In this case report, we describe a primary osteoblastic intradiploic meningioma with a clinical and radiological appearance simulating osteoma or fibrous dysplasia.
Introduction
This paper discusses how best to manage a patient with primary intraosseous meningioma, with particular consideration given to the merits of cranioplasty and dural biopsy. Rarely, meningiomas may arise from arachnoid cells within the diploe of the skull. The latter are usually destroyed in the process and there is increased vascularity of the tumour. Bony destruction results in the tumour lying subcutaneously with or without an intracranial component.1 These patients usually present with symptoms and signs of a painless gradually expanding mass. If associated with a significant intracranial component, they may present with headache, seizures and focal neurological signs, such as limb weakness or dysphasia depending on the location of the lesion. Under the microscope, the characteristic appearance is that of a spindle cell tumour composed of lobules and whorls of bland cells often with scattered psammoma bodies; there are, however, rarer subtypes showing different morphological features. Meningiomas account for 15–20% of primary intracranial neoplasms with the incidence peaking in the fourth and fifth decades and a female:male ratio of almost 2:1.2
Osteomas of the skull typically present as a slowly growing, expansile mass. Often this is a painless process. However, there may be headaches or localized pain over the swelling. The pain is classically worse at night and relieved by administration of salicylates.3 They are the most common primary tumours of the calvaria. The outer table is the most frequently involved with a well-demarcated homogenous and dense projection. Unlike in meningiomas, the diploe are preserved and the vascular channels not increased. Osteomas present as hot lesions on nuclear bone scans.4 Histologically, they are composed of dense, mature and predominantly lamellar bone.
Fibrous dysplasia involving the skull high on the calvaria is of the cystic type with a higher incidence below 30 years of age. It may present as an incidental finding or with local pain, swelling and cranial nerve involvement if it affects the cranial nerve foramina. Widening of the diploe with thinning of the outer and inner tables and a ground glass appearance on X-ray is typical but not characteristic. Microscopically, the typical appearance is of narrow, curved and misshaped bony trabeculae, so called ‘Chinese letters’, which are interspersed with fibrous tissue of variable cellularity.
Other pathologies causing focal or localized increase in bone density include the en-plaque variety of meningiomas which often involve the sphenoid bone and are associated with hyperostosis. Osteoblastic metastases such as those originating from prostatic carcinoma are also recognized. Rarer causes include the early stages of Paget's disease, hyperostosis frontalis interna, osteosarcomas and ossifying fibromas.4
The symptoms, signs and radiological appearances may be of little help in distinguishing one diagnosis from another. Radiologically, intraosseous meningiomas, osteomas and fibrous dysplasia may have similar appearances on CT scan.5 Primary intrasseous meningiomas are heterogenous in appearance. Osteomas appear as hyperdense, smooth and well-demarcated lesions. Fibrous dysplasia may demonstrate a ground glass appearance with thinning of the inner and outer tables of the skull.6
Case report
A 64-year-old woman presented to her general practitioner (GP) with a three-year history of a right frontal skull swelling. Over the past year this swelling had increased in size. The patient was referred to the neurosurgery clinic where examination revealed a sessile non-tender mass (approximately 4.3 x 1.6 cm). The overlying skin was intact with normal hair growth. There was no headache and there were no focal neurological signs or symptoms.
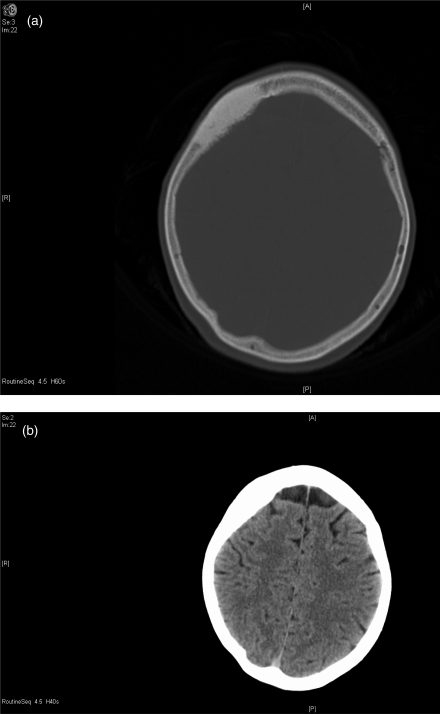
The initial skull X-ray was suggestive of an osteoma. Bone scintigraphy was normal. A CT scan of the head showed a sclerotic thickened area of the right frontal bone with no significant mass effect on the underlying cerebrum (Figure 1). No brain or meningeal enhancement was noted on the scans. The findings were suggestive of an osteoma, with fibrous dysplasia as another possibility. Review of the scans by a second radiologist confirmed an area of sclerosis and non-destructive expansion of the right frontal bone. However, this was thought to represent an intraosseous meningioma.
Figure 1.
CT head from patient (a) showing lesion and (b) showing no soft tissue involvement
The patient was treated surgically and underwent a small skin incision overlying the lesion. The latter was chiselled off and sent for pathological examination in order to obtain a tissue diagnosis. The contour of the skull was restored.
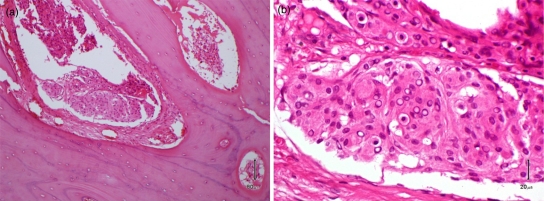
Histologically the sample contained fragments of mature bone, whereby some of the bone marrow spaces were replaced by a spindle cell tumour forming lobules and whorls (Figure 2). It was composed of cells with oval nuclei, some nuclear pseudoinclusions, eosiniophilic cytoplasm and indistinct cytoplasmic borders. Mitotic figures were not present. The features were consistent with an intraosseous meningioma of meningothelial subtype (WHO Grade I).
Figure 2.
Histology of the lesion with bony spaces containing lobules and whorls of spindle cells (a) showing round/oval nuclei with nuclear pseudoinclusions typical of meningothelial cells and best appreciated at higher magnification (b)
The patient was subsequently readmitted and underwent a total excision of the tumour and cranioplasty. The involved right frontal bone was excised and replaced with a titanium mesh.
Discussion
Given the uncertainty of diagnosis in this case, a partial resection of the lesion was carried out in the first place in order to obtain a tissue diagnosis and simultaneously achieve a good cosmetic result by remodelling the contour of the involved area of skull. The alternative option involving total excision of the involved bone and cranioplasty at first presentation carries a slightly increased risk of bleeding, infection and seizures. On the other hand, such an approach would have avoided a second procedure.
It is clear from this case that excision followed by cranioplasty is necessary when a primary intradiploic tumour is suspected. Furthermore, given the existence of cases where there has been dural involvement subsequent to initial treatment, dural biopsy for histological analysis should be considered at the time of the initial treatment.7 Given the absence of dural involvement on radiology in this case, a biopsy was not taken; however, this would be important in cases of uncertain aetiology involving convexity regions. A surgical plan for total excision including dural biopsy would need to be considered from the start.
DECLARATIONS
Competing interests
None declared
Funding
None
Ethical approval
Written informed consent to publication has been obtained from the patient or next of kin
Guarantor
RAI
Contributorship
SB, RAI and MH wrote the article and contributed equally to the paper; SB, RAI, MH and MG revised drafts of the paper; MH provided pathological slides
Acknowledgements
The authors thank Richard Stacey, consultant neurosurgeon, for his involvement in caring for the patient
Reviewer
Amad Khan
References
- 1.Kulali A, Ilcayto R, Rahmanali O Primary calvarial ectopic meningiomas. Neurochirurgia (Stuttg) 1991;34:174–7 [DOI] [PubMed] [Google Scholar]
- 2.Lang FF, Macdonald OK, Fuller GN, DeMonte F Primary extradural meningiomas: A report on nine cases and review of the CT-era literature. J Neurosurg 2000;93:940–50 [DOI] [PubMed] [Google Scholar]
- 3.Eppley BL, Kim W, Sadove AM Large osteomas of the cranial vault. J Craniofac Surg 2003;14:97. [DOI] [PubMed] [Google Scholar]
- 4.Greenberg MS Handbook of Neurosurgery. Seventh edn Stuttgart: Georg Thieme Verlag KG, 2010 [Google Scholar]
- 5.Arana E, Marti-Bonmati L CT and MR imaging of focal calvarial lesions. Am J Roentgenol 1999;172:1683. [DOI] [PubMed] [Google Scholar]
- 6.Changhong L, Naiyin C, Yuehuan G, Lianzhong Z Primary intraosseous meningiomas of the skull. Clin Radiol 1997;52:546–9 [DOI] [PubMed] [Google Scholar]
- 7.Bassiouni H, Asgari S, Hübschen U, König HJ, Stolke D Dural involvement in primary extradural meningiomas of the cranial vault. J Neurosurg 2006;105:51–9 [DOI] [PubMed] [Google Scholar]