Abstract
We recently described acidified citrate cysteine medium (ACCM), which supports host cell-free (axenic) growth of Coxiella burnetii. After 6 days of incubation, greater than 3 logs of growth was achieved with the avirulent Nine Mile phase II (NMII) strain. Here, we describe modified ACCM and culture conditions that support improved growth of C. burnetii and their use in genetic transformation and pathogen isolation from tissue samples. ACCM was modified by replacing fetal bovine serum with methyl-β-cyclodextrin to generate ACCM-2. Cultivation of NMII in ACCM-2 with moderate shaking and in 2.5% oxygen yielded 4 to 5 logs of growth over 7 days. Similar growth was achieved with the virulent Nine Mile phase I and G isolates of C. burnetii. Colonies that developed after 6 days of growth in ACCM-2 agarose were approximately 0.5 mm in diameter, roughly 5-fold larger than those formed in ACCM agarose. By electron microscopy, colonies consisted primarily of the C. burnetii small cell variant morphological form. NMII was successfully cultured in ACCM-2 when medium was inoculated with as little as 10 genome equivalents contained in tissue homogenates from infected SCID mice. A completely axenic C. burnetii genetic transformation system was developed using ACCM-2 that allowed isolation of transformants in about 2 1/2 weeks. Transformation experiments demonstrated clonal populations in colonies and a transformation frequency of approximately 5 × 10−5. Cultivation in ACCM-2 will accelerate development of C. burnetii genetic tools and provide a sensitive means of primary isolation of the pathogen from Q fever patients.
INTRODUCTION
Coxiella burnetii is a wide-ranging zoonotic pathogen that causes a debilitating influenza-like illness in humans called Q fever (20). Following infection of a eukaryotic host cell, this intracellular bacterium replicates exclusively within a phagolysosome-like parasitophorous vacuole (PV) (16). C. burnetii directs development of the PV (15, 24) and manipulates other host cell functions such as apoptotic signaling (18, 29). The mechanisms by which C. burnetii modifies the host cell and causes disease are largely unknown. Indeed, lipopolysaccharide is the only defined virulence factor of C. burnetii with the full-length molecule of phase I bacteria required for full virulence (21).
The obligate intracellular nature of C. burnetii has severely impeded development of genetic tools for virulence factor discovery. Beare et al. (3) recently genetically transformed C. burnetii to chloramphenicol resistance and mCherry red fluorescent protein expression using the mariner-based Himar1 transposon. However, a significant limitation of the procedure is the 8 to 12 weeks required for expansion and clonal isolation of individual transposon mutants using cell culture-based propagation of C. burnetii. Moreover, the micromanipulation method used for harvesting clonal C. burnetii from an individual PV is technically challenging.
The recent description of a method for axenic (host cell-free) propagation of C. burnetii is a significant technological advance that will facilitate biochemical and genetic studies of the pathogen (22). A growth medium called acidified citrate cysteine medium (ACCM) was developed that supports roughly 3 logs (log10) of growth of C. burnetii over 6 days in a microaerobic environment. Minute (approximately 0.1 mm in diameter) colonies also develop over the same time frame in semisolid ACCM agarose. In the current study, we describe a modified version of ACCM called ACCM-2 that supports improved growth of C. burnetii in liquid medium and as colonies in agarose plates. Colonies contained clonal populations, thereby facilitating development of a fully axenic system for C. burnetii genetic transformation that substantially reduces the time of transformant isolation. ACCM-2 cultures were also successfully started with infected animal tissue homogenates containing small numbers of C. burnetii, thereby providing a potential means of obtaining clinical isolates from Q fever patients.
MATERIALS AND METHODS
C. burnetii isolates and host cell-based propagation.
C. burnetii Nine Mile phase II, clone 4 (NMII; RSA439), and low-passage-number stocks of Nine Mile phase I (NMI; RSA493) and G (Q212) isolates were used in this study. Host cell-based growth of C. burnetii was accomplished using African green monkey kidney (Vero) fibroblasts (CCL-81; American Type Culture Collection) grown in RPMI medium (Invitrogen, Carlsbad, CA) supplemented with 2% fetal bovine serum (FBS) at 37°C in a 5% CO2 atmosphere. Bacteria were purified from host cells using differential centrifugation as previously described (10) and stored at −80°C.
Axenic cultivation.
A modified form of ACCM (22) called ACCM-2, in which 1% FBS is replaced with 1 mg/ml methyl-β-cyclodextrin (Mβ-CD), was developed. C. burnetii was cultivated in T-75 cell culture flasks or 0.2-μm-pore-size-filter-capped 125-ml Erlenmeyer flasks containing 20 ml of medium, T-25 flasks containing 5 ml of medium, or 6-well tissue culture plates containing 3 ml of medium per well. Cultures were incubated at 37°C in a 2.5% O2 and 5% CO2 environment using a CO-170 incubator (New Brunswick Scientific, NJ). Oxygen was displaced by nitrogen gas. Where indicated, Erlenmeyer flasks were shaken at 75 rpm. C. burnetii replication was measured by optical density at 600 nm (OD600) or quantitative PCR (Q-PCR) of genome equivalents (GE) using a dotA probe as previously described (22).
C. burnetii colonies were established using a modified soft agarose overlay method in which bacteria are grown in the top medium layer. A 0.25% ACCM-2 agarose base in 100- by 20-mm petri dishes was created by mixing 10 ml of filter-sterilized 2× ACCM-2 with 10 ml of 0.5% (wt/vol in water) melted UltraPure agarose (Invitrogen). The bacterial inoculum was mixed with 2.5 ml of 0.1% melted ACCM-2 agarose equilibrated to 37°C, which was prepared by mixing together 1.25 ml of 2× ACCM-2, 0.75 ml of water, and 0.5 ml of 0.5% melted agarose. This solution was poured on top of the solidified ACCM-2 agarose base. Plates were refrigerated (4°C) for 30 min to aid solidification of the top agarose and then placed in a laminar airflow biosafety cabinet with lids ajar for 20 min to remove condensation. Plates were incubated for 6 days as described above for ACCM-2 to allow colony development.
Electron microscopy of C. burnetii propagated as colonies.
NMII grown as colonies was obtained from ACCM-2 agarose plates incubated for 6 days. The top agarose was removed using a cell scraper, and then the agarose base was rinsed with 1 ml phosphate-buffered saline (PBS; 10 mM Na2HPO4, 10 mM NaH2PO4, 150 mM NaCl, pH 7.8). The agarose and rinse samples were combined in 2-ml microcentrifuge tubes, and then samples were disrupted by repeated pipetting to release bacteria embedded in agarose. Samples were centrifuged at 2,000 × g for 5 min to pellet the agarose, and then supernatants were transferred to clean 1.5-ml microcentrifuge tubes that were centrifuged at 20,000 × g for 15 min to pellet C. burnetii. Bacteria were fixed for 2 h in 2.5% glutaraldehyde (vol/vol) with 0.05 M sucrose in 0.1 M sodium cacodylate buffer. Subsequent postfixation steps were performed with microwave irradiation in cycles of 2 min on, 2 min off, 2 min on at 250 W under vacuum (Pelco 3451; Ted Pella, Redding, CA). Samples were then incubated in 0.5% osmium tetroxide–0.8% potassium ferricyanide in 0.1 M sodium cacodylate, followed by 1% tannic acid in distilled water and finally 1% uranyl acetate in distilled water. Samples were dehydrated in a graded ethanol series for 1 min under vacuum and then infiltrated with Spurr's resin by incubation in graded Spurr's solutions (1:3, 1:1, 3:1 [Spurr's:ethanol]) using a microwave processor at 5-min cycles before embedding in Spurr's resin. Sections (80 nm) were cut using a Leica UC6 ultramicrotome (Leica Microsystems, Vienna, Austria) and stained with 1% uranyl acetate and Reynolds lead citrate. Samples were examined with a Hitachi H-7500 electron microscope (Hitachi, Pleasanton, CA), and images were captured with a Hamamatsu XR-100 digital camera system (AMT, Danvers, MA).
Establishment of antibiotic MICs.
The MICs of chloramphenicol and kanamycin required to inhibit NMII growth in ACCM-2 were determined by incubating organisms in medium containing 0.375, 0.75, 1.5, or 3 μg/ml of chloramphenicol or 125, 250, 375, or 500 μg/ml of kanamycin. Chloramphenicol and kanamycin were dissolved in ethanol and water, respectively. Solvents had no effect on C. burnetii growth when tested at the highest concentrations used in the assay. Growth in liquid ACCM-2 was measured by determining the OD600s of cultures grown in 3 ml of medium in a 6-well tissue culture plate. MICs were also established for NMII growth in ACCM-2 agarose using a CFU assay.
Colony genotyping.
ACCM-2 agarose was plated with equal numbers of wild-type NMII and an NMII transformant termed NMII-MC1 that contains a Himar1 transposon insertion between CBU0316 and CBU0317 (3, 4). Fourteen random colonies were picked from plates after 6 days of growth. A Zeiss Stemi 2000 stereo microscope was used to help visualize colonies averaging 0.5 mm in diameter. Colony locations were marked, and then individual colonies were extracted from the agarose overlay using a P-1000 pipette tip. To facilitate removal of colonies, the pipette tip opening was enlarged to approximately 5 mm in diameter by cutting the tip end. These modified tips were autoclaved prior to use. Each agarose plug was added to 1.0 ml of ACCM-2 in a sterile 1.5-ml microcentrifuge tube, and organisms were released from the agarose by repeated pipetting. The mixture was then added to 2 ml of sterile ACCM-2 (3 ml total) in 6-well plates that were incubated for 6 days to expand colony populations. Cultures were genotyped for the presence of NMII or NMII-MC1 by using PCR. Two microliters of culture medium was added directly to a PCR mix that contained primers specific to CBU0316 (CBU0316-F, forward primer) and CBU0317 (CBU0317-R, reverse primer) (Table 1). PCRs were conducted using AccuPrime Taq DNA polymerase (Invitrogen), and reaction products were analyzed by gel electrophoresis using a 0.8% agarose gel. Products of 1.6 and 4.8 kb are expected from amplification of NMII and NMII-MC1 genomic DNA, respectively.
Table 1.
Primers used in this study
| Primer | Sequence (5′–3′) |
|---|---|
| CBU0316-F | GCAAAACAAGAGCAAAATATTGTTTACC |
| CBU0317-R | TTGATCGTTCCAGAGACAG |
| MCforpJB2581-F | ACAGGAAACAGAATTCAGGAGAAATTACTATGGTCTCTAAGGGCGAGGAAGACAAC |
| MCforpJB2581-R | CGACTCTAGAGGATCCTTATTTGTACAGCTCATCCATGCC |
| CAT-P1169F | TCATGAAGGAGGGCCCTTATGGAGAAAAAAATCACTGGATATACC |
| CAT-pJB2581-HindIIIrecR | GCAGGCATGCAAGCTTTTACGCCCCGCCCTGCCACTC |
| Kan-P1169F | TCATGAAGGAGGGCCCTTATGATTGAACAAGATGGATTGC |
| Kan-pJB2581-HindIIIrecR | GCAGGCATGCAAGCTTTCAGAAGAACTCGTCAAGAAGGCGATAG |
| P1169-pJB2581-Ab-HindIIIrecF | CAAAACAGCCAAGCTTATGGCTTCGTTTCGCAGCG |
| P1169-R | AAGGGCCCTCCTTCATGAAGGATTAATGTCATTATTTATTTATGGGG |
Transformation of NMII.
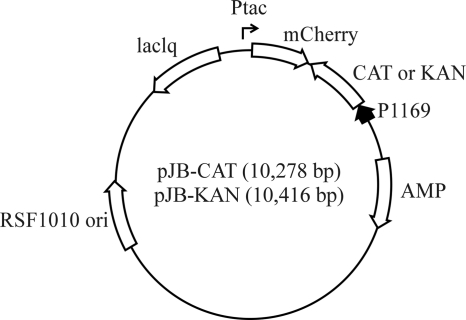
The plasmids pJB-CAT and pJB-KAN (Fig. 1), conferring resistance to chloramphenicol and kanamycin, respectively, were used to transform NMII, and were constructed using pJB2581 as the backbone (2). The cyaA gene of pJB2581 was first replaced with the mCherry gene, which was amplified by PCR from p1898-Tn (3) using primers MCforpJB2581-F and MCforpJB2581-R (Table 1), and cloned into plasmid digested with EcoRI and BamHI. The chloramphenicol acetyltransferase (CAT) gene was amplified from pJB2581 using the primers CAT-P1169F and CAT-pJB2581-HindIIIrecR, and the kanamycin resistance gene (KAN) was amplified from pCR2.1-topo using the primers KAN-P1169F and KAN-pJB2581-HindIIIrecR. The CBU1169 promoter (P1169) was amplified from C. burnetii genomic DNA using the primers P1169-pJB2581-Ab-HindIIIrecF and P1169-R. The CAT and KAN genes were placed downstream from P1169 to create P1169-CAT and P1169-KAN cassettes using overlapping PCR and the primers P1169-pJB2581-Ab-HindIIIrecF and CAT-pJB2581-HindIIIrecR or KAN-pJB2581-HindIIIrecR, respectively. P1169-CAT and P1169-KAN cassettes were cloned into HindIII-digested pJB2581::mCherry using the In-fusion kit (BD Clontech, Mountain View, CA) to create pJB-CAT and pJB-KAN, respectively. PCR was conducted with AccuPrime Pfx polymerase (Invitrogen) and primers from Integrated DNA Technologies (Coralville, IA).
Fig. 1.
Composite map of pJB-CAT and pJB-KAN. Plasmids contain a RSF1010 origin of replication and a chloramphenicol or kanamycin resistance gene under the control of the C. burnetii CBU1169 promoter.
Transformation experiments used NMII cultured for 6 days in ACCM-2. Cultures were grown with shaking in Erlenmeyer flasks. Bacteria were pelleted by centrifugation for 15 min at 16,000 × g, washed in 10% glycerol, pelleted again, and then suspended in 10% glycerol at a cell density of approximately 4 × 109 GE/ml. Organisms were kept on ice until electroporation. Fifty microliters of C. burnetii suspension (2 × 108 GE) was mixed with 10 μg of pJB-CAT or pJB-KAN and placed in a 0.1-cm electroporation cuvette (precooled on ice). Cells were electroporated at 18 kV, 500 Ω, and 25 μF for 7 to 13 ms, which results in approximately 50% killing (unpublished observations). Immediately following electroporation, 950 μl of RPMI cell culture medium was added to the cuvette and the sample was mixed, and then 200 μl was added to 3 ml of ACCM-2 in a 6-well plate. Cultures were incubated overnight, and then kanamycin (final concentration of 375 μg/ml) or chloramphenicol (final concentration of 3 μg/ml) was added to the medium for transformant selection. C. burnetii transformants were cultured for a total of 4 days; then, 100 μl of the culture was plated on antibiotic-containing ACCM-2 agarose.
Genes conferring resistance to chloramphenicol, kanamycin, or ampicillin are approved for C. burnetii genetic transformation by the Rocky Mountain Laboratories Institutional Biosafety Committee and the Centers for Disease Control and Prevention Select Agents Program.
SCID mice infections.
Six-week-old SCID mice (NOD.CB17-Prkdcscid/J) were purchased from Jackson Laboratory. Three mice per group were challenged intratracheally or intraperitoneally with 106 GE of ACCM-2-grown NMII. At 7 days postinfection, lungs, liver, and spleen were aseptically harvested and stored at −80°C. At the time of processing, whole organs were disrupted by gentle mechanical homogenization in 5 ml of ACCM-2. To quantify bacterial load by Q-PCR, 50 μl of tissue homogenate was processed using the High-Pure PCR template kit (Roche) and NMII GE were determined using primers specific for the C. burnetii com1 gene as previously described (6). Culture positivity was determined by inoculating 5 ml of ACCM-2 in T-25 flasks with 50 μl of 100-fold-diluted tissue homogenates containing known amounts of NMII GE. After a 7-day incubation, 1 ml of each ACCM-2 culture was centrifuged at 15,000 × g for 20 min to pellet NMII. The bacterial pellet was suspended in 100 μl of sucrose phosphate buffer (PBS containing 250 mM sucrose), and 25 μl was processed for Q-PCR as described above. Animal experiments were performed according to protocol number AUP2009-20 approved by the University Animal Care Committee of Texas A&M University.
RESULTS
NMII growth is improved in ACCM-2.
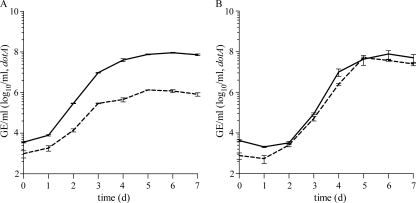
ACCM contains FBS and supports roughly 3 logs of NMII growth over a 6-day incubation without shaking (22). We found that by replacing FBS with 1.0 mg/ml Mβ-CD to generate ACCM-2, and by slowly shaking the cultures (75 rpm), growth yield of NMII was improved. NMII cultures were initiated with approximately 103 organisms/ml, and the OD600 and GE were measured over a 7-day incubation. Cultures in ACCM without shaking and in ACCM-2 with shaking showed OD600 increases from 0 to 0.160 ± 0.004 and 0.587 ± 0.003, respectively. Q-PCR showed GE increases of 2.9 ± 0.075 and 4.4 ± 0.042 logs in ACCM without shaking and in ACCM-2 with shaking, respectively (Fig. 2A). The log phase (1 to 3 days postinoculation) generation time of NMII in ACCM-2 was 4.7 h, 4.4 h less than that observed in ACCM (22). Shaking of ACCM moderately improved NMII growth but not to the level of growth in shaken ACCM-2 (data not shown).
Fig. 2.
Cultivation of C. burnetii in ACCM-2. (A) Growth of NMII in ACCM-2 with shaking (solid line) and ACCM without shaking (dotted line). (B) Growth of the virulent C. burnetii NMI (dotted line) and G (solid line) isolates in ACCM-2 with shaking. Growth was measured by enumerating GE, and results are from three separate cultures ± the standard error of the mean.
ACCM-2 supports growth of virulent C. burnetii.
The avirulent NMII isolate was used to develop ACCM (22) and ACCM-2 culture methods. To confirm that ACCM-2 supports growth of virulent C. burnetii isolates, media were inoculated with the NMI and G isolates (5) and their growth was assessed. In ACCM-2, NMI and G exhibited growth yield equivalent to that observed for NMII with 4.5 ± 0.094 and 4.1 ± 0.378 logs of growth over 7 days, respectively (Fig. 2B).
Colony growth is improved in ACCM-2 agarose.
NMII forms minute (approximately 0.1-mm-diameter) colonies in ACCM agarose (22). To test whether improved growth of NMII in ACCM-2 correlated with larger colonies in ACCM-2 agarose, NMII was plated and colony size was assessed after a 6-day incubation. Colonies in ACCM-2 agarose were 5-fold larger (approximately 0.5 mm in diameter) than those in ACCM agarose (Fig. 3A and B). Colonies in ACCM-2 agarose were primarily comprised of the small cell variant (SCV) form of C. burnetii as assessed by size and characteristic condensed chromatin (9) (Fig. 3C). Virulent NMI and G strains formed colonies in ACCM-2 agarose similar in size to those formed by NMII (data not shown).
Fig. 3.
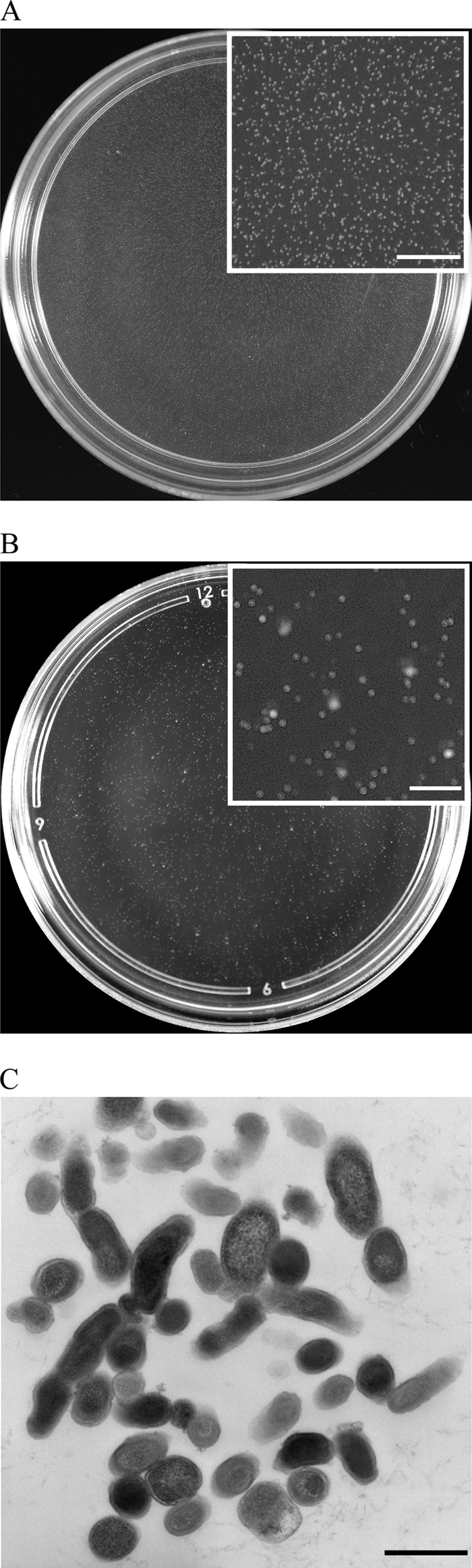
Colony formation by C. burnetii in ACCM and ACCM-2 agarose. (A) Representative ACCM plate showing NMII colonies that average approximately 0.1 mm in diameter. Scale bar, 10 mm. (B) Representative ACCM-2 plate showing NMII colonies that average approximately 0.5 mm in diameter. Scale bar, 10 mm. (C) Electron microscopy of colony-grown C. burnetii showing primarily the SCV morphological form. Scale bar, 0.5 μm.
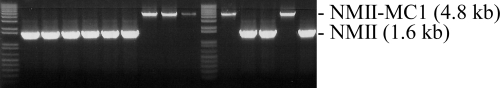
C. burnetii colonies in ACCM-2 agarose are clonal.
The plating efficiency of NMII in ACCM-2 agarose was 1 to 2 GE per colony formed, suggesting that colonies develop from single organisms. To confirm clonality, ACCM-2 agarose was plated with equal numbers of wild-type NMII and a NMII transformant termed NMII-MC1 that contains a Himar1 transposon insertion between CBU0316 and CBU0317 conferring mCherry expression and chloramphenicol resistance (3, 4). NMII-MC1 and NMII have been previously shown to grow at equal rates (4). Fourteen random colonies were picked from plates after 6 days of growth, expanded in ACCM-2, and then genotyped by PCR. Each colony contained either NMII or NMII-MC1 but not both (Fig. 4), illustrating the clonality of C. burnetii colonies in ACCM-2 agarose.
Fig. 4.
NMII colonies in ACCM-2 agarose are clonal. Equal numbers of NMII and NMII-MC1, which contains a Himar1 transposon insertion between CBU0316 and CBU0317, were plated in ACCM-2 agarose. Fourteen random colonies were picked after 6 days of growth and genotyped as described in Materials and Methods. Each colony contained either NMII (1.6-kb band) or NMII-MC1 (4.8-kb band) but not both, showing the clonality of C. burnetii colonies in ACCM-2 agarose.
Culture in ACCM-2 accelerates C. burnetii genetic transformation.
The host cell-based C. burnetii genetic transformation protocol described by Beare et al. (3) requires 8 to 12 weeks for clonal isolation of transformants. Therefore, we investigated whether ACCM-2 culture methods could accelerate the procedure. The first step was to determine the MICs of chloramphenicol and kanamycin in ACCM-2. NMII was cultured under different antibiotic concentrations, and growth was measured by OD600 in ACCM-2, or colony development in ACCM-2 agarose, after a 6-day incubation. The MICs of chloramphenicol and kanamycin in ACCM-2 were 1.5 μg/ml and 375 μg/ml, respectively. The MICs of chloramphenicol and kanamycin in ACCM-2 agarose were 3.0 μg/ml and 375 μg/ml, respectively.
We next optimized a procedure for isolating C. burnetii transformants and established a transformation frequency. The plasmids pJB-CAT and pJB-KAN, conferring chloramphenicol and kanamycin resistance, respectively, were constructed for these experiments (see Fig. 1 and Materials and Methods). These plasmids contain an RSF1010 origin of replication that can support autonomous replication of heterologous plasmid DNA in C. burnetii (7). Following electroporation, optimal recovery of antibiotic-resistant colonies in ACCM-2 agarose was observed if organisms were plated after 4 days of recovery in ACCM-2. Almost no colonies were observed prior to this point. Based on colony counts, an estimated 8 × 104 pJB-CAT and 4 × 104 pJB-KAN transformants were present in ACCM-2 before plating. Assuming that the 1 × 108 viable C. burnetii transformants remaining after electroporation underwent eight divisions during recovery in ACCM-2, we estimate a transformation frequency of approximately 5 × 10−5. Thus, genetic transformants can be recovered for analysis in as little as 16 days using axenic culture: 4 days of transformant recovery in ACCM-2, 6 days of colony development in ACCM-2 agarose, and 6 days of colony expansion in ACCM-2.
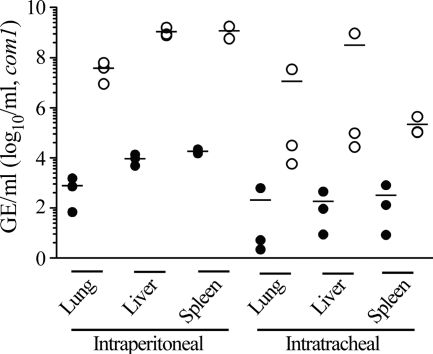
ACCM-2 supports growth of C. burnetii isolated from animal tissue.
Cell culture-based methods of isolating virulent C. burnetii from clinical samples have variable success rates (13, 27). Therefore, we tested whether ACCM-2 can be used to isolate C. burnetii from animal tissue. As a model, NMII-infected SCID mice were employed (1, 23, 25). Mice were infected intratracheally or intraperitoneally, and lungs, liver, and spleen were harvested at 7 days postinfection. Five ml of ACCM-2 was inoculated with a 1:100 dilution of tissue homogenate, and growth over 7 days was measured by Q-PCR (Fig. 5). Based on the starting number of GE/ml, NMII burdens were highest in tissues harvested from mice infected intraperitoneally. NMII was recovered by axenic cultivation from all tissues, with GE increases of several logs observed for all inocula. The method was highly sensitive, with several cultures successfully started with fewer than 100 total C. burnetii GE. In fact, one 5-ml culture was started with 10 GE contained in diluted lung homogenate from a mouse infected intraperitoneally (Fig. 5).
Fig. 5.
ACCM-2 supports culture of C. burnetii from infected animal tissue. ACCM-2 was inoculated with a 1:100 dilution of total lung, liver, or spleen homogenates derived from NMII-infected SCID mice infected by intraperitoneal or intratracheal routes as described in Materials and Methods. Closed symbols indicate the starting numbers of GE/ml. Open symbols indicate the numbers of GE/ml after a 7-day incubation. Depicted data are the means of three ACCM-2 cultures individually started with tissue homogenates from three infected mice.
DISCUSSION
In the current study, we describe improved ACCM-based culture methods and their use in a fully axenic system for C. burnetii genetic transformation and isolation of the pathogen from tissue. Culturing of C. burnetii in gently shaken ACCM-2, containing Mβ-CD instead of FBS, results in an approximately 1.5 log increase in bacterial yield compared to that obtained when culturing in ACCM. Pathogen generation time in ACCM-2 is reduced to 4.7 h, almost half of that observed in ACCM. In addition, average colony size is increased by about 5-fold to a diameter of approximately 0.5 mm, greatly facilitating the isolation and characterization of clonal populations of C. burnetii.
The use of ACCM-2 in C. burnetii genetic transformation has several advantages over the previously described Vero cell system of transformant propagation (3). First, the time required to isolate clonal populations of C. burnetii transformants is reduced from 2 to 3 months to as little as 16 days. Second, axenic culture allows recovery of some C. burnetii transformants incapable of intracellular growth. Third, transformation frequency can be estimated.
The substitution of Mβ-CD for FBS in ACCM-2 improves C. burnetii growth. Cyclodextrins can also replace FBS in Helicobacter pylori culture medium (19) and similarly improves growth of Bordetella pertussis (17). Improved growth may result from Mβ-CD sequestration of inhibitory metabolites, such as certain fatty acids (11).
C. burnetii colony size increases as the agarose percentage decreases (A. Omsland and R. A. Heinzen, unpublished observations). By mixing the bacterial inoculum with a low-density (0.1%) ACCM-2 agarose top medium, colonies develop to approximately 0.5 mm in diameter. By applying the overlay agarose containing C. burnetii to a higher-density (0.25%) agarose base, a stable matrix is achieved that allows handling of plates with minimal disruption of the overlay medium. We are uncertain why C. burnetii colonies are so small, but potential explanations include the presence of a toxic component in the agarose or the release by C. burnetii of a metabolite that changes the microenvironment, such as a basic compound that neutralizes local pH, thereby inhibiting C. burnetii metabolism (14). Alternatively, the observation that colonies are primarily comprised of SCVs, a stationary-phase cell form, suggests that the agarose immediately adjacent to colonies has been depleted of nutrients. Despite the colonies' small size, C. burnetii displays a nearly one-genome-per-colony plating efficiency in ACCM-2 agarose, indicating that a conventional CFU assay can be used to accurately assess C. burnetii viability.
Approximately 6 GE of avirulent C. burnetii in phase II is required to produce one infectious focus-forming unit (FFU) in Vero cells (8). In contrast, roughly 300 GE of virulent C. burnetii in phase I is required to produce a single FFU (R. A. Heinzen, unpublished data). This behavior is attributed to the hydrophilic nature of phase I C. burnetii, conferred by O-antigen sugars, which nonspecifically inhibit host cell plasma membrane interactions relative to hydrophobic phase II organisms, with a truncated lipopolysaccharide (LPS) (28). The low infectivity of virulent phase I C. burnetii for cell culture likely lowers the success rate of primary isolation using tissue culture systems. Here, we demonstrate that mouse tissue samples containing as little as 10 NMII GE can initiate cultures in ACCM-2. Thus, axenic culture in ACCM-2 should provide a sensitive method for isolating virulent C. burnetii in clinical samples. Indeed, recent large Q fever outbreaks in Europe (12, 26) reinforce the need for such an enhanced surveillance and diagnostic tool.
ACKNOWLEDGMENTS
We thank Gary Hettrick and Anita Mora for graphic support.
This work was supported by the Intramural Research Program of the National Institutes of Health, National Institute of Allergy and Infectious Diseases (to R.A.H.), and by Public Health Service grants RO1AI037744, R21AI088430, and R56AI090142-01 from the National Institute of Allergy and Infectious Diseases (to J.E.S.).
Footnotes
Published ahead of print on 8 April 2011.
REFERENCES
- 1. Andoh M., Russell-Lodrigue K. E., Zhang G., Samuel J. E. 2005. Comparative virulence of phase I and II Coxiella burnetii in immunodeficient mice. Ann. N. Y. Acad. Sci. 1063:167–170 [DOI] [PubMed] [Google Scholar]
- 2. Bardill J. P., Miller J. L., Vogel J. P. 2005. IcmS-dependent translocation of SdeA into macrophages by the Legionella pneumophila type IV secretion system. Mol. Microbiol. 56:90–103 [DOI] [PubMed] [Google Scholar]
- 3. Beare P. A., et al. 2009. Characterization of a Coxiella burnetii ftsZ mutant generated by Himar1 transposon mutagenesis. J. Bacteriol. 191:1369–1381 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Beare P. A., Omsland A., Cockrell D. C., Howe D., Heinzen R. A. 2010. Expansion of the Coxiella burnetii genetics tool box using axenic culture. Abstr. 24th Meet. Am. Soc. Rickettsiol., abstr. 94 [Google Scholar]
- 5. Beare P. A., et al. 2009. Comparative genomics reveal extensive transposon-mediated genomic plasticity and diversity among potential effector proteins within the genus Coxiella. Infect. Immun. 77:642–656 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Brennan R. E., Samuel J. E. 2003. Evaluation of Coxiella burnetii antibiotic susceptibilities by real-time PCR assay. J. Clin. Microbiol. 41:1869–1874 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Chen C., et al. 2010. Large-scale identification and translocation of type IV secretion substrates by Coxiella burnetii. Proc. Natl. Acad. Sci. U. S. A. 107:21755–21760 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Cockrell D. C., Beare P. A., Fischer E. R., Howe D., Heinzen R. A. 2008. A method for purifying obligate intracellular Coxiella burnetii that employs digitonin lysis of host cells. J. Microbiol. Methods 72:321–325 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Coleman S. A., et al. 2007. Proteome and antigen profiling of Coxiella burnetii developmental forms. Infect. Immun. 75:290–298 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Coleman S. A., Fischer E. R., Howe D., Mead D. J., Heinzen R. A. 2004. Temporal analysis of Coxiella burnetii morphological differentiation. J. Bacteriol. 186:7344–7352 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Frohlich B. T., et al. 1996. Formation and cell-medium partitioning of autoinhibitory free fatty acids and cyclodextrin's effect in the cultivation of Bordetella pertussis. J. Biotechnol. 45:137–148 [DOI] [PubMed] [Google Scholar]
- 12. Gilsdorf A., et al. 2008. Large Q fever outbreak due to sheep farming near residential areas, Germany, 2005. Epidemiol. Infect. 136:1084–1087 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Gouriet F., Fenollar F., Patrice J. Y., Drancourt M., Raoult D. 2005. Use of shell-vial cell culture assay for isolation of bacteria from clinical specimens: 13 years of experience. J. Clin. Microbiol. 43:4993–5002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Hackstadt T., Williams J. C. 1981. Biochemical stratagem for obligate parasitism of eukaryotic cells by Coxiella burnetii. Proc. Natl. Acad. Sci. U. S. A. 78:3240–3244 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Howe D., Melnicakova J., Barak I., Heinzen R. A. 2003. Maturation of the Coxiella burnetii parasitophorous vacuole requires bacterial protein synthesis but not replication. Cell. Microbiol. 5:469–480 [DOI] [PubMed] [Google Scholar]
- 16. Howe D., Shannon J. G., Winfree S., Dorward D. W., Heinzen R. A. 2010. Coxiella burnetii phase I and II variants replicate with similar kinetics in degradative phagolysosome-like compartments of human macrophages. Infect. Immun. 78:3465–3474 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Imaizumi A., Suzuki Y., Ono S., Sato H., Sato Y. 1983. Heptakis(2,6-O-dimethyl)beta-cyclodextrin: a novel growth stimulant for Bordetella pertussis phase I. J. Clin. Microbiol. 17:781–786 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Luhrmann A., Roy C. R. 2007. Coxiella burnetii inhibits activation of host cell apoptosis through a mechanism that involves preventing cytochrome c release from mitochondria. Infect. Immun. 75:5282–5290 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Marchini A., et al. 1995. Cyclodextrins for growth of Helicobacter pylori and production of vacuolating cytotoxin. Arch. Microbiol. 164:290–293 [DOI] [PubMed] [Google Scholar]
- 20. Maurin M., Raoult D. 1999. Q fever. Clin. Microbiol. Rev. 12:518–553 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Moos A., Hackstadt T. 1987. Comparative virulence of intra- and interstrain lipopolysaccharide variants of Coxiella burnetii in the guinea pig model. Infect. Immun. 55:1144–1150 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Omsland A., et al. 2009. Host cell-free growth of the Q fever bacterium Coxiella burnetii. Proc. Natl. Acad. Sci. U. S. A. 106:4430–4434 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Read A. J., Erickson S., Harmsen A. G. 2010. Role of CD4+ and CD8+ T cells in clearance of primary pulmonary infection with Coxiella burnetii. Infect. Immun. 78:3019–3026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Romano P. S., Gutierrez M. G., Beron W., Rabinovitch M., Colombo M. I. 2007. The autophagic pathway is actively modulated by phase II Coxiella burnetii to efficiently replicate in the host cell. Cell. Microbiol. 9:891–909 [DOI] [PubMed] [Google Scholar]
- 25. Russell-Lodrigue K. E., et al. 2009. Coxiella burnetii isolates cause genogroup-specific virulence in mouse and guinea pig models of acute Q fever. Infect. Immun. 77:5640–5650 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Schimmer B., et al. 2009. Sustained intensive transmission of Q fever in the south of the Netherlands, 2009. Euro Surveill. 14:19210. [DOI] [PubMed] [Google Scholar]
- 27. Spyridaki I., Gikas A., Kofteridis D., Psaroulaki A., Tselentis Y. 1998. Q fever in the Greek island of Crete: detection, isolation, and molecular identification of eight strains of Coxiella burnetii from clinical samples. J. Clin. Microbiol. 36:2063–2067 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Voth D. E., Heinzen R. A. 2007. Lounging in a lysosome: the intracellular lifestyle of Coxiella burnetii. Cell. Microbiol. 9:829–840 [DOI] [PubMed] [Google Scholar]
- 29. Voth D. E., Howe D., Heinzen R. A. 2007. Coxiella burnetii inhibits apoptosis in human THP-1 cells and monkey primary alveolar macrophages. Infect. Immun. 75:4263–4271 [DOI] [PMC free article] [PubMed] [Google Scholar]