We report two cases of Valsalva retinopathy that have developed during the last trimester of pregnancy with spontaneous resolution and improvement of visual acuity.
Case 1
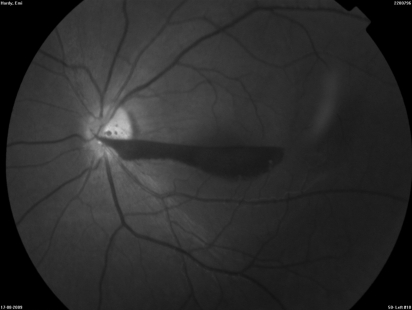
A 26-year-old Caucasian woman at 37 weeks gestation presented to the eye casualty with a sudden history of reduced vision and floaters in the left eye following an episode of sneezing. Her visual acuity was 6/6 and 6/60 in her right and left eyes, respectively. Anterior segment examination was unremarkable. Pupil reactions were normal. Fundus examination of the right eye was normal. Fundus examination of the left eye showed a premacular and vitreous haemorrhage (Figure 1). The patient was reviewed 2 weeks after she had a normal vaginal delivery and her vision had spontaneously improved to 6/6 in the left eye with near-total resolution of the retinal and vitreous haemorrhage.
Figure 1.
Color fundus photograph of the left eye showing a preretinal and subhyaloid haemorrhage
Case 2
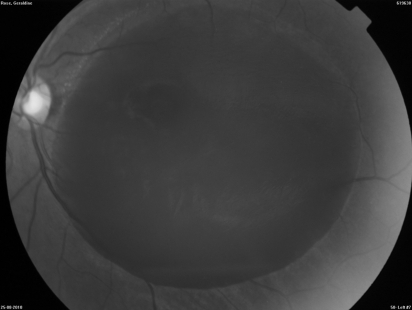
A 34-year-old Afro-Caribbean woman at 37 weeks gestation presented to eye casualty because of sudden blurring of vision in the left eye following an episode of vomiting. Her visual acuity was 6/6 and counting fingers in the right and left eyes, respectively. Anterior segment examination was unremarkable. Fundus examination of the right eye was normal and in the left showed a premacular (subhyaloid) haemorrhage (Figure 2). Her blood pressure, full blood count, coagulation profile, fasting blood sugar, sickle cell tests were all normal. The patient was managed conservatively. The patient had an elective Caesarian section at 38 weeks. At 5-month follow-up, her corrected visual acuity improved to 6/6 with complete resolution of the subhyaloid haemorrhage.
Figure 2.
Color fundus photograph of the left eye showing a dense premacular subhyaloid haemorrhage
Discussion
Valsalva retinopathy is a unilateral or bilateral condition that occurs when increased intra-thoracic or intra-abdominal pressure transmitted to the eye causes a sharp rise in the intraocular venous pressure and rupture of superficial retinal capillaries. Patients usually give a history of sudden visual loss following a bout of heaving lifting, straining, coughing or vomiting.1
Pregnancy is known to exert several hormonal, immunological and hematologic changes that increase the risk of haemorrhage and valsalva retinopathy. Moreover, the enlarging uterus causes elevation of intra-abdominal pressure and compresses the veins leading to increase in the intravenous pressure which increases the risk further.2
Valsalva maneuvers typically result in superficial retinal haemorrhages (sub-internal limiting membrane; subhyaloid) with a predilection for the macula, but subretinal, retinal and vitreous haemorrhages have been reported.
The prognosis is variable; however complete visual recovery over several months is possible. Some patients may develop a poor visual outcome due to the presumed toxic effects of a dense premacular haemorrhage on the retinal pigment epithelium and/or epiretinal membrane formation. Appropriate investigations to rule out known causes of retinal and vitreal haemorhages should be done.2
Different techniques have been employed to treat premacular haemorrhage. Several case series have demonstrated the feasibility of Nd-YAG laser to puncture the posterior aspect of the vitreous thereby allowing drainage of premacular haemorrhage into the vitreous cavity. This may allow rapid restoration of vision and reduce the risk of visual loss associated with longstanding premacular haemorrhages,3,4 however there is a risk of photomechanical retinal injury. Others have suggested early YAG laser treatment to achieve maximum benefit and allow complete drainage of the haemorrhage.5 Vitrectomy surgery has also been used with success.6 We present two cases in whom a conservative approach was adopted with a good outcome. The current literature lacks useful data to address the safety to YAG laser or surgical interventions to the fetus and the ideal timing for any proposed intervention. There is also no general agreement on the optimum obstetric and anaesthetic management of such cases. Our first patient had a normal vaginal delivery while the second patient delivered by Caesarean section, however there is no evidence that Caesarean section is necessary or that a spontaneous vaginal delivery may increase the risk of recurrent haemorrhage. Furthermore, general anaesthesia may cause a re-bleed due to vasodilation induced by hypoxia and hypercarpea, thereby increasing the retinal venous pressure.7 Extubation may lead to significant rises in venous pressure secondary to coughing. Epidural anaesthesia has been also associated with retinal haemorrhage due to an increase in the cerebrospinal fluid pressure within the epidural space which may lead to elevated retinal venous pressure and subsequent haemorrhage.7
In summary, we report two patients with Valsalva retinopathy during pregnancy managed conservatively with a good outcome. Close discussion between the treating ophthalmologist and obstetrician is necessary to discuss the treatment options and the possible risks with each method of delivery and anaesthesia.
DECLARATIONS
Competing interests
None declared
Funding
None
Ethical approval
Written consent to publication has been obtained from the patients
Guarantor
HZ
Contributorship
HED conceived and designed the idea, acquired the data and drafted the manuscript; AS drafted and critically revised the manuscript; CJM critically revised the manuscript; HJZ critically revised the manuscript and supervised the study
Acknowledgements
None
Reviewer
Deb Sahu
References
- 1.Chapman-Davies A, Lazarevic A Valsalva retinopathy. Clin Exp Optom 2002;85:42–5 [DOI] [PubMed] [Google Scholar]
- 2.Al-Mujaini AS, Montana CC Valsalva retinopathy in pregnancy. J Med Case Reports 2008,2:101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rennie CA, Newman DK, Snead MP, Flanagan DW Nd:YAG laser treatment for premacular subhyaloid hemorrhage. Eye (Lond) 2001;15:519–24 [DOI] [PubMed] [Google Scholar]
- 4.Ulbig MW, Mangouritsas G, Rothbacher HH, Hamilton AM, McHugh JD Long term results after drainage of premacular subhyaloid hemorrhage into the vitreous with pulsed Nd:YAG laser. Arch Ophthalmol 1988;116:1465–9 [DOI] [PubMed] [Google Scholar]
- 5.Cheung CMG, Benson MT Post-chemotherapy premacular subhyaloid hemorrhage. Eye (Lond) 2003;17:97–9 [DOI] [PubMed] [Google Scholar]
- 6.Conway MD, Peyman GA, Recaseus M Intravitreal tPa and SF6 promote clearing of premacular subhyaloid hemorrhages in shaken and battered baby syndrome. Ophthalmic Surg Lasers 1999;30:435–41 [PubMed] [Google Scholar]
- 7.Chidley KE, Law R, Vanner G Caesarean section following a recent retinal hemorrhage. Anaesthesia 1998;53:477–85 [DOI] [PubMed] [Google Scholar]