff and consensus among consultants about change in practice both at national and local level.[37,42] At the same time, it is also necessary to advocate for establishment of a more structured approach to manage surgical patients during the initial phase of the perioperative process to permit implementation of guidelines whose use can significantly reduce unnecessary tests.[16] This calls for establishment of preoperative assessment clinics to provide cost-effective quality patient care,[1] where the anesthesiologists who understand the risk factors of both the patients as well as surgery, can clinically evaluate and order appropriate and necessary investigations for a particular patient.[20]
Key Points
Performing routine tests in all surgical patients as a screening tool is inefficient, unnecessary, and expensive.
The value of preoperative screening lies in the clinician's assessment; the selective tests are then ordered considering specific information obtained from patient's interview, examination, review of medical records and the type, and invasiveness of proposed surgery and anesthesia.
The tests should be done only if results are likely to affect patient management and postoperative outcome.
They should not be guided by tradition, vested interest, or cost alone.
It is a misconception that obtaining battery of routine tests provides medico-legal protection against liability.
Adoption of guidelines for testing can maximize the yield and prevent waste of resource and time.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Practice advisory for pre-anaesthesia evaluation: A report by American Society of Anesthesiologists Task Fore on Preanaesthesia evaluation. Anesthesiology. 2002;96:485–96. doi: 10.1097/00000542-200202000-00037. [DOI] [PubMed] [Google Scholar]
- 2.Bryson GL. Has preoperative testing become a habit? Can J Anesth. 2005;52:557–61. doi: 10.1007/BF03015762. [DOI] [PubMed] [Google Scholar]
- 3.Kaplan EB, Sheiner LB, Boeckmann AJ, Roizen MF, Beal SL, Cohen SN, et al. The usefulness of pre-operative laboratory screening. JAMA. 1985;253:3576–81. [PubMed] [Google Scholar]
- 4.Turnbull KM, Buck C. The value of pre-operative screening investigations in otherwise healthy individuals. Arch Intern Med. 1985;147:1101. [PubMed] [Google Scholar]
- 5.Allison JG, Bromley HR. Unnecessary preoperative investigations evaluation and cost analysis. Am Surg. 1996;62:686–9. [PubMed] [Google Scholar]
- 6.Smetana GW, Macpherson DS. The case against preoperative laboratory testing. Med Clin North Am. 2003;87:7–40. doi: 10.1016/s0025-7125(02)00147-5. [DOI] [PubMed] [Google Scholar]
- 7.Shah SA, Sajid T, Asif M, Khan F, Ghani R. Significance and cost effectiveness of preoperative routine laboratory investigation in young healthy patients undergoing elective ear, nose and throat surgery. J Ayub Med Coll Abbotabad. 2007;19:3–6. [PubMed] [Google Scholar]
- 8.Chung F, Yuan H, Yin L, Vairavanathan S, Wong DT. Elimination of testing in ambulatory surgery. Anesth Analg. 2009;108:467–75. doi: 10.1213/ane.0b013e318176bc19. [DOI] [PubMed] [Google Scholar]
- 9.Sarayrah MA, Habaiben E. Preoperative blood testing in pediatric age group: Is it necessary? Mid East J Fam Med. 2009:7–9. [Google Scholar]
- 10.Johnson RK, Montimer AJ. Routine Preoperative blood testing: Is it necessary? Anaesthesia. 2002;57:914–7. doi: 10.1046/j.1365-2044.2002.02750.x. [DOI] [PubMed] [Google Scholar]
- 11.Dzankic S, Pastor D, Gonzalez C, Leung JM. The prevalence predictive value of abnormal preoperative tests in elderly surgical patients. Anesth Analg. 2001;93:301–8. doi: 10.1097/00000539-200108000-00013. [DOI] [PubMed] [Google Scholar]
- 12.Bryson GL, Wyand S, Bragg PR. Preoperative testing is inconsistent with published guidelines and rarely changes management. Can J Anesthe. 2006;53:236–41. doi: 10.1007/BF03022208. [DOI] [PubMed] [Google Scholar]
- 13.Fischer S. Cost effective preoperative evaluation and testing. Chest. 1999;115:965–1005. doi: 10.1378/chest.115.suppl_2.96s. [DOI] [PubMed] [Google Scholar]
- 14.Roizen MF, Lichtor JL. Preoperative assessment and premedication for adults. In: Healy TEJ, Knight PR, editors. 7th ed. Wylie and Churchill Davidson's A practice of Anesthesia; 2003. pp. 415–25. [Google Scholar]
- 15.Fischer SP, Bader AM, Sweitzer B. Preoperative evaluation. In: Miller RD, Eriksson LI, Fleisher LA, Wiener-Kronish JP, Young WL, editors. 7th ed. Millers Anesthesia Churchill Livingstone Elsevier; 2010. pp. 1001–66. [Google Scholar]
- 16.Pasternak LR. Preoperative testing: Moving from individual testing to risk management. Anesth Analg. 2009;108:393–4. doi: 10.1213/ane.0b013e31819278ea. [DOI] [PubMed] [Google Scholar]
- 17.Roizen MF. More preoperative assessment by physicians and less by laboratory tests. N Eng J Med. 2000;342:204–5. doi: 10.1056/NEJM200001203420311. [DOI] [PubMed] [Google Scholar]
- 18.MacPherson RD, Reeve SA, Stewart TV, Cunningham AE, Craven ML, Fox G, et al. Effective strategy to guide pathology test ordering in surgical patient. ANZ J Surg. 2005;75:138–43. doi: 10.1111/j.1445-2197.2005.03316.x. [DOI] [PubMed] [Google Scholar]
- 19.Pasternak LR. Pre- operative laboratory testing: General issues and considerations. Anesthesiol Clin North America. 2004;22:13–25. doi: 10.1016/S0889-8537(03)00115-9. [DOI] [PubMed] [Google Scholar]
- 20.Badar AM. Pre-operative testing. Curr Anesth Reports. 2001;1:67–9. [Google Scholar]
- 21.Schein OD, Katz J, Bass EB, Tielsch JM, Lubomski LH, Feldman MA, et al. The value of routine preoperative medical testing before cataract surgery.Study of medical testing for cataract surgery. N Engl J Med. 2000;342:168–75. doi: 10.1056/NEJM200001203420304. [DOI] [PubMed] [Google Scholar]
- 22.Klein AA, Arrowsmith JE. Should routine preoperative testing be abandoned? Anesthesia. 2010;65:974–6. doi: 10.1111/j.1365-2044.2010.06503.x. [DOI] [PubMed] [Google Scholar]
- 23.Narr BJ, Hansen TR, Warner MA. Preoperative laboratory screening in healthy Mayo patients: Cost effective elimination of tests and unchanged outcomes. Mayo clinic Proc. 1991;66:155–9. doi: 10.1016/s0025-6196(12)60487-x. [DOI] [PubMed] [Google Scholar]
- 24.O'Connor ME, Drasner K. Preoperative laboratory testing of children undergoing elective surgery. Anesth Analg. 1990;70:176–80. [PubMed] [Google Scholar]
- 25.Hesse S, Seebaner A, Sschwender D. Ambulatory anaesthesia: Which preoperative screening tests are required. Anaesthetist. 1999;48:108–15. doi: 10.1007/s001010050674. [DOI] [PubMed] [Google Scholar]
- 26.Perez A, Planell J, Bacardaz C, Hounie A, Franci J, Brotons C, et al. Value of routine preoperative tests: A multicentre study in four general hospitals. Br J Anaesth. 1994;74:250–6. doi: 10.1093/bja/74.3.250. [DOI] [PubMed] [Google Scholar]
- 27.Alsumaits BM, Alhumood SA, Ivanova T, Mores M, Edeia M. A prospective evaluation of preoperative screening laboratory tests in general surgery patients. Med Princ Pract. 2002;11:42–5. doi: 10.1159/000048660. [DOI] [PubMed] [Google Scholar]
- 28.Mantha S, Roizen MF, Madduri J, Rajender Y, Shanti Naidu K, Gayatri K. Usefulness of routine preoperative testing: A prospective single observer study. J Clin Anesth. 2005;17:51–7. doi: 10.1016/j.jclinane.2004.04.002. [DOI] [PubMed] [Google Scholar]
- 29.Narr BJ, Warner ME, Shreoder DR, Warner MA. Outcomes of patients with no laboratory assessment before anesthesia and a surgical procedure. Mayo Clin Proceedings. 1997;72:505–9. doi: 10.4065/72.6.505. [DOI] [PubMed] [Google Scholar]
- 30.Munro J, Booth A, Nichol J. Routine pre operative testing: A systematic review of the evidence. Health Technol Assess. 1997;12:1–62. [PubMed] [Google Scholar]
- 31.Silvestri L, Maffessanti M, Gregori D, Berlot G, Gullo A. Usefulness of routine preoperative chest radiography for anaesthetic management: A prospective multicentre pilot study. Eur J Anaesthesiol. 1999;16:749–60. doi: 10.1046/j.1365-2346.1999.00577.x. [DOI] [PubMed] [Google Scholar]
- 32.St Clair CM, Shah M, Diver E, Sharyn L, William B, Xuming S, et al. Adherence to evidence-based guidelines for preoperative testing in women undergoing gynaecologic surgery. Obstet Gynecol. 2010;116:694–700. doi: 10.1097/AOG.0b013e3181ec448d. [DOI] [PubMed] [Google Scholar]
- 33.Joo HS, Wong J, Naik VN, Savoldelli GL. The value of screening preoperative chest X-ray: A systematic review. Can J Anesth. 2005;52:568–74. doi: 10.1007/BF03015764. [DOI] [PubMed] [Google Scholar]
- 34.Liu LL, Dzankic S, Leung JM. Preoperative electrocardiogram abnormalities do not predict postoperative cardiac complications in geriatric surgical patients. J Am Geriatr Soc. 2002;50:1086–91. doi: 10.1046/j.1532-5415.2002.t01-1-50303.x. [DOI] [PubMed] [Google Scholar]
- 35.Macpherson DS. Pre operative laboratory testing: Should any test be routine before surgery. Med Clin North Am. 1993;77:289–308. doi: 10.1016/s0025-7125(16)30252-8. [DOI] [PubMed] [Google Scholar]
- 36.Ranasinghe P, Perera YS, Abayadeera A. Preoperative investigations in elective surgery: Practices and costs at the national hospital of Sri Lanka. Sri Lankan J Anaesthesiol. 2010;18:29–35. [Google Scholar]
- 37.Ferrando A, Ivaldi C, Buttiglieri A, Pagano E, Bonetto C, Arione R, et al. Guidelines for preoperative assessment: Impact on clinical practices and costs. Int J Qual Health Care. 2005;17:323–9. doi: 10.1093/intqhc/mzi039. [DOI] [PubMed] [Google Scholar]
- 38.Finegan B, Saifudin R, Mc Alister FA O'Connor P. Selective ordering of preoperative investigations by anesthesiologists reduces the number and cost of tests. Can J Anesth. 2005;52:575–80. doi: 10.1007/BF03015765. [DOI] [PubMed] [Google Scholar]
- 39.Velanovich V. Collective Review: Preoperative laboratory evaluation. J Am Coll Surg. 1996;183:79–87. [PubMed] [Google Scholar]
- 40.Eiicho I. Role of preoperative laboratory tests in preoperative assessment. J Japn Soc Clin Anesth. 2005;25:582–7. [Google Scholar]
- 41.Fleisher LA. Preoperative evaluation. In: Barash PG, Cullen BF, Stoelting RK, Cohalen M, Stock MC, editors. Clinical Anaesthesia. 6th ed. Lippincott Williams and Wilkins; 2009. pp. 473–89. [Google Scholar]
- 42.Olson RP, Stone A, Lubarstry D. The prevalence and significance of low preoperative hemoglobin in ASA I or II outpatient surgery candidates. Anesth Analg. 2005;101:1337–40. doi: 10.1213/01.ANE.0000180836.02142.E6. [DOI] [PubMed] [Google Scholar]
- 43.Hepner DL. The role of testing in the preoperative evaluation. Cleve Clin J Med. 2009;76:S22–S27. doi: 10.3949/ccjm.76.s4.04. [DOI] [PubMed] [Google Scholar]
- 44.Traub NL. Preoperative testing. In: Smith RB, Dobson TF, N Spell N, Walker HK, editors. Medical management of surgical patients: A text book of perioperative medicine. 4th ed. England: Cambridge University Press; 2006. pp. 32–37. [Google Scholar]
- 45.Michota FD, Frost SD. The preoperative evaluation: Use the history and physical examination rather than routine testing. Cleve Clin J Med. 2004;71:63–70. doi: 10.3949/ccjm.71.1.63. [DOI] [PubMed] [Google Scholar]
- 46.Fleisher Lee A. Preoperative preparation in Evidence-based practice of anesthesiology. Saunders Elsevier Health Science. (2nd ed) 2009:9–19. [Google Scholar]
- 47.Yuan H, Chung F, Wong D, Edward R. Current preoperative testing practices in ambulatory surgery are widely disparate: A survey of CAS members. Can J Anesth. 2005;52:675–9. doi: 10.1007/BF03016552. [DOI] [PubMed] [Google Scholar]
- 48.Carlisle J, Langham J, Thoms G. Editorial I Guidelines for preoperative testing. Brit J Anesth. 2004;93:495–497. doi: 10.1093/bja/aeh230. [DOI] [PubMed] [Google Scholar]
- 49.NCCAC. London: NICE; 2003. Preoperative Tests, The Use of Routine Preoperative Tests for Elective Surgery- Evidence, Methods and Guidance. [Google Scholar]
- 50.Mancuso CA. Impact of new guidelines on physicians ordering of preoperative tests. J Gen Int Med. 1999;14:166–172. doi: 10.1046/j.1525-1497.1999.00308.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Power LM, Thackray NM. Reduction of preoperative investigations with the introduction of an anaesthetist led preoperative assessment clinic. Anaesth Intensive care. 1999;27:481–8. doi: 10.1177/0310057X9902700508. [DOI] [PubMed] [Google Scholar]
- 52.Garcia-Miguel FJ, Serrano-Aguilar PG, Lopez-Bastida J. Preoperative assessment. Lancet. 2003;362:1749–57. doi: 10.1016/s0140-6736(03)14857-x. [DOI] [PubMed] [Google Scholar]
- 53.Barazzoni F, Grilli R, Amicosante AM, Brescianini S, Marca MA, Baggi M, et al. Impact of end use involvement in implementing guidelines on routine preoperative tests. Int J Qual Health Care. 2002;8:1–7. doi: 10.1093/intqhc/14.4.321. [DOI] [PubMed] [Google Scholar]


