Abstract
Background
It is unclear whether anti-tumour necrosis factor alpha and biological agents with different mechanisms of action have similar safety. This study evaluated the incidence of hospitalised infections among rheumatoid arthritis (RA) patients starting or switching various biological agents.
Methods
Using a database from a large US healthcare organisation from January 2005 to August 2009, the authors identified enrollees with RA and their treatment episodes entailing the new use of a biological agent, stratified by no biological use in the previous year (‘biological-free’) or switching from a different biological agent (‘switchers’). Outcomes were hospitalised infections identified using previously validated algorithms. Proportional hazards models estimated the hazard ratio of hospitalised infections, comparing each biological agent with infliximab.
Results
Among 7847 biological treatment episodes, 63% were for biological-free patients and 37% for switchers. There were 364 hospitalised infections. Rates of hospitalised infection among biological-free patients and switchers were 4.6 and 7.0 per 100 person-years, respectively (p<0.0001). After multivariable adjustment controlling for biological-free/switcher status and other infection-related factors and compared with infliximab, users of abatacept (HR 0.68, 95% CI 0.48 to 0.96), adalimumab (HR 0.52, 0.39 to 0.71), etanercept (HR 0.64, 0.49 to 0.84) and rituximab (HR 0.81, 0.55 to 1.20) had lower rates of hospitalised infection. Patient risk factors contributed more to the risk of infection than did the risk associated with specific biological therapies.
Conclusion
The rate of hospitalised infections among RA patients was highest for infliximab. Most of the variability in patients’ risk of infection was driven by factors other than biological agent exposure.
Numerous factors contribute to the decision to choose biological agents for the treatment of rheumatoid arthritis (RA). Appropriately powered randomised studies directly comparing biological agents are lacking, but for the average patient, the tumour necrosis factor alpha antagonist (anti-TNF) agents are thought to have efficacy that is relatively comparable to one another and perhaps to other biological therapies with different mechanisms of action.1-4 Given efficacy that many consider relatively comparable, other considerations such as safety may be important in choosing among the biological agents for an individual patient.
Some previous reports have suggested that anti-TNF therapies may differ in their respective safety profiles.5-8 A relatively small trial comparing abatacept and infliximab suggested safety-related differences between these two agents.9 Few other data exist with which to compare the anti-TNF biological agents with newer agents including abatacept and rituximab. One potentially confounding factor is that most patients receive these biological agents with non-tumour necrosis factor alpha mechanisms of action only after failing one or more anti-TNF therapies, consistent with some national guidelines.10 Generally, these more refractory patients are thought to be at higher risk of serious infections due to their age, comorbidities or concomitant therapies such as glucocorticoid use. However, current knowledge is inadequate to determine whether patients who switch biological therapies might be at higher risk of infections compared with those who are biological agent naive.
In light of these evidence gaps, we evaluated the drug-specific absolute and relative incidence of hospitalised bacterial infections among RA patients. We compared the individual biological agents with one another, and also compared the patients starting these agents who were free of recent biological exposure with those who were switching from one biological agent to another. Finally, because of uncertainty regarding physicians’ comfort with restarting the same or a different biological agent after a hospitalised infection, we descriptively characterised whether patients were started on the same or a different biological agent in the 6 months after a hospitalised infection.
METHODS
Eligible patient population and observation period
We used the administrative medical and pharmacy databases of Aetna, one of the largest health insurers in the USA that provides medical and/or pharmacy benefits to more than 18 million individuals through numerous employer sponsored and individual plans. We identified RA patients on the basis of International Classification of Disease, 9th Edition (ICD-9) codes. Patients were eligible to be under observation after they had at least two ICD-9 codes for RA (ICD-9 714.X) from a physician office visit separated by over 7 days and occurring within 1 year, or with one or more physician RA diagnosis code followed by a prescription for methotrexate or a biological agent. Patients with malignancy (excluding non-melanoma skin cancer) were excluded.
After meeting eligibility criteria, patients must also have had at least one prescription or infusion for an anti-TNF or non-anti-TNF biological agent that they had not received in the preceding 12 months, consistent with a new user design.11 The date of the biological prescription/infusion defined the ‘index date’ and began a new treatment episode. Patients must have had medical and pharmacy benefits in the 12 months before the index date and throughout follow-up. Individuals aged 65 years and older were included only if they were enrolled in the health plan through Medicare Advantage (with a pharmacy benefit). Any other type of health plan coverage (eg, commercial) for these older individuals is often a secondary, concomitant payor to governmental insurance (ie, Medicare), and enrollees’ claims profile in the health plan data may be incomplete. The 12-month ‘baseline’ period was used for covariate assessment for all non-time-varying covariates.
Biological exposures
At the start of each new treatment episode, patients were assigned into one of several biological exposure groups, which included infliximab, etanercept, adalimumab, abatacept and rituximab. The use of golimumab or certolisumab was insufficient to study these agents. We classified patients as ‘biological-free’, if they had no exposure to any biological medication in the preceding 1 year baseline period, or as ‘switchers’ if they had received a different biological agent in the baseline period. Because of left censoring, some biological-free patients may have received a biological agent even before the baseline period and thus might not be truly ‘biological-naive’.
Exposure was defined as the current use of the biological agent. We specified days of exposure for injectable biological agents as the days supply plus a 90-day ‘extension’ period. The extension was added because patients who become ill often stop medications, and using an extension may capture exposure relevant to outcomes.12 For infused drugs, in which days supply is inapplicable, we assigned days of exposure as 30 days to abatacept, 180 days to rituximab and 56 days to infliximab; the same 90-day extension was added to each. As part of a sensitivity analysis, we shortened this extension to 30 days.
Outcome of interest
The outcome of interest was the first hospitalisation with at least one infection. We identified infections using a comprehensive set of ICD-9 codes developed as part of a systematic literature review and two validation studies in RA patients. The validation studies compared cases identified using these codes with cases confirmed using hospital medical records abstracted across the USA13 and with cases confirmed by abstracting records from a university hospital.14
Controlling for confounders through an infection risk score
To control for confounding, we derived and validated an infection-specific disease risk score. A disease risk score15 allows for multivariable reduction into a single composite measure, and is similar to a propensity score16,17 except that it models the risk for the outcome rather than the risk for exposure. The WHO FRAX calculator18 and several well-known cardiovascular risk calculators (eg, Framingham)19 are examples of disease risk scores. Disease risk scores achieve similar control for confounding compared with traditional multivariable adjustment, but are more efficient when outcome data are sparse. The infection risk score was used to control for infection-related confounding for all factors unrelated to biological therapy and biological-free/switcher status by computing a predicted infection score for each subject (see supplementary appendix).
Statistical analysis and covariate selection
For each treatment episode, patients were censored at the time of their first hospitalised infection, after they stopped taking the biological medication, lost medical or pharmacy benefits in the health plan (which would impede ascertaining their exposures and outcomes), started a new biological treatment episode or reached the end of the study. The study period was 1 January 2005 to 31 August 2009. The characteristics of the patients contributing biological-free and switch treatment episodes were compared. We used Cox proportional hazards models to estimate the adjusted hazard risk (HR) of infection. We used infliximab as the reference exposure group because it had sufficient data to serve as the comparator group for both the biological-free and switcher subcohorts. A sensitivity analysis used etanercept as the referent. The Cox models were stratified by biological-free versus switcher status, allowing the baseline infection hazard for these two groups to differ while still providing a combined HR. The proportional hazards assumption was verified using the SAS statement ASSESS to inspect the martingale residuals visually over the follow-up time. Control for confounding was achieved through adjustment for the infection risk score, modelled in quintiles. In a sensitivity analysis, we controlled for the infection risk score in deciles. Additional sensitivity analyses censored all observation time at 6 months and at 12 months, in order to account for the possibility that the risk of infection varied between agents over time.
In order to describe the discrimination of the statistical models in relation to the contribution of patients’ infection risk score and their biological use, we calculated concordance probabilities from the Cox models.20 Concordance probabilities are similar to an area under the receiver-operator curve and allow for estimation of the incremental discrimination of adding variables to a statistical model, similar to a change in a c statistic.
Finally, we identified all biological-treated patients who developed a hospitalised infection and had at least 6 months of follow-up in the health plan after hospital discharge. Over that 6-month period, we described the cumulative proportion of people who restarted the same biological agent and those who changed to a different biological agent. Analyses were performed using SAS version 9.2. The study was approved by the university institutional review board.
RESULTS
A total of 4916 treatment episodes occurred among biological-free patients, and an additional 2931 treatment episodes occurred in biological switchers. The mean age of the biological-free and switcher groups was 49 years, and three-quarters were women (table 1). A total of 823 patients was represented in both the biological-free cohort (17.0% of cohort) and the switcher cohort (38.9% of cohort). Fewer than 1% of patients over the age of 65 years were censored due to not being fully observable in the health plan. Compared with biological-free patients, switchers were more likely to have comorbidities such as chronic obstructive pulmonary disease and diabetes, to use narcotics and to use prednisone and at higher doses. Most of the abatacept and rituximab treatment episodes were assigned to the switcher group.
Table 1.
| Biological-free (N=4916) |
Switcher (N=2931) |
|
|---|---|---|
| Unique patients (n) | 4874 | 2118 |
| Age (years) | 49.5±11.6 | 49.2±11.0 |
| Female (%) | 75.8 | 76.9 |
| COPD (%) | 12.9 | 15.7 |
| Peptic ulcer disease (%) | 0.9 | 1.6 |
| Diabetes (%) | 8.8 | 10.9 |
| Charlson comorbidity score | 0.4±0.8 | 0.4±0.8 |
| Mammography (%) | 24.3 | 26.6 |
| Any rheumatoid factor laboratory test (%) | 50.4 | 36.0 |
| Any hospital infection (%) | 6.8 | 9.9 |
| Any non-infection hospitalisation (%) | 28.1 | 31.6 |
| Any outpatient infection (%) | 39.8 | 47.8 |
| No of outpatient visits | 12.1±7.2 | 15.0±8.5 |
| Biological agent initiated (%) | ||
| Abatacept | 6.5 | 20.8 |
| Adalimumab | 30.4 | 29.2 |
| Etanercept | 39.0 | 19.4 |
| Infliximab | 20.8 | 17.9 |
| Rituximab | 3.3 | 12.6 |
| Narcotic use (%) | 59.7 | 70.3 |
| Prednisone (mg/day) | ||
| None | 47.3 | 40.9 |
| Low (<5) | 36.8 | 33.2 |
| Medium (5–10) | 10.9 | 14.0 |
| Moderate to high (>10) | 5.0 | 12.0 |
Measured in the 1-year baseline period.
A treatment episode is defined as new use of a biological agent with no use of that specific medication in the preceding year. A treatment episode continued until the patient experienced an infection, stopped taking the medication (plus a 90-day extension), became unobservable in the health plan data because of loss of medical or pharmacy benefits or reached the end of the study.
Biological-free means no use of any biological agent in the preceding year. Switcher means use of a different biological agent in the preceding year.
COPD, chronic obstructive pulmonary disease.
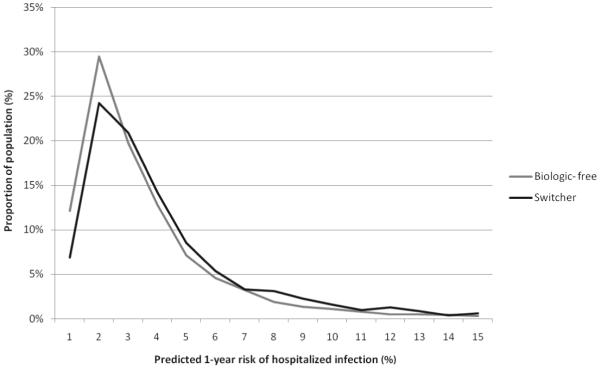
Using the infection risk score, we estimated for each biological-treated patient contributing to the analysis the 1-year predicted risk of a hospitalised infection associated with components included in the infection risk score (which did not include biological agent use). As shown in figure 1, the 1-year predicted risk for hospitalisation with infection due to patient factors (and independent of biological agent use) varied across a wide range. In addition, the switcher group had a somewhat higher predicted risk of infection than the biological-free group (mean prediction infection risk score 4.2% vs 5.2%, p<0.0001).
Figure 1.
Distribution of predicted infection risk among biological-free versus switchers. The x-axis is the 1-year predicted risk of hospitalised infection, expressed as a percentage ranging from 0 to 100. The y-axis is the cumulative distribution of infection risk in the biological-free and switcher groups; the area under each of the two curves sums to 100%, representing all patients in that group. The x-axis was right-truncated at 15% to facilitate visual inspection; 97% of the biological-free patients had a predicted 1-year infection risk of 15% or less; 94% of the switcher patients had a predicted 1-year infection risk of 15% or less.
After applying censoring criteria, including censoring patients once they stopped taking the biological agent, the median (IQR) follow-up was 7.7 months (4.0–14.1) after the index date; the median (IQR) follow-up was slightly greater among the biological-free patients (8.4 months (4.3–15.4), 4611 person-years of exposure) than for the switcher group (6.6 months (3.4–12.1), 2205 person-years of exposure). A total of 364 unique hospitalisations with at least one infection occurred. The site and type of infections are shown in table 2. Pneumonia, skin and soft tissue and septicemia were the most common types of infections.
Table 2.
Type and number of hospitalised infections experienced by biological agent users (n=364 unique hospitalisations)*
| Site/type of infection | n (%) |
|---|---|
| Pneumonia | 124 (23.7) |
| Skin and soft tissue infection | 90 (17.2) |
| Septicaemia/bacteraemia | 87 (16.6) |
| Genitourinary tract infection | 83 (15.8) |
| Upper respiratory tract infection | 41 (7.8) |
| Abdominal abscess | 22 (4.2) |
| Gastroenteritis | 16 (3.1) |
| Device-associated infections | 11 (2.1) |
| Septic arthritis | 10 (1.9) |
|
†Aspergillosis (1), coccidioidomycosis (1), cryptococcosis (1), endemic mycosis (1), histoplasmosis (3), legionellosis (2), nocardiosis actinomycosis (1), non-tuberculosis mycobacteria (1), toxoplasmosis (1), tuberculosis (5), zoster (6) |
23 (4.4) |
| Other, including encephalitis, endocarditis, osteomyelitis, meningitis | 17 (3.2) |
Data were combined for the biological-free and switcher groups given similar distributions of the types of infections.
More than one type of infection may occur during a hospitalisation.
Numbers in parentheses refer to the number of hospitalised infections of that specific type.
Overall, the mean rate of hospitalised infection among biological-free patients was 4.6 per 100 patient-years and was lower than the mean rate of infection for switchers (7.0 per 100 patient-years, p<0.0001 vs biological-free patients). The rate of infection for each specific biological agent was consistently one to three per 100 person-years higher among the switcher versus the biological-free patients except for rituximab. Among rituximab users, the rate of hospitalised infection was 10.4 (6.3, 17.2) among biological-free patients and 7.1 (4.6, 10.9) among switchers.
The main results of the study are described in figure 2 and table 3. Compared with infliximab and after adjusting for the infection risk score, the rate of infection was significantly lower for most other drugs (figure 2) in both the biological-free and switcher subcohorts. The combined HR shown in figure 2 that pooled results for the biological-free and switcher cohorts are shown numerically in table 3. The differences in the HR yielded much smaller differences in the absolute rate of infection for low-risk patients compared with high-risk patients. For example, among low-risk biological-free patients and comparing infliximab with adalimumab users (combined HR 0.52), there was a −2.1 per 100 person-years lower rate of infections among adalimumab users for low-risk patients and a −8.2 per 100 patient-years difference for high-risk patients. The quintile of the predicted infection risk score had a strong dose-dependent relationship with the rate of infection (bottom half of table 3). Indeed, the HR associated with the infection risk score were much greater in magnitude than the differences between the biological agents.
Figure 2.
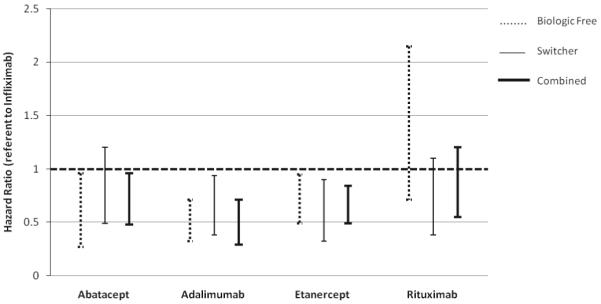
Adjusted* HR of hospitalised infection for biological-free, switcher and combined cohorts, compared with infliximab. *Adjusted for quintile of the infection risk score, described in the supplementary appendix (available online only).
Table 3.
Multivariable adjusted* rates of hospitalised infection and associated rate differences for biological-free low and high-risk patient subgroups
| Infection rate difference† compared with infliximab among biological-free patients (rate per 100 patient-years) |
|||
|---|---|---|---|
| Adjusted* HR (95% CI) | Low‡ baseline infection risk | High‡ baseline infection risk | |
| Infliximab | 1.0 (referent) | Referent | Referent |
| Abatacept | 0.68 (0.48 to 0.96) | −1.5 | −7.9 |
| Adalimumab | 0.52 (0.39 to 0.71) | −2.1 | −8.2 |
| Etanercept | 0.64 (0.49 to 0.84) | −1.3 | −5.4 |
| Rituximab | 0.81 (0.55 to 1.20) | −0.8 | 6.4 |
| Infection risk score | |||
| Quintile 1 | 1.0 (referent) | ||
| Quintile 2 | 1.19 (0.73 to 1.92) | ||
| Quintile 3 | 2.04 (1.31 to 3.18) | ||
| Quintile 4 | 3.08 (2.03 to 4.67) | ||
| Quintile 5 | 5.28 (3.54 to 7.88) | ||
Results were adjusted for biological-free vs switcher status and quintile of the infection risk score. The infection risk score included factors associated with infection as described in the supplementary appendix. The HR in this column reflect the same results as the ‘Combined’ results in figure 2.).
Negative numbers indicate a rate that is lower than the rate for infliximab.
Low and high baseline infection risk was defined as patients with a predicted infection risk below and above 5.2 per 100 patient-years, respectively.
The results of the sensitivity analyses for table 3 that defined current use with a 30-day extension period and of the analysis that controlled for the infection risk score in deciles were similar to the primary results (data not shown). Additional sensitivity analyses that censored patients at 6 months and at 12 months yielded similar magnitude HR and statistical significance to the primary results. In the sensitivity analysis that used etanercept rather than infliximab as the referent group in the adjusted Cox models, there was no significant difference in the rate of infection between etanercept and any of the other biological agents except for infliximab.
The concordance probability for infection including only the predicted infection risk score and biological-free/switcher status in the model was 0.67; after adding the specific biological drugs to the model, it increased minimally to 0.68. In contrast, the concordance probability with only the specific biological drugs and biological-free/switcher status in the model was 0.59.
Among the 240 patients with a hospitalised infection who had at least 6 months of follow-up, a majority of patients (69.2%) were re-started on the same biological agent within 6 months and did not switch biological agents. An additional 6.7% of patients restarted the same biological agent but switched within 6 months to a different agent. Ten per cent of patients switched to a different biological agent within 6 months after hospital discharge, and the remaining 14.2% of patients did not use any biological agent. Data were insufficient to characterise the risk for subsequent hospitalised infection after re-starting or changing biological therapy.
DISCUSSION
In this analysis of RA patients enrolled in a large US health plan, the rate of hospitalised infections for specific biological agents varied across a relatively small range. Patients switching biological agents had an increased rate of infection in the range of one to three per 100 patient-years compared with those not receiving biologic agents in the previous 12 months. The rate of hospitalised infections for patients treated with infliximab was higher than for other agents. However, to put these findings into context, patient characteristics that were part of the infection risk score contributed to much wider variability in the rate of serious infections than the risk associated with specific biological drugs.
A substantial body of literature supports a modest increase in the risk of serious infection for patients treated with anti-TNF agents compared with non-biological disease-modifying antirheumatic drugs (DMARD).21-23 The rate of infections for biological-treated patients compared with those receiving non-biological DMARD reported in past studies is typically a difference of one to three per 100 person-years. We found rate differences similar to this magnitude for patients switching to a new biological agent. A higher infection risk among infliximab users compared with some other anti-TNF therapies has previously been observed(5), although may be most different for opportunistic infections (6–8). Consistent with earlier findings,24 pneumonia and soft tissue infections were the most common infections observed in our cohort.
The clinical importance of RR in the range of approximately 0.5–0.8, as we found in table 3, is a matter of judgement. For patients at low risk of infection, this translates into a relatively small rate difference of approximately two per 100 patient-years. For patients at higher baseline infection risk, the magnitude of the rate difference is greater, in the range of five to eight per 100 patient-years. An earlier survey of the membership of the American College of Rheumatology suggested that rate differences less than six to eight per 100 person-years may not be very important to clinical decision-making.25 The magnitude of the incremental risk related to biological treatments compared with patients’ baseline infection risk may impact both patients and physicians’ perceptions of the risk of starting biological agents and should be examined prospectively in relation to treatment preferences for RA medications.
Our results provide useful information to put differences in the safety profiles of biological agents into context. The contribution of demographics, comorbidities and glucocorticoid use on infection risk (summarised as a single infection risk score) contributed substantially greater variability to infection risk compared with smaller differences in infection risk between individual biological agents. Similarly, the improvement in the discrimination of the infection risk model was substantial after adding the infection risk score, and was minimal after adding the biological agents. While some of these infection risk factors are not modifiable (eg, age), others might be to a variable extent (eg, glucocorticoid use, some comorbidities), and may offset any increased infection risk associated with use of specific biologics.
The strengths of our study include a large population of patients receiving care in a real-world setting. Unlike clinical trials and even some registries, patients were included in these safety-focused analyses irrespective of age or concomitant comorbidities. Despite these strengths, the results of our study must be interpreted in light of its design. Administrative data provide limited information on RA disease severity and comorbidity. This yields potential residual confounding. We also lacked hospital medical records to confirm the infections, although our claims-based algorithms have been validated in two large studies.13,14 We observed a modest number of outcome events for some exposures, especially for rituximab, which led to CI that were wider than for other agents. We also observed higher rates of infection for biological-free rituximab users, which probably reflects channelling of higher risk patients to this agent. Although we had a somewhat limited ability to examine risk in specific time windows after biological agent initiation,5,12 most of our follow-up time occurred within the first year after initiation, and sensitivity analyses that censored observation time at 6 or 12 months supported our primary findings. Finally, enrollees in the health plan were relatively young and healthy, and these results may not be generalisable to older patients or those with a higher burden of comorbidities.
In conclusion, we found wide variability in patients’ risk of serious infections related to demographics, comorbidities and other patient-specific factors, and much less variability related to the individual biological agent or switching patterns. A majority of patients were continued on the same biological therapy despite having been hospitalised with an infection, despite little information on the safety of this practice. More attention needs to be focused on patient-specific, potentially modifiable risk factors for infection such as glucocorticoid use and immunisations. The ultimate importance of perceived safety risks associated with biological agents in relation to patients’ other infection risk factors, and the impact of these perceptions on treatment selection, may be useful to examine in future studies.
Supplementary Material
Acknowledgments
Funding This work was supported by the Agency for Healthcare Research and Quality (R01HS018517) and the Doris Duke Charitable Foundation. Some of the investigators receive support from the National Institutes of Health (AR053351).
Footnotes
Ethics approval This study was conducted with the approval of the University of Alabama at Birmingham institutional review board.
Provenance and peer review Not commissioned; externally peer reviewed.
REFERENCES
- 1.Singh JA, Christensen R, Wells GA, et al. Biologics for rheumatoid arthritis: an overview of Cochrane reviews. Cochrane Database Syst Rev. 2009;4:CD007848. doi: 10.1002/14651858.CD007848.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Singh JA, Christensen R, Wells GA, et al. A network meta-analysis of randomized controlled trials of biologics for rheumatoid arthritis: a Cochrane overview. Can Med Assoc J. 2009;181:787–96. doi: 10.1503/cmaj.091391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bergman GJ, Hochberg MC, Boers M, et al. Indirect comparison of tocilizumab and other biologic agents in patients with rheumatoid arthritis and inadequate response to disease-modifying antirheumatic drugs. Semin Arthritis Rheum. 2010;39:425–41. doi: 10.1016/j.semarthrit.2009.12.002. [DOI] [PubMed] [Google Scholar]
- 4.Salliot C, Finckh A, Katchamart W, et al. Indirect comparisons of the efficacy of biological antirheumatic agents in rheumatoid arthritis in patients with an inadequate response to conventional disease-modifying antirheumatic drugs or to an anti-tumour necrosis factor agent: a meta-analysis. Ann Rheum Dis. 2011;70:266–71. doi: 10.1136/ard.2010.132134. [DOI] [PubMed] [Google Scholar]
- 5.Curtis JR, Xi J, Patkar N, et al. Drug-specific and time-dependent risks of bacterial infection among patients with rheumatoid arthritis who were exposed to tumor necrosis factor alpha antagonists. Arthritis Rheum. 2007;56:4226–7. doi: 10.1002/art.23050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tubach F, Salmon D, Ravaud P, et al. Research Axed on Tolerance of Biotherapies Group Risk of tuberculosis is higher with anti-tumor necrosis factor monoclonal antibody therapy than with soluble tumor necrosis factor receptor therapy: the three-year prospective French Research Axed on Tolerance of Biotherapies registry. Arthritis Rheum. 2009;60:1884–94. doi: 10.1002/art.24632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dixon WG, Hyrich KL, Watson KD, et al. BSRBR Control Centre Consortium. BSR Biologics Register Drug-specific risk of tuberculosis in patients with rheumatoid arthritis treated with anti-TNF therapy: results from the British Society for Rheumatology Biologics Register (BSRBR) Ann Rheum Dis. 2010;69:522–8. doi: 10.1136/ard.2009.118935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Salmon-Ceron D, Tubach F, Lortholary O, et al. Drug-specific risk of non-tuberculosis opportunistic infections in patients receiving anti-TNF therapy reported to the 3-year prospective French RATIO registry. Ann Rheum Dis. 2011;70:616–23. doi: 10.1136/ard.2010.137422. [DOI] [PubMed] [Google Scholar]
- 9.Schiff M, Keiserman M, Codding C, et al. Efficacy and safety of abatacept or infliximab vs placebo in ATTEST: a phase III, multi-centre, randomised, double-blind, placebo-controlled study in patients with rheumatoid arthritis and an inadequate response to methotrexate. Ann Rheum Dis. 2008;67:1096–103. doi: 10.1136/ard.2007.080002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Saag KG, Teng GG, Patkar NM, et al. American College of Rheumatology American College of Rheumatology 2008 recommendations for the use of nonbiologic and biologic disease-modifying antirheumatic drugs in rheumatoid arthritis. Arthritis Rheum. 2008;59:762–84. doi: 10.1002/art.23721. [DOI] [PubMed] [Google Scholar]
- 11.Ray WA. Evaluating medication effects outside of clinical trials: new-user designs. Am J Epidemiol. 2003;158:915–20. doi: 10.1093/aje/kwg231. [DOI] [PubMed] [Google Scholar]
- 12.Dixon WG, Symmons DP, Lunt M, et al. British Society for Rheumatology Biologics Register Control Centre Consortium. British Society for Rheumatology Biologics Register Serious infection following anti-tumor necrosis factor alpha therapy in patients with rheumatoid arthritis: lessons from interpreting data from observational studies. Arthritis Rheum. 2007;56:2896–904. doi: 10.1002/art.22808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Curtis JR, Patkar N, Xie A, et al. Risk of serious bacterial infections among rheumatoid arthritis patients exposed to tumor necrosis factor alpha antagonists. Arthritis Rheum. 2007;56:1125–33. doi: 10.1002/art.22504. [DOI] [PubMed] [Google Scholar]
- 14.Patkar NM, Curtis JR, Teng GG, et al. Administrative codes combined with medical records based criteria accurately identified bacterial infections among rheumatoid arthritis patients. J Clin Epidemiol. 2009;62:321–7. 327.e1–7. doi: 10.1016/j.jclinepi.2008.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Miettinen OS. Stratification by a multivariate confounder score. Am J Epidemiol. 1976;104:609–20. doi: 10.1093/oxfordjournals.aje.a112339. [DOI] [PubMed] [Google Scholar]
- 16.Cadarette SM, Gagne JJ, Solomon DH, et al. Confounder summary scores when comparing the effects of multiple drug exposures. Pharmacoepidemiol Drug Saf. 2010;19:2–9. doi: 10.1002/pds.1845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Stürmer T, Schneeweiss S, Brookhart MA, et al. Analytic strategies to adjust confounding using exposure propensity scores and disease risk scores: nonsteroidal antiinflammatory drugs and short-term mortality in the elderly. Am J Epidemiol. 2005;161:891–8. doi: 10.1093/aje/kwi106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.FRAX [accessed 31 May 2008];Welcome to FRAX. http://shef.ac.uk/FRAX.
- 19.Wilson PW, D’Agostino RB, Levy D, et al. Prediction of coronary heart disease using risk factor categories. Circulation. 1998;97:1837–47. doi: 10.1161/01.cir.97.18.1837. [DOI] [PubMed] [Google Scholar]
- 20.Gonen M, Hellar G. Concordance probability and discriminary power in proportional hazards regression. Biometrika. 2005;92:965–70. [Google Scholar]
- 21.Curtis JR, Jain A, Askling J, et al. A comparison of patient characteristics and outcomes in selected European and U.S. rheumatoid arthritis registries. Semin Arthritis Rheum. 2010;40:2–14.e1. doi: 10.1016/j.semarthrit.2010.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Listing J, Strangfeld A, Kary S, et al. Infections in patients with rheumatoid arthritis treated with biologic agents. Arthritis Rheum. 2005;52:3403–12. doi: 10.1002/art.21386. [DOI] [PubMed] [Google Scholar]
- 23.Askling J, Fored CM, Brandt L, et al. Time-dependent increase in risk of hospitalisation with infection among Swedish RA patients treated with TNF antagonists. Ann Rheum Dis. 2007;66:1339–44. doi: 10.1136/ard.2006.062760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Doran MF, Crowson CS, Pond GR, et al. Frequency of infection in patients with rheumatoid arthritis compared with controls: a population-based study. Arthritis Rheum. 2002;46:2287–93. doi: 10.1002/art.10524. [DOI] [PubMed] [Google Scholar]
- 25.Manno R, Calabrese L, Curtis J, et al. Evaluating immunization knowledge and practices by rheumatologists. Arthritis Rheum. 2008;58:4007. [Google Scholar]
- 26.Doran MF, Crowson CS, Pond GR, et al. Predictors of infection in rheumatoid arthritis. Arthritis Rheum. 2002;46:2294–300. doi: 10.1002/art.10529. [DOI] [PubMed] [Google Scholar]
- 27.Ting G, Schneeweiss S, Scranton R, et al. Development of a health care utilisation data-based index for rheumatoid arthritis severity: a preliminary study. Arthritis Res Ther. 2008;10:R95. doi: 10.1186/ar2482. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.