Abstract
Widened perivascular spaces known as Virchow-Robin spaces (VRS) are often seen on MRI and are usually incidental findings. It is unclear if enlarged VRS can be associated with neurological deficits. In this report, we describe a case of lobar dementia associated with unusual VRS widening in one cerebral hemisphere. A 77-year-old woman, seen at a memory clinic, presented with progressive cognitive decline, left hemianopsia, and mild pyramidal signs on the left side. On MRI, unusually wide VRS were visible, predominantly in the right centrum semiovale and the right temporo-occipital white matter. The clinical syndrome was consistent with the extent and location of the abnormally dilated VRS. The high MR signal in white matter bridges between the VRS suggested parenchymal damage, possibly representing gliotic white matter. No evidence for another etiology was found on cerebral MRI and rCBF SPECT. As a conclusion, enlarged VRS in one cerebral hemisphere may be associated with cognitive change and neurological deficits.
Key Words: Virchow-Robin spaces, Lobar dementia, Magnetic resonance imaging
Introduction
Virchow-Robin spaces (VRS) are perivascular spaces that surround small arteries and arterioles as they enter the brain parenchyma. They are usually considered normal findings on MRI of healthy people [1]. In general, even patients with huge widening of VRS remain asymptomatic, as described in Mathias et al. [2]. However, in few patient reports, unusually broad VRS were associated with neurological symptoms thought to be caused by mass effect with or without obstructive hydrocephalus [3, 4]. In some cases, surgical removal of giant VRS provided neurological improvement. Here, we describe clinical and radiological findings supporting the hypothesis that in rare cases widening of VRS in one hemisphere can be associated with focal neurological and cognitive deficits.
Case Report
A 77-year-old woman presented with a 2-year history of cognitive decline and reading difficulties. The patient was unable to keep appointments or to manage her financial affairs and often lost topographical orientation. On the Informant Questionnaire on Cognitive Decline in the Elderly, her mean score was 4.3, indicating considerable deterioration over the past 2 years. On Mini-Mental State Examination, her total score was 21/30. The patient's hearing was unimpaired, and the best-corrected visual acuity of each eye was 0.7. Further neuropsychological evaluation was performed using the Consortium to Establish a Registry for Alzheimer Disease-Neuropsychological Assessment Battery. The Trail Making Test A and B and the Stroop test were administered for better evaluation of executive function. The results showed marked deficits in memory, particularly figural memory, in visuoconstructive abilities and in spontaneous and adaptive cognitive flexibility.
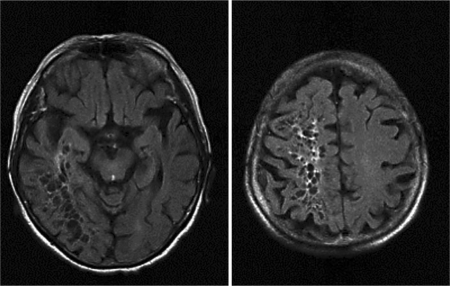
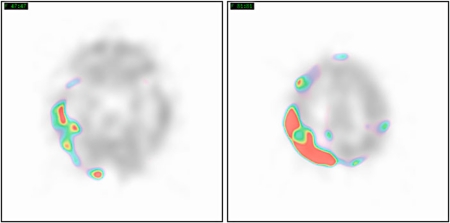
Neurological examination revealed a left homonymous hemianopsia and a pronator drift of the left arm. The clinical picture suggested a right posterior and mediotemporal cerebral lesion. On MRI, the right temporo-occipital and dorsal centroparietal white matter was replaced by innumerable large holes of up to 10 mm in diameter (fig. 1). On FLAIR images, hyperintense signal changes were observed between the cystic spaces, most likely representing narrow bridges of gliotic white matter. Regional cerebral blood flow (rCBF) SPECT revealed regions of hypoperfusion in the areas with the enlarged VRS (fig. 2). The hippocampi appeared normal in size (fig. 3). There was no evidence for a mass effect or a neurodegenerative, vascular, metabolic or inflammatory disorder, as evaluated by blood tests and brain imaging.
Fig. 1.
MR FLAIR images show dilated VRS in the right temporo-occipital white matter and the right centrum semiovale. Note the hyperintense signal in white matter bridges between the cavities.
Fig. 2.
rCBF SPECT reveals extended areas of hypoperfusion in the right parietal and right temporo-occipital grey matter.
Fig. 3.
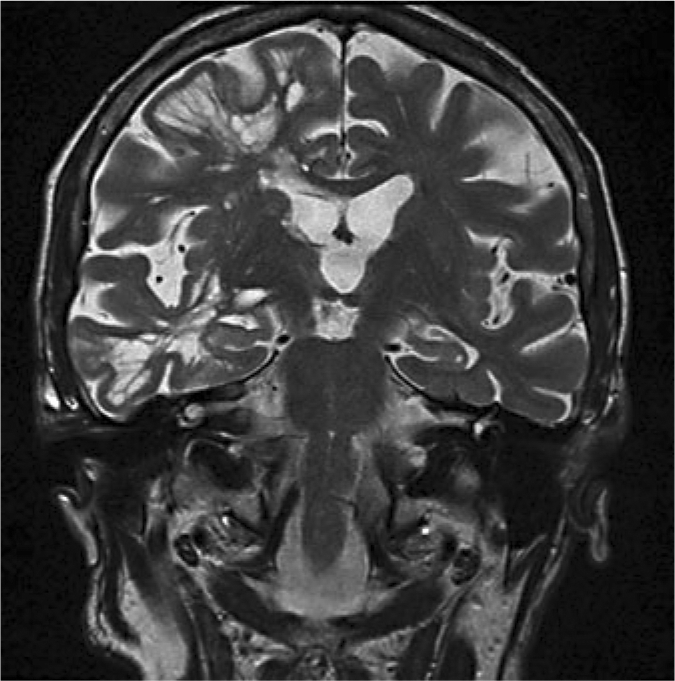
Coronal MR T2-weighted image displays regular-sized hippocampi, extreme widening of VRS in the areas of the right temporal and frontal lobe and an enlarged right insular cistern.
Three months later, depressed mood and irritability led to the patient's admission to a psychiatric hospital. As an inpatient, she developed an acute confusional state triggered by bronchopneumonia. She recovered slowly from delirium. However, because of persistent impairment of cognitive functions and activities of daily living, the patient was admitted to a nursing home.
Discussion
To the best of our knowledge, this case is the first to describe a link between lobar type of dementia and dilated VRS in one cerebral hemisphere. The differential diagnosis of hemianopsia and focal dementia includes posterior cortical atrophy (PCA), multi-infarct dementia and the visual variant of Creutzfeldt-Jakob disease. However, no cortical atrophy, territorial infarction or DWI signal alterations are visible on MRI. The absence of cortical atrophy and the co-localization of hypoperfusion with extremely widened VRS revealed by SPECT speak against a diagnosis of PCA. In addition, the long duration of symptoms, the absence of cerebellar and extrapyramidal signs, and the lack of cortical DWI and deep gray matter abnormalities on MRI make a diagnosis of Creutzfeldt-Jakob disease unlikely. The congruence between the focal neurological and cognitive findings and the distribution of abnormal VRS suggests a causal relationship.
Vital and Julien [5] reported the case of a patient with early-onset dementia and widespread dilatation of perivascular spaces in both cerebral hemispheres. Routine CSF analysis was normal, and there were no signs of brain atrophy or ischemic brain lesions on MRI. Autopsy material from the subcortical white matter revealed fibrosis of some small blood vessels and widened VRS. The white matter adjacent to the dilated VRS was of normal histological appearance. The authors considered enlarged VRS as a new form of vascular leukoencephalopathy. However, the mechanism of VRS enlargement in their case remained unknown. In particular, there was no evidence for an ischemic or hemorrhagic origin of the lesions.
The function of VRS is not well known. Detection of immunocompetent cells in VRS and physiological experiments examining the pathway of tracers injected into the interstitial fluid of rat brains point to an immunological function of VRS and to their impact on bulk flow and interstitial fluid drainage [1, 6].
Several mechanisms underlying the dilatation of VRS have been discussed, among them changes in the vascular permeability, shrinkage of cerebral tissue or vascular ectasia [7]. In our patient, extreme widening of VRS may well have resulted from an ‘ex vacuo effect’ due to a local white matter pathology, as suggested by the hyperintense MR signal in the spaces between the VRS. The lesion probably occurred late in the life of the patient, as indicated by her clinical history.
The clinical significance of dilated VRS in vascular disorders and dementia has to be clarified. The prevalence of dilated VRS seems to increase in elderly people as well as in patients with small vessel disease [1, 5, 8, 9, 10], but an independent statistical association between dilated VRS and cognitive impairment has not been found [11, 12].
Nevertheless, our report indicates that largely dilated VRS should be included in the differential diagnosis of dementia. In case of enlarged VRS in a patient with lobar dementia, the topographical distribution should be carefully studied in order to link the neurological syndrome to VRS.
Limitations of this study are the lack of a CSF examination and necropsy results. The patient, who is still alive, did not agree to undergo lumbar puncture. Therefore, atypical Alzheimer's disease or other neurodegenerative disorders that can underlie PCA, such as dementia with Lewy bodies and corticobasal degeneration, cannot be ruled out.
References
- 1.Groeschel S, Chong WK, Surtees R, Hanefeld F. Virchow-Robin spaces on magnetic resonance images: normative data, their dilatation, and a review of the literature. Neuroradiology. 2006;48:745–754. doi: 10.1007/s00234-006-0112-1. [DOI] [PubMed] [Google Scholar]
- 2.Mathias J, Koessler L, Brissart H, Foscolo S, Schmitt E, Bracard S, Braun M, Kremer S. Giant cystic widening of Virchow-Robin spaces: an anatomofunctional study. AJNR Am J Neuroradiol. 2007;28:1523–1525. doi: 10.3174/ajnr.A0622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.House P, Salzman KL, Osborn AG, MacDonald JD, Jensen RL, Couldwell WT. Surgical considerations regarding giant dilatations of the perivascular spaces. J Neurosurg. 2004;100:820–824. doi: 10.3171/jns.2004.100.5.0820. [DOI] [PubMed] [Google Scholar]
- 4.Marnet D, Noudel R, Peruzzi P, Bazin A, Bernard MH, Scherpereel B, Pluot M, Rousseaux P. Dilatation des espaces périvasculaires de Virchow-Robin (Lacunes de type III): corrélations radio-cliniques. Rev Neurol (Paris) 2007;163:561–571. doi: 10.1016/s0035-3787(07)90462-2. [DOI] [PubMed] [Google Scholar]
- 5.Vital C, Julien J. Widespread dilatation of perivascular spaces: a leukoencephalopathy causing dementia. Neurology. 1997;48:1310–1313. doi: 10.1212/wnl.48.5.1310. [DOI] [PubMed] [Google Scholar]
- 6.Zhang ET, Inman CB, Weller RO. Interrelationships of the pia mater and the perivascular (Virchow-Robin) spaces in the human cerebrum. J Anat. 1990;170:111–123. [PMC free article] [PubMed] [Google Scholar]
- 7.Ogawa T, Okudera T, Fukasawa, Hashimoto M, Inugami A, Fujita H, Hatazawa J, Shimosegawa E, Noguchi K, Uemura K, Nakajima S, Yasui N. Unusual widening of Virchow-Robin spaces: MR appearance. AJNR Am J Neuroradiol. 1995;16:1238–1242. [PMC free article] [PubMed] [Google Scholar]
- 8.Patankar TF, Mitra D, Varma A, Snowden J, Neary D, Jackson A. Dilatation of the Virchow-Robin space is a sensitive indicator of cerebral microvascular disease: study in elderly patients with dementia. AJNR Am J Neuroradiol. 2005;26:1512–1520. [PMC free article] [PubMed] [Google Scholar]
- 9.Cumurciuc R, Guichard JP, Reizine D, Gray F, Bousser MG, Chabriat H. Dilatation of Virchow-Robin spaces in CADASIL. Eur J Neurol. 2006;13:187–190. doi: 10.1111/j.1468-1331.2006.01113.x. [DOI] [PubMed] [Google Scholar]
- 10.Rouhl RPW, van Oostenbrugge RJ, Knottnerus ILH, Staals JEA, Lodder J. Virchow-Robin spaces relate to cerebral small vessel disease severity. J Neurol. 2008;255:692–696. doi: 10.1007/s00415-008-0777-y. [DOI] [PubMed] [Google Scholar]
- 11.Heier LA, Bauer CJ, Schwartz L, Zimmerman RD, Morgello S, Deck MDF. Large Virchow-Robin spaces: MR-clinical correlation. AJNR Am J Neuroradiol. 1989;10:929–936. [PMC free article] [PubMed] [Google Scholar]
- 12.MacLullich AMJ, Wardlaw JM, Ferguson KJ, Starr JM, Seckl JR, Deary IJ. Enlarged perivascular spaces are associated with cognitive function in healthy elderly men. J Neurol Neurosurg Psychiatry. 2004;75:1519–1523. doi: 10.1136/jnnp.2003.030858. [DOI] [PMC free article] [PubMed] [Google Scholar]