Abstract
Background:
Severe sepsis leads to organ failure and results in high mortality. Organ dysfunction is an independent prognostic factor for intensive care unit (ICU) mortality. The objective of the present study was to determine the effect of acute organ dysfunction for ICU mortality in patients with severe sepsis using administrative data.
Materials and Methods:
A multicenter cross-sectional study was performed in 2008. The study was conducted in 112 teaching hospitals in Japan. All cases with severe sepsis in ICU were identified from administrative data.
Results:
Administrative data acquired for 4196 severe septic cases of 75,069 cases entered in the ICU were used to assess patient outcomes. Cardiovascular dysfunction was identified as the most major organ dysfunction (73.0%), and the followings were respiratory dysfunction (69.4%) and renal dysfunction (39.0%), respectively. The ICU mortality and 28-day means 28-day from ICU entry. were 18.8% and 27.7%, respectively. After adjustment for age, gender, and severity of illness, the hazard ratio of 2, 3, and ≥4, the organ dysfunctions for one organ failure on ICU mortality was 1.6, 2.0, and 2.7, respectively.
Conclusions:
We showed that the number of organ dysfunction was a useful indicator for ICU mortality on administrative data. The hepatic dysfunction was the highest mortality among organ dysfunctions. The hazard ratio of ICU death in severe septic patients with multiple organ dysfunctions was average 2.2 times higher than severe septic patients with single organ dysfunction.
Keywords: Intensive care units, multicenter study, multiple organ failure, mortality, sepsis
Introduction
Severe sepsis is one of the leading causes of morbidity and high mortality in intensive care units (ICUs).[1] Septic patients had more severe organ dysfunction, longer intensive care unit and hospital lengths of stay, and higher mortality rate than patients without sepsis.[2,3]
There was a significant increase in ICU mortality with increasing number of organ dysfunction,[4] and administrative data have been used to perform the study on ICU research.[5–9] The aim of the present study is to determine the effect of acute organ dysfunction for ICU mortality in patients with severe sepsis using the administrative data.
Material and Methods
Data source
Data were obtained from the Quality Indicator/Improvement Project, which collects administrative detailed claim data from acute care hospitals in Japan. In voluntary participating hospitals, 112 ICUs were included in 2009. Administrative data were comprised of clinical information and healthcare claim data. Clinical information included patient demographics, primary and secondary diagnoses, comorbidities at the time of and after admission, operative data, severity of illnesses, as well as any special treatments (i.e. radiation therapy, artificial respiration, chemotherapy). In contrast, healthcare claim data itemized the type, quantity, and fees for all tests, medications, procedures, use of intensive or specialized care, and nursing services.
Cases and selection criteria
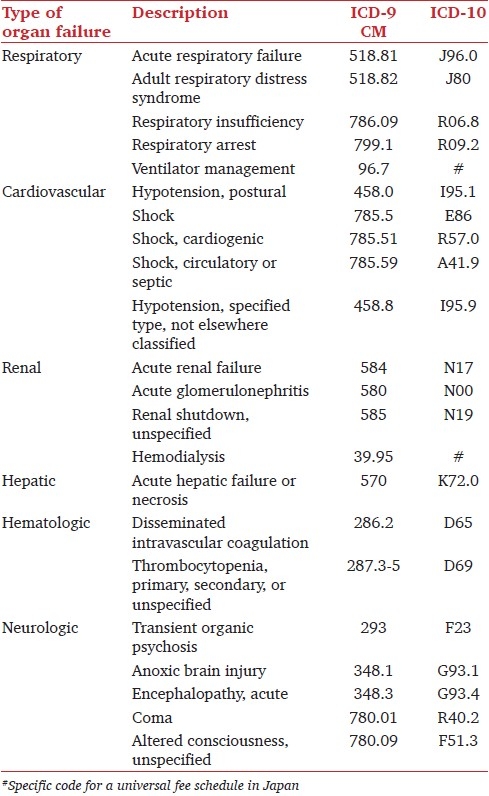
The following selection criteria were used in the study: (i) primary diagnosis of sepsis (codes in the International Classification of Diseases, 10th version) [Table 1]; (ii) complication of acute organ dysfunction classified by Martin et al.;[5] and (iii) discharge date between January 1 and December 31st, 2009. We excluded less than 18-year old cases. In addition, we did not analyze metabolic dysfunction as acute organ dysfunction, since SOFA score, which was the general and principal indicator for evaluation of acute organ dysfunction in critically ill patients, did not include this item. We defined severe sepsis as fulfillment of (i) and (ii), as well as previous studies.[5,6]
Table 1.
Translation of ICD-9 CM to ICD-10 code in the study
Evaluation of cases
The patient characteristics were express by age, gender, severity of illness, acute organ dysfunction, admission course, reason for ICU entry, and underlying disease. We evaluated severity of illness using the Critical care Outcome Prediction Equation (COPE) model derived by Duke et al., which has an area under the ROC curve of 0.83–0.84 and relatively few variables, and is the model based on administrative data alone.[10]
The intervention for severe septic patients was presented by mechanical ventilation, renal replacement therapy, use of catecholamine; dopamine, dobutamine, noradrenalin, and adrenaline including SOFA score.
Patient outcomes
The ICU mortality, 28-day mortality, hospital mortality, the length of ICU stay, and the length of hospital stay were evaluated. The ICU, 28-day, and hospital mortality rate was calculated by dividing the number of non-survivors following ICU discharge, day 28, and hospital discharge by the total number of severe septic cases, respectively.
Impact of ICU mortality on acute organ dysfunction
First, Kaplan–Meier curve was expressed for the association between the number of organ dysfunction ad ICU mortality. Log-rank statistics was performed on each factor. Second, Cox proportional hazard model was performed for unadjusted and adjusted evaluation of the effect of acute organ dysfunction on ICU mortality. We adjusted ICU mortality with age, gender, and severity of illness. In addition, impact of each organ dysfunction was assessed using hazards ratio.
Statistical analysis
All data are shown as means ± SD, or percentages. P < 0.05 was considered to be significant. All statistical analyses were performed using SPSS 11.0J (SPSS Inc., Chicago, IL). The Institutional Review Board of the Faculty of Medicine at the Graduate School of Medicine of Kyoto University, Japan, approved this study.
Results
The data used for this study was from 75,069 ICU patients discharged from 112 hospitals. Of these, 4252 (5.7%) were identified as severe septic cases, but only 56 (1.3%) matched the exclusion criteria, leaving 4196 (98.7%) that were included in our analysis.
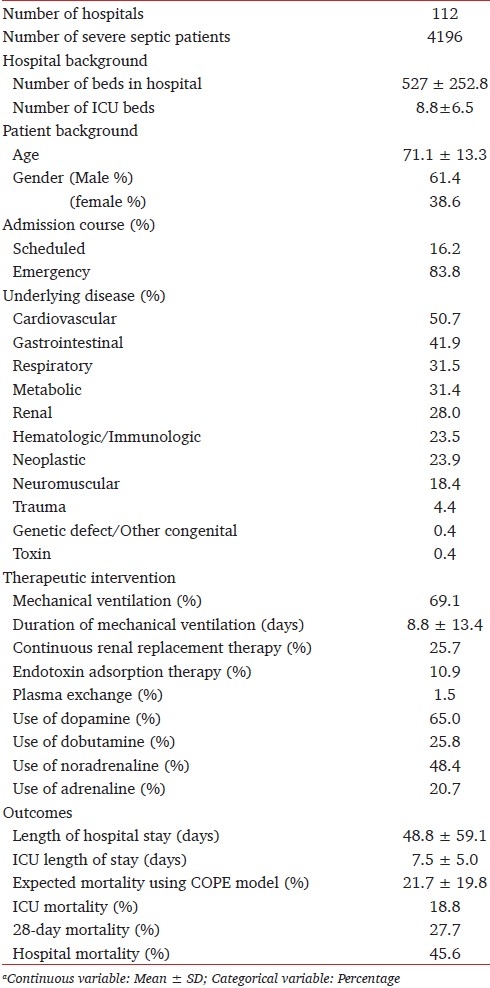
Patient background is shown in Table 2. Over half of the patients were male (n =2575, 61.4%), and had internal medical disease caused without surgery as reason for ICU entry (n = 2562, 61.1%). Therapeutic intervention for severe septic patients was most commonly performed using mechanical ventilation (n = 2900, 69.1%), followed by dopamine use (n = 2726, 65.0%). Continuous renal replacement therapy, which was the most frequently used, was performed in 1080 cases (25.7%) of the patients performing renal replacement therapy.
Table 2.
Hospital and patient backgrounds in ICU patients with severe sepsisa
Patient outcomes
The length of ICU stay was 7.5 days in severe septic patients. The ICU mortality in severe septic patients was 18.8%. However the hospital mortality was nearly 2.5 times higher than the ICU mortality, though the expected mortality using COPE model was 21.7%. The length of hospital stay was over a month in severe septic patients.
Cox proportional hazard model for ICU mortality on acute organ dysfunction
In our severe septic cases, 1582 patients (37.7%) had two organ dysfunction, and 3055 (72.8%) had multiple organ dysfunction. In patients with more than or equal to 4 organ dysfunctions, ICU mortality (38.9%) was over four times compared to single organ dysfunction (8.9%) [Table 3]. [Figure 1] showed a Kaplan-Meier curve calculating from ICU entry in each number of organ dysfunctions. After adjustment for age, gender, and severity of illness, the hazard ratio (HR) increased in increasing number of organ dysfunction (1.6, 2.0, and 2.7 in 2-, 3-, and ≥4 organ dysfunctions, respectively) [Table 3].
Table 3.
Hazard ratio of multiple organ dysfunctions on ICU mortality
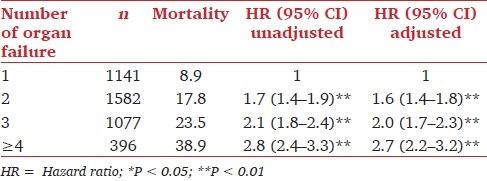
Figure 1.
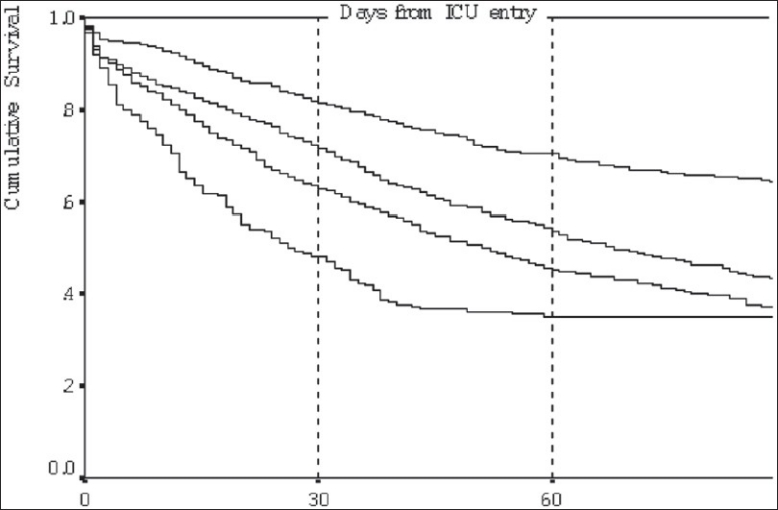
Kaplan– Meier curve of each number of organ dysfunctions: Mortality is calculated from the entry into the ICU. 1; single organ dysfunction, 2; two organ dysfunctions, 3; three organ dysfunctions, ≥4; over four organ dysfunctions
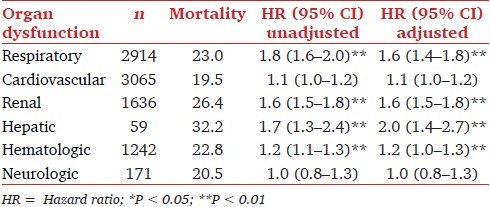
Majority of patients (n = 3065, 73.0%) had cardiovascular dysfunction, and following was respiratory dysfunction (n = 2194, 69.4%). Hepatic dysfunction was minority (n = 59, 1.4%), however, ICU mortality and hazard ratio with hepatic dysfunction was the most highest in other dysfunction (32.2% and 2.0, respectively). However, cardiovascular and neurologic dysfunctions were not significant factor for the ICU death (P = 0.178 and P = 0.703, respectively) [Table 4].
Table 4.
Hazard ratio of organ dysfunction on ICU mortality
Discussion
Our best finding was the identification of the increasing hazard ratio of the increasing number of organ dysfunction for the death of ICU using administrative data, without respect to combination of organ dysfunctions. The hazard ratio of ICU death in severe septic patients with multiple organ dysfunctions was average 2.2 times higher than severe septic patients with single organ dysfunction. Mortality of severe sepsis patients is greater than 30%[1,11] and an important theme challenging improvement of patient outcomes such as surviving sepsis campaign.[12–15] Recently, it was shown that acute organ dysfunction was useful prognostic indicator for ICU mortality, especially that there was a significant increase in ICU mortality with increasing number of organ failures.[4,16] Such result was reported in the study for dogs.[17]
Cardiovascular dysfunction was strong factor in organ dysfunctions, and a number of organ dysfunctions were available for assessment of ICU death compared to SOFA score.[4] Hepatic dysfunction was the strongest factor for ICU death in this study. However, impact of ICU mortality on cardiovascular dysfunction was not significant for ICU death. Concerning cardiovascular dysfunction, our study and the report of N for et al.[4] was controversial. It might be caused by our subject of only severe sepsis or selection bias such as the variety during recording physicians under administrative data.
In this study, severe septic patients had ICU mortality of 18.8%, and 28-day mortality of 27.7%. Hospital mortality was very high (45.6%), and there was extreme difference between our hospital mortality and the expected mortality calculating from the COPE model. However in Japan, acute care hospitals have had the role of acute care, sub-acute care, and terminal care. Although functional distinction in each hospital has been developed recently, the length of hospital stay was too long (45.6 days) compared with other advanced countries (18–30% in hospital mortality and 12–17 days in hospital stay.[5,18,19] So we considered that the hospital mortality was very high in Japan. However, ICU mortality and the duration of ICU stay in our study were similar to the values of 10–35% and 7 days found by Vincent et al.[2] So we believe that it is acceptable for us to compare ICU examination among advanced countries including Japan.
In the point of multicenter study, administrative data was a useful tool due to comparative accessible collection and uniformity of large population database. In Japan, administrative data introduced in 2004 included records of patient information and daily medical care. From these data, the types of all tests, medications and procedures and the use of intensive or special care and nursing services can be itemized on a daily basis. So we considered that administrative data was a valuable instrument for examination between acute organ dysfunction and ICU mortality in severe sepsis in a multicenter observational study. However, in fact, it was indicated that administrative data was inappropriate for the sole means of conducting surveillance for healthcare-associated infections.[20] So it was expected that administrative coding data further reflected the actual condition.
There are several limitations in the present study. First, our data did not include physiological data and severity scores. Therefore, we could not identify clinical indicators for organ dysfunction such as the ratio of arterial oxygen concentration to the fraction of inspired oxygen (P/F ratio), value of liver enzyme, blood urea nitrogen (BUN), and creatinine, and the severity scores such as SOFA, the Acute Physiology and Chronic Health Evaluation (APACHE), the Mortality Prediction Model (MPM), and the Simplified Acute Physiology Score (SAPS). For the adjustment of severity, we used the Critical care Outcome Prediction Equation (COPE) model using administrative data and simple variables. The COPE model is favored because it has an acceptable area under the ROC curve and relatively few variables, and is currently the only model based on administrative data alone.[10] When the physiological data and general scoring systems were used in the analysis, significant indicators for mortality in severe sepsis[11] were demonstrated. However, administrative data was capable on large population, comparable source among institutions, accuracy of clinical information, and relatively small effort in analysis. Second, the administrative data include information on a “calendar day” basis, rather than an hourly basis, and therefore the first ICU day was defined by a calendar day. So the representative data in patient background was including a small error. But our focus was to determine the hazard ratio of organ dysfunction for ICU death, and we considered that this error could not affect our conclusion.
Conclusions
This study examined the hazard ratio of ICU death for organ dysfunctions in patients with severe septic patients using administrative data. The hazard ratio of ICU death in severe septic patients with multiple organ dysfunctions was average 2.2 times higher than severe septic patients with single organ dysfunction. We demonstrated the ability of large administrative datasets to predict ICU mortality by focusing on acute organ dysfunction in severe septic patients.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Levy MM, Dellinger RP, Townsend SR, Linde-Zwirble WT, Marshall JC, Bion J, et al. The surviving sepsis campaign: Results of an international guideline-based performance improvement program targeting severe sepsis. Crit Care Med. 2010;38:367–74. doi: 10.1097/CCM.0b013e3181cb0cdc. [DOI] [PubMed] [Google Scholar]
- 2.Vincent JL, Sakr Y, Sprung CL, Ranieri VM, Reinhart K, Gerlach H, et al. Sepsis in European intensive care units: Results of the SOAP study. Crit Care Med. 2006;34:344–53. doi: 10.1097/01.ccm.0000194725.48928.3a. [DOI] [PubMed] [Google Scholar]
- 3.Ingraham AM, Xiong W, Hemmila MR, Shafi S, Goble S, Neal ML, et al. The attributable mortality and length of stay of trauma-related complications: A matched cohort study. Ann Surg. 2010;252:358–62. doi: 10.1097/SLA.0b013e3181e623bf. [DOI] [PubMed] [Google Scholar]
- 4.Nfor TK, Walsh TS, Prescott RJ. The impact of organ failures and their relationship with outcome in intensive care: Analysis of a prospective multicentre database of adult admissions. Anaesthesia. 2006;61:731–8. doi: 10.1111/j.1365-2044.2006.04707.x. [DOI] [PubMed] [Google Scholar]
- 5.Martin GS, Mannino DM, Eaton S, Moss M. The epidemiology of sepsis in the United States from 1979 through 2000. N Engl J Med. 2003;348:1546–54. doi: 10.1056/NEJMoa022139. [DOI] [PubMed] [Google Scholar]
- 6.Angus DC, Linde-Zwirble WT, Lidicker J, Clermont G, Carcillo J, Pinsky MR. Epidemiology of severe sepsis in the United States: Analysis of incidence, outcome, and associated costs of care. Crit Care Med. 2001;29:1303–10. doi: 10.1097/00003246-200107000-00002. [DOI] [PubMed] [Google Scholar]
- 7.Hartman ME, Linde-Zwirble WT, Angus DC, Watson RS. Trends in admissions for pediatric status asthmaticus in New Jersey over a 15-year period. Pediatrics. 2010;126:e904–11. doi: 10.1542/peds.2009-3239. [DOI] [PubMed] [Google Scholar]
- 8.Wu SC, Chen JS, Wang HM, Hung YN, Liu TW, Tang ST. Determinants of ICU care in the last month of life for Taiwanese cancer decedents, 2001 to 2006. Chest. 2010;138:1071–7. doi: 10.1378/chest.09-2662. [DOI] [PubMed] [Google Scholar]
- 9.LeMaster CH, Schuur JD, Pandya D, Pallin DJ, Silvia J, Yokoe D, et al. Infection and natural history of emergency department-placed central venous catheters. Ann Emerg Med. 2010;56:492–7. doi: 10.1016/j.annemergmed.2010.05.033. [DOI] [PubMed] [Google Scholar]
- 10.Duke GJ, Santamaria J, Shann F, Stow P, Pilcher D, Ernest D, et al. Critical care outcome prediction equation (COPE) for adult intensive care. Crit Care Resusc. 2008;10:35–41. [PubMed] [Google Scholar]
- 11.Martin CM, Priestap F, Fisher H, Fowler RA, Heyland DK, Keenan SP, et al. A prospective, observational registry of patients with severe sepsis: The Canadian Sepsis Treatment and Response Registry. Crit Care Med. 2009;37:81–8. doi: 10.1097/CCM.0b013e31819285f0. [DOI] [PubMed] [Google Scholar]
- 12.Torgersen C, Dünser MW, Schmittinger CA, Pettilä V, Ruokonen E, Wenzel V, et al. Current approach to the haemodynamic management of septic shock patients in European intensive care units: A cross-sectional, self-reported questionnaire-based survey. Eur J Anaesthesiol. 2011;28:284–90. doi: 10.1097/EJA.0b013e3283405062. [DOI] [PubMed] [Google Scholar]
- 13.Marshall JC, Dellinger RP, Levy M. The surviving sepsis campaign: A history and perspective. Surg Infect. 2010;11:275–81. doi: 10.1089/sur.2010.024. [DOI] [PubMed] [Google Scholar]
- 14.Machado FR, Mazza BF. Improving mortality in sepsis: Analysis of clinical trials. Shock. 2010;34:54–8. doi: 10.1097/SHK.0b013e3181e7e8b4. [DOI] [PubMed] [Google Scholar]
- 15.Gerber K. Surviving sepsis: A trust-wide approach.A multi-disciplinary team approach to implementing evidence-based guidelines. Nurs Crit Care. 2010;15:141–51. doi: 10.1111/j.1478-5153.2009.00378.x. [DOI] [PubMed] [Google Scholar]
- 16.Park MR, Jeon K, Song JU, Lim SY, Park SY, Lee JE, et al. Outcomes in critically ill patients with hematologic malignancies who received renal replacement therapy for acute kidney injury in an intensive care unit. J Crit Care. 2011;26:107.e1–6. doi: 10.1016/j.jcrc.2010.07.006. [DOI] [PubMed] [Google Scholar]
- 17.Kenney EM, Rozanski EA, Rush JE, deLaforcade-Buress AM, Berg JR, Silverstein DC, et al. Association between outcome and organ system dysfunction in dogs with sepsis: 114 cases (2003-2007) J Am Vet Med Assoc. 2010;236:83–7. doi: 10.2460/javma.236.1.83. [DOI] [PubMed] [Google Scholar]
- 18.Lever A, Mackenzie L. Sepsis: Definition, epidemiology, and diagnosis. BMJ. 2007;335:879–83. doi: 10.1136/bmj.39346.495880.AE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jacobson S, Johansson G, Winso O. Primary sepsis in a university hospital in northern Sweden: A retrospective study. Acta Anaesthesiol Scand. 2004;48:960–7. doi: 10.1111/j.0001-5172.2004.00458.x. [DOI] [PubMed] [Google Scholar]
- 20.Jhung MA, Banerjee SN. Administrative coding data and health care-associated infections. Clin Infect Dis. 2009;49:949–55. doi: 10.1086/605086. [DOI] [PubMed] [Google Scholar]


