Abstract
Context
Spinal cord injury and/or disorders (SCI/D) is a costly chronic condition. Impaired mobility, and lengthy travel distances to access specialty providers are barriers that can have adverse impact on expenses and quality of care. Although ample opportunities for use of telehealth technologies exist between medical facilities, and from clinical to home settings, field experience has largely been focused on home telehealth services to promote better patient self-management skills and improve clinical outcomes.
Findings
This paper provides an overview of published literature on use of telehealth technologies with the SCI/D population. Presentation of case studies describe telehealth as a potential strategy for addressing disparities in providing quality care, and explore comprehensive management of multiple health issues in individuals with SCI/D. Experiences of providers in both private sector health-care systems and VHA medical facilities are described. Development of telehealth clinical protocols and adaptive devices that can be integrated with equipment to accommodate for the functional limitations in the SCI/D population are discussed as necessary for expansion of use of telehealth services. Rigorous research studies are lacking. As use of this technology spreads and issues surrounding implementation are addressed, we look forward to increased research to assess and evaluate its efficacy in the SCI/D population.
Conclusion/clinical relevance
Telehealth in the home setting appears to be able to help persons with SCI/D remain in the community. As the use of telehealth increases, research will be necessary in both clinical and home settings to assess its efficacy in improving outcomes in the SCI/D population.
Keywords: Telehealth, Veterans, Spinal cord injuries, Preventive care, Accessibility
Introduction
Persons with spinal cord injury and/or disorders (SCI/D) are among the most complex and costly to patients to manage in any healthcare system.1 Ongoing management and treatment of acute and chronic health issues in this population routinely involve multiple body organ systems, including genitourinary, gastrointestinal, skin, respiratory, cardiovascular, autonomic nervous, and neuromuscular systems, as well as psychosocial issues. Limited mobility as a consequence of the disability, in addition to long distances to providers who are experienced in caring for those with SCI/D, creates geographic barriers to access and can have an adverse impact on expenses and quality of care. By giving an overview of published literature review and presenting case presentations, the goal of this article is to discuss telehealth services as a potential strategy for addressing disparities in providing quality care to people with SCI/D and explore comprehensive management of the multiple health issues faced by persons with SCI/D. Telehealth is defined as the delivery of health-related services and information via telecommunications technologies. Telehealth is the umbrella term used to describe clinical encounters between patients and healthcare providers at distant locations. Telehealth may be used for preventive, diagnostic, educational, and/or therapeutic intervention. Other terms for telehealth include telemedicine, telerehabilitation, or teleclinical specialty activities, which are described in more detail below.
Background
SCI/D care encompasses a broad range of conditions with traumatic and non-traumatic etiologies. Motor vehicle accidents, falls, diving accidents, gunshot wounds, and war injuries are the most common causes of traumatic spinal cord injury (SCI). Medical conditions that can result in non-traumatic SCI/D include, but are not limited to the following: tumors causing compression to the spinal cord, occlusion of spinal blood vessels due to arterial emboli or inflammatory vasculitis, developmental disorders (i.e. spinal bifida), neurodegenerative diseases, demyelinative diseases (i.e. multiple sclerosis), inflammatory disorders (i.e. transverse myelitis), and vascular conditions (i.e. arteriovenous malformation).
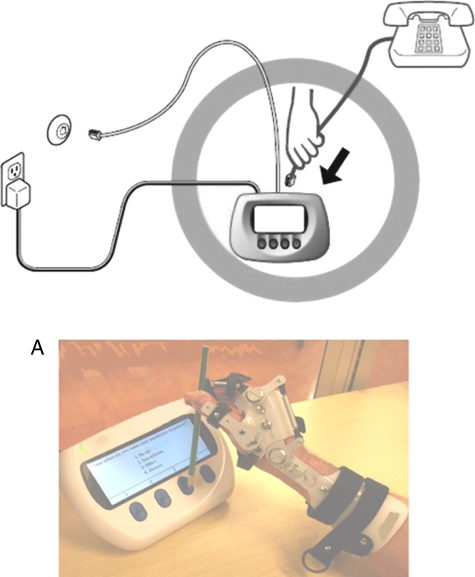
Figure 1.
Disease monitoring and messaging device setup with telephone in patient's home. (A) Device adapted for individual with hand impairment.
There are approximately 300 000 people living in the USA with a SCI and an additional 12 000 new cases each year.2 In the early 1970s, the National Institute on Disability and Rehabilitation Research (NIDRR) established a Spinal Cord Injury Model Systems of Care Network, which included medical facilities across the USA to provide comprehensive medical, vocational, and other rehabilitation services. Currently, there are 14 SCI Model Systems centers in the USA. To qualify for designation as a Model System and to receive funding from NIDRR, rehabilitation programs must provide continuity of care to include emergency medical services, expertise in treating trauma, a comprehensive rehabilitation program, vocational and psychological counseling services, and community reintegration services. Model systems must also conduct research of interest to NIDRR and collect data on SCI/D.3
In addition to the NIDRR SCI Model Systems of Care, the Department of Veterans Affairs, Veterans Health Administration (VHA) has developed the largest single network of SCI/D care in the nation. A disproportionately high percentage of persons with SCI/D are veterans, as almost 17% of persons with SCI/D in the USA are veterans. Therefore, SCI/D is an area of focus for the clinical care of veterans. Interdisciplinary teams at the 24 regional SCI/D centers located in Veterans Affairs (VA) facilities across the nation deliver primary care, acute rehabilitation, ongoing rehabilitation, disability management, health maintenance, and respite care. The SCI/D centers support 134 primary care teams at local VHA outpatient clinics designed to provide comprehensive lifelong healthcare for veterans with SCI/D.
Although the use of telehealth technologies is expanding rapidly into mainstream healthcare service delivery, there are only a handful of reports of applications that are specific to the SCI/D population. Telehealth services are often introduced to patient populations before research studies have been conducted to assess its efficacy. Our review of the existing literature indicates that some articles simply provided a description of telehealth applications that can be utilized by the SCI/D population, although a few have evaluated the use of specific telehealth interventions.
We identified limited access to specialty care, as well as the high cost of healthcare utilization by people with SCI/D as an issue that could be addressed by increased access to telehealth services. In addition, anecdotal clinical experiences and intervention studies will be used to illustrate that telehealth applications are feasible, have the potential to increase access to care, and lower the costs of SCI/D care. However, as promising as this technology is for increasing access to care for this population, rigorous research studies have not yet been conducted to evaluate the use of telehealth in the SCI/D population. As use of this technology spreads and the many issues surrounding its implementation are addressed, we look forward to increased research to assess its efficacy in the SCI/D population.
Access to care for individuals with SCI/D
Most healthcare providers with specialty training in either SCI/D care or rehabilitation generally provide care in tertiary care centers located in metropolitan areas. Providers in less populated areas may have less experience with specialty medical and psychosocial management of SCI/D. Fragmentation of specialty care that results from attitudinal differences, limitations in physical and staff resources of healthcare facilities, as well as transportation limitations, are obstacles that can hinder access to quality care for persons with SCI/D living in rural areas.4 Furthermore, quality and satisfaction with life activities can also be compromised especially when persons with SCI/D return from initial rehabilitation after SCI to their non-urban communities to face physically inaccessible buildings including their own homes as well as local churches, recreational establishments, and shopping facilities. Persons with SCI/D living in non-urban areas may be less likely to receive effective diagnostic evaluations and treatments from their local primary care facilities; healthcare providers in less urban areas may lack training and/or experience to recognize the unique challenges of the SCI/D patient. Telehealth offers the promise of a potentially low-cost methodology for increasing access to specialty care for the SCI/D population.
Cost of SCI/D care
Several studies have estimated the cost of caring for a person with SCI in the first year following injury. Dryden et al.5 identified 233 individuals with SCI and followed this group for a 6-year period. The cases were matched (1:5) with randomly selected controls from the general population. They found that in comparison with a general population control group, persons with SCI were 2.6 times more likely to be re-hospitalized and 2.7 times more likely to visit a physician. SCI persons also spent an average of 3.3 more days in the hospital and needed 30 times more hours of home care services.5 Another study (1995) found that average healthcare costs are about $200 000 in the first year of injury, with inpatient hospitalization for rehabilitation accounting for about 80% of this cost.6 Given the administrative pressures to reduce healthcare costs by reducing lengths of stay, there is potential risk for an increase in secondary complications post-discharge. One study found an association between shorter lengths of stay and re-hospitalization for pressure ulcers, a common problem in SCI/D.7 For persons with SCI/D, the risk for development of secondary complications due to reductions in length of hospital stay can be further exacerbated by having overall limited access to healthcare. A 2-year prospective study conducted by Knoll et al.8 found lack of access to primary care services in the first year, was a significant predictor for the development of pressure ulcers in the second year post-SCI. A retrospective, cohort study that reviewed primary care physician utilization patterns, specialist and emergency department visits of adults with traumatic SCI 1 year after the initial injury, concluded that higher emergency department visits may result from limited availability/accessibility of primary care services for SCI patients, especially in rural areas.9
Lengthy distance of travel to access specialty care, overall higher costs for SCI/D care, and the potential adverse impact of shortened lengths of hospital stays, are all factors that provide a compelling rationale to utilize telehealth technologies as a means to provide specialty services to address medical, rehabilitation, vocational, and mental health issues. With ongoing management to maintain optimal health and function, there is a potential for increasing access and lowering the chance of developing costly secondary complications in persons with SCI.
Literature review
Hatzakis et al.10 extrapolated findings from research conducted using telehealth to manage pressure ulcers, depression, and mobility impairments in patients of various disease states with rehabilitation issues, to argue the benefit of applying this technology to other chronic care patient populations. The authors reported that the clinical and financial benefits appear to be numerous.
In a pilot study that examined utilization of telehealth to improve outcomes in those with new and existing spinal cord injuries, Phillips et al.11 studied 11 subjects receiving telephone services in combination with still imaging as a means to promote positive self-care activity (including skin management) following discharge from rehabilitation. Clinical judgment and patient willingness to participate in sessions dictated the number of completed telehealth appointments. Results from this study indicate that telehealth can be successful in promoting skin care as well as other positive healthcare activities. The authors highlighted that positive outcomes from their video-based intervention support the need to conduct more rigorous clinically controlled studies in order to validate the widespread development and use of telehealth practices.12
One of the most common and costly problems in the SCI/D population continues to be the management and treatment of pressure ulcers. Pressure ulcers are a serious and potentially preventable condition for persons with SCI/D. Due to the lack of sensation and mobility, pressure ulcers are a serious, costly, and life-long complication of SCI/D. Once a person with SCI/D has had a severe pressure sore, he/she is at very high risk of developing additional skin breakdown. Since the 1990s, the Shepherd Center (the Model Systems Center in Atlanta, Georgia) has used telehealth for pressure ulcer prevention and management with patients who live long distances from a specialty clinic/medical center. In 2000, Mathewson et al.12 reported on the effectiveness and efficiency of monitoring a small sample of patients with pressure ulcers by using a still-image videophone. The nurse facilitating these weekly telehealth sessions was able to visually observe progress in the healing process. Important verbal information provided to the nurse wound care characteristics that could not be ascertained from the still images (i.e. odors from the wound, etc.). This telehealth application was well received by patients and eliminated costly and time-consuming long-distance ambulance transport to specialty care clinics for wound management.12
In 2001, preliminary results from a study regarding quality-of-life outcomes and mean annual hospital days indicate telehealth technology may positively impact post-discharge physical and psychological health of individuals with acute SCI.13 A total of 111 persons with acute SCI participated in the study during initial rehabilitation and were randomized into one of three groups lasting 9 weeks: telephone-based intervention following discharge, video-based intervention, or standard follow-up care. A year of follow-up monitoring days of hospitalization, depressive symptoms, and health-related quality of life found that mean annual hospital days for the standard care group were more than double than for the video group and 1.5 times more than for the telephone group.
Using telehealth technologies (e.g. home-based disease monitoring and messaging or videophone devices), depending on criteria met at patient assessment, Galea et al.14 provided feedback on a small customized and comprehensive rehabilitation program from the VA SCI Center in Bronx, New York. Their rationale for using telehealth technologies included the facilitation of continuity of care that encompassed medical, rehabilitation, psychological, and nutritional issues post-discharge. Patients with chronic co-morbidities or poor medication compliance utilized a text-based disease monitoring and messaging device (DMD). With this device, patients responded to daily questions about their condition. Based on their responses, feedback and adjustments were made to their care plan. Patients meeting the criteria of having more complex needs (e.g. pressure ulcer management, ventilator dependence, tracheostomies, new injuries, and those with high caregiver dependence) were scheduled for weekly videophone visits with members of the SCI interdisciplinary team. Depending on individual needs, in some cases, patients received direct viewing of pressure ulcers, dietary education, home safety evaluations, home exercise programs, psychosocial counseling, and information regarding proper installation and use of prosthesis or assistive devices. Patients participating in this intervention had an overall lower number of inpatient hospitalization days and lower length of stay in comparison with those receiving usual care.
In one of the few published randomized clinical trials measuring changes in self-efficacy in mobility-impaired patients that included patients with SCI/D, community-dwelling adults were found to have benefited equally from traditional in-home visits as compared to an intervention delivered via telehealth.15 This study included 82 individuals adjusting to new mobility devices (i.e. wheelchair or walker) in the community. Patients were randomized to a 4-week cycle of 1 hour per week occupation and physical therapy (PT) sessions targeting six specific mobility/transfer tasks that were delivered by a therapist either in the traditional home setting or remotely via telehealth using real-time audio and video imaging. No significant differences were found between those receiving care from a therapist in the home vs. remotely via telehealth.
Telehealth technologies
Telehealth technologies are telecommunication systems used to transfer patient information and/or conduct clinical encounters when the healthcare provider and patient are physically located at different locations. We define telehealth technologies by (1) the setting of equipment use, (2) type of data transferred, (3) timing of information transfer, (4) the way in which transmission occurs, and (5) the parties involved.
Setting of equipment use. Telehealth communication settings can involve encounters between patients and/or providers at different medical facilities or between providers at a medical facility and the patient's home.
Type of data transmitted. Data from telehealth encounters may include text, audio, video, or a combination of data types.
Timing of data transfer. Information transferred from telehealth encounters can be interactive (i.e. real time videoconferencing) or asynchronous (i.e. ‘store and forward’). With real-time videoconferencing, all participants involved are present to review and discuss data transmitted during the encounter. In a store and forward encounter, data is collected from the patient and/or provider at one location and transferred to a storage medium. The stored data is retrieved for review at a later date by a provider at a location distant from that of the patient and/or provider.
Method of information transfer. Data can be transmitted in a variety of ways, including use of analog/plain old telephone lines, digital lines, internet-based, and wireless technologies.
Parties involved. Clinical telehealth encounters can be used to communicate with individual patients or providers, as well as groups of patients or providers.
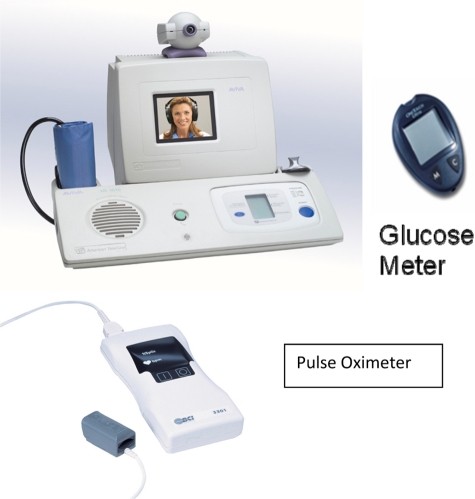
Videoconferencing may be used to facilitate communications between medical facilities (Fig. 5) and/or home telehealth settings (Fig. 2) to allow for real-time, synchronous, video-based clinical encounters between patients and/or providers. Real time encounters include assessments and evaluations as part of the clinical decision making process. Videoconferencing capabilities can be expanded to integrate with peripheral devices, including computers, diagnostic medical equipment, cameras, blood pressure, glucose and pulse oximeter monitors, weight scales, stethoscopes, and other instruments that are routinely found in a medical office to facilitate physical examinations (Fig. 3). Simultaneous transmission of voice, video, and data allow for the viewing and discussion of diagnostic test results or images during the clinical encounter.
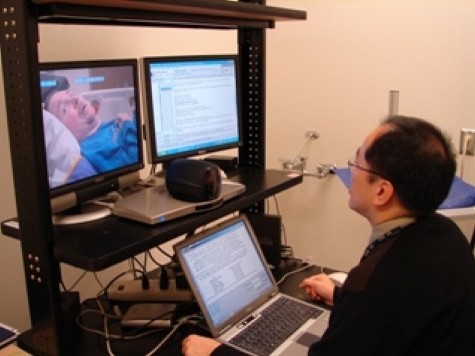
Figure 5.
Clinic to clinic telehealth (real-time communication).
Figure 2.

Videophone.
Figure 3.
Video Monitoring with peripheral devices.
Provider-to-provider communication. For the SCI/D population, videoconferencing between two facilities can be used to facilitate specialty medical consultations, where visual information can be used to enhance clinical decision-making. Examples for SCI/D include wound, bladder or bowel management issues, medical rehabilitation (e.g., physical and/or occupational therapy) focused communications, psychological counseling, and discussions related to admission transfer and discharge planning. Rehabilitation therapy encounters can include wheelchair assessment and evaluation, shoulder pain management, discussion of issues related to activities of daily living (ADLs) or instrumental activities of daily living (IADLs), rehabilitation evaluation or follow-up assessments. Videoconferencing technology can also be used to facilitate support groups as well as educate groups of patients or providers located at multiple facilities. The list of clinical telehealth applications described above is only a sampling of unlimited possibilities.
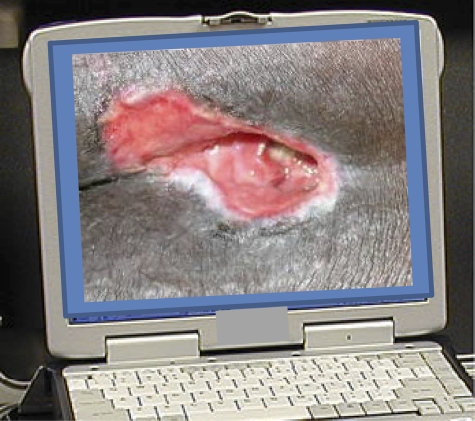
Timing of information transfer. Store and forward telehealth refers to processes by which clinical information (e.g. still images, motion video) can be stored and then sent to another site for specialty clinical evaluation at a later time (Fig. 4). Across facilities, store and forward telehealth technologies can be used to conduct screenings in large populations to identify common problems that could benefit from early intervention. An example of a store and forward telehealth application is the VA diabetic retinal imaging program, where digital retinal images are taken at a patient facility location and then transmitted and stored at another location, where the image is interpreted by a specialty provider at a future time.16 This process facilitates patients who live in remote locations to have access to high-quality specialty care.
Figure 4.
Store and forward (provider reviews information after it is collected remotely).
Home setting. In the home telehealth setting, store and forward applications can involve the asynchronous transfer of data from messaging devices (DMD) located in patients' homes to a medical center server, where providers can more efficiently monitor a panel of patient responses to make decisions regarding those who need immediate follow-up and interventions. Patients use the devices to respond to a series of daily questions surrounding their knowledge, behavior, and symptoms related to their condition. Questions that are administered to patients are integrated into Disease Management Protocols (DMPs). Patient responses are uploaded on a daily basis from the DMDs connected to the patient's home phone to secure databases that nurse case managers (CMs) can access via the internet. In this way, CMs are able to monitor a panel of patients by reviewing patients' daily responses to assess patients who may require urgent clinical follow-up. When a patient's response raises concerns, the CM can contact and/or intervene directly with the patient as needed. DMPs permit CMs to provide daily support to patients and their caregivers. Individuals using the DMPs receive support for their self-care behaviors (e.g. medication compliance, diet, and exercise) that are tailored to their unique conditions. Information received can be used to provide targeted interventions at the first sign of symptoms or gaps in behavior or knowledge that, if not addressed, could lead to escalation of symptoms or even hospitalization.
A VHA field work group recently developed a DMP specific for use with the spinal cord-injured population. The SCI DMP contains content related to general medical and psychosocial health, safety, pressure ulcer prevention, bladder and bowel management, activities and independent activities of daily living (i.e. ADLs and IADLs), sexuality issues, wheelchair, shoulder and pain management items that are specific to the spinal cord-injured population.
Clinical applications using telehealth in the SCI/D population
Case presentation #1
Co-management of pressure ulcers between SCI Tertiary Care Center and local SCI Outpatient Clinic
History/assessment: Fifty-five-year-old man with diagnosis of multiple sclerosis, chronic, non-healing right lower extremity stage III pressure ulcers with underlying osteomyelitis. They were primarily managed by patient's local SCI primary care team.
Indication for teleconsultation: For personal reasons, patient declined admission or transfer to SCI specialty care center.
Goal(s) achieved: Through videoconferencing between the patient, his wife, the physician assistant, wound care nurse at the local SCI clinic, and the consultant team at the SCI Center, the pressure ulcers were successfully co-managed. These ulcers continued to heal over the next 3 months.
Outcome: The patient's pressure ulcers were managed through teleconsultation between the SCI Tertiary Care Center and local SCI outpatient clinic, avoiding admission to the SCI Center, which would have been the standard practice. Therefore, the patient's request to stay home and not to be admitted to the SCI Tertiary Care Center was honored without adverse clinical outcomes.
Case presentation #2
Home telehealth visits for proper skin care practices
History/assessment: Forty-nine-year-old male with tetraplegia (C4 ASIA B) presents with diffuse asteatotic eczema and weeping excoriations on his lower extremities putting him at risk for infections. He had a skin biopsy done by dermatology and managed by the SCI/D wound specialist with improvement in skin integrity. On each return visit from home, his skin would have active dermatitis. The factors contributing to his chronic dermatitis were the overuse of soap, aggressive cleaning of his skin during baths, and infrequent use of proper emollients.
Indication for home telehealth visits: To help maintain the integrity of his skin education, support and close guidance of skin care was provided to the patient and his caregiver at home.
Intervention/treatment: Upon discharge home, a telehealth videophone device was used to provide direct observation and education of patient and caregiver about the need for more gentle washing and the need to avoid vigorous rubbing of the skin on his extremities. Recommendations were made for continuation of the antibiotic ointment applied to open areas on the skin by the caregiver until the patient's skin was healed. Education was also provided regarding emollients to be applied to healed skin on extremities daily to maintain proper skin integrity.
Goal(s) achieved: Videophone communication between medical facility and patient's home facilitated caregiver education and support. After initial videophone visit with the patient and caregiver to review recommendations and answer questions the patient received videophone visits weekly. Videophone visit 2 weeks after discharge showed affected areas beginning to heal. His caregiver was instructed to apply a thin layer of urea 10% lotion twice a day after gently washing skin. Based on visual inspection by videophone 3 weeks later, the urea lotion was discontinued as the skin was completely healed and treatment changed to a thin amount of aloe vista ointment daily to maintain proper skin integrity.
Outcome: Although the same recommendations for healing the skin lesions and prevention of recurrence were given to the patient at previous clinic visits, there was no resolution. With use of the telehealth videophone, better and sustained success was achieved. The patient's skin lesions healed. The patient also expressed satisfaction and confidence that the recommendations were beneficial as he was seeing sustained results. He also expressed confidence that his caregiver would be able to comply with recommendations given the added guidance from the telehealth provider. The caregiver expressed feeling supported and less guilty about the care she was providing to her brother. She also expressed feeling confident that she could access the providers and get her questions answered as she was providing the care to make sure she did it properly to achieve healing and prevent recurrence. The patient's skin condition improved and maintained good skin integrity after this intervention. Follow-up monthly videophone visits were made by a wound care specialist for monitoring skin integrity, reinforcement of caregiver education, and to provide support as clinically indicated.
Case presentation #3
Telehealth to discuss durable medical equipment
History/assessment: Fifty-two-year-old female with paraplegia (T4 ASIA B), admitted to SCI Center due to increase in spasticity which limited her ability to perform ADLs and functional transfers. Because patient lives 3 hours drive from the SCI Center, telehealth was used to facilitate continued skill development at local hospital prior to discharge to home.
Indication for telehealth: Occupational therapists (OTs) from the tertiary care SCI Center and local SCI outpatient clinic used teleconferencing to discuss optimal durable medical equipment for patient at risk for falls secondary to increase in bilateral left extremity spasticity and home physical barriers.
Intervention/treatment: Although the local spoke facility occupational therapist (OT) was knowledgeable about the patient's current functional status and physical limitations of the patient's home environment, the OT at the SCI Center had more advanced information on SCI equipment options. Both therapists discussed appropriate equipment for the existing home environment to provide most independence with ADLs and transfers.
Goal(s) achieved: Using provider–provider videoconferencing, SCI Center therapist demonstrated use of specialized equipment with local therapist to determine whether equipment could be used safely in patient home setting. Decision was made to use recommended equipment to decrease fall risk and request additional home assistance for ADLs and transfers.
Outcome: Additional home health assistance was provided to the patient. The recommended equipment was received and training provided to the patient's caregiver on safe usage. Although the patient continued to require assistance with ADLs and transfers, she had no falls utilizing the new equipment.
Case presentation #4
Psychological telehealth visits
History/assessment: A 45-year-old male with tetraplegia (T1 ASIA C SCI) and mood disorder, received his rehabilitation, post-injury, from a tertiary care SCI Center before moving home. As part of the rehabilitation process, the patient received individual psychotherapy twice a week and couples counseling sessions were scheduled when his wife was visiting from their home 300 miles away.
Indication for telehealth: Following the patient's move back home, he and his wife attempted behavioral health counseling with their hometown VA clinic. However, the couple found it difficult to develop the therapeutic relationship experienced with the SCI Center psychologist. The psychologist suggested starting weekly videoconferencing sessions to help with transition back to home and work life and to discuss recurring and evolving issues that were impacting his relationship with his wife post-SCI.
Intervention/treatment: Telehealth services focused on marital challenges and changes in the dynamic of the couple that ensued following the veteran's disability. The psychologist assisted the patient and his wife with adjustment to the physical limitations of an SCI. Examples include focus on current potential vs. wishful thinking, intimacy issues, being proactive regarding social activity decisions as a means to avoid isolation, and potential for development or exacerbation of depressive symptoms. This couple was elated with the availability of telehealth technology that helped to facilitate family stability and reintegration of the veteran back into his community of choice.
Goal(s) achieved: Monitoring of mood disorder and provision of cognitive behavioral therapy from a preferred provider to assist in the patient's reintegration into family and work life within his community of choice.
Outcome: Couple progressed satisfactorily and reports no further problems.
Case presentation #5
Urological teleconsultation
History/assessment: Patient with multiple sclerosis and neurogenic bladder reported skin problems with the use of external condom catheter, requested to have insertion of indwelling catheter. This patient also did not tolerate the use of anti-cholinergic agents for the management of his neurogenic bladder.
Indication for telehealth: Local SCI outpatient clinic primary care providers requested consultation with a neuro-urologist to better understand treatment options for neurogenic bladder (indwelling catheter vs. suprapubic catheter), and whether urodynamic testing would be beneficial.
Intervention/treatment: A telehealth conference between the local SCI outpatient clinic providers, patient and the SCI Center neuro-urologist took place to address whether: (1) urodynamics evaluation would be helpful to determine function of bladder and sphincter to rule out bladder sphincter dyssynergia, (2) anti-cholinergic medication was necessary, and (3) high bladder pressures that might put the patient at risk for upper tract problems. Various bladder drainage options and their pros and cons were discussed in detail. It was finally determined that urodynamics evaluation would not change the treatment plan, and that it was appropriate for the patient to have an indwelling catheter for bladder management. The patient was to be monitored for any complication and if so, alternative bladder management option was to be considered.
Goal(s) achieved: Telehealth consultation with an SCI Center neuro-urologist provided guidance to local SCI outpatient clinic providers and patient for the most appropriate bladder management method.
Outcome: Patient received neuro-urology specialty consultation that was not available at the local SCI outpatient clinic, and avoided unnecessary procedure.
Case presentation #6
Discharge planning/coordination of care meeting
History/assessment: Patient is a 34-year-old male with tetraplegia (C3 ASIA A), secondary to cervical ependymoma. He was electively admitted to an SCI Center inpatient unit from a Local Spinal Cord outpatient clinic for: (1) follow-up with hematology/oncology service with routine magnetic resonance imaging (MRI) of the spinal cord and (2) inpatient evaluation of progressive spasticity and rehabilitation after an unsuccessful trial of outpatient management of spasticity issues that affected his upper extremity (UE) functionality and control of his motorized wheelchair.
Indication for telehealth: Discharge Planning meeting between SCI Center and local SCI outpatient clinic to address various complex rehabilitation issues, including his spasticity management and power mobility issues, in order to provide progress report on the achievements during the inpatient rehabilitation stay, and describe follow-up requirements to the local SCI outpatient clinic after discharge from the SCI Center.
Intervention/treatment: During hospitalization, the patient's spasticity medications were adjusted to optimize the therapeutic balance between motor strength and UE functionality. He was seen 5–6 times per week by an SCI OT to improve his functional UE range of motion, to adjust his balanced forearm orthosis (BFO) for self-feeding, and in collaboration with a vocational rehabilitation counselor, to assess the use of assistive technologies to improve his ability to use a computer. Physical Therapy (PT) was consulted for evaluation and treatment of bed mobility, transfers, and truncal stability.
Goal(s) achieved: Prior to discharge, a telehealth conference was scheduled with the patient, local SCI outpatient clinic nurse and social worker, SCI Center social worker, physical therapist, OT, psychologist, and attending physician. During the meeting, local outpatient providers were informed that the routine MRI ruled out recurrence of ependymoma, medications were adjusted to improve motor strength and functionality with degree of spasticity tolerated by the patient. With respect to OT progress, it was explained that BFO was adjusted to allow patient to self-feed at home and that recommendations for home computer workstation set-up was being coordinated between his therapist, prosthetics and his vocational rehabilitation counselor. Further home BFO training with a local OT was recommended. With respect to PT, it was recommended that a local PT continue therapy started at the SCI Center, with the patient and his caregiver on a stretching program and transfer training program so that the patient would continue in his ability to transfer with moderate assistance. Future plans for evaluation during patient's next scheduled admission for routine follow-up of spinal tumor included evaluation for potential tendon transfer and functional electrical stimulation cycle training.
Outcomes: Precise and detailed progress report and follow-up recommendations were given by the SCI Center team to the local SCI outpatient clinic team, with active participation by the patient. This allowed seamless transition between the inpatient stay and further outpatient management for a complex rehabilitation patient.
Development of SCI/D telehealth applications
As described in this article, use of telehealth technologies in the SCI/D population has been reported to provide socioeconomic benefits related to patient education and care. Telehealth services appear to be an especially helpful and efficient option for providing care to patients with SCI/D living in rural areas, those living long distances from specialty care clinics, and for those where travel itself may worsen a medical condition (i.e. pressure ulcers). Early telehealth studies and projects have identified a need for not only improved telecommunication technologies, but also for better health care team coordination to facilitate smoother interaction between providers and patients.17 The James A. Haley Veterans Hospital SCI/D Center in Tampa, Florida has used telehealth since the early years of 2000 to provide specialty care to veterans in their hometown communities through videoconferencing between the SCI/D Center and the patient's local outpatient clinic. This clinical video telehealth program has resulted in a decrease in inpatient admissions, and has also served to encourage the patient to explore and use community resources.17
In the USA, the NIDRR Spinal Cord Injury Model Systems of Care Network and VHA Spinal Cord Injury/Disorders System of Care, described earlier, represent established networks of care that can be utilized as a physical foundation for building telehealth programs across each of these facilities. SCI/D specific clinical applications for telehealth include providing specialty medical, equipment, vocational or other consultation for individual patients, or to exchange interdisciplinary expertise across SCI/D tertiary centers (e.g. grand rounds). These services can continue to expand to train primary care providers on specialty care issues, and serve patients at smaller primary care clinics that feed into the NIDRR and VHA Systems of Care.
As for home telehealth applications, to date, telehealth technologies have primarily been developed for use with able-bodied populations. Assistive devices that can integrate with telehealth technologies have been explored in terms of their potential to help with the SCI/D population but are virtually non-existent at the current time. Currently, telehealth services for persons with SCI/D may necessitate the assistance of a caregiver so that privacy assumed of a typical provider–patient encounter may be compromised. We can only expect that as technology improves, these capabilities will be included in the hardware and software for telehealth applications. Future technological improvements will help to overcome the physical barriers (i.e. lack of hand function) common in this population. On the other hand, they also provide an opportunity to educate caregivers about the patient's condition.
The socioeconomic benefits also apply to home telehealth programs. This includes being able to identify and educate patients about potential problems to provide earlier intervention, minimize emergency room visits, and hospitalizations. Frequently reported but difficult to deal with common SCI/D complications (e.g. type 2 diabetes, hypertension, obesity, bladder infections, and depression), can be targeted and promptly addressed. Another benefit of telehealth can be the provision of consistent psychological support to those aging with SCI/D and their informal caregivers.18 A SCI/D DMP for use with home telehealth DMDs was recently developed by a VHA SCI field work group, and is scheduled to be released shortly. Areas in need of development are protocols that incorporate clinical practice guidelines into patient-and provider-focused home telehealth applications.14,19 Further development of more sophisticated telehealth protocols will never replace in-person interaction between patient and provider but may eventually make it easier for patients to receive high-quality, state-of-the-art care at home.
Broad questions of socioeconomic efficacy and equity continue to present barriers to large-scale implementation of telehealth services.20 Future research must include randomized clinical trials with sufficient sample sizes and robust research designs capable of comparing telehealth services with conventional care.10,14 Studies to-date lack rigorous designs and robust sample sizes, which limit the ability to examine differences between subgroups and statistical power needed to draw conclusions regarding specific telehealth interventions. Since many studies have only described feasibility and estimated cost savings, these outcomes need to be rigorously evaluated and quality of life and satisfaction outcomes need to be addressed as well. Other outcomes of interest may include improved medical status, clinical outcomes, impact on system resources and organizational management, provider and patient attitudes, provider–patient relationships and communication among clinical and administrative stakeholders at the program and systems levels.
Aside from the need for protocols for implementing evidence-based practice guidelines, effective implementation of specific clinical telehealth interventions for the SCI/D population needs further fine tuning. Opportunities for clinical program development and collaboration between healthcare providers are abundant. Telehealth services that are built upon a patient-centered model have the potential to greatly enhance the quality of life of persons with SCI and disorders.
Acknowledgments
This material was supported in part by the Department of Veterans Affairs, Veterans Health Administration, Health Services Research and Development, Quality Enhancement Research Initiative. The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs or the United States Government.
References
- 1.Yu W, Ravelo A, Wagner TH, Barnett PG. The relationships among age, chronic conditions, and healthcare costs. Am J Manag Care 2004;10(12):909–16 [PubMed] [Google Scholar]
- 2.Soopramanien A, Pain H, Stainthorpe A, Menarini M, Ventura M. Using telemedicine to provide post-discharge support. J Telemed Telecare 2005;11Suppl 1:68–70 [DOI] [PubMed] [Google Scholar]
- 3.National Spinal Cord Association Resource Center. Factsheet #4b: Spinal Cord Injury Rehabilitation Programs: CARF/NIDRR. Available from: http://www.makoa.org/nscia/fact04b.html#NIDRR.
- 4.Bloeman-Vrencken JHA, DeWitte LP, Post MWM. Follow-up care for persons with spinal cord injury living in the community: a systematic review of interventions and their evaluation. Spinal Cord 2005;43:462–75 [DOI] [PubMed] [Google Scholar]
- 5.Dryden DM, Saunders LD, Rowe BH, May LA, Yiannakoulias N, Svenson LW, et al. Utilization of health services following spinal cord injury: a 6-year follow-up study. Spinal Cord 2004;42(9):513–25 [DOI] [PubMed] [Google Scholar]
- 6.Waters RL, Apple DF, Jr, Meyer PR, Jr, et al. Emergency and acute management of spinal trauma. In: Stover SL, DeLisa JA, Whiteneck GG. (eds.) Spinal cord injury: clinical outcomes from the model systems. Gaithersburg, MD: Aspin Publishers, Inc; 1995 [Google Scholar]
- 7.Jones ML, Evans RW. Outcomes in managed care environment. Top Spinal Cord Inj Rehabil 1998;3:61–73 [Google Scholar]
- 8.Knoll T, Neri MT, Ho PS. Secondary conditions in spinal cord injury: results from a prospective survey. Disabil Rehabil 2007;29(15):1229–37 [DOI] [PubMed] [Google Scholar]
- 9.Munce SSE, Guilcehr SJ, Couris CM, et al. Physician utilization among adults with traumatic spinal cord injury in Ontario: a population-based study. Spinal Cord 2009; 2009 Jun; 47(6):470–6 Epub 2009 Jan 20. [DOI] [PubMed] [Google Scholar]
- 10.Hatzakis M, Haselkorn J, Williams R, Turner A, Nichol P. Telemedicine and the delivery of health services to veterans with multiple sclerosis. J Rehabil Res Dev 2003;40(3):265–82 [PubMed] [Google Scholar]
- 11.Phillips VL, Temkin AJ, Vesmarovich SH, Burns R. A feasibility study of video-based home telecare for clients with spinal cord injuries. J Telemed Telecare 1998;4(4):219–23 [DOI] [PubMed] [Google Scholar]
- 12.Mathewson C, Adkins VK, Jones ML. Initial experiences with telerehabilitation and contingency management programs for the prevention and management of pressure ulceration in patients with spinal cord injuries. J Wound Ostomy Continence Nurs 2000;27(5):269–71 [DOI] [PubMed] [Google Scholar]
- 13.Phillips VL, Vesmarovich S, Hauber R, Wiggers E, Egner A. Telehealth: reaching out to newly injured spinal cord patients. Public Health Rep 2001;116Suppl 1:94–102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Galea M, Tumminia J, Garback L. Telerehabilitation in spinal cord injury persons: a novel approach. Telemed J E Health 2006;12:160–2 [DOI] [PubMed] [Google Scholar]
- 15.Sanford JA, Griffiths PC, Richardson P, Hargraves K, Butterfield T, Hoenig H. The effects of in-home rehabilitation on task self-efficacy in mobility-impaired adults: a randomized clinical trial. J Am Geriatr Soc 2006;54:1641–8 [DOI] [PubMed] [Google Scholar]
- 16.Conlin PR, Fisch BM, Orcutt JC, Hetrick BJ, Darkins AW. Framework for a national teleretinal imaging program to screen for diabetic retinopathy in Veterans Health Administration patients. JRRD 2006;43(6):741–8 [DOI] [PubMed] [Google Scholar]
- 17.Weinel D. The sunshine network teleconsultation initiative. SCI Nurs 2000;17(1):22–30 [PubMed] [Google Scholar]
- 18.Mozer E, Franklin B, Rose J. Psychotherapeutic intervention by telephone. Clin Interv Aging 2008;3(2):391–6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lapierre NM, Blackmer J, Coutu-Wakulczyk G, Dehoux E. Autonomic dysreflexia and telehealth. Can Nurs 2006;102(7):20–5 [PubMed] [Google Scholar]
- 20.Wakeford L, Wittman PP, Schmeler MR. Telerehabilitation position paper. Am J Occup Ther 2005;59(6):656–60 [DOI] [PubMed] [Google Scholar]