Abstract
A 26-year-old man presented to accident and emergency with a 1-week history of fever, rigors and sudden onset of severe left testicular pain. The symptoms started without trauma and pain radiated to the abdomen and was worse on walking. He had raised temperature and inflammatory markers. He reattended 2 days later with progressive bilateral groin pain, night sweats and the blood cultures grew Staphylococcus aureus. Repeat cultures were sent and the patient was arranged to be followed up in clinic. He returned 5 days later with worsening symptoms. S aureus was grown from the second blood culture, so he was admitted for intravenous flucloxacillin. MRI of the pelvis showed a small fluid collection around the pubic symphysis and extensive periarticular bone marrow oedema consistent with septic arthritis and a retropubic abscess. He was treated with a 8-week course of flucloxacillin with complete resolution.
Background
Septic arthritis of the pubic symphysis is rare. The symptoms can mimic a myriad of pathologies masking the true diagnosis. Radiographic signs can be delayed or undetected in certain modalities of radiological investigation. Therefore, the diagnosis can be missed and treatment delayed. We describe one such case presenting to our institution which highlights these difficulties and reiterates the importance of maintaining a high level of suspicion based on the clinical symptoms and key points in the history to ensure prompt treatment and avoid severe complications.
Case presentation
A previously healthy 26-year-old man presented to accident and emergency with a 1-week history of fever, rigors and sudden onset of severe left testicular pain. The symptoms started a day after playing a football match, though the patient denied any history of trauma. The pain radiated to the abdomen and was worse on walking. He had a temperature of 39.2ºC and a normal testicular and abdominal examination.
Investigations
The blood cultures grew Staphylococcus aureus. Repeat cultures again grew same bacterium. C reactive protein had risen to 337 mg/l with an erythrocyte sedimentation rate of 56 mm/h. Echocardiogram was normal and autoimmune screen was negative.
MRI of the pelvis (transverse and longitudinal section) showed a small fluid collection around the pubic symphysis and extensive periarticular bone marrow oedema consistent with septic arthritis and a retropubic abscess (figure 1A–C).
Figure 1.
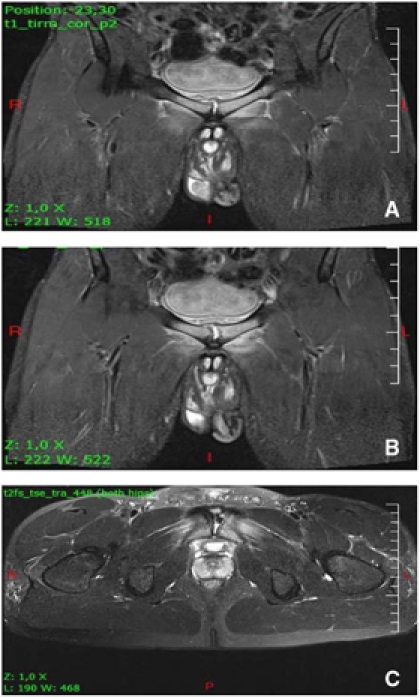
MRI of the pelvis ((A,B) longitudinal section, (C) transverse section) showing a small fluid collection around the pubic symphysis and extensive periarticular bone marrow oedema consistent with septic arthritis and a retropubic abscess.
Treatment
The abscess was deemed undrainable due to its size and position. The patient was prescribed intravenous flucloxacillin 1 g four times a day for 2 weeks and discharged with further 2 weeks of oral flucloxacillin at 500 mg four times a day on microbiologist’s advice. A repeat MRI 4 weeks later showed an improvement in the collection but persistent septic arthritis, and further 4 weeks of flucloxacillin was continued on the previous dose.
Outcome and follow-up
A repeat MRI 4 weeks later showed an improvement in the collection but persistent septic arthritis, so a further course of antibiotics was prescribed. Fortunately, the fever settled and the patient mobilised full weight-bearing. Swimming and cycling were encouraged but heavy contact sports were avoided for a few months.
He eventually made a full recovery and was discharged from the outpatient clinic.
Discussion
The pubic symphysis is the insertion point of the hip adductors and rectus abdominus muscles. Inflammation and infection at this site is a recognised complication in athletes whose activities consist of repetitive over-adduction and twisting such as that experienced by footballers.1 2 It presents with pain on hip abduction, pubic tenderness, pain while walking, difficulty weight-bearing and testicular, suprapubic and abdominal pain.1 In the context of no overt sepsis this is described as osteitis pubis and is in itself a rare diagnosis.3 An even rarer diagnosis is septic arthritis which can often be misdiagnosed as osteitis pubis but is importantly associated with sudden onset of pain, fever and positive blood cultures or aspirate.1 4 There is some debate as to whether these two pathologies represent a spectrum of disease with septic arthritis occurring in those predisposed to repetitive strain and an existing osteitis pubis.1 2 S aureus is commonly implicated in septic arthritis occurring in athletes.2 4 The pathogenesis is thought to be due to microtrauma with repetitive movement during sports that makes it susceptible to seeding of S aureus (which is transiently present in the body) and subsequent colonisation.5 MRI scanning is the most reliable method of detecting the disease as the changes on CT scan and radiograph can be delayed.2 In our case, the presenting symptoms and signs were typical of a pubic symphysis septic arthritis and highlights that this disease can be associated with varying levels of sporting activity. The absence of early radiological and CT signs suggests that the septic arthritis had arisen spontaneously. Retropubic abscess formation is secondary to the septic arthritis of the pubic symphysis.6 7 The ideal treatment is a prolonged course of intravenous and oral antibiotics and abscess drainage if possible.1 3 Awareness and early recognition can prevent disease progression and unnecessary invasive treatment.8 9
Learning points.
-
▶
Septic arthritis is a rare presentation but should be suspected in patients presenting with groin pain, pubic tenderness, difficulty walking, abdominal/genital symptoms and fever.
-
▶
Radiological results can be misleading as changes can take time to evolve. Therefore, treatment should be based on clinical suspicion.
-
▶
Positive blood cultures or aspirate need to be obtained early on and positive results treated promptly with intravenous antibiotics to prevent disease progression to osteomyelitis and invasive management such as surgical debridement.
Footnotes
Competing interests None.
Patient consent Obtained.
References
- 1.Pauli S, Willemsen P, Declerck K, et al. Osteomyelitis pubis versus osteitis pubis: a case presentation and review of the literature. Br J Sports Med 2002;36:71–3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ross JJ, Hu LT. Septic arthritis of the pubic symphysis: review of 100 cases. Medicine (Baltimore) 2003;82:340–5 [DOI] [PubMed] [Google Scholar]
- 3.Choi H, McCartney M, Best TM. Treatment of osteitis pubis and osteomyelitis of the pubic symphysis in athletes: a systematic review. Br J Sports Med 2011;45:57–64 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Karpos PA, Spindler KP, Pierce MA, et al. Osteomyelitis of the pubic symphysis in athletes: a case report and literature review. Med Sci Sports Exerc 1995;27:473–9 [PubMed] [Google Scholar]
- 5.Cunningham R, Cockayne A, Humphreys H. Clinical and molecular aspects of the pathogenesis of Staphylococcus aureus bone and joint infections. J Med Microbiol 1996;44:157–64 [DOI] [PubMed] [Google Scholar]
- 6.Lorenzo G, Meseguer MA, del Rio P, et al. Prevesical abscess secondary to pubis symphysis septic arthritis. Pediatr Infect Dis J 2000;19:896–8 [DOI] [PubMed] [Google Scholar]
- 7.Yoshida S, Nakagomi K, Goto S. Abscess formation in the prevesical space and bilateral thigh muscles secondary to osteomyelitis of the pubis–basis of the anatomy between the prevesical space and femoral sheath. Scand J Urol Nephrol 2004;38:440–1 [DOI] [PubMed] [Google Scholar]
- 8.Pang KW, Maffulli N, Chan KM. Acute abdomen: an atypical presentation of pubic osteomyelitis. Bull Hosp Jt Dis 1995;54:106–8 [PubMed] [Google Scholar]
- 9.Sexton DJ, Heskestad L, Lambeth WR, et al. Postoperative pubic osteomyelitis misdiagnosed as osteitis pubis: report of four cases and review. Clin Infect Dis 1993;17:695–700 [DOI] [PubMed] [Google Scholar]


