Abstract
A roundtable to discuss the measurement of vitamin B-12 (cobalamin) status biomarkers in NHANES took place in July 2010. NHANES stopped measuring vitamin B-12–related biomarkers after 2006. The roundtable reviewed 3 biomarkers of vitamin B-12 status used in past NHANES—serum vitamin B-12, methylmalonic acid (MMA), and total homocysteine (tHcy)—and discussed the potential utility of measuring holotranscobalamin (holoTC) for future NHANES. The roundtable focused on public health considerations and the quality of the measurement procedures and reference methods and materials that past NHANES used or that are available for future NHANES. Roundtable members supported reinstating vitamin B-12 status measures in NHANES. They noted evolving concerns and uncertainties regarding whether subclinical (mild, asymptomatic) vitamin B-12 deficiency is a public health concern. They identified the need for evidence from clinical trials to address causal relations between subclinical vitamin B-12 deficiency and adverse health outcomes as well as appropriate cutoffs for interpreting vitamin B-12–related biomarkers. They agreed that problems with sensitivity and specificity of individual biomarkers underscore the need for including at least one biomarker of circulating vitamin B-12 (serum vitamin B-12 or holoTC) and one functional biomarker (MMA or tHcy) in NHANES. The inclusion of both serum vitamin B-12 and plasma MMA, which have been associated with cognitive dysfunction and anemia in NHANES and in other population-based studies, was preferable to provide continuity with past NHANES. Reliable measurement procedures are available, and National Institute of Standards and Technology reference materials are available or in development for serum vitamin B-12 and MMA.
INTRODUCTION
The NHANES are a valuable source of data on the nutritional and health status of the US population. The surveys require highly accurate measurement procedures to ensure that their prevalence estimates are comparable with commonly used cutoffs of nutrient adequacy and safety, and that trends in these estimates over time are attributable to real changes in nutritional status.
Currently, NHANES does not measure serum vitamin B-12 or any other vitamin B-12–related biomarkers. However, NHANES II (1976–1980), the second half of NHANES III (1991–1994), and NHANES 1999–2006 measured serum vitamin B-12 concentrations. Furthermore, NHANES III (1988–1994) and NHANES 1999–2004 measured methylmalonic acid (MMA) concentrations, and NHANES III (1991–1994) and NHANES 1999–2006 measured total homocysteine (tHcy) concentrations.
The National Center for Health Statistics of the Centers for Disease Control and Prevention and the Office of Dietary Supplements of the National Institutes of Health convened a roundtable panel on July 15–16, 2010, in Rockville, MD, to review the measurement of biomarkers of folate and vitamin B-12 status in NHANES. In this article, we summarize the roundtable's discussion, which focused on the following: 1) public health considerations for including vitamin B-12–related biomarkers in NHANES and 2) the quality of the vitamin B-12–related measurement procedures and reference methods and materials that NHANES uses or that are available for future NHANES. Other articles in this supplement issue summarize general background information on biomarker measurement and use issues and the roundtable's review of folate status biomarkers (1–3). In an introductory article, we describe how the individual articles in this supplement fit within the overall roundtable process (4). We also describe the relevance of the roundtable review and dialogue to clinical and research settings outside the NHANES context.
THE ROUNDTABLE
The roundtable panel consisted of 23 experts in folate and vitamin B-12 assessment, clinical laboratory science, and biostatistics and 10 scientists from US government agencies that generate or use NHANES data and develop reference methods and materials for these measures.
The roundtable reviewed 3 biomarkers of vitamin B-12 status used in NHANES: vitamin B-12, MMA, and tHcy. This article, in comparison to the folate-related biomarkers summary (3), includes the roundtable's discussions of tHcy because vitamin B-12 status is the predominant nutrient determinant of high tHcy concentrations among US population groups (5–7). The roundtable also considered holotranscobalamin's (holoTC's) possible utility as an indicator of vitamin B-12 status for future NHANES (8, 9).
The roundtable reviewed vitamin B-12–related public health and measurement quality issues in the context of the NHANES mission and capabilities. The experts did not consider broader research and clinical application issues for these biomarkers or differences in the measurement procedures that research, clinical, and commercial laboratories use. The roundtable identified and discussed the scientific issues involved in deciding whether to include vitamin B-12–related biomarkers in future NHANES. For ease of use, we used the more common terminology of “vitamin B-12” in place of the more precise terminology of “cobalamin” (9). When we used serum vitamin B-12 data in this article, we converted the values to pmol/L (1.0 pg/mL or ng/L = 0.7378 pmol/L). For plasma MMA, we converted the values to nmol/L (1.0 ng/mL or μg/L = 8.468 nmol/L).
MONITORING OF VITAMIN B-12 STATUS IN NHANES
The roundtable focused on 2 key vitamin B-12–related monitoring issues: 1) the public health need for assessing vitamin B-12 status and 2) the usefulness of several biomarkers in conducting these assessments. Ralph Carmel outlined key issues for the roundtable to consider (9). Regan Bailey provided data on vitamin B-12 status assessments for adults in NHANES.
Public health need for monitoring of vitamin B-12 status
The roundtable considered whether the primary purpose of monitoring the US population's vitamin B-12 status is to determine the prevalence of the uncommon and serious clinical vitamin B-12 deficiency characterized by megaloblastic anemia and/or neurocognitive dysfunction; ≈94% of these cases arise from pernicious anemia. Alternatively, the primary purpose could be to monitor the more common subclinical (mild, asymptomatic) vitamin B-12 deficiency, defined by abnormal concentrations of vitamin B-12–related biomarkers [also referred to as SCCD or subclinical cobalamin deficiency (9)]. Approximately 1–2% of the elderly US population has clinical vitamin B-12 deficiency, and ≈10–20% has subclinical deficiency (10).
Because NHANES is not well suited for monitoring rare medical conditions such as pernicious anemia, the roundtable found the question posed by Carmel as to whether monitoring the more common subclinical deficiency has public health merit (9) to be a helpful anchor point for their overall dialogue. The common assumption that detecting subclinical deficiency early is important to enable public health interventions that prevent its progression to clinical deficiency lacks confirmatory evidence (9). Subclinical deficiency often arises from different causes (eg, malabsorption of food-bound cobalamin or unidentified causes) than does clinical deficiency (eg, absence of intrinsic factor due to pernicious anemia) (9, 10). Moreover, limited evidence suggests that many individuals with subclinical deficiency, even without treatment, spontaneously regain normal vitamin B-12 status or experience no further deterioration after several years, raising questions about the public health concerns with subclinical deficiency (9–11).
Subclinical vitamin B-12 deficiency per se may adversely affect cognitive or neurologic function. Results from some, but not all, observational studies show associations between vitamin B-12 deficiency and cognitive impairment (12–17). The roundtable noted, however, that no clinical trials have confirmed a causal relation between subclinical vitamin B-12 deficiency and adverse outcomes. Therefore, the roundtable agreed that the public health implications of subclinical vitamin B-12 deficiency are uncertain, although the observational evidence on adverse effects is of concern and warrants further evaluation.
Biomarkers of vitamin B-12 status
The roundtable considered the usefulness of available biomarkers for assessing vitamin B-12 status in NHANES. Biomarker usefulness depends on the status component being measured and whether (and, if so, how) factors unrelated to vitamin B-12 status affect these biomarkers. The roundtable also discussed whether commonly used deficiency cutoffs are meaningful for the NHANES sample (the general US population) and for the NHANES measurement procedures.
Currently available biomarkers can be categorized as those that directly measure the vitamin B-12 in blood and those that measure metabolites that accumulate with inadequate amounts of vitamin B-12 (8–10, 18). Serum vitamin B-12 and holoTC measure circulating vitamin B-12 concentrations. These biomarkers therefore reflect the broad vitamin B-12 status range from high risk of severe deficiency to adequacy. MMA and tHcy, which are functional (metabolic) measures of vitamin B-12 status, accumulate when concentrations of vitamin B-12 are inadequate; tHcy also accumulates with inadequate amounts of folate and, to a lesser degree, riboflavin and vitamin B-6. These functional measures are useful for identifying subclinical vitamin B-12 status and reflect early changes in vitamin B-12 status. Information from both types of biomarkers can yield a more accurate assessment of vitamin B-12 status than information from only one vitamin B-12 status category (9).
Factors unrelated to vitamin B-12 status affect all 4 biomarkers (8–10, 18–20). Impaired renal function alters MMA and tHcy and, to a lesser extent, holoTC and serum vitamin B-12 concentrations. Other factors, such as individual genetic variation, disease conditions, prescription and other drug use, and pregnancy can also affect the biomarkers. Measurement procedure errors and other technological problems produce spuriously high or low biomarker concentrations (9). These factors adversely affect the biomarkers’ sensitivity and specificity and result in false-positive or false-negative classifications of vitamin B-12 deficiency.
These classification errors are particularly important for surveys such as NHANES that cannot conduct the follow-up diagnostic testing required for vitamin B-12 deficiency diagnosis and treatment (9). For example, high MMA and tHcy concentrations occur across all serum vitamin B-12 concentrations, although they are most prevalent in people with the lowest vitamin B-12 concentrations (9). Clinical data show that ≈2.5–5.2% of patients with diagnosed vitamin B-12 deficiency have serum vitamin B-12 concentrations above a commonly used cutoff for low values (148 pmol/L), and an even higher proportion of persons with abnormal MMA or tHcy concentrations have serum vitamin B-12 concentrations >148 pmol/L (9). Approximately 20% of persons with low serum vitamin B-12 concentrations have neither clinical nor metabolic signs of vitamin B-12 deficiency. The roundtable agreed that because of problems with these biomarkers’ sensitivity and specificity, measuring a circulating biomarker (vitamin B-12 or holoTC) and a functional biomarker (MMA or tHcy) concurrently is preferable to measuring only one biomarker in NHANES.
The roundtable also reviewed the relevance of common cutoffs for the NHANES population. The vitamin B-12 cutoffs that scientists and clinicians use generally are consistent with 2 or 3 SDs from a reference range's mean. A cutoff value consistent with 2 SDs is ≈200 pmol/L, and a value of 148 pmol/L is consistent with 3 SDs (9, 18). A cutoff of 148 pmol/L misses 3–5% of patients with clinical deficiency, whereas ≈200 pmol/L identifies all patients but produces more false-positive results. Systematic bias and spurious results affected some measurement procedures used in the past to derive reference ranges (9). The cutoff used affects NHANES prevalence estimates. Using cutoffs similar to those used in the published literature, Regan Bailey (personal communication, 2011) found a prevalence (least-squared percentage ± SE) of 2.8 ± 0.2% for serum vitamin B-12 concentrations <148 pmol/L, 10.5 ± 0.4% for concentrations <198 pmol/L, and 25.6 ± 0.6% at <258 pmol/L in an NHANES sample of people aged ≥60 y with impaired but controlled renal function.
MMA cutoffs also range considerably, from 210 to 480 nmol/L (9). Researchers have based MMA cutoff values on an approximation of the inflection point at which MMA concentrations start to increase with decreasing serum vitamin B-12 concentrations or on a percentile of a population-based reference range, or on fully cobalamin-replete subjects (12, 18, 21). The cutoff value used affects prevalence estimates. In an NHANES sample of adults aged ≥60 y in whom impaired renal function was controlled, Regan Bailey found that a cutoff >376 nmol/L resulted in a prevalence of 2.4%, whereas a cutoff >271 nmol/L produced a prevalence of 5.9% (RL Bailey, personal communication, 2011).
The roundtable discussed the urgent need to base cutoffs for biomarker concentrations on adverse outcome occurrences. The need for such cutoffs is particularly critical for subclinical vitamin B-12 deficiency, which is the predominant type of vitamin B-12 deficiency in NHANES populations because it is asymptomatic and research has not confirmed a causal relation between subclinical deficiency and adverse health outcomes. Validation of cutoff values requires clinical trials and accurate and reliable measurement procedures. Cross-sectional studies, such as NHANES, and other observational studies cannot validate cutoffs, although these studies can help generate hypotheses and examine relations between variables.
MEASURES OF VITAMIN B-12ndashRELATED BIOMARKERS IN NHANES
The roundtable reviewed the quality and appropriateness of NHANES procedures to measure vitamin B-12–related biomarkers. Except for 2 special postsurvey projects at Tufts University that used surplus sera to measure MMA and tHcy in the second phase of NHANES III (1991–1994) (22, 23), the Division of Laboratory Science at the National Center for Environmental Health (NCEH) of the Centers for Disease Control and Prevention measured serum vitamin B-12 and plasma MMA and tHcy in NHANES. Christine Pfeiffer reviewed the NCEH laboratory procedures and results for the roundtable.
Measurement of serum vitamin B-12 in NHANES
NHANES used the Bio-Rad Quantaphase II radioimmunoassay (RIA) kit for (Bio-Rad Laboratories, Hercules, CA) all serum vitamin B-12 measures except for the 1976–80 survey, which used the Quantaphase I kit (Table 1) (24–28). In 2007, the manufacturer discontinued the Bio-Rad RIA. The loss of this assay kit and the finding that serum vitamin B-12 concentrations collected from NHANES III (1991–1994) to NHANES 2006 had not changed appreciably (1) resulted in a decision to drop measures of vitamin B-12 status after NHANES 2006.
TABLE 1.
Vitamin B-12 biomarker measurement in NHANES1
| Survey | Measurement procedure | Matrix | Laboratory | Population age |
| 1974–1975 | — | — | — | — |
| 1976–1980 | Bio-Rad QP I | Serum | NCEH | 6 mo–74 y, subset |
| 1988–1991 | — | — | — | — |
| 1991–1994 | Bio-Rad QP II | Serum | NCEH | ≥4 y |
| 1999–2000 | Bio-Rad QP II | Serum | NCEH | ≥3 y |
| 2001–2002 | Bio-Rad QP II | Serum | NCEH | ≥3 y |
| 2003–2004 | Bio-Rad QP II | Serum | NCEH | ≥1 y |
| 2005–2006 | Bio-Rad QP II | Serum | NCEH | ≥1 y |
| 2007–2008 | — | — | — | — |
| 2009–2010 | — | — | — | — |
QP, Quantaphase (Bio-Rad Laboratories, Hercules, CA); NCEH, National Center for Environmental Health, Centers for Disease Control and Prevention.
With the Quantaphase II kit, the NCEH obtained long-term CVs (NHANES 1999–2004) of 3–6% for concentrations of ≈280–1200 pmol/L (29). Quality-control (QC) pools were stable and reproducible across all surveys. For reference material 81/563 from the National Institute for Biological Standards and Control (NIBSC; http://www.nibsc.ac.uk/products/biological_reference_materials.aspx), the NCEH obtained a mean (±SD) value of 234 ± 14 pmol (n = 27) from 1994 to 2006 compared with an NIBSC-certified concentration of 236 pmol/ampule. Over several years in the College of American Pathologists (http://www.cap.org/apps/cap.portal) proficiency testing program, the NCEH results were ≈20% higher than the College of American Pathologists all-laboratory trimmed mean; the Bio-Rad RIA had no peer group using this measurement procedure with which to directly compare results.
Because the NCEH anticipated that NHANES might consider reinstating vitamin B-12 measures at a later date, it evaluated the Roche Elecsys 170 chemiluminescent measurement procedure (Roche, Basel, Switzerland). The result was 373 pmol/ampule for the NIBSC 03/178 reference material, with an assigned reference value of 354 pmol/ampule. When the NCEH fortified a serum pool with this reference material, complete recovery resulted (103%). The NCEH used its Roche E-170 procedure to characterize 3 levels of National Institute of Standards and Technology (NIST) standard reference material (SRM) 3951 (30), which is under development. The NIST will use results from higher-order reference measurement procedures to assign this SRM's target values. NCEH-measured mean (±SD) vitamin B-12 concentrations were 42.6 ± 5.8 (CV: 13.7%), 114.4 ± 6.0 (CV: 5.3%), and 283.1 ± 7.3 pmol/L (CV: 2.6%) (n = 12) for this reference material. The NCEH obtained within-day CVs (n = 10) of 0.9–2.1% for its low and high (≈175 and 825 pmol/L) QC pools. Between-day CVs over 5 mo (n = 22) were 3.8–6.5% for 5 QC pools with concentrations of ≈200–900 pmol/L. The manufacturer-specified limit of detection for this serum vitamin B-12 measurement procedure was 22 pmol/L.
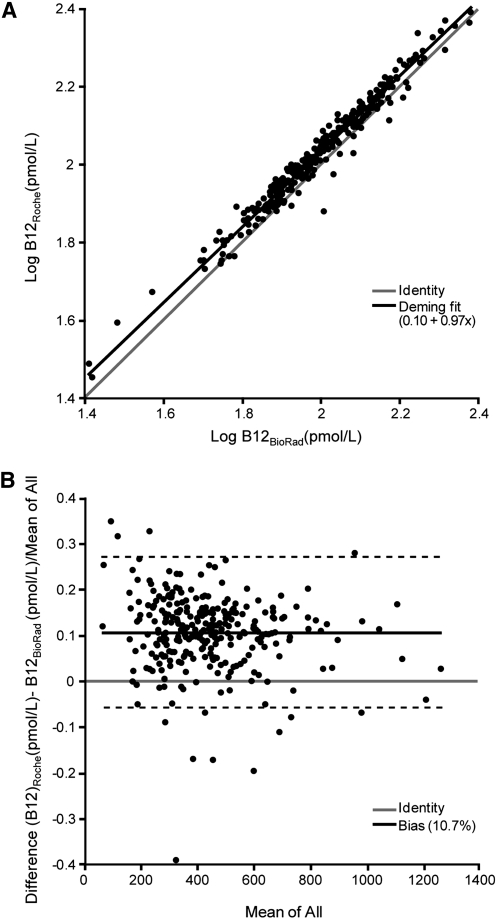
In a crossover study (n = 280), the NCEH reanalyzed NHANES samples it had previously measured with the Bio-Rad Quantaphase II RIA by using the Roche E-170 measurement procedure to determine the procedures’ comparability. The median was 390 pmol/L for the Bio-Rad and 438 pmol/L for the Roche procedure, and the Pearson correlation coefficient was 0.98 over a range of ≈45–1100 pmol/L. A log transformation removed the distribution's skewness with a Deming regression fit of log vitamin B-12Roche = 0.97 × log vitamin B-12Bio-Rad + 0.10 pmol/L and showed a small but significant constant and proportional bias (Figure 1A). The Bland-Altman bias plot showed a mean relative bias of 10.7% for the Roche procedure compared with the Bio-Rad procedure, with 95% limits of agreement from −5.6% to 27% (Figure 1B).
FIGURE 1.
Crossover study (n = 280) comparing serum vitamin B-12 (B12) results using 2 different measurement procedures. A: Scatter plot with Deming regression fit of log-transformed vitamin B-12 concentrations as measured by the Roche E-170 procedure (Roche, Basel, Switzerland). compared with the Bio-Rad Quantaphase II radioimmunoassay (Bio-Rad Laboratories, Hercules, CA). The Deming equation was: log B12Roche = 0.97 × log B12Bio-Rad + 0.10 pmol/L. The SE was 0.012 for the slope and 0.025 for the intercept. B: Bland-Altman difference plot of vitamin B-12 concentrations between the Roche E-170 procedure and the Bio-Rad Quantaphase II radioimmunoassay. Each data point represents the relative difference between the 2 assays as a function of the mean between the 2 assays. The mean relative bias for the Roche procedure compared with the Bio-Rad procedure was 10.7%, and the 95% limits of agreement were from −5.6% to 27%.
Measurement of plasma MMA in NHANES
The NCEH used gas chromatography/mass spectrometry (GC/MS) to measure plasma MMA in NHANES (Table 2) (31–34), resulting in long-term CVs (NHANES 1999–2004) of 3–8% for low QC pools (≈100–500 nmol/L), 2–4% for medium QC pools (1000–2000 nmol/L), and 2.0–3.5% for high QC pools (≈10,000 nmol/L). QC pools were stable and reproducible across all surveys. As a participant in the Danish External Quality Assessment program since 2000, the NCEH's MMA results have consistently been within the acceptance interval that the program calculated from biological variation (±21% of the program mean). The NCEH's results were, on average, 6% lower than the program mean.
TABLE 2.
Methylmalonic acid measurements in NHANES1
| Survey | Measurement procedure | Matrix | Laboratory | Population age |
| 1974–1975 | — | — | — | — |
| 1976–1980 | — | — | — | — |
| 1988–1994 | GC/MS | Surplus serum | Tufts University | 30–39 y, ≥65 y |
| 1999–2000 | GC/MS | Plasma | NCEH | ≥3 y |
| 2001–2002 | GC/MS | Plasma | NCEH | ≥3 y |
| 2003–2004 | GC/MS | Plasma | NCEH | ≥3 y |
| 2005–2006 | — | — | — | — |
| 2007–2008 | — | — | — | — |
| 2009–2010 | — | — | — | — |
GC/MS, gas chromatography/mass spectrometry; Tufts University, Jean Mayer US Department of Agriculture Human Nutrition Research Center on Aging, Boston, MA; NCEH, National Center for Environmental Health, Centers for Disease Control and Prevention.
If NHANES reinstates MMA measures in future surveys, the NCEH could use their GC/MS measurement procedure because the NCEH has maintained proficiency in this procedure despite its absence from recent NHANES. However, the NCEH is considering using a liquid chromatography–mass spectrometry (LC-MS/MS) procedure similar to the one that several laboratories have recently used (35–37). The roundtable encouraged the NCEH to use LC-MS/MS for future analyses.
Measurement of tHcy in NHANES
The measurement procedures, QC data, and survey comparability of tHcy in NHANES are described elsewhere (38–45) and are summarized in Table 3. The NCEH observed long-term (NHANES 1999–2004) CVs of 3–5% for multiple QC pools covering a tHcy concentration range of ≈6–27 μmol/L (45). QC pools were stable and reproducible in all surveys. The NCEH Abbott AxSym (Abbott Diagnostics, Abbott Park, IL) results were within 10% of the NIST SRM 1955 certified values, 9% higher for the low level (≈4 μmol/L), 1% higher for the medium level (≈9 μmol/L), and 6% lower for the high level (≈18 μmol/L). As a participant in the Danish external quality assurance program in 2000–2008, the NCEH consistently obtained tHcy results within the program's acceptance interval on the basis of biological variation (±17% of the program mean). The NCEH's results were, on average, 0.2% higher than the program mean.
TABLE 3.
Total homocysteine measurements in NHANES1
| Survey | Measurement procedure | Matrix | Laboratory | Population age |
| 1974–1975 | — | — | — | — |
| 1976–1980 | — | — | — | — |
| 1988–1991 | — | — | — | — |
| 1991–1994 | HPLC-FD | Surplus serum | Tufts | ≥12 y |
| 1999–2000 | Abbott FPIA IMx | Plasma | NCEH | ≥3 y |
| 2001 | Abbott FPIA IMx | Plasma | NCEH | ≥3 y |
| 2002 | Abbot FPIA AxSYM | Plasma | NCEH | ≥3 y |
| 2003–2004 | Abbott FPIA AxSYM | Plasma | NCEH | ≥3 y |
| 2005–2006 | Abbott FPIA AxSYM | Plasma | NCEH | ≥20 y |
| 2007–2008 | — | — | — | — |
| 2009–2010 | — | — | — | — |
HPLC-FD, HPLC with fluorescence detection; FPIA, fluorescence polarization immunoassay (AxSYM and IMx; Abbott Diagnostics, Abbott Park, IL); NCEH, National Center for Environmental Health, Centers for Disease Control and Prevention; Tufts, Tufts University, Jean Mayer US Department of Agriculture Human Nutrition Research Center on Aging, Boston, MA.
Possible measurement of holoTC in NHANES
Ebba Nexo (8) described several procedures for assessing holoTC, including a new enzyme-linked immunosorbent assay procedure on the Abbott AxSym analyzer platform. This procedure is easier to use than previous ones and can measure holoTC directly without sample pretreatment (46). In a comparison study in Europe, all available methods gave similar values (47). Enzyme-linked immunosorbent assay measurement had a 4–5% imprecision rate and a 5–20 pmol/L method-dependent detection limit.
NIST REFERENCE METHODS AND MATERIALS
The roundtable reviewed the quality and appropriateness of the NIST reference methods and materials for use in NHANES to achieve traceability of NHANES measurements to a higher-order reference method and materials. Karen Phinney discussed the development of reference methods and materials for vitamin B-12, tHcy, and MMA at the NIST.
NIST methods and materials for vitamin B-12 and MMA
Currently, the NIST has no SRM with certified values for vitamin B-12 or MMA, although it provides information values for vitamin B-12 using RIA in SRM 1955 (48). The NIST is developing SRM 3951 (30) for serum vitamin B-12 with target pools of 74 pmol/L (100 pg/mL), 148 pmol/L (200 pg/mL), and 332 pmol/L (450 pg/mL). The 332-pmol/L pool is “normal” serum, whereas the 2 lower pools are a blend of normal and serum stripped of its naturally occurring vitamin B-12.
Unique challenges in developing a higher-order vitamin B-12 measurement procedure include the forms of vitamin B-12 to measure. One challenge is whether converting all forms to cyanocobalamin and measuring this compound to determine total serum vitamin B-12 best meets user needs. Also, do users need to evaluate the different biologically relevant species? Another challenge is the low concentrations that will be encountered in some individuals with low vitamin B-12 status (≈100 pmol/L or less) of serum vitamin B-12. To account for potential analyte losses during sample preparation, a stable-isotope–labeled internal standard should be used, but chemical synthesis of an isotopically labeled form of vitamin B-12 is not currently feasible. A labeled form of vitamin B-12 would be the ideal internal standard because it should behave similarly to the unlabeled endogenous form, including binding to the 2 circulating vitamin B-12 binding proteins (haptocorrin and transcobolamin). Alternative options might be a labeled compound produced by bacteria or partial chemical synthesis incorporating isotopically labeled precursor compounds.
The NIST has not found a good internal standard candidate among other structurally related compounds. On the basis of preliminary work using LC-MS/MS, the NIST has identified some vitamin B-12 species that it could quantify. Remaining challenges include obtaining the needed sensitivity, developing an appropriate quantitation mechanism, and obtaining sufficient precision to certify concentration values in the reference materials. The roundtable suggested developing a valid LC-MS/MS method to measure total cobalamin after converting all species to cyanocobalamin. Characterization of vitamin B-12 species is a long-term goal, but a need exists now for an SRM for total cobalamin.
The NIST is currently developing MMA reference methods and materials. Phinney reported that GC/MS and LC-MS/MS procedures using derivatized or underivatized compounds work well. The NIST is developing new reference materials for SRM 909 (49) and finds that these materials are appropriate for SRM use (MMA concentration of ≈170 nmol/L). The NIST's SRM 1950 (50) materials are also appropriate (MMA of ≈300 nmol/L). However, SRM 3591 (30), which is under development, is not appropriate (MMA of ≈35 nmol/L).
NIST methods and materials for tHcy
NIST SRM 1955 has certified values for mean (±expanded uncertainty) tHcy concentrations of 3.98 ± 0.18 μmol/L, 8.85 ± 0.60 μmol/L, and 17.7 ± 1.1 μmol/L (48, 51–53). Level 2 is a naturally occurring serum material, level 1 is diluted, and level 3 is fortified to achieve target concentrations. In a commutability study with 20 fresh-frozen samples and a limited concentration range, SRM 1955 was commutable across 14 commercial tHcy immuno- and enzymatic assays (54). The Joint Committee for Traceability in Laboratory Medicine database lists the NIST GC-MS and LC-MS/MS methods as reference measurement procedures (55).
ROUNDTABLE DIALOGUE: VITAMIN B-12ndashRELATED BIOMARKERS IN NHANES
The roundtable members were generally satisfied with the measurement and reference material issues and therefore focused their discussion on issues relating to reinstating vitamin B-12 status biomarkers in future NHANES.
Reinstatement of vitamin B-12 biomarkers in NHANES
Overall, the roundtable experts supported reinstating vitamin B-12–related biomarker measurement in future NHANES and discussed possible reasons to justify its inclusion in future NHANES. The roundtable noted that interest in monitoring vitamin B-12 status began with folic acid fortification of cereal grains in the United States in 1996, because this fortification might mask hematologic symptoms of vitamin B-12 deficiency, resulting in diagnosis and treatment delays that would promote the progression of mild vitamin B-12 insufficiency to more clinically severe deficiency. However, before and after fortification, median serum vitamin B-12 concentrations (343–356 pmol/L) and the prevalence of serum vitamin B-12 concentrations <148 pmol/L (2.7–4.8%) did not change appreciably (29). Only 2% of the US population had high MMA concentrations indicating inadequate vitamin B-12 status (>370 nmol/L) in NHANES 1999–2000, although prevalence in persons aged ≥60 y was 7% (56).
The roundtable noted that the lack of change in serum vitamin B-12 concentrations may be misleading because of the long latency period required to develop vitamin B-12 deficiency. Alternatively, the assumption that mild vitamin B-12 deficiency is very likely to progress to more severe clinical deficiency may be erroneous (9). Some roundtable experts noted that the ratio of high folate concentrations to low vitamin B-12 status generated the most concern about potential adverse effects of folic acid fortification. Selhub et al (15) observed anemia and cognitive impairment ≈5 times more often in the group with elevated folate status (>59 nmol/L) in combination with low vitamin B-12 status (serum <148 pmol/L or MMA >210 nmol/L) than in the group with normal vitamin B-12 and folate status.
The roundtable noted that the evolving observational evidence that suggests an association between subclinical vitamin B-12 deficiencies and adverse effects is of concern. However, pending the availability of clinical trials to confirm a causal relation between mild vitamin B-12 deficiency and adverse effects, whether mild vitamin B-12 deficiency imposes a public health risk is uncertain. Beginning in 2011, NHANES will include 3 cognitive function measures. Several experts thought that these new data would be useful to explore previously observed associations with the more limited cognitive function data in past NHANES. However, others questioned the relevance to vitamin B-12 deficiency of cognitive function tests designed to detect Alzheimer disease or the continued need for more NHANES hypothesis-generating research, given that several observational studies have already identified associations between vitamin B-12 status and cognitive function. Another reason to reinstate vitamin B-12 biomarker measures is the need for population-based prevalence estimates as new data become available from clinical trials. NHANES data could also provide useful information on the quantitative relation between intakes and biomarker concentrations, although malabsorption problems with some vitamin B-12 insufficiencies would complicate such analyses. Some experts suggested estimating absorption status by a blood test (eg, intrinsic factor antibody) in people with low vitamin B-12 status to distinguish patients with pernicious anemia from those with low vitamin B-12 status due to other causes.
The roundtable considered population-based changes beyond the aging US population that could affect vitamin B-12 status and would justify including vitamin B-12 biomarkers in future NHANES. More people use proton pump inhibitors and histamine 2 receptor antagonists (H2 blockers) that may decrease vitamin B-12 absorption; these are now available over-the-counter (57, 58). Other changes, such as the common use of antibiotics in children and young and middle-aged adults, could improve vitamin B-12 status by decreasing Helicobacter pylori infections that have statistical associations with decreased vitamin B-12 absorption. Increased adoption of vegan diets, the substitution of chicken for beef, and decreased use of dairy products could lower vitamin B-12 intakes. Several experts felt that as the use of vitamin B-12–containing supplements (including some with doses of 1000–2000 μg/d) and fortified foods increases, monitoring long-term, high vitamin B-12 intakes would be useful to evaluate the safety of chronic exposures to excessively high intakes in healthy populations. Monitoring vitamin B-12 intakes could help assess whether lifestyle changes are associated with changes in vitamin B-12 status.
Which biomarkers should future NHANES include?
The roundtable addressed which biomarkers to include in NHANES if the program reinstates vitamin B-12 status monitoring. Given each biomarker's sensitivity and specificity problems, the results of a single biomarker measurement would be difficult to interpret. But if NHANES can measure only one biomarker, some experts felt that this measure should reflect the broad range of vitamin B-12 status in the US population. Vitamin B-12 and holoTC increase continuously with increasing intakes, at least until vitamin B-12 saturates the transport proteins, and therefore reflect a broad range of intakes and status. Other roundtable experts felt that the sensitivity of MMA and tHcy to early inadequacies in vitamin B-12 status and marginal vitamin B-12 intakes could support the use of either one as the sole NHANES biomarker. Mean corpuscular volume to detect megaloblastic anemia would not be useful because <10% of patients with vitamin B-12 deficiency have megaloblastic anemia, and high mean corpuscular volume is more likely to reflect alcohol abuse than vitamin B-12 deficiency (9).
However, the roundtable strongly urged that, given the sensitivity and specificity problems of all vitamin B-12–related biomarkers, future NHANES should concurrently measure at least one biomarker of circulating concentrations of vitamin B-12 (vitamin B-12 or holoTC) and one biomarker of functional vitamin B-12 status (MMA or tHcy). If a choice must be made between serum vitamin B-12 and holoTC, holoTC has the advantage of not being affected by “false-positive” low vitamin B-12 concentrations such as those caused by genetically determined haptocorrin deficiencies. These conditions result in low circulating vitamin B-12 concentrations but have no adverse effect on vitamin B-12 status because they do not affect holoTC, which is the universal transport protein for vitamin B-12 uptake in all cells. However, the roundtable also recognized that holoTC measurement is new and would benefit from additional performance studies to engender full confidence in the use of holoTC for population-based surveys. Therefore, at this time, the roundtable agreed that serum vitamin B-12 is preferable over holoTC as the measure of circulating concentrations of vitamin B-12. MMA is preferable to tHcy if a choice must be made between these biomarkers because it increases with vitamin B-12 inadequacy, but not with folate inadequacy, whereas both of these nutrient deficiencies affect tHcy.
The roundtable generally agreed that, if NHANES reinstates 2 vitamin B-12–related biomarkers, serum vitamin B-12 and plasma MMA would provide continuity with past surveys and provide circulating and functional indicators of vitamin B-12 status. These variables have shown associations with anemia and cognitive decline in previous NHANES and in other studies (12–15, 59). Reliable measurement procedures are available, and the NIST is developing reference materials. The roundtable also suggested that NHANES periodically measure vitamin B-12, holoTC, MMA, and tHcy concurrently to provide valuable information on their relations in the general population and on how prevalence estimates vary by biomarker or biomarker combinations.
SUMMARY
In July 2010, a roundtable reviewed the measurement of vitamin B-12 status biomarkers in NHANES. The roundtable was uncertain whether subclinical vitamin B-12 deficiency is a public health problem warranting population-based monitoring. However, associations between subclinical vitamin B-12 deficiency and adverse health outcomes in observational studies are of concern and urgently need further evaluation in clinical trials. Clinical trials must use accurate and reliable measurement procedures to determine appropriate cutoffs for biomarker concentrations to identify at-risk populations. The roundtable was generally satisfied with the vitamin B-12 biomarker measurement procedures that past NHANES have used or that are available for use in future NHANES, as well as the reference methods and materials available from, or under development by, the NIST. The experts supported reinstating vitamin B-12–related biomarkers in future NHANES and suggested several public health and environmental reasons for doing so. Finally, the roundtable agreed that future NHANES should include at least 2 biomarkers—1 of circulating vitamin B-12 concentrations (preferably vitamin B-12) and 1 metabolic indicator of vitamin B-12 insufficiency (preferably MMA).
Acknowledgments
We thank Anne Thurn and Claudia Faigen of the Office of Dietary Supplements, National Institutes of Health; Kimberly Potter, Megan McNamee, and Therese Gibson of ICF International; and Mike Bykowski of Consolidated Solutions and Innovations for their outstanding logistical, organizational, and follow-up support. We thank Deborah Berlyne for her expert and timely technical editing services.
The authors’ responsibilities were as follows—MFP, CLJ, EAY, and PMC: conceived and sponsored the roundtable project; MFP, CLJ, EAY, PMC, RLB, DAL, AMM, JLM, CMP, KWP, CS, BS, and TT: served on the planning committee; EAY, CLJ, JHE, JM, RAD-A, CS, BS, CMP, KWP, JS, RC, EN, RLB, and DAL: presented data and background information; EAY: drafted the manuscript with considerable input from CMP and KWP; EAY, CLJ, and PMC: had primary responsibility for the final manuscript content; and all authors: fully participated in the roundtable discussions and read and approved the final manuscript. RG and DWJ serve on the Scientific Advisory Boards of Emisphere Technologies Inc of Cedar Knolls, NJ, and PAR Pharmaceuticals of Woodcliff Lake, NJ. DWJ also serves on the Scientific Advisory Board of Diazyme-GA, La Jolla, CA. For the past 3 y, AMM carried out a research project that was funded by Axis Shield Diagnostics and also carried a consulting agreement with this firm. RC's hospital filed a patent application for his work on the genetics of transcobalamin I deficiency. None of the other authors had any personal or financial conflicts of interest.
REFERENCES
- 1.Yetley EA, Johnson CL. Folate and vitamin B-12 biomarkers in NHANES: history of their measurement and use. Am J Clin Nutr 2011;94(suppl):332S–31S [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bock JL, Eckfeldt JH. Advances in standardization of laboratory measurement procedures: implications for measuring biomarkers of folate and vitamin B-12 status in NHANES. Am J Clin Nutr 2011;94(suppl):332S–6S [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Yetley EA, Pfeiffer CM, Phinney KW, et al. Biomarkers of folate status in NHANES: a roundtable summary. Am J Clin Nutr 2011;94(suppl):303S–12S [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yetley EA, Coates PM, Johnson CL. Overview of a roundtable on NHANES monitoring of biomarkers of folate and vitamin B-12 status: measurement procedure issues. Am J Clin Nutr 2011;94(suppl):297S–392S [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Green R, Miller JW. Vitamin B12 deficiency is the dominant nutritional cause of hyperhomocysteinemia in a folic acid-fortified population. Clin Chem Lab Med 2005;43:1048–51 [DOI] [PubMed] [Google Scholar]
- 6.Carmel R, Green R, Jacobsen DW, Rasmussen K, Florea M, Azen C. Serum cobalamin, homocysteine, and methylmalonic acid concentrations in a multiethnic elderly population: ethnic and sex differences in cobalamin and metabolite abnormalities. Am J Clin Nutr 1999;70:904–10 [DOI] [PubMed] [Google Scholar]
- 7.Ganji V, Kafai MR. Demographic, lifestyle, and health characteristics and serum B vitamin status are determinants of plasma total homocysteine concentration in the post-folic acid fortification period, 1999-2004. J Nutr 2009;139:345–52 [DOI] [PubMed] [Google Scholar]
- 8.Nexo E., Hoffmann-Lücke E. Holotranscobalamin, a marker of vitamin B-12 status: analytical aspects and clinical utility. Am J Clin Nutr 2011;94(suppl):359S–65S [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Carmel R. Biomarkers of cobalamin (vitamin B-12) status in the epidemiologic setting: a critical overview of context, applications, and performance characteristics of cobalamin, methylmalonic acid, and holotranscobalamin II. Am J Clin Nutr 2011;94(suppl):348S–58S [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Carmel R, Sarrai M. Diagnosis and management of clinical and subclinical cobalamin deficiency: advances and controversies. Curr Hematol Rep 2006;5:23–33 [DOI] [PubMed] [Google Scholar]
- 11.Hvas A-M, Ellegaard J, Nexo E. Increased plasma methylmalonic acid level does not predict clinical manifestations of vitamin B12 deficiency. Arch Intern Med 2001;161:1534–41 [DOI] [PubMed] [Google Scholar]
- 12.Morris MS, Jacques PF, Rosenberg IH, Selhub J. Folate and vitamin B-12 status in relation to anemia, macrocytosis, and cognitive impairment in older Americans in the age of folic acid fortification. Am J Clin Nutr 2007;85:193–200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Garrod MG, Green R, Allen LH, et al. Fraction of total plasma vitamin B12 bound to transcobalamin correlates with cognitive function in elderly Latinos with depressive symptoms. Clin Chem 2008;54:1210–7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Riggs KM, Spiro A, III, Tucker K, Rush D. Relations of vitamin B-12, vitamin B-6, folate and homocysteine to cognitive performance in the Normative Aging Study. Am J Clin Nutr 1996;63:306–14 [DOI] [PubMed] [Google Scholar]
- 15.Selhub J, Morris MS, Jacques PF, Rosenberg IH. Folate-vitamin B-12 interaction in relation to cognitive impairment, anemia, and biochemical indicators of vitamin B-12 deficiency. Am J Clin Nutr 2009;89:702S–6S [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Miller JW, Garrod MG, Allen LH, Haan MN, Green R. Metabolic evidence of vitamin B-12 deficiency, including high homocysteine and methylmalonic acid and low holotranscobalamin, is more pronounced in older adults with elevated plasma folate. Am J Clin Nutr 2009;90:1586–92 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Clarke R, Sherliker P, Hin H, et al. Folate and vitamin B12 status in relation to cognitive impairment and anaemia in the setting of voluntary fortification in the UK. Br J Nutr 2008;100:1054–9 [DOI] [PubMed] [Google Scholar]
- 18.Green R. Indicators for assessing folate and vitamin B12 status and for monitoring the efficacy of intervention strategies. Food Nutr Bull 2008;29:S52–63 [DOI] [PubMed] [Google Scholar]
- 19.Vogiatzoglou A, Oulhaj A, Smith AD, et al. Determinants of plasma methylmalonic acid in a large population: implications for assessment of vitamin B12 status. Clin Chem 2009;55:2198–206 [DOI] [PubMed] [Google Scholar]
- 20.Hvas A-M, Nexo E. Holotranscobalamin—a first choice assay for diagnosing early vitamin B deficiency? J Intern Med 2005;257:289–98 [DOI] [PubMed] [Google Scholar]
- 21.Clarke R, Sherliker P, Hin H, et al. Detection of vitamin B12 deficiency in older people by measuring vitamin B12 or the active fraction of vitamin B12, holotranscobalamin. Clin Chem 2007;53:963–70 [DOI] [PubMed] [Google Scholar]
- 22.Selhub J, Jacques PF, Rosenberg IH, et al. Serum total homocysteine concentrations in the third National Health and Nutrition Examination Survey (1991-1994): population reference ranges and contribution of vitamin status to high serum concentrations. Ann Intern Med 1999;131:331–9 [DOI] [PubMed] [Google Scholar]
- 23.Morris MS, Jacques PF, Rosenberg IH, Selhub J. Elevated serum methylmalonic acid concentrations are common among elderly Americans. J Nutr 2002;132:2799–803 [DOI] [PubMed] [Google Scholar]
- 24.Gunter EW, Lewis BG, Koncikowski SM. Laboratory procedures used for the third National Health and Nutrition Examination Survey (NHANES III), 1988-1994. Atlanta, GA: Centers for Disease Control and Prevention; Hyattsville, MD: National Center for Health Statistics, 1996. Available from: http://www.cdc.gov/nchs/data/nhanes/nhanes3/cdrom/nchs/manuals/labman.pdf (cited 4 December 2010) [Google Scholar]
- 25.Centers for Disease Control and Prevention NHANES 1999-2000: folate/vitamin B12, serum and whole blood, Bio-Rad Laboratories’ “Quantaphase II folate/vitamin B12” radioassay kit. Available from: http://www.cdc.gov/nchs/data/nhanes/nhanes_99_00/lab06_met_folate_b12.pdf (cited 4 December 2010)
- 26.Centers for Disease Control and Prevention NHANES 2001-2002: folate/vitamin B12, serum and whole blood, Bio-Rad Laboratories “Quantaphase II Folate/Vitamin B12” radioassay kit. Available from: http://www.cdc.gov/nchs/data/nhanes/nhanes_01_02/l06_b_met_folate_b12.pdf (cited 4 December 2010)
- 27.Centers for Disease Control and Prevention NHANES 2003-2004: folate/vitamin B12, serum and whole blood, Bio-Rad Laboratories’ “Quantaphase II Folate/Vitamin B12” Radioassay Kit. Available from: http://www.cdc.gov/nchs/data/nhanes/nhanes_03_04/l06_c_met_folates%20B12.pdf (cited 4 December 2010)
- 28.Centers for Disease Control and Prevention NHANES 2005-2006: folate/vitamin B12, serum and whole blood, Laboratories “Quantaphase II Folate/Vitamin B12” radioassay kit. Available from: http://www.cdc.gov/nchs/data/nhanes/nhanes_05_06/folate_b12_d_met.pdf (cited 4 December 2010)
- 29.Pfeiffer CM, Johnson CL, Jain RB, et al. Trends in blood folate and vitamin B-12 concentrations in the United States, 1988–2004. Am J Clin Nutr 2007;86:718–27 [DOI] [PubMed] [Google Scholar]
- 30.National Institute of Standards and Technology Development of standard reference materials for vitamins B6 and B12 in human serum. Available from: http://www.nist.gov/mml/analytical/organic/vitsb6andb12inserum.cfm (cited 4 December 2010)
- 31.Centers for Disease Control and Prevention NHANES 1999-2000: methylmalonic acid (MMA), serum, GC/MS. Available from: http://www.cdc.gov/nchs/data/nhanes/nhanes_99_00/lab06_met_methylmalonic_acid.pdf (cited 4 December 2010)
- 32.Centers for Disease Control and Prevention NHANES 2001-2002: methylmalonic acid (MMA), plasma or serum, GC/MS. Available from: http://www.cdc.gov/nchs/data/nhanes/nhanes_01_02/l06_b_met_methylmalonic_acid.pdf (cited 4 December 2010)
- 33.Centers for Disease Control and Prevention NHANES 2003-2004: methylmalonic acid (MMA), plasma or serum, GC/MS. Available from: http://www.cdc.gov/nchs/data/nhanes/nhanes_03_04/l06_c_met_mma.pdf (cited 4 December 2010)
- 34.Pfeiffer CM, Gunter EW. Automated assay for methylmalonic acid (MMA) in plasma. 51st Annual Meeting of American Association of Clinical Chemists, New Orleans, LA, July 1999. Clin Chem 1999;45(suppl 6):A166 (abstr. 593) [Google Scholar]
- 35.Blom HJ. Rooij AV, Hogeveen M. A simple high-throughput method for the determination of plasma methylmalonic acid by liquid chromatography-tandem mass spectrometry. Clin Chem Lab Med 2007;45:645–50 [DOI] [PubMed] [Google Scholar]
- 36.Lakso H-A, Appelblad P, Schneede J. Quantification of methylmalonic acid in human plasma with hydrophilic interaction liquid chromatography separation and mass spectrometric detection. Clin Chem 2008;54:2028–35 [DOI] [PubMed] [Google Scholar]
- 37.Fasching C, Singh J. Quantitation of methylmalonic acid in plasma using liquid chromatography-tandem mass spectrometry. Methods Mol Biol 2010;603:371–8 [DOI] [PubMed] [Google Scholar]
- 38.Centers for Disease Control and Prevention NHANES 1999-2000: total homocysteine (tHcy), plasma, Abbott homocysteine (HCY) assay. Available from: http://www.cdc.gov/nchs/data/nhanes/nhanes_99_00/lab06_met_homocysteine.pdf (cited 4 December 2010)
- 39.Centers for Disease Control and Prevention. NHANES 2001-2002: total homocysteine (tHcy), plasma, “Abbott AxSYM homocysteine (HCY) assay.”. Available from: http://www.cdc.gov/nchs/data/nhanes/nhanes_01_02/l06_b_met_homocysteine_Axsym.pdf (cited 4 December 2010)
- 40.Centers for Disease Control and Prevention NHANES 2001-2002: total homocysteine (tHcy), plasma, Abbott IMX homocysteine (HCY) assay. Available from: http://www.cdc.gov/nchs/data/nhanes/nhanes_01_02/l06_b_met_homocysteine_IMX.pdf (cited 4 December 2010)
- 41.Centers for Disease Control and Prevention NHANES 2003-2004: total homocysteine (tHcy), plasma, Abbot homocysteine (HCY) assay. Available from: http://www.cdc.gov/nchs/data/nhanes/nhanes_03_04/l06_c_met_homocysteine.pdf (cited 4 December 2010)
- 42.Centers for Disease Control and Prevention. NHANES 2005-2006: total homocysteine (tHcy), plasma, “Abbott Homocysteine (HCY) assay.”. Available from: http://www.cdc.gov/nchs/data/nhanes/nhanes_05_06/hcy_d_met.pdf (cited 4 December 2010)
- 43.Pfeiffer CM, Twite D, Shih J, Holets-McCormack SR, Gunter EW. Method comparison for total plasma homocysteine between the Abbott IMx analyzer and an HPLC assay with internal standardization. Clin Chem 1999;45:152–3 [PubMed] [Google Scholar]
- 44.Pfeiffer CM, Caudill SP, Gunter EW, et al. Analysis of factors influencing the comparison of homocysteine values between the third National Health and Nutrition Examination Survey (NHANES) and NHANES 1999+. J Nutr 2000;130:2850–4 [DOI] [PubMed] [Google Scholar]
- 45.Pfeiffer CM, Osterloh JD, Kennedy-Stephenson J, et al. Trends in circulating concentrations of total homocysteine among US adolescents and adults: findings from the 1991-1994 and 1999-2004 National Health and Nutrition Examination Surveys. Clin Chem 2008;54:801–13 [DOI] [PubMed] [Google Scholar]
- 46.Brady J, Wilson L, McGregor L, Valente E, Orning L. Active B12: a rapid, automated assay for holotranscobalamin on the Abbott AxSYM analyzer. Clin Chem 2008;54:567–73 [DOI] [PubMed] [Google Scholar]
- 47.Morkbak AL, Heimdal RM, Emmens K, et al. Evaluation of the technical performance of novel holotranscobalamin (holoTC) assays in a multicenter European demonstration project. Clin Chem Lab Med 2005;43:1058–64 [DOI] [PubMed] [Google Scholar]
- 48.National Institute of Standards and Technology Certificate of analysis, standard reference material 1955, homocysteine and folate in frozen human serum. April 2008. Available from: https://www-s.nist.gov/srmors/certificates/1955.pdf?cfid=1126897&cftoken=ad62a5219ffb884e-41496e79-a2d7-bed2-991ce742a98a0716&jsessionid=f030a960d9d22f92f6db3a34674d5a634a2a (cited 4 December 2010) [DOI] [PubMed]
- 49.National Institute of Standards and Technology Certificate of analysis, standard reference material 909b, human serum. November 2003. Available from: http://ts.nist.gov/measurementservices/referencematerials/archived_certificates/909b.Nov19.2003.pdf (cited 4 December 2010)
- 50.National Institute of Standards and Technology Development of a standard reference material for metabolites in plasma. Available from: http://www.nist.gov/mml/analytical/organic/metabolitesinserum.cfm (cited 4 December 2010)
- 51.Satterfield MB, Sniegoski LT, Welch MJ, Nelson BC. Comparison of isotope dilution mass spectrometry methods for the determination of total homocysteine in plasma and serum. Anal Chem 2003;75:4631–8 [DOI] [PubMed] [Google Scholar]
- 52.Satterfield MB, Sniegoski LT, Sharpless KE, et al. Development of a new standard reference material: SRM 1955 (homocysteine and folate in human serum). Anal Bioanal Chem 2006;385:612–22 [DOI] [PubMed] [Google Scholar]
- 53.Nelson BC, Pfeiffer CM, Sniegoski LT, Satterfield MB. Development and evaluation of an isotope dilution LC/MS method for the determination of total homocysteine in human plasma. Anal Chem 2003;75:775–84 [DOI] [PubMed] [Google Scholar]
- 54.Nelson BC, Pfeiffer CM, Zhang M, Duewer DL, Sharpless KE, Lippa KA. Commutability of NIST SRM 1955 homocysteine and folate in frozen human serum with selected total homocysteine immunoassays and enzymatic assays. Clin Chim Acta 2008;395:99–105 [DOI] [PubMed] [Google Scholar]
- 55.JCTLM/Joint Committee on Traceability in Laboratory Medicine Isotope dilution mass spectrometry methods for homocysteine in blood serum. Sèvres Cedex, France: Bureau International des Poids et Mesures. Available from: http://www.bipm.org/jctlm/search.do?sortBy=Analyte_Name&searchString=homocysteine&analyteCategory=&matrixCategory=&countryCode=&status=P&type=isRMP&x=38&y=4 (cited 4 December 2010)
- 56.Pfeiffer CM, Caudill SP, Gunter EW, Osterloh J, Sampson EJ. Biochemical indicators of B vitamin status in the US population after folic acid fortification: results from the National Health and Nutrition Examination Survey 1999–2000. Am J Clin Nutr 2005;82:442–50 [DOI] [PubMed] [Google Scholar]
- 57.Valuck RJ, Ruscin JM. A case-control study on adverse effects: H2 blocker or proton pump inhibitor use and risk of vitamin B12 deficiency in older adults. J Clin Epidemiol 2004;57:422–8 [DOI] [PubMed] [Google Scholar]
- 58.Howden CW. Vitamin B12 levels during prolonged treatment with proton pump inhibitors. J Clin Gastroenterol 2000;30:29–33 [DOI] [PubMed] [Google Scholar]
- 59.Clarke R, Birks J, Nexo E, et al. Low vitamin B-12 status and risk of cognitive decline in older adults. Am J Clin Nutr 2007;86:1384–91 [DOI] [PubMed] [Google Scholar]