Abstract
Low functional literacy and low health literacy continue to be under-recognized and are associated with poorer patient health outcomes. Health literacy is a dynamic state influenced by how well a healthcare system delivers information and services that match patients’ abilities, needs and preferences. Oncology care poses considerable health literacy demands on patients who are expected to process high stakes information about complex multidisciplinary treatment over lengths of time. Much of the information provided to patients in clinical care and research is beyond their literacy levels. In this paper, we provide an overview of currently available guidelines and resources to improve how the needs of patients with diverse literacy skills are met by cancer care providers and clinics. We present recommendations for health literacy assessment in clinical practice and ways to enhance the usability of health information and services by improving written materials and verbal communication, incorporating multimedia and culturally appropriate approaches, and promoting health literacy in cancer care settings. The paper also includes a list of additional resources that can be used to develop and implement health literacy initiatives in cancer care clinics.
The National Assessment of Adult Literacy (NAAL) reported that approximately 30 million Americans were functionally illiterate in 2003, meaning they could not perform basic reading tasks necessary to function fully in society.1 Literacy is strongly correlated with health literacy—the ability to obtain, process, and understand health information to make appropriate decisions—with the latter involving content-specific demands.2–4 The NAAL found that an estimated 36% of US adults had only Basic or Below Basic health literacy skills and that vulnerable populations (racial/ethnic minorities, older adults, and those with low income) had lower health literacy. These findings are concerning given the complex demands placed on patients to read, write, compute, solve problems, and understand novel information in order to navigate healthcare systems and achieve good health.
Research has demonstrated that low literacy and low health literacy are associated with impaired patient-provider communication, patient nonadherence, increased hospitalization, and poorer health. Low literacy is also associated with patient exclusion from clinical trials and other studies, adverse reactions, and poor understanding of medical information.5,6 In addition, low health literacy has been associated with receipt of fewer preventative procedures, and less knowledge of disease self-management and ability to participate in treatment decisions.2,4,5,7–9 These findings have implications for the quality and costs of health-care for patients with low health literacy.10
Current conceptualizations of health literacy consider patients’ abilities as well as the demands of the healthcare system and its ability to deliver appropriate information and services.4,11 Good health literacy is a dynamic state reached when patients’ skills, preferences, and expectations connect with those of healthcare providers and resources. From a patient's perspective, health literacy touches countless aspects of care such as selecting providers, completing forms, comprehending concepts such as probability and risk, and understanding how to take medications. As expectations for patients to take active roles in healthcare increase, there are added demands to seek information, make health decisions, engage in self-management, and understand rights and responsibilities. Cancer and other chronic illnesses pose additional health literacy demands.
Oncology patients are expected to process large amounts of information about complex care delivered by multiple providers over long courses of time while also contending with related financial and legal documents.12 Ironically, patients and their families are asked to assimilate crucial information at times of great stress (eg, before surgery, shortly after diagnosis or disease recurrence, during end-of-life decisions) that are associated with anxiety-induced decreases in attention, comprehension, and retention. Further, patients often feel pressure during these critical times to make treatment decisions quickly given the seriousness of the disease.13 Many oncology providers are aware of these challenges and subsequently provide supplemental written material such as pamphlets about cancer and treatment, and sheets describing preparation for procedures. Unfortunately, much of this material is written at reading levels beyond those of patients’, and studies have found that recall of information by patients with cancer can be limited and inaccurate.13 Clearly, there is room to improve how the needs of patients with low literacy and health literacy are met; in this paper, we provide recommendations for oncology providers and clinics.
Health Literacy Assessment in Clinical Practice
To better match healthcare materials and services to patients’ literacy skills, accurate and clinically feasible assessment methods are needed. Using self-reported educational level has been shown to inaccurately estimate patients’ literacy.13,14 Numerous reading assessment tools exist, including ones that are composed of medical terms and content. The two most widely used measures are the rapid estimate of Adult Literacy in Medicine (REALM) and the Test of Functional Health Literacy in Adults (TOFHLA).15,16
The REALM is a word recognition and pronunciation test that does not require comprehension, whereas the TOFHLA uses actual materials patients may encounter in healthcare settings to determine how well they can perform the basic reading comprehension and numeracy tasks necessary to function successfully in those environments. Although neither test offers comprehensive health literacy assessment, each has been shown to predict patients’ health knowledge, behaviors, and outcomes.11 Studies implementing these measures with patients in oncology clinics have found them easy to administer and score and acceptable to patients regardless of their literacy levels, which helps dispel concerns that patients may be offended.13 A short version of the TOFHLA takes approximately 7 minutes to complete, whereas the REALM can be completed in just a few minutes.13,17 However, a trained interviewer is required to administer both tests.
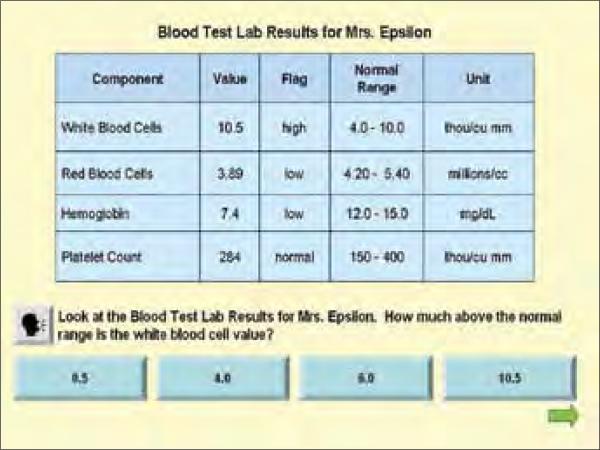
More recent efforts are being made to develop health literacy tests that patients can self-administer. For example, a Talking Touchscreen has been developed, pairing a touch-screen computer with audio components that allow patients to choose to have questions read aloud (Figure 1). The Talking Touchscreen has proven to be user-friendly and acceptable to individuals regardless of literacy levels or computer skills.18–20 Health literacy measures using this technology will soon be available in english and Spanish.
Figure 1. Screen Image of a Health Literacy Assessment Quantitative Item from the Talking Touchscreen.
Respondents can press the gray speaker button to hear the question read out loud and answer the question by pressing one of the blue response buttons.
Another method is to capture the interactive aspect of health literacy by assessing patient reports of how understandable information is made in healthcare settings. The Consumer Assessment of Healthcare Providers and Systems (CAHPS) program, whose standardized surveys of patients’ healthcare experiences have provided valuable benchmark data, has recently developed a Health Literacy item Set that can serve as a measure of providers’ health literacy practices (available in English and Spanish at http://www.cahps.ahrq.gov/content/products/HL/PROD_HL_intro.asp). The CAHPS Health Literacy item Set includes items addressing communication with physicians about health problems and concerns, medications, tests, forms, and disease self-management. Thus, the measure can help providers and clinics identify areas of strength and topics for quality improvement. Further, the items have all been mapped to health literacy practice recommendations by the American Medical Association.
The utility of in-clinic health literacy assessment will depend on how the data are used and connected to improved communication strategies. Measures used for screening purposes can identify patients who may require additional support; this may be especially valuable when comprehension of health information is critical (eg, when patients need to make decisions regarding stem cell transplant or hospice care). Health literacy data aggregated at the clinic level can help identify what education materials and communication strategies are appropriate and gauge the effectiveness of practice changes after they are implemented. Another approach is to assume that all patients benefit from improved communication and to implement universal precautions based on best practices. existing health literacy interventions consist primarily of making health information and services more usable.
Improving the Usability of Health Information
WRITTEN MATERIALS
Printed materials, such as test results, discharge documents, home care instructions, medication inserts, and insurance and social service forms are often written at reading levels mis-matched to those of the intended audience.4,21 As a first step, the reading level of all written patient materials should be tested. However, reducing the reading level is an incomplete solution. Whenever possible, plain language should be used.
Material using plain language can be understood relatively quickly and makes relevant information easy to find and understand.22 Components of plain language include using familiar words and the active voice, avoiding or defining medical jargon and technical terms, simplifying grammar, breaking information into understandable chunks preceded by headings, and presenting key information first and reiterating it later. Certain features should be avoided, because individuals with low literacy find them difficult to understand; those include text in all capitals, italics, acronyms or abbreviations, quotes, long lines or lists, and statistics (these should be placed in parentheses or replaced with descriptive words, such as many or most, when possible).22–24 Likewise, good formatting can increase the readability of patient materials, for example, using bullets and at least 12-point font and leaving plenty of white space. The understandability of written materials can also be improved by using a conversational style, limiting messages (to three to four per document), keeping them short, and presenting them one at a time.23,24 Graphics and visual cues can highlight or illustrate important information if care is taken to make them understandable. It is best to keep to one message per visual, place images in context, use brief captions where necessary, and avoid visuals that are abstract or merely decorative.23,24 Lastly, materials intended to influence patient behavior should be made actionable by stating what is to be gained from the information and what steps should be taken, as well as listing resources and focusing on the positive whenever possible. This is important because the way health information is presented can increase patients’ self-efficacy, or beliefs that they can accomplish certain tasks, which is associated with attempts to change health behaviors.25 So, for example, the take-home forms for patients receiving a new chemotherapy treatment should follow the above guidelines and describe possible adverse effects, group them in categories, emphasize the most common ones, and clearly state what patients should do if symptoms occur before their next medical visit.
While written materials are being developed, it is critical to test their usability and acceptability. Patient input is important, because research suggests that more information is not always better (eg, when patients are facing decisions).25 For instance, many cancer care clinics would benefit from patient feedback on the comprehensive orientation binders they provide to new patients.
The readability of written materials presented to patients at critical points in their care—for example, consent documents for medical procedures, treatment, and participation in clinical trials—is often higher than patients’ reading levels.5,21,26,27 Easy-to-read consent forms have been developed and are preferred by patients, associated with reduced anxiety, and not found offensive by well educated patients.5,26,27 Likewise, advance directives, which have low completion rates, are usually written at disproportionately high reading levels and include substantial medical and legal terminology. However, easier-to-read advance directives have been designed, are preferred by patients, and are associated with higher completion rates.28
VERBAL COMMUNICATION
Many of the recommendations for good written materials apply to verbal messages (eg, using plain language, keeping content simple and actionable). Patient-provider communication is also an opportunity to complement the information in written materials and check for understanding in a shame-free environment. For example, oncology clinicians should refer to written prescriptions and other take-home materials while explaining what each medication is for, dosages, adverse effects, and so forth, so that patients are familiar with where to find the information later. Likewise, it is common practice to verbally review written consent forms with patients and confirm understanding.
Research has linked providers’ communication skills with patient outcomes, such as satisfaction and adherence.3 Accordingly, communication skills, particularly those that are patient-centered (responsive to values, preferences, and needs), are becoming an essential part of medical practice and involve collaborative efforts with patients. Along those lines, the Partnership for Clear Health Communication (Table 1) created the Ask Me 3 patient and provider education tools and implementation guides to improve patient-provider communication. Available in English, Spanish, and other languages, the Ask Me 3 materials promote three basic questions that patients should ask: “what is my main problem?” “what do i need to do?” and “why is it important for me to do this?” These kinds of patient prompt sheets have been found to improve patient confidence and anxiety.29 Providers can also work with patients to achieve understanding of health information by using the teach-back method in which the person receiving the message is asked to restate it using their own words.24 Other key provider communication skills include active listening and asking open-ended questions (those beginning with what or how) versus closed-ended ones (those with response options of only yes or no) to minimize opportunities for misunderstandings.
Table 1.
Internet Resources on Health Literacy
| SOURCE | TITLE | LINK (URL) |
|---|---|---|
| For More Background on Health Literacy | ||
| US Department of Education, Institute of Education Sciences, National Center for Education Statistics | The Health Literacy of America's Adults: Results from the 2003 National Assessment of Adult Literacy | www.nces.ed.gov/pubsearch/pubsinfo.asp?pubid=2006483 |
| US National Institutes of Health, National Library of Medicine | Current Bibliographies in Medicine: Understanding Health Literacy and Its Barriers | www.nlm.nih.gov/pubs/cbm/healthliteracybarriers.html |
| Institute of Medicine | Health Literacy: A Prescription to End Confusion | www.nap.edu/openbook.php?isbn=0309091179 |
| US Department of Health and Human Services | ||
| Office of Disease Prevention and Health Promotion | Quick Guide to Health Literacy | www.health.gov/communication/literacy/quickguide |
| Healthy People 2010, Health Communication | www.healthypeople.gov/Document/HTML/Volume1/11HealthCom.htm | |
| Communicating Health: Priorities and Strategies for Progress | www.odphp.osophs.dhhs.gov/projects/HealthComm/ | |
| Health Resources and Services Administration | Health Literacy | www.hrsa.gov/healthliteracy/default.htm |
| Office of the Surgeon General | Proceedings of the Surgeon General's Workshop on Improving Health Literacy | www.surgeongeneral.gov/topics/healthliteracy/toc.html |
| Agency for Healthcare Research and Quality | Health Literacy and Cultural Competency | www.ahrq.gov/browse/hlitix.htm |
| Literacy and Health Outcomes | www.ahrq.gov/clinic/tp/littp.htm | |
| For More on Accessible Health Materials | ||
| US National Institutes of Health, National Cancer Institute | Pink Book—Making Health Communication Programs Work | www.cancer.gov/pinkbook |
| American Medical Association | Health Literacy | www.amafoundation.org/go/healthliteracy |
| The Joint Commission | Improving Health Literacy to Protect Patient Safety | www.jointcommission.org/newsroom/presskits/health_literacy |
| Harvard School of Public Health | Teaching Patients with Low Literacy Skills, Second Edition | www.hsph.harvard.edu/healthliteracy/doak.html |
| The Plain Language Action and Information Network | PlainLanguage.gov: Improving Communications from the Federal Government to the Public | www.plainlanguage.gov |
| National Patient Safety Foundation | Partnership for Clear Health Communication | www.npsf.org/pchc/index.php |
| US Department of Health and Human Services | ||
| Centers for Disease Control and Prevention | Scientific and Technical Information: Simply Put | www.cdc.gov/DHDSP/cdcynergy_training/Content/activeinformation/resources/simpput.pdf |
| Health Marketing | www.cdc.gov/healthmarketing/cdcynergy | |
| Usability.gov | Your Guide for Developing Usable and Useful Web Sites | www.usability.gov |
| Office of Minority Health | National Standards for Culturally and and Linguistically Appropriate Services in Health Care: Final Report | www.omhrc.gov/assets/pdf/checked/finalreport.pdf |
| Hablamos Juntos | Language Policy and Practice in Health Care | www.hablamosjuntos.org |
MULTIMEDIA APPROACHES
The vast amount of internet searching for health information demonstrates an interest in multimedia sources. Technology platforms have been recommended as a means of improving health information delivery.3,30 The usability of these new modalities benefits from the elements that improve written and verbal communication. Other components of patient-centered multimedia platforms include easy navigation, interactive features and personalized content, enhancement of content via audio files or video, and feedback from usability testing with the intended audience throughout the development process.31
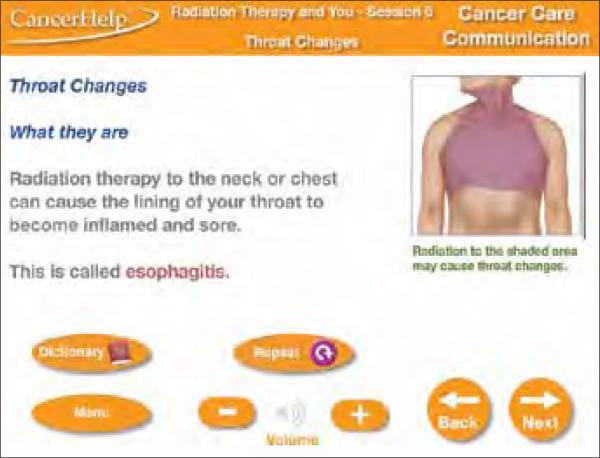
An example of a multimedia tool used in cancer centers is the CancerHelp Patient Education Software, which consists of material from the National Cancer Institute presented in audiovisual slideshows on touchscreen computer kiosks. All information is read aloud and can be printed; thus, it is accessible to individuals at all literacy levels (Figure 2). Two of the authors (EAH and SFG) are conducting a study, in collaboration with the CancerHelp Institute, to enhance the software (eg, by adding navigational features, videos, a local resource module, and an interactive medical visit checklist to serve as a prompt sheet for patient-provider discussion) and to test its effectiveness in a randomized clinical trial.
Figure 2. Screen Image of a CancerHelp Patient Education Slide from a Talking Touchscreen Kiosk.
All CancerHelp screens currently use similar format and navigational features. © 2010 The CancerHelp Institute
Improving the Usability of Health services
Health literacy demands are placed on patients as soon as they set foot in a hospital or clinic. Abundant signs, maps, directions, instructions, and schedules containing unfamiliar phrases and symbols can confuse and overwhelm persons with limited literacy.32,33 The physical environment can be made more accessible through use of clear signage and universal symbols, such as those developed by the Robert Wood Johnson Foundation and Hablamos Juntos (Table 1).
Other in-clinic strategies to promote health literacy include developing and distributing glossaries of commonly used terms, including family members in discussions at patients’ requests, and allowing patients multiple opportunities to meet with providers when they are required to process substantial information (eg, when considering new treatments). The interdisciplinary staffs at many cancer centers are great assets in meeting patients’ health literacy needs. Oncology nurses and pharmacists can reinforce information conveyed by oncologists, and allied health professionals, such as social workers, psychologists, and dieticians, can provide specialized information and services. In addition, patient navigators, who are healthcare workers or highly trained liaisons, can provide assistance by coordinating services, facilitating referrals, and finding appropriate resources.32 Such support can be critical to patients faced with tasks that involve high health literacy demands (eg, completing registration forms, understanding and managing medical bills).
CULTURALLY APPROPRIATE APPROACHES
Health literacy originates from interactions of cultural and social factors with healthcare characteristics. Linguistic and cultural mismatches between patients and services can exacerbate communication difficulties for patients with limited literacy.4,30 Given the extent of diversity in the United States, it is essential that healthcare providers and services move from a “culture of medicine” to cultural competency, or the ability to recognize and address patient beliefs, attitudes, and preferences. Integral to cultural competency is the ability to communicate in linguistically and culturally appropriate manners.
As a starting point, clinics should know the basic sociodemographic makeup of their patient populations in order to ensure that the materials and services they provide are relevant. Written and multimedia materials should reflect the cultural diversity, language, and literacy skills of the intended users.25 In particular, clinics that serve patients with limited English proficiency should provide multilingual plain language health materials and trained medical interpreters. Multilingual written materials should be professionally translated and field tested.23
PROMOTING HEALTH LITERACY
All clinic staff need to be aware of health literacy, armed with appropriate materials, and contributing to a responsive environment in order for initiatives to be successful. Staff, across disciplines, should be trained in health literacy practices in orientations, regular workshops, and continuing medical education exercises. Accountability can be established by adding health literacy promotion to the communication skills included in employee and program evaluations and by convening a workgroup to oversee initiatives.33 Clinics can also embed health literacy into their mission statements, strategic plans, policies, and best practices. Given that promoting health literacy requires effort on the part of cancer care providers, whose jobs are already demanding, we have attempted to facilitate the process by providing a list of resources that can be used to develop and implement initiatives (Table 1). In addition, the Agency for Healthcare research and Quality will be releasing in 2010 a Health Literacy Universal Precautions Toolkit that is designed to assist clinics in integrating health literacy strategies into their practices with minimal burden on resources.
Acknowledgments
The authors thank Celia M. Muench, MSIR, and Ed Miller, BA, for providing materials from the CancerHelp Patient Education Software. We also thank Cindy Brach, MPP, Darren A. DeWalt, MD, MPH, and Beverly A. Weidmer, MA, for providing information about upcoming health literacy tools from the Agency for Healthcare Research and Quality.
This manuscript was partially supported by grant R18-HS017300 from the Agency for Healthcare Research and Quality and grant R01-HL081485 from the National Heart, Lung, and Blood Institute.
Footnotes
Conflicts of interest: None to disclose.
Contributor Information
Sofia F. Garcia, Department of Medical Social Sciences, Northwestern University Feinberg School of Medicine, Chicago, Illinois..
Elizabeth A. Hahn, Department of Medical Social Sciences, Northwestern University Feinberg School of Medicine, Chicago, Illinois..
Elizabeth A. Jacobs, Division of General Medicine and Primary Care, John H. Stroger Jr. Hospital of Cook County and Rush University Medical Center, Chicago, Illinois..
References
- 1.Kutner M, National Center for Education Statistics . Literacy in Everyday Life: Results from the 2003 National Assessment of Adult Literacy (NCES 2007-480) US Department of Education; National Center for Education Statistics; Washington, DC: 2007. [Google Scholar]
- 2.Kutner M, Greenberg E, Jin Y, Paulsen C. The Health Literacy of America's Adults. National Center for Education Statistics: US Department of Education; Washington, DC: 2006. NCES publication 2006-483. [Google Scholar]
- 3.US Department of Health and Human Services . Healthy People 2010: Understanding and Improving Health. 2nd ed. US Government Printing Office; Washington, DC: 2000. [Google Scholar]
- 4.Committee on Health Literacy. Nielsen-Bohlman L, Panzer AM, Kindig DA. Health Literacy: A Prescription to End Confusion. The National Academies Press; Washington, DC: 2004. [PubMed] [Google Scholar]
- 5.Berkman ND, DeWalt DA, Pignone MP, et al. Evidence Report/Technology Assessment no. 87. Agency for Healthcare Research and Quality; AHRQ publication 04-E007-2; Rockville, MD: 2004. Literacy and Health Outcomes. [Google Scholar]
- 6.Hahn EA, Cella D. Health outcomes assessment in vulnerable populations: measurement challenges and recommendations. Arch Phys Med Rehabil. 2003;84(suppl 2):S35–S42. doi: 10.1053/apmr.2003.50245. [12692770] [DOI] [PubMed] [Google Scholar]
- 7.Baker DW, Gazmararian JA, Williams MV, et al. Functional health literacy and the risk of hospital admission among Medicare managed care enrollees. Am J Public Health. 2002;92:1278–1283. doi: 10.2105/ajph.92.8.1278. [12144984] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kim SP, Knight SJ, Tomori C, et al. Health literacy and shared decision making for prostate cancer patients with low socioeconomic status. Cancer Invest. 2001;19:684–691. doi: 10.1081/cnv-100106143. [11577809] [DOI] [PubMed] [Google Scholar]
- 9.Scott TL, Gazmararian JA, Williams MV, Baker DW. Health literacy and preventive health care use among Medicare enrollees in a managed care organization. Med Care. 2002;40:395–404. doi: 10.1097/00005650-200205000-00005. [11961474] [DOI] [PubMed] [Google Scholar]
- 10.Howard DH, Gazmararian J, Parker RM. The impact of low health literacy on the medical costs of Medicare managed care enrollees. Am J Med. 2005;118:371–377. doi: 10.1016/j.amjmed.2005.01.010. [15808134] [DOI] [PubMed] [Google Scholar]
- 11.Baker DW. The meaning and the measure of health literacy. J Gen Intern Med. 2006;21:878–883. doi: 10.1111/j.1525-1497.2006.00540.x. [16881951] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Westin SN, Bustillos D, Gano JB, et al. Social factors affecting treatment of cervical cancer: ethical issues and policy implications. Obstet Gynecol. 2008;111:747–751. doi: 10.1097/AOG.0b013e318165f1a9. [18310380] [DOI] [PubMed] [Google Scholar]
- 13.Foltz A, Sullivan J. Get real: clinical testing of patients’ reading abilities. Cancer Nurs. 1998;21:162–166. doi: 10.1097/00002820-199806000-00002. [9615506] [DOI] [PubMed] [Google Scholar]
- 14.Jubelirer SJ, Linton JC, Magnetti SM. Reading versus comprehension: implications for patient education and consent in an outpatient oncology clinic. J Cancer Educ. 1994;9:26–29. doi: 10.1080/08858199409528261. [DOI] [PubMed] [Google Scholar]
- 15.Davis TC, Long SW, Jackson RH, et al. Rapid estimate of adult literacy in medicine: a shortened screening instrument. Fam Med. 1993;25:391–395. [8349060] [PubMed] [Google Scholar]
- 16.Parker RM, Baker DW, Williams MV, Nurss JR. The test of functional health literacy in adults: a new instrument for measuring patients’ literacy skills. J Gen Intern Med. 1995;10:537–541. doi: 10.1007/BF02640361. [8576769] [DOI] [PubMed] [Google Scholar]
- 17.Baker DW, Williams MV, Parker RM, Gazmararian JA, Nurss J. Development of a brief test to measure functional health literacy. Patient Educ Couns. 1999;38:33–42. doi: 10.1016/s0738-3991(98)00116-5. [14528569] [DOI] [PubMed] [Google Scholar]
- 18.Yost KJ, Webster K, Baker DW, Choi SW, Bode RK, Hahn EA. Bilingual health literacy assessment using the Talking Touchscreen/la Pantalla Parlanchina: development and pilot testing. Patient Educ Couns. 2009;75:295–301. doi: 10.1016/j.pec.2009.02.020. [19386462] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hahn EA, Cella D, Dobrez DG, et al. Quality of life assessment for low literacy Latinos: a new multimedia program for self-administration. J Oncol Manag. 2003;12:9–12. [14619989] [PubMed] [Google Scholar]
- 20.Hahn EA, Cella D, Dobrez D, et al. The Talking Touchscreen: a new approach to outcomes assessment in low literacy. Psychooncology. 2004;13:86–95. doi: 10.1002/pon.719. [14872527] [DOI] [PubMed] [Google Scholar]
- 21.Rudd RE, Renzulli D, Pereira A, Daltroy L. Literacy demands in health care settings: the patient perspective. In: Schwartzberg JG, VanGeest J, Wang CC, editors. Understanding Health Literacy: Implications for Medicine and Public Health. American Medical Association; Chicago, IL: 2005. pp. 69–84. [Google Scholar]
- 22.Plain Language Action and Information Network (PLAIN) [March 8, 2010];Improving communication from the Federal Government to the Public. www.plainlanguage.gov/.
- 23.Centers for Disease Control and Prevention [March 15, 2010];Scientific and technical information: simply put. 1999 www.cdc.gov/DHDSP/cdcynergy_training/Content/activeinformation/resources/simpput.pdf.
- 24.Doak CC, Doak LG, Root JH. Teaching Patients with Low Literacy Skills. J.B. Lippincott; Philadelphia, PA: 1996. [Google Scholar]
- 25.National Cancer Institute [March 8, 2010];Pink Book–Making Health Communications Programs Work. 1989 www.cancer.gov/pinkbook.
- 26.Paasche-Orlow MK. The challenges of informed consent for low-literate populations. In: Schwartzberg JG, VanGeest J, Wang CC, editors. Understanding Health Literacy: Implications for Medicine and Public Health. American Medical Association; Chicago, IL: 2005. pp. 119–140. [Google Scholar]
- 27.Coyne CA, Xu R, Raich P, et al. Randomized, controlled trial of an easy-to-read informed consent statement for clinical trial participation: a study of the Eastern Cooperative Oncology Group. J Clin Oncol. 2003;21:836–842. doi: 10.1200/JCO.2003.07.022. [12610182] [DOI] [PubMed] [Google Scholar]
- 28.Sudore RL, Landefeld CS, Barnes DE, et al. An advance directive redesigned to meet the literacy level of most adults: a randomized trial. Patient Educ Couns. 2007;69:165–195. doi: 10.1016/j.pec.2007.08.015. [17942272] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Brown RF, Butow PN, Dunn SM, Tattersall MH. Promoting patient participation and shortening cancer consultations: a randomised trial. Br J Cancer. 2001;85:1273–1279. doi: 10.1054/bjoc.2001.2073. [11720460] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Surgeon General.. Proceedings of the Surgeon General's 2006 Workshop on Improving Health Literacy.; 2006; [March 8, 2010]. www.surgeongeneral.gov/topics/healthliteracy/toc.html. [Google Scholar]
- 31.US Department of Health and Human Services [March 8, 2010];Usability Basics. http://www.usability.gov/basics/index.html.
- 32.US Department of Health and Human Services, Office of Disease Prevention and Health Promotion [March 8, 2010];Quick guide to health literacy. 2006 www.health.gov/communication/literacy/quick-guide/.
- 33.The Joint Commission. [March 15, 2010];What did the doctor say? Improving health literacy to protect patient safety. 2007 www.jointcommission.org/newsroom/presskits/health_literacy.