Abstract
PURPOSE
This study describes parent and adolescent perspectives on clinical need for and attitudes toward care for attention-deficit/hyperactivity disorder (ADHD), and explores how these views related to past year mental health service use.
METHODS
Parent and adolescent interviews were conducted six years after school district screening for ADHD. Mental health service use, adolescent and parent perceived clinical need (ADHD symptoms, disruptive behavior disorders, anxiety/depression, functioning) and enabling attitudes (treatment receptivity, ADHD stigma) as well as parent factors (caregiver strain, distress, instrumental social support) were assessed using standardized measures. Nested logistic regression modeling was used to determine the hierarchical contribution of parent and adolescent perspectives on past year service use, adjusting for prior mental health service use. Stepwise regression was conducted to identify which variables were most predictive of service use.
RESULTS
Most (79%) adolescents at high risk for ADHD had a history of lifetime mental health service use, but only 42% had received any mental health services in the past year. In hierarchical modeling, only parent inattention ratings and medication receptivity and adolescent ADHD stigma perceptions contributed significantly to improved model fit. Stepwise regression confirmed these three predictors (OR 1.2, 3.8, and 0.2, respectively) and identified adolescents-reported functioning as an additional service use predictor (OR 1.1).
CONCLUSION
Adolescents’ perceptions about stigma related to ADHD are influential in treatment receipt. Quality improvement interventions for adolescents with ADHD should include psychoeducational interventions for adolescents and their parents that target medication receptivity and stigma about ADHD.
INTRODUCTION
More than one-half of children with attention-deficit/hyperactivity disorder (ADHD) continue to have symptoms and impairment during adolescence and young adulthood [1], yet little is known about how individual and parent-level factors influence service use during this key transitional period. The need for additional research [2] is underscored by the absence of recommendations in national ADHD treatment guidelines on how care should be tailored for adolescents and young adults [3, 4]. In addition, quality improvement interventions to promote continuous care for adolescents with ADHD are warranted because medication and behavioral interventions in home and school settings have been found effective [5, 6], but older youth are more likely to drop out of treatment than their school-age counterparts [7, 8]. Under-treatment may also increase an adolescent’s risk for adverse long-term consequences for ADHD, such as school failure, juvenile justice involvement or motor vehicle accidents [9–11]. Thus, it is of public health significance to further our understanding of which factors improve the likelihood of adolescents with ADHD to receive continuous care.
Based on the well established Behavioral Model of Access [12], access to ADHD treatment during childhood has been shown to be influenced by factors at the individual, caregiver, provider, and system levels [13, 14]. Children from racial and ethnic minority backgrounds, girls and children enrolled in publicly-funded health insurance plans are less likely to receive stimulant medication treatment than children from Caucasian backgrounds, boys and privately insured children [15]. Several caregiver factors also have emerged as predictors of ADHD treatment for children. Highly stressed parents have been shown to seek more medical care, particularly for their young children [16], and several studies have documented high levels of parent stress and caregiver strain associated with ADHD [17, 18]. Conversely, lower levels of parental social network support have been found to increase the likelihood that parents seek ADHD treatment for their child [18].
Among adolescents with ADHD, the likelihood of receiving ADHD care may also be influenced by an interplay of individual and caregiver factors that are unique to this developmental stage. Earlier studies suggest that adolescents’ increasing treatment drop-out and medication non-adherence rates may be attributable to both declining parental control over adolescents’ health behavior and negative attitudes held by adolescents towards mental health treatment [19]. Furthermore, substantial ADHD stigma concerns among participating youth were identified in a recent nationally representative survey [20]. Such stigma perceptions may impede help-seeking or promote discontinuation of treatment because adolescents are developmentally sensitive about public opinions and seek peer approval.
Nevertheless, significant gaps exist on adolescents’ views about ADHD and mental health care, how their perspectives may influence the continuity of mental health care, and how the impact of adolescent perspectives on mental health service use compares to those of their parents. This study therefore describes perceived clinical need and attitudes relevant to ADHD care from both adolescent and parent treatment need perspectives and explores how these influence a teen’s likelihood for receiving mental health services. We hypothesize that parent perspectives, including perceptions of clinical need for care, treatment receptivity and caregiver emotional and instrumental support increase the odds of past year mental health service use. We also explore whether adolescent perspectives, especially treatment receptivity and ADHD stigma perceptions, emerge as significant predictors of past year mental health service use when adjusting for prior mental health service use, and hypothesized parent factors.
METHODS
Participants and procedures
This research uses data from a longitudinal cohort study assessing detection and access to care for ADHD in a representative school district sample which followed participants in multiple study waves between 1998 and 2006 [15]. Interviews for this report occurred in 2004 to 2005, on average 6.8 years (SD 0.47) after the initial screening, during study wave 4.
To identify students at high risk for ADHD, a random sample of children, oversampling girls by a factor of two, was derived from public school records of 12,009 kindergarten through fifth graders from a North Florida school district. Of 1,615 children screened, 29.5% (n=476) were deemed at “high risk for ADHD” on enrollment if they: 1) were diagnosed or treated for ADHD; 2) were considered by parent or teachers to have ADHD; or 3) elicited behavioral concerns and had parent-reported scores on the Swanson-Nolan-and Pelham-IV (SNAP-IV) [21] at or greater than 1.5 standard deviations above the norm. Subsequently high risk students underwent diagnostic assessment for ADHD, oppositional defiant disorder (ODD), and conduct disorder (CD) using the parent version of the NIMH Diagnostic Interview Schedule for Children-4th version (DISC-4.0) at study wave 2 [22] or the Kiddie-SADS-Present and Lifetime Version (K-SADS PL) at study wave 4 [23]. For wave 4 interviews we interviewed 192 of 372 eligible adolescents (52%); 70 (19%) declined participation and 110 (30%) were lost to follow-up. Study participants did not differ from those who refused or were lost to follow-up on race, gender or poverty status. For 30 youths who rejoined the study in adolescence and could have outgrown ADHD symptoms since initial screening, we used the semi-structured K-SADS instead of the DISC-4 to ascertain their ADHD diagnoses because we expected better performance for lifetime assessment. In addition, for this analysis, 24 of the 192 adolescents interviewed were excluded because they were unlikely to need ADHD treatment, as indicated by not meeting DSM-IV criteria for ADHD, no prior lifetime history of ADHD treatment, and fewer than four ADHD symptoms displayed at follow-up interview in 2004–2005.
Of the 168 adolescents studied, 53% were female (n=89), 35% were from African American backgrounds (n=58), and 58% (n=97) qualified for free or reduced lunch status. Their average age was 15.0 years (s.d. 1.67). Health insurance information was available for 113 or 168 adolescents and almost all (n=105 of 113, 93%) had health insurance coverage, one-half (n = 58, 51%) through private sources and the remainder (n = 47, 42%) through public insurance carriers. More than 60% (n=100, 61%) met full DSM-IV criteria for ADHD during diagnostic interviews (combined subtype: n=53, 32%; inattentive subtype: n=34, 21%; hyperactive/impulsive subtype: n=13, 8%), and 74% (n=120) screened positive for ADHD on the Vanderbilt Attention Deficit/Hyperactivity Disorder Parent Rating Scale [24] at the 2004–2005 follow-up interview.
The study was approved by the University Institutional Review Board and the school district research office. Informed consent (parents and young adults) or child assent (adolescents) were obtained from all subjects, who received a stipend of $40 (parents) or $30 (adolescents) for their participation. Trained research assistants conducted personal interviews with parents and adolescents in homes, community locations, or at our research center.
Measurement
Predictors
Demographic information
Information about child age, gender, race, and poverty status was obtained from school registration records and verified at the study wave 1 interview.
Parent perspectives
Clinical Need
The Vanderbilt Attention Deficit/Hyperactivity Disorder Parent Rating Scale (VADPRS) was used to assess symptoms of ADHD, disruptive behavior and internalizing disorders [24]. The 47-item VADPRS uses a 4-point scale (0 = never, 3 = very often). Internal consistency and concurrent validity have been established [24]. Parents completed the Columbia Impairment Scale (CIS), a 13-item measure of functioning using a 5-point scale (0 = no problem, 4 = a very bad problem). The CIS has been reported to have high internal consistency (Cronbach’s α = .85) and test-retest reliability (r = .89) in an ethnically and economically diverse child sample; scores above 14 are considered clinically relevant [25].
Treatment receptivity
Parents answered questions about their receptivity towards medication and counseling, taken from the Child and Adolescent Services Assessment (CASA) [26], “Do you think that getting medications for a serious emotional or behavioral problem would be (has been) a good idea for your child?” and “Do you think that getting counseling for a serious emotional or behavioral problem would be (has been) a good idea for your child?” Responses to each question occurred on a 4-point scale (0 = yes, definitely a good idea; 1 = probably a good idea; 2 = probably not a good idea; 3 = definitely not a good idea). Separate receptivity variables were created for medications and for counseling that distinguished ‘receptive’ (treatment definitely/probably a good idea) from ‘unreceptive’ (treatment definitely/probably not a good idea) parents.
Caregiver factors
Parents completed the Caregiver Strain Questionnaire (CSQ), a 21-item adult self-report instrument assessing the impact of caring for a child with emotional or behavioral problems such as demands on time, financial strain, worry, guilt, and embarrassment. Responses are scored on a 5-point scale from “not at all” to “very much” a problem. The CSQ yields a global strain scale (lower score = less strain) and has satisfactory psychometric performance [27]. Parents completed the Mental Health Inventory (MHI) [28], a 5-item screener of psychological distress developed for use in general populations. Questions like “How much of the time, during the last month, have you felt downhearted and blue?” are scored on a 6-point scale (1 = All of the time, 6 = None of the time). The MHI produces an overall score ranging from 5–30 (higher = better mental health) and has shown satisfactory psychometric characteristics [28]. Parents also completed the Norbeck Social Support Questionnaire (NSSQ) [29]. The NSSQ assesses parents’ network characteristics, including network size, composition and perceived support. Two items assess instrumental support received for parenting, like child care or transportation, on a 4-point scale (0 = not at all; 4 = a great deal). Adequate psychometric performance has been established, including test-retest reliability (.85–.92), internal consistency (.88–.96), and concurrent validity [29, 30].
Adolescent perspectives
Clinical Need
Adolescents completed the Behavior Assessment System for Children Self Report of Personality (BASC-SRP). The 186-item BASC-SRP uses a true/false answer format and yields an overall summary score of emotional and behavioral functioning, the Emotional Symptom Index (ESI) [31]. The BASC-SRP has been used in diverse populations and found to have adequate reliability and validity [31]. Like their parent, adolescents also completed the CIS to assess their perceptions of functioning.
Treatment receptivity
Like their parent, adolescents answered questions about their receptivity towards medication and counseling, taken from the Child and Adolescent Services Assessment (CASA) [26], and with the identical 4-point response scale and scoring to distinguish receptive from unreceptive respondents. The wording of the adolescents’ questions was “Do you think that getting medications for a serious emotional or behavioral problem would be (has been) a good idea for you?” and “Do you think that getting counseling for a serious emotional or behavioral problem would be (has been) a good idea for you?”
ADHD stigma
Adolescents also completed the ADHD Stigma Questionnaire (ASQ) to assess their stigma perceptions related to ADHD [32]. The 26-item ASQ assesses perceptions of public stigma associated with ADHD, so participants are not be required to reveal personal ADHD experiences. Adolescents respond to statements like “People with ADHD work hard to keep it a secret” on a 4-point scale (1 = strongly disagree; 2 = disagree; 3 = agree; 4 = strongly agree). The measure yields an overall stigma score (range 1–4; higher score = more perceived stigma). The ASQ has shown acceptable psychometric properties in a diverse community sample of adolescents, including high internal consistency (alpha = .93), good test-retest reliability (two-week intraclass correlation coefficient =.71) and support for convergent and divergent validity [32].
Outcomes
Mental Health Services Use
Receipt of mental health treatment services was assessed using the Child and Adolescent Services Assessment (CASA) [26], a parent-report measure that inquires about mental health service use from 33 treatment settings including inpatient, outpatient and informal care. If a mental health service was ever used, detailed information about services use in the past twelve months, such as number of sessions, type of services, and prescribed medication type, dose, and frequency, was gathered. Validity studies have shown good to excellent agreement between CASA parent reports and medical records for receiving outpatient services [33, 34], and excellent agreement on details of the child’s medication regimens [34]. Adolescents were identified as receiving mental health treatment in the past 12 months if their parent reported any inpatient or outpatient mental health care during 12 months prior to the interview date. To control for past treatment in the multivariate analyses, the variable “prior treatment” was constructed using longitudinal data from prior interview waves to identify adolescents who received any mental health services more than 12 months prior to the interview date.
Statistical analyses
Agreement was examined using correlation for continuous data and kappa statistics for binary data. Differences in adolescent demographics, parent perspectives (i.e., clinical need, medication/counseling receptivity, psychological distress, caregiver strain, instrumental support) and adolescent perspectives (i.e., clinical need, medication/counseling receptivity, ADHD stigma) by past year mental health services use shown in Table 1 was examined using chi-square test of proportions and Student T-tests. Effect sizes were calculated when groups were significantly different, using Cohen’s d for continuous variables and odds ratios for categorical variables. To model mental health service use in past year, shown in Table 2, we fit a sequence of nested logistic regression models that included variables significantly associated with service use in the bivariate analyses, organized into six potential predictor domains (i.e., prior mental health treatment, parent report of adolescent need, parent attitude, caregiver strain, adolescent perspectives of need, and adolescent attitudes). Sociodemographic characteristics were not included in the logistic modeling because they were not associated with past year mental health service use in our bivariate analyses. We tested the sequential nested models to investigate the hierarchical contribution of the variable domains to predict past year mental health service use. For each model, significant improvement in model fit was tested using goodness of fit analysis (i.e., computation of chi-square statistics based on differences of – 2 LOG L between models and the corresponding difference of model degrees of freedom). Finally, shown in Table 3 we used a stepwise logistic model to identify the variables that were most predictive of mental health service use in the last 12 months.
Table 1.
Relationship between parent and adolescent perspectives and any mental health service use in past 12 months
| Any Mental Health Service Use in past 12 months | p-valuea | Effect Sizesb | ||||
|---|---|---|---|---|---|---|
| Yes (N=71) | No (N=97) | |||||
| Mean/n | SD/% | Mean/n | SD/% | |||
| Demographics | ||||||
| Gender (female) | 38 | 54% | 51 | 53% | 0.9036 | - |
| Race (African American) | 21 | 30% | 37 | 38% | 0.2486 | - |
| Receive free/reduced lunch | 40 | 56% | 57 | 59% | 0.7533 | - |
| Health insurancec | 51 | 94% | 54 | 92% | 0.5456 | - |
| Parent perspectives | ||||||
| Clinical need | ||||||
| Inattentiond | 5.17 | 2.97 | 3.46 | 3.17 | 0.0005 | 0.55 |
| Hyperactivity/impulsivityd | 3.07 | 2.86 | 2.55 | 2.70 | 0.2266 | - |
| Anxiety/depressiond | 1.42 | 1.66 | 0.72 | 1.39 | 0.0034 | 0.46 |
| ODDd | 2.97 | 2.76 | 2.33 | 2.79 | 0.1406 | - |
| CDd | 0.72 | 1.41 | 0.54 | 1.13 | 0.3530 | - |
| CISe | 15.14 | 8.31 | 11.94 | 7.72 | 0.0055 | 0.44 |
| Treatment receptivity | ||||||
| Medication | 61 | 86% | 58 | 60% | 0.0002 | 4.10 |
| Counseling | 68 | 96% | 91 | 94% | 0.5773 | - |
| Caregiver Factors | ||||||
| MHIf | 18.97 | 1.83 | 18.92 | 2.15 | 0.8637 | - |
| Caregiver Strain | 6.17 | 2.51 | 5.26 | 2.22 | 0.0140 | 0.39 |
| Instrumental Support | 2.35 | 0.91 | 2.53 | 1.07 | 0.2687 | - |
| Adolescent perspectives | ||||||
| Clinical need | ||||||
| BASC-ESIg | 50.04 | 10.11 | 47.81 | 9.17 | 0.1398 | - |
| CISe | 13.57 | 7.24 | 10.16 | 6.97 | 0.0024 | 0.48 |
| Treatment receptivity | ||||||
| Medication | 54 | 77% | 56 | 58% | 0.0090 | 2.47 |
| Counseling | 47 | 67% | 74 | 76% | 0.1918 | - |
| ADHD Stigma Perception | 2.17 | 0.46 | 2.36 | 0.42 | 0.0075 | 0.43 |
Notes:
Significance: Chi-square and Fisher’s exact test for categorical variables; t-test for continuous variables.
Effect sizes: for continuous variables Cohen’s d and for categorical variables odds ratios.
Health insurance information was available for 113 participants
Symptom counts from Vanderbilt Attention Deficit/Hyperactivity Disorder Parent Rating Scale
Columbia Impairment Scale
Mental Health Inventory
Basic Assessment System for Children, Emotional Symptom Index
Table 2.
Nested logistic modeling of parent and adolescent variables associated with mental health services use in past 12 months
| Model 1 (prior) | Model 2 (prior, parent need) | Model 3 (prior, parent need, parent receptivity) | Model 4 (prior, parent need, parent receptivity, caregiver strain) | Model 5 (prior, parent need, parent receptivity, caregiver strain, adol need) | Model 6 (prior, parent need, parent receptivity, caregiver strain, adol need, adol receptivity) | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | |
| Prior Treatment | 2.3 | 1.12–4.57 | 1.9 | 0.88–3.88 | 1.6 | 0.75–3.46 | 1.6 | 0.75–3.47 | 1.7 | 0.80–3.82 | 1.7 | 0.73–3.77 |
| Parent Perspectives | ||||||||||||
| Clinical need | ||||||||||||
| Inattentiona | 1.2 | 1.03–1.36 | 1.2 | 1.03–1.38 | 1.2 | 1.03–1.38 | 1.2 | 1.04–1.39 | 1.2 | 1.00–1.35 | ||
| Hyperactivitya | 0.9 | 0.78–1.06 | 0.9 | 0.75–1.03 | 0.9 | 0.74–1.03 | 0.9 | 0.75–1.05 | 0.9 | 0.79–1.11 | ||
| Anx/Depressiona | 1.2 | 0.93–1.53 | 1.1 | 0.87–1.46 | 1.1 | 0.87–1.46 | 1.1 | 0.83–1.41 | 1.1 | 0.86–1.52 | ||
| CIS | 1.0 | 0.96–1.07 | 1.0 | 0.98–1.09 | 1.0 | 0.96–1.10 | 1.0 | 0.93–1.09 | 1.0 | 0.91–1.10 | ||
| Medication receptivity | 4.1 | 1.76–9.50 | 4.1 | 1.76–9.52 | 3.6 | 1.54–8.62 | 3.6 | 1.47–8.61 | ||||
| Caregiver strain | 1.0 | 0.81–1.29 | 1.0 | 0.83–1.32 | 1.1 | 0.83–1.34 | ||||||
| Adolescent Perspectives | ||||||||||||
| Clinical need: CIS | 1.0 | 0.98–1.11 | 1.1 | 1.00–1.13 | ||||||||
| Medication receptivity | 2.0 | 0.93–4.43 | ||||||||||
| ADHD Stigma | 0.3 | 0.11–0.70 | ||||||||||
| 2 LOG Lb | 221.69 | 206.89c | 194.78c | 194.74 | 192.68 | 179.19c | ||||||
Notes: prior = prior treatment; adol = adolescent; OR = odds ratio; 95% CI = 95% confidence interval; Anx/Depression = anxiety and depression screen positive on Vanderbilt; CIS = Columbia Impairment Scale; Bolded OR and 95% CI = p<.05
scores from Vanderbilt
Significant improvement in model fit was tested using goodness of fit analysis (i.e., computation of chi-square statistics based on differences of – 2 LOG L between models and the corresponding difference of model degrees of freedom).
Model fit significantly improved over previous model.
Table 3.
Stepwise modeling of parent and adolescent variables associated with mental health services use in past 12 months
| OR | 95% CI | p-value | |
|---|---|---|---|
| Parent Perspectives | |||
| Clinical need: Inattentiona | 1.2 | 1.05–1.31 | 0.00604291 |
| Medication receptivity | 3.8 | 1.62–8.71 | 0.00200046 |
| Adolescent Perspectives | |||
| Clinical need: CIS | 1.1 | 1.02–1.13 | 0.00810732 |
| ADHD Stigma | 0.2 | 0.10–0.59 | 0.00151690 |
Notes: OR = odds ratio; 95% CI = 95% confidence interval; CIS = Columbia Impairment Scale;
scores from Vanderbilt
RESULTS
Lifetime and past year mental health service use
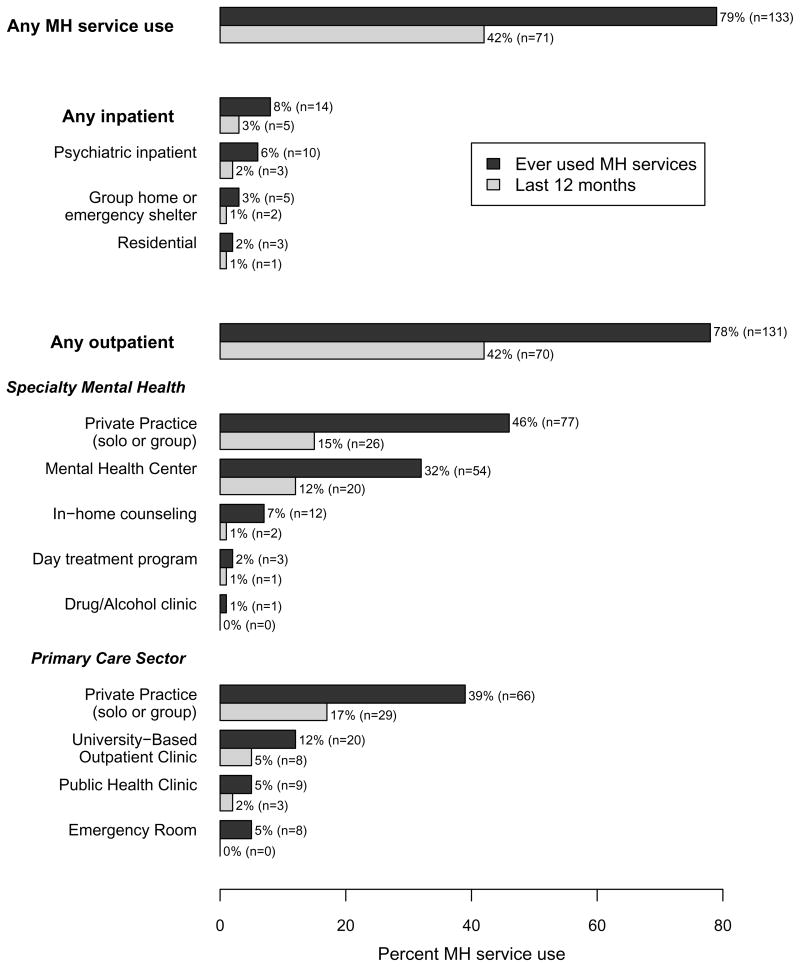
Most high-risk adolescents (n = 133, 79%) had received some mental health intervention during their lifetime but less than one-half (n = 71, 42%) had used any mental health services in the past 12 months (for details see Graph). Of the adolescents who had received any mental health services in the past year, most (54/71, 76%) also had prior mental health services. Use of inpatient services was rare (ever: n = 14, 8%; past year: n = 5, 3%), and of the 14 adolescents with lifetime inpatient service use, most (n = 12, 86%) also had a history of outpatient service use.
Graph.
Lifetime and past year mental health (MH) service use
Agreement between parent and adolescent perspectives
Adolescent self reports of emotional adjustment (ESI scores) correlated moderately to strongly with parents’ anxiety/depression ratings on the Vanderbilt (r=.48; p<.0001), but were not related to parental reporting of symptoms of inattention (r=.06; p=.42), hyperactivity/impulsivity (r=.05; p=.54), oppositional defiance (r=.11; p=.16) or conduct problems (r=.15; p=.06). Parent and adolescent CIS scores were also moderately to strongly related (r=.51; p<.0001). However, agreement between parent and adolescent receptivity to the use of psychotropic medications (KAPPA = .09, p = .24) or counseling services (KAPPA = −.02, p = .71) was poor.
Bivariate relationship between parent and adolescent views and past year mental health services use
Past year mental health service use was related to several parent and adolescent perspectives of clinical need and attitudes, and to caregiver strain, but not to sociodemographic characteristics or public or private health insurance coverage. Of the parent perspectives, higher ratings of inattention, anxiety/depression and functional impairment, but not of hyperactivity/impulsivity, ODD or CD symptoms, were associated with obtaining mental health treatment for their adolescent. Positive parent attitudes towards medication and higher levels of caregiver strain were also related to past year mental health service use. Three adolescent-reported perspectives, higher functional impairment, positive attitudes towards medications and lower ADHD stigma perceptions, were associated with obtaining mental health care in the past year. Further details about the comparisons, including estimates, p-values and effect sizes, are shown in Table 1.
Parent and adolescent perspectives as independent predictors of past year mental health services use
As shown in Table 2, parental perceptions of adolescent inattention symptoms and medication receptivity were significant independent predictors of past year mental health service use, as evidenced by statistically significant odds ratios and improved model fit after the addition of each variable. Of the three adolescent perspectives, only the addition of adolescent ADHD stigma perception resulted in further improvement of model fit in Model 6. Higher stigma perceptions significantly lowered the odds of mental health service use.
Stepwise regression confirmed the three predictors from the nested modeling (parental inattention ratings, parent medication receptivity and adolescent ADHD stigma) and identified adolescent-reported functioning as an additional predictor of past year mental health use. As shown in Table 3 each unit increase of parental inattention and adolescent-rated functional impairment raised the odds of service use by 1.2 and 1.1 respectively. Having a medication-receptive parent raised the adolescent’s odds of mental health service use by 3.8, whereas increases in ADHD stigma scores lowered the odds by a factor of five.
DISCUSSION
Overall, findings from this study suggest that a substantial proportion of children at high risk for ADHD drop out of care, and that adolescent perceived stigma about ADHD is influential, above and beyond parent perspectives, in receiving mental health services in the past year. Less than one-half of the cohort youth with ongoing ADHD treatment needs who had ever received mental health services were still receiving them, consistent with other studies reporting high rates of ADHD treatment discontinuation in adolescence [7, 8]. Our study suggests that mental health service receipt in the past year was associated with specific parent- and adolescent-reported need (symptoms and functioning, respectively) and attitudinal variables (medication receptivity and ADHD stigma, respectively), but not with prior mental health treatment or with sociodemographic characteristics.
Study findings suggest that it is important to elicit both parent and adolescent perceptions of clinical need during ADHD assessment and treatment planning. Parents and adolescents had poor agreement on externalizing disorder symptoms, but were more aligned in their perceptions of functional impairment. Interestingly, parental ratings of inattention, but not of hyperactivity/impulsivity, ODD or CD were associated with mental health service use. This finding may reflect the increasing importance of attentional capacities during adolescence, when school assignment become more complex and inattentive ADHD symptoms result in notable performance problems, a clear signal that help is needed. Conversely, behaviors associated with ODD and CD may be interpreted to be typical adolescent misbehavior, a developmental phenomenon that needs to be coped with, but that does not prompt a doctor visit. Our study did not elicit parental explanatory models of adolescent behaviors, thus we can only offer speculation about the underlying reasons for this interesting finding.
Of note, adolescents with ADHD in our study endorsed high rates of functional impairment, even though their psychopathology self-reports were in the normative range. We hypothesize that this discrepancy may be due to adolescents’ concern about stigma associated with acknowledging ADHD symptoms, unlike reporting of functional problems. We suggest that gathering adolescent-reported functioning may add valuable information on clinical need during the ADHD assessment process and provide an opportunity to give voice to adolescent perspectives.
Both parent and adolescent medication receptivity were related to service use, but exhibited no agreement with each other. This was a surprising finding, as one might assume that adolescents are influenced by family attitudes towards medication treatment. Limited research exists on parent-child agreement for treatment receptivity. If confirmed in other studies, our findings emphasize the importance of eliciting both parent and youth medication attitudes during clinical encounters in order to enhance adolescents’ treatment engagement and adherence.
Adolescents’ perception of ADHD stigma emerged as a strong predictor of service use. Stigma related to mental health problems may be particularly influential to service use for teens, as respondents in a national child survey were more likely to make negative attributions about peers with ADHD than peers with asthma, particularly with respect to the likelihood of antisocial behavior and violence [20]. Because concerns about stigma may be particularly pertinent for adolescents who are developmentally sensitive about others’ opinions and seek peer approval, their stigma perceptions may prevent help-seeking or prompt treatment discontinuation.
Surprisingly, sociodemographic characteristics, including gender and race, which were associated with service use in previous studies, did not show an association with treatment receipt in adolescence. Conclusions however about the lack of health disparities cannot be made because our sample size was relatively small, comparisons by race/ethnicity were limited to African-American and Caucasian youth, and the study population was restricted to one public school district population.
Interpretation of these findings should be considered within the context of several other study limitations. External validity may have been limited by study attrition; those lost to follow-up did not differ from participants by sociodemographic characteristics, but may have differed on unmeasured constructs. Conclusions about a causal pathway between adolescent perceptions of medication treatment receptivity and ADHD stigma are also beyond the scope of this study’s design. To address these limitations, future studies examining the extent adolescent perspectives moderate mental health service use should include larger and more ethnically diverse community-based samples.
Despite these limitations, study findings suggest that adolescents exercise control over their ADHD treatment, as their self-assessment of functioning and perceptions of ADHD stigma are associated with mental health services use in the past year. Quality improvement interventions for adolescents with ADHD should include developmentally sensitive psychoeducational interventions that target medication treatment attitudes and stigma about ADHD. Furthermore, pediatricians should consider monitoring adolescent-reported functioning, along with parent-reported ADHD symptom ratings, to gauge treatment response. In this manner pediatricians model shared decision-making for the family and support adolescents’ transition to future independent medical encounters for ADHD care.
Acknowledgments
Source of support: This study was supported by grant RO1MH57399 from the National Institute of Mental Health
(The corresponding author affirms that she has listed everyone who contributed significantly to the work in the Acknowledgements): We would like to thank Li Wei, College of Education, University of Florida for assistance with the statistical analysis, and the parents and adolescents who made the study possible.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Regina Bussing, Departments of Psychiatry, Clinical and Health Psychology and Pediatrics, University of Florida, Gainesville, Florida
Bonnie T. Zima, Department of Psychiatry, University of California, Los Angeles
Dana M. Mason, Department of Psychiatry, University of Florida, Gainesville, Florida
Phillip C. Porter, College of Education, University of Florida, Gainesville, Florida
Cynthia W. Garvan, Florida, College of Education, University of Florida, Gainesville, Florida
References
- 1.Lara C, Fayyad J, de Graaf R, et al. Childhood predictors of adult attention-deficit/hyperactivity disorder: Results from the World Health Organization World Mental Health Survey initiative. Biological Psychiatry. 2009 Jan;65(1):46–54. doi: 10.1016/j.biopsych.2008.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Robin AL, Wender E. ADHD in adolescence: increase SAM’s involvement. Journal of Adolescent Health. 2000;27(5):295–295. doi: 10.1016/s1054-139x(00)00188-9. [DOI] [PubMed] [Google Scholar]
- 3.Clinical practice guideline: treatment of the school-aged child with attention-deficit/hyperactivity disorder. Pediatrics. 2001 Oct;108(4):1033–1044. doi: 10.1542/peds.108.4.1033. [DOI] [PubMed] [Google Scholar]
- 4.Pliszka S. Practice parameter for the assessment and treatment of children and adolescents with attention-deficit/hyperactivity disorder. J Am Acad Child Adolesc Psychiatry. 2007 Jul;46(7):894–921. doi: 10.1097/chi.0b013e318054e724. [DOI] [PubMed] [Google Scholar]
- 5.Barkley RA. Adolescents with attention-deficit/hyperactivity disorder: an overview of empirically based treatments. J Psychiatr Pract. 2004 Jan;10(1):39–56. doi: 10.1097/00131746-200401000-00005. [DOI] [PubMed] [Google Scholar]
- 6.DuPaul GJ, Evans SW. School-based interventions for adolescents with attention-deficit/hyperactivity disorder. Adolesc Med State Art Rev. 2008;19(2):300–312. [PubMed] [Google Scholar]
- 7.Garland A, Zigler E. Psychological correlates of help-seeking attitudes among children and adolescents. American Journal of Orthopsychiatry. 1994;64:586–593. doi: 10.1037/h0079573. [DOI] [PubMed] [Google Scholar]
- 8.Harpaz-Rotem I, Leslie D, Rosenheck RA. Treatment retention among children entering a new episode of mental health care. Psychiatr Serv. 2004 Sep;55(9):1022–1028. doi: 10.1176/appi.ps.55.9.1022. [DOI] [PubMed] [Google Scholar]
- 9.Bussing R, Mason DM, Bell L, et al. Adolescent outcomes of childhood attention-deficit/hyperactivity disorder in a diverse community sample. J Am Acad Child Adolesc Psychiatry. 2010 Jun;49(6):595–605. doi: 10.1016/j.jaac.2010.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Loe IM, Feldman HM. Academic and educational outcomes of children with ADHD. Ambulatory Pediatrics. 2007 Jan-Feb;7(1 Suppl):82–90. doi: 10.1016/j.ambp.2006.05.005. [DOI] [PubMed] [Google Scholar]
- 11.Satterfield JH, Faller KJ, Crinella FM, et al. A 30-year prospective follow-up study of hyperactive boys with conduct problems: adult criminality. J Am Acad Child Adolesc Psychiatry. 2007 May;46(5):601–610. doi: 10.1097/chi.0b013e318033ff59. [DOI] [PubMed] [Google Scholar]
- 12.Andersen RM. Revisiting the behavioral model and access to medical care: does it matter? J Health Soc Behav. 1995;36(1):1–10. [PubMed] [Google Scholar]
- 13.Eiraldi RB, Mazzuca LB, Clarke AT, et al. Service Utilization among ethnic minority children with ADHD: a model of help-seeking behavior. Administration and policy in mental health. 2006 Sep;33(5):607–622. doi: 10.1007/s10488-006-0063-1. [DOI] [PubMed] [Google Scholar]
- 14.Leslie LK, Wolraich ML. ADHD service use patterns in youth. J Pediatr Psychol. 2007 Jul;32(6):695–710. doi: 10.1093/jpepsy/jsm023. [DOI] [PubMed] [Google Scholar]
- 15.Bussing R, Zima B, Gary FA, et al. Barriers to Detection, Help-seeking and Service Use for Children with ADHD Symptoms. Journal of Behavioral Health Services & Research. 2003;30(2):176–189. doi: 10.1007/BF02289806. [DOI] [PubMed] [Google Scholar]
- 16.Tessler R, Mechanic D. Factors affecting children’s use of physician services in a prepaid group practice. Med Care. 1978 Jan;16(1):33–46. doi: 10.1097/00005650-197801000-00003. [DOI] [PubMed] [Google Scholar]
- 17.Podolski CL, Nigg JT. Parent stress and coping in relation to child ADHD severity and associated child disruptive behavior problems. J Clin Child Psychol. 2001 Dec;30(4):503–513. doi: 10.1207/S15374424JCCP3004_07. [DOI] [PubMed] [Google Scholar]
- 18.Bussing R, Zima BT, Gary FA, et al. Social networks, caregiver strain, and utilization of mental health services among elementary school students at high risk for ADHD. J Am Acad Child Adolesc Psychiatry. 2003 Jul;42(7):842–850. doi: 10.1097/01.CHI.0000046876.27264.BF. [DOI] [PubMed] [Google Scholar]
- 19.Goldston DB, Reboussin BA, Kancler C, et al. Rates and predictors of aftercare services among formerly hospitalized adolescents: a prospective naturalistic study. J Am Acad Child Adolesc Psychiatry. 2003 Jan;42(1):49–56. doi: 10.1097/00004583-200301000-00010. [DOI] [PubMed] [Google Scholar]
- 20.Walker JS, Coleman D, Lee J, et al. Children’s stigmatization of childhood depression and ADHD: magnitude and demographic variation in a national sample. J Am Acad Child Adolesc Psychiatry. 2008 Aug;47(8):912–920. doi: 10.1097/CHI.0b013e318179961a. [DOI] [PubMed] [Google Scholar]
- 21.Bussing R, Fernandez M, Harwood M, et al. Parent and teacher SNAP-IV ratings of attention deficit hyperactivity disorder symptoms: psychometric properties and normative ratings from a school district sample. Assessment. 2008 Sep;15(3):317–328. doi: 10.1177/1073191107313888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Shaffer D, Fisher P, Lucas CP, et al. NIMH Diagnostic Interview Schedule for Children Version IV (NIMH DISC-IV): description, differences from previous versions, and reliability of some common diagnoses. J Am Acad Child Adolesc Psychiatry. 2000 Jan;39(1):28–38. doi: 10.1097/00004583-200001000-00014. [DOI] [PubMed] [Google Scholar]
- 23.Kaufman J, Birmaher B, Brent DA, et al. K-Sads-PL. Journal of the American Academy of Child and Adolescent Psychiatry. 2000 Oct;39(10):1208. doi: 10.1097/00004583-200010000-00002. [DOI] [PubMed] [Google Scholar]
- 24.Wolraich ML, Lambert W, Doffing MA, et al. Psychometric properties of the Vanderbilt ADHD diagnostic parent rating scale in a referred population. J Pediatr Psychol. 2003 Dec;28(8):559–567. doi: 10.1093/jpepsy/jsg046. [DOI] [PubMed] [Google Scholar]
- 25.Bird HR, Gould MS, Staghezza BM. Patterns of diagnostic comorbidity in a community sample of children aged 9 through 16 years. Journal of the American Academy of Child and Adolescent Psychiatry. 1993;32(2):361–368. doi: 10.1097/00004583-199303000-00018. [DOI] [PubMed] [Google Scholar]
- 26.Burns BJ, Angold A, Magruder-Habib K, et al. The Child and Adolescent Services Assessment (CASA) Durham, N.C: Duke Medical Center; 1992. [Google Scholar]
- 27.Brannan AM, Heflinger CA, Bickman L. The Caregiver Strain Questionnaire: Measuring the Impact on the Family of Living with a Child with Serious Emotional Disturbance. Journal of Emotional and Behavioral Disorders 1997 Winter. 1997;5(4):212–222. [Google Scholar]
- 28.Berwick DM, Murphy JM, Goldman PA, et al. Performance of a five-item mental health screening test. Med Care. 1991;29(2):169–176. doi: 10.1097/00005650-199102000-00008. [DOI] [PubMed] [Google Scholar]
- 29.Norbeck JS, Lindsey AM, Carrieri VL. The development of an instrument to measure social support. Nurs Res. 1981;30(5):264–269. [PubMed] [Google Scholar]
- 30.Norbeck JS, Lindsey AM, Carrieri VL. Further development of the Norbeck Social Support Questionnaire: normative data and validity testing. Nurs Res. 1983;32(1):4–9. [PubMed] [Google Scholar]
- 31.Reynolds CR, Reynolds CR, Kamphaus RW. The clinician’s guide to the Behavior Assessment System for Children (BASC) New York, NY: Guilford Press; 2002. [Google Scholar]
- 32.Kellison I, Bussing R, Bell L, et al. Assessment of stigma associated with attention-deficit hyperactivity disorder: psychometric evaluation of the ADHD stigma questionnaire. Psychiatry Res. 2010 Jul 30;178(2):363–369. doi: 10.1016/j.psychres.2009.04.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ascher BH, Farmer EMZ, Burns BJ, et al. The Child and Adolescent Services Assessment (CASA): Description and psychometrics. Journal of Emotional & Behavioral Disorders. 1996;4(1):12–20. [Google Scholar]
- 34.Bussing R, Mason DM, Leon CE, et al. Agreement between CASA parent reports and provider records of children’s ADHD services. The journal of behavioral health services & research. 2003 Oct-Dec;30(4):462–469. doi: 10.1007/BF02287433. [DOI] [PubMed] [Google Scholar]