Abstract
Background
The Surgical Morbidity and Mortality conference has long been used as an opportunity for both process improvement and resident education. With recent heightened focus on creating environments of safety and on meeting the ACGME General Competencies, novel approaches are required. With the understanding that the provision of medical care is an inherently multi-disciplinary enterprise, we advocate the creation and use of a Multi-disciplinary Morbidity and Mortality conference (MM&M) as a means to establish this culture of safety while teaching the ACGME General Competencies to surgery residents.
Methods
A quarterly MM&M conference was implemented to foster communication between disciplines, provide a forum for quality improvement, and enhance patient care. All stakeholders in the peri-operative enterprise attend, including the departments of surgery, anesthesia, radiology, pharmacy, nursing, environmental services, risk management and patient services. Cases that expose system issues with potential to harm patients are discussed in an open, nonconfrontational forum. Solutions are presented and initiatives developed to improve patient outcomes. We retrospectively reviewed the topics presented since the conference's inception, grouping them into one of 7 categories. We then evaluated the completion of the improvement initiatives developed after discussion at the conference.
Results
Over a 21-month period, 11 cases were discussed with 23 “actionable” initiatives for quality improvement. Cases were grouped by category; procedures (36.5%), process (36.5%), patient-related (9%), communication (9%), medication (9%), device (0%), and ethics (0%). All cases discussed addressed at least four of the six ACGME General Competencies.
Conclusions
Like the practice of medicine, the occurrence of adverse outcomes is frequently multi-disciplinary. An MM&M conference is useful in its potential to meet ACGME General Competencies, engender a culture of patient safety, and rapidly achieve quality-improvement and systems health care delivery initiatives in a large academic medical center.
Keywords: Multi-disciplinary Morbidity and Mortality, ACGME General Competencies, Surgical Education
Introduction
“I will prescribe regimens for the good of my patients according to my ability and my judgment and will never do harm to anyone.”
-The Hippocratic Oath
A commitment to patient safety and well-being has been a central tenet of the medical profession for centuries. However, the Institute of Medicine's (IOM) To Err is Human report revealed that we are failing in upholding this core pillar of medical practice[1]. In 1983, the Accreditation Council for Graduate Medical Education (ACMGE) mandated that all medical training programs incorporate a regular Morbidity and Mortality (M&M) conference into their educational paradigm, in an effort to formalize the discussion of cases in which an unintended event may have adversely affected patient outcome[2]. These M&M conferences provide a forum in which to identify adverse patient outcomes, openly discuss medical mistakes, disseminate information learned from experience, and reinforce a sense of professional accountability for patient safety[3]. As a powerful teaching tool, M&M conferences play an important role in raising the next generation of surgeons in an environment that emphasizes reflection on outcomes with a commitment to addressing those systems and human factor issues that set the stage for lapses in patient safety[4].
Surgeons have long been champions of the importance of improving patient care by examining bad outcomes. Ernest Armory Codman, an early 20th century surgeon, can be credited with establishing one of the earliest M&M formats, with his “end result system” to document complications and outcomes[3]. While early forms of M&M conferences were frequently structured so as to assign responsibility for adverse events, a more recent paradigm has focused on identifying system-based errors and their potential contributions to adverse medical outcomes[5]. Unfortunately, M&M conference attendance is frequently limited to physicians from the hosting specialty, despite the fact that the practice of medicine is an inherently multi-disciplinary endeavor, requiring close teamwork among a variety of professionals across specialties. Safe patient care cannot be provided outside of a team approach[6]. Indeed, Baker et al.[7] assert that to successfully address system-based errors, “it is imperative that the case be reviewed by multiple specialties at one time”.
The ACGME mandate to incorporate the six General Competencies into residency education strives to accomplish the overall goals of improving resident performance, augmenting the effectiveness of the training program, and achieving better patient care. This mandate outlines the areas of competency required of all physicians, including patient care, medical knowledge, practice-based learning and improvement, interpersonal and communication skills, professionalism, and systems-based practice. Effective incorporation of the General Competencies into resident training is a challenging goal facing every program director. Practice-based learning improvement (PBLI) and systems-based practice (SBP) have been particularly challenging to conceptualize[8]. The dynamic relationships between patient safety, teamwork in healthcare and graduate medical education have prompted novel approaches to integrating these concepts into residency training programs. Multidisciplinary rounds streamline patient care by including pharmacists, nurses, physical therapists, and social workers in the daily decisions made by physicians[9]. The multidisciplinary nature fosters efficient communication and improves the efficiency of care delivered. Multidisciplinary M&M conferences have been used to focus on patient safety, highlight system-issues that may adversely affect patient outcome, and create solutions to address these issues [5, 10–12]. We believe that the use of a Multi-disciplinary Morbidity and Mortality (MM&M) conference presents a unique opportunity to incorporate all six ACGME competencies effectively and efficiently into a surgical residency training program.
Methods
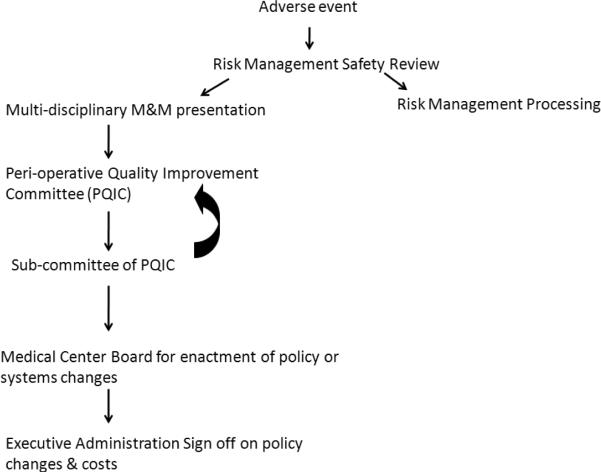
We believe that the establishment of a culture of safety is the first step in providing quality patient care, that the delivery of healthcare requires a team approach, and that systems-based problems rather than individual culpability underlie most adverse events. Based upon this understanding, our institution implemented a MM&M conference in 2008. The conference is a quarterly, 90-minute session attended by all members of the peri-operative enterprise, from environmental services to administrators, anesthesiologists, nurses, pharmacists, radiologists, and surgeons. The conference is organized by a committee formed specifically for this purpose. Cases associated with adverse patient outcomes are reviewed by Risk Management on a weekly basis. Based upon educational value, adverse patient events, or “near miss” status, appropriate cases are selected for presentation. At each conference, residents and faculty involved in the case present the patient's medical history, reason for admission, and clinical course. Based on the root cause analysis, discussions are focused on understanding the interface between systems and human factors as sources of error. Throughout the conference, a moderator facilitates group discussion, fields questions, and emphasizes learning objectives. At the end of the conference, an experienced clinician and the institution's safety officer summarize the teaching points and propose changes to prevent a recurrence of the systems-issue that precipitated the adverse event. Furthermore, participants are asked to submit evaluations to assess whether the conference effectively accomplished its learning objectives, and whether the attendees anticipate changes in their practice based upon what was learned. After presentation at MM&M, cases are referred to the Peri-operative Quality Improvement Committee (PQIC) for implementation of proposed policy changes (Figure I). All policy changes are approved by the Executive Medical Board of Vanderbilt University Medical Center. Each subsequent conference begins with an update on the changes enacted by sub-committees of the PQIC and subsequent improvements in the system of care or patient safety.
Figure I.
Process of Case Selection for Presentation at MM&M
After obtaining IRB exemption, we retrospectively reviewed the topics presented since the inception of the MM&M conference, grouping them into one of seven categories adapted from previously published reports[10]. We then evaluated the patient care improvements that resulted from the sessions. Cases were grouped by the following categories: procedures, process, patient-related, device, communication, medication, and ethics. Examples of cases by category can be found in Table I. Finally, we evaluated each case to determine which of the six ACGME General Competencies were explicitly addressed. Category assignments and determination of the General Competencies addressed by each case were determined by three reviewers.
Table I.
Case examples by category
| CATEGORY | EXAMPLE |
|---|---|
| Procedures | Hematoma after epidural placement |
| Process | Management of dislodged tracheostomy |
| Patient-related | Physiologic parameters governing timing of operative interventions in critically ill patients |
| Device | Not presented |
| Communication | Relaying news of an adverse event to family members |
| Medication | Administration of pre-operative antibiotics |
| Ethics | Not presented |
Results
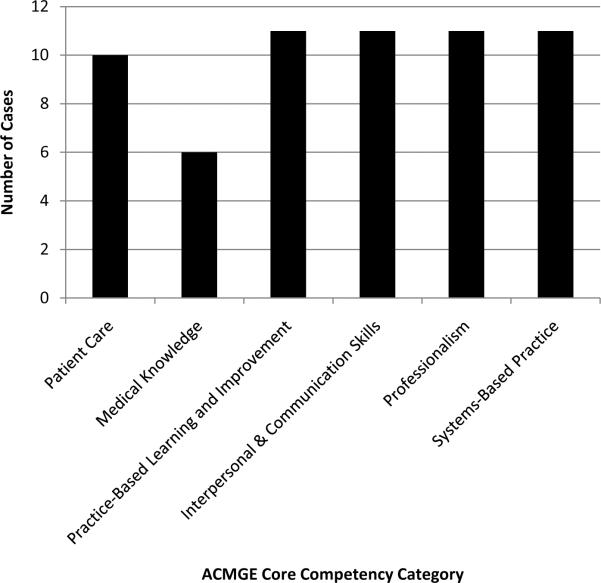
Over a 21-month period, 11 cases were discussed with 23 proposed initiatives for quality improvement. Cases by topic are presented in Figure II, and were classified as four procedure-related (36.5%), four process-related (36%), one patient-related (9%), one solely-communication error (9%), one medication error (9%), and none ethics-related (0%) or device-related (0%). Twenty-three safety initiatives resulted from MM&M discussion; of these, 15 have been completed. Examples of initiatives proposed are displayed in Table II. All of the cases covered since implementation of the conference have addressed at least four of the six ACGME general competencies, providing a novel approach to incorporating these objectives into all graduate training programs in the field of Surgical Sciences (Figure III).
Figure II.
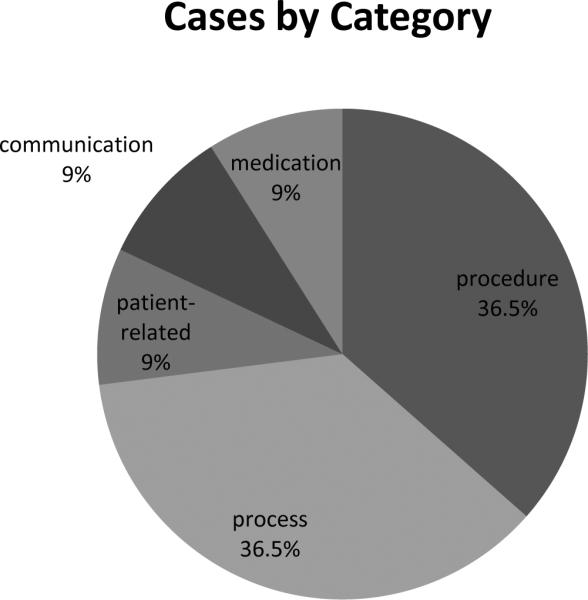
Presented cases by category
Table II.
Examples of quality-improvement initiatives implemented as a result of the MM&M conference.
| EXAMPLES OF QUALITY-IMPROVEMENT INITIATIVES |
|---|
| Educational module to teach management of dislodged tracheostomy |
| Product warning label added to surgical scrub remover nationwide by manufacturer |
| Development of institution-wide protocol for addressing hematoma after epidural placement |
Figure III.
Number of cases discussed in MM&M Conference fulfilling each of the ACGME Core Competencies
Example Case
A patient was taken to the operating room for two minor procedures to be performed sequentially. At the termination of the first, the patient was re-prepped and draped in anticipation of the second procedure. During the re-prepping process, an alcohol-based skin prep remover was used at the first operative site. Concurrently, bovie electrocautery was used to control a small bleeding vessel in the skin at the second operative site. The electrocautery spark came in contact with the alcohol-based skin prep remover, igniting it. The patient suffered second degree burns.
This case was reviewed during the MM&M conference, and resulted in several system-based changes. First, warning labels were placed on the product throughout the institution, reminding providers of the risks associated with using alcohol-based skin prep removers in the presence of an electric spark. Protocols were implemented to prohibit use of such products prior to removal of the electrocautery device from the field. Additionally, more stringent operating room fire drills and mandatory completion of an electronic learning module on fire safety were required of all operating room personnel. Furthermore, discussions with the product manufacturer resulted in warning labels being placed on the product nationally to warn against the dangers of using the product in the presence of potential electrical spark. This case fulfills all six ACGME General Competencies as outlined in Table III.
Table III.
Examples of manner in which all ACMGE Core Competencies are addressed by a single “Fire in the OR” case discussion in MM&M Conference.
| Patient Care | Medical Knowledge | Practice-Based Learning and Improvement | Interpersonal and Communication Skills | Professionalism | Systems-Based Practice |
|---|---|---|---|---|---|
| Discussed manner by which to protect patient from risk of fire during electrocautery | Electronic learning module created to teach operating room personnel the physics of electrocautery and its safe use | Promote providers' self-reflection on their own behavior in preventing fires in the operating room | Established guidelines by which operating room personnel are to communicate a fire hazard and guidelines to follow when responding to a fire | Highlighted response by operating surgeons to protect patient and minimize harm during sentinel event | Implementation of institutional policy regarding use of alcohol-based skin prep, and national labeling change to warn of danger |
Discussion
Improving patient outcomes necessitates creating a culture of safety. The well known concept of the trajectory of error is a series of preventable human errors. Despite the best efforts of medical professionals, human error continues to confound the achievement of a “zero harm” healthcare system. In order to create such a culture of safety, one must first understand the factors contributing to human error. While old paradigms sought to explain failure by blaming individuals for poor judgment or wrong decisions, and prevent error by increasing complexity of the system, the new view of human error takes a different approach. Human error is rather a “symptom of trouble deeper inside the system” and can only be addressed by understanding that human error is not random but is connected to the system in which an individual operates. Furthermore, a culture of safety can only be created by fostering its practice at “all levels of an organization”[13]. Adverse events are multi-factorial in nature, and require a system- based approach to correct. As holes in the system are identified, it is crucial to place data in context by reconstructing the situation that produced and accompanied the event, so as to resist the temptation to rely solely on hindsight to identify errors. While one cannot change the human tendency to occasionally err, the conditions under which individuals work can be changed to make unsafe actions less likely to occur[14]. Solutions to prevent error require commitment from all levels, and must be monitored over time to evaluate efficacy. High Reliability Organizations, such as nuclear power plants and air traffic control systems are those that must operate as near as possible to a failure-free standard, or great harm may come to a great many people[14]. These organizations serve as models of how to deal with unexpected events by careful attention to ongoing operations, anticipation of pitfalls, resilience in the face of failures, involvement of experts, and a commitment to establishing a culture of safety[15]. The healthcare enterprise should strive to be included in this group of “zero harm” organizations.
Subsequent to the IOM report highlighting the need to address medical mistakes, methods to improve the system of healthcare delivery, and thereby patient care, have been implemented by hospitals across the country. This focus on patient safety extends to the education sector with increasing demands placed on residency programs to incorporate curriculum to address these topics explicitly. Training programs are uniquely poised to address issues of patient safety and improved quality of care as they strive to train the next generation of physicians in the “science and methods of patient safety and quality improvement” [16]. Meanwhile, work hour restrictions continue to whittle away the time available for education, and programs struggle to find a balance between service and education in an 80-hour work week. It is into this setting that the ACGME endorsed the Outcome Project in 1999, to assess the outcomes of residency education across six general competencies- patient care, medical knowledge, practice-based learning and improvement, interpersonal and communication skills, professionalism, and systems-based practice [17].
Even though our institution's MM&M conference was not initially based upon the ACGME Competencies on its inception, the insightful residency program can incorporate these principles into every aspect of its curriculum to maximize educational opportunities. The ACGME mandate to incorporate the six general competencies into resident education provides an opportunity to integrate competencies and patient safety by the establishment of a Multidisciplinary Morbidity and Mortality conference. Furthermore, such an approach facilitates compliance with ACGME requirements without further stretching already-limited educational time. We believe that a Multi-disciplinary Morbidity & Mortality Conference provides a unique opportunity to achieve these principles, particularly the more difficult ones of PBLI and SBP, although we recognize that other educational conferences may offer a similar opportunity. In solidifying the healthcare team concept, programs not only foster communication between medical providers and empower all members of the healthcare team to contribute to quality improvement, but also educate the next generation of physicians to build a culture of cooperation in their own practices, thus improving patient outcomes. This environment of open communication and cooperation becomes even more important when one understands that failures of communication underlie three-quarters of adverse events and represent an important system flaw. Multidisciplinary conferences provide a forum where cooperation among specialties must be encouraged, and each group may benefit from the expertise of the other disciplines[7].
Limitations of this study include its description of an MM&M conference at a single institution, which may not be generalizable to other institutions. While the implementation of a similar conference at other institutions may be expected to offer similar success in initiatives to improve patient care, considerable time is required to make such a conference successful. Support from institutional administration, program directors, and safety officers, as well as backing from the diverse members of the peri-operative enterprise are required to ensure success. The establishment of a dedicated committee to monitor and track and long-term compliance with quality-improvement initiatives arising from the MM&M conference is beneficial to ensure timely changes to the healthcare delivery system. In addition, the results discussed here are largely qualitative in nature and describe the process of implementing a MM&M conference at our institution. Additional research is needed to quantify the impact of this conference on patient safety and quality improvement. Finally, determination of the topics presented and ACGME General Competency addressed by each case are subjective, although they have been determined by three reviewers in our study.
Acknowledgments
Financial support was provided in part by an NIH T32 training grant in Diabetes and Endocrinology 5T32DK007061-35 (RK) and an AHRQ Health Services Training Grant T32 HS013833-08 (MPL and JS).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Podium presentation at the American College of Surgeons Clinical Congress, October 5, 2010
Conflict of Interest Statement The authors have no conflicts of interest to report relative to the preparation or publication of this manuscript.
ACGME General Competencies addressed: Patient care, Medical knowledge, Practice-based learning & improvement, Interpersonal & communication skills, Professionalism, Systems-based practice
REFERENCES
- 1.Kohn KT, Corrigan JM, Donaldson MS. To Err is Human: Building a Safer Health System. National Academy Press; Washington, D.C.: 1999. [PubMed] [Google Scholar]
- 2.Essentials and Information Items Accreditation Council for Graduate Medical Education. Graduate Medical Education Directory 1995–1996 [Google Scholar]
- 3.Orlander JD, Barber TW, Fincke BG. The morbidity and mortality conference: the delicate nature of learning from error. Acad Med. 2002;77(10):1001–6. doi: 10.1097/00001888-200210000-00011. [DOI] [PubMed] [Google Scholar]
- 4.Harbison SP, Regehr G. Faculty and resident opinions regarding the role of morbidity and mortality conference. aM j sURG. 1999;177(2):136–9. doi: 10.1016/s0002-9610(98)00319-5. [DOI] [PubMed] [Google Scholar]
- 5.AHRQ [cited 2010 July 12, 2010];Transforming the morbidity and mortality conference into an instrument for systemwide improvement. Available from: http://www.ahrq.gov/downloads/pub/advances2/vol2/Advances-Deis_82.pdf. [PubMed]
- 6.Manser T. Teamwork and patient safety in dynamic domains of healthcare: a review of the literature. Acta Anaesthesiologica Scandinavica. 2009;53:143–141. doi: 10.1111/j.1399-6576.2008.01717.x. [DOI] [PubMed] [Google Scholar]
- 7.Baker S, Darin M, Lateef O. Multidisciplinary Morbidity and Mortality Conferences: Improving Patient Safety by Modifying a Medical Tradition. The Joint Commission Perspectives on Patient Safety. 2010;10(2):8–10. [Google Scholar]
- 8.Ziegelstein RC, Fieback NH. “The mirror” and “the village”: a new method for teaching practice-based learning and improvement and systems-based practice. Acad Med. 2004;79(1):83–8. doi: 10.1097/00001888-200401000-00018. [DOI] [PubMed] [Google Scholar]
- 9.Dutton R. Daily multidisciplinary rounds shorten length of stay for trauma patients. Journal of Trauma, Injury, Infection and Critical Care. 2003;55(5):913–919. doi: 10.1097/01.TA.0000093395.34097.56. [DOI] [PubMed] [Google Scholar]
- 10.Tuong B, Schnitzer Z, Pehora C, et al. The experience of conducting multidisciplinary morbidity and mortality reviews in a pediatric interventional radiology service: a retrospective study. Journal of Vascular Interventional Radiology. 2009;20:77–86. doi: 10.1016/j.jvir.2008.09.013. [DOI] [PubMed] [Google Scholar]
- 11.AHRQ Healthcare Innovations Exchange [cited 2010 July 7, 2010];Hospital Revamps Morbidity and Mortality Conferences to Focus on System-wide Improvement Leading to Better Identification and Addressing of Quality Problems. 2010 Available from: http://www.innovations.ahrq.gov/content.aspx?id=2219.
- 12.Hiner J, White S, Fields W. Infusing evidence-based practice into interdisciplinary perinatal morbidity and mortality conferences. J Perinat Neonatal Nurs. 2009;23(3):251–7. doi: 10.1097/JPN.0b013e3181af6ebb. [DOI] [PubMed] [Google Scholar]
- 13.Dekker S. The Field Guide to Understanding Human Error. Ashgate Publishing Company; Burlington, VT: 2006. p. 236. [Google Scholar]
- 14.Reason J. Managing the Risks of Organizational Accidents. Ashgate Publishing Company; Burlington, VT: 2006. p. 252. [Google Scholar]
- 15.Weick K, Sutcliff K. University of Michigan Business School Management Series. Jossey-Bass; San Francisco, CA: 2001. Managing the Unexpected. [Google Scholar]
- 16.Voss JD, May NB, Schlorling JB, et al. Changing conversations: teaching safety and quality in residency training. Acad Med. 2008;83(11):1080–7. doi: 10.1097/ACM.0b013e31818927f8. [DOI] [PubMed] [Google Scholar]
- 17.Swing S. ACGME launches outcome assessment project. JAMA. 1998;279:1492. [Google Scholar]