Abstract
Abstract To the extent that men who have sex with men (MSM) use the Internet, it serves as a promising medium for behavioral intervention. The present study sought to investigate the efficacy of a web-based skills training and motivational intervention in a randomized trial (N = 112) conducted completely online. After a detailed assessment, MSM were randomly assigned to an online intervention or a control website. The experimental intervention consisted of risk assessment and feedback, motivational exercises, skills training, and education while the control intervention focused on relaxation skills. Follow-up data were collected 3 months later and analyzed with repeated-measures MANOVA. Although both groups evidenced across-the-board reductions in unprotected sex, perhaps due to the detailed assessment, the experimental group showed greater reductions with the riskiest partners, those of positive or unknown serostatus. Thus, this study gives preliminary evidence that a brief web-based intervention offering cognitive behavioral skills training and motivational enhancement can effectively reduce sexual risk in MSM.
Keywords: HIV prevention, Internet interventions, Web-based prevention, Skills training, Motivation, Reaching young MSM, Reaching rural MSM, Computer-based safer sex intervention
Introduction
According to a recent report by the Centers for Disease Control and Prevention, new, more sophisticated assays that differentiate new from longstanding infections have indicated that the incidence of HIV in the US is higher than previously estimated (CDC 2008; Hall et al. 2008). Back calculations from these assays have indicated that annual HIV incidence peaked in 1984–1985 at 130,000 infections, decreased to a nadir of 49,000 infections in the early 1990s, and has remained relatively stable since 2000 at about 55,000 per year (Hall et al. 2008). The number of infections attributable to intravenous drug use has decreased since the late 1990s; however, HIV incidence among men who have sex with men (MSM) has been steadily increasing since the early 1990s (Hall et al. 2008). Concurrent increases in rates of gonorrhea and syphilis among MSM are also concerning (Wolitski et al. 2001). These STIs increase the efficiency of HIV transmission and are related to more rapid HIV disease progression (Herbst et al. 2005). Increases in HIV and STIs suggest that risky sexual behavior has risen despite advances made in the 1980s and early 1990s.
Several reasons have been postulated for this apparent increase in risky sex. First, improved treatments have decreased the mortality rate of HIV/AIDS and may have led to reduced concern about HIV and sexual risk. In general, younger men have not witnessed as many AIDS deaths as their older counterparts (Vanable et al. 2000). Moreover, the availability of effective antiretroviral medications has been associated with a widely held yet possibly dangerous perception that HIV infection is a manageable, albeit chronic, condition, akin to adult-onset diabetes (Hoy-Ellis and Fredriksen-Goldsen 2007). Seeking sex through Internet chat rooms has also been implicated as a significant contributor to the increase in risky sexual behavior in MSM (Bull et al. 2004; Elford et al. 2004) and was shown to be a factor when syphilis cases went from 48 in 1998 to 495 in 2002 in San Francisco, with MSM accounting for most of the increase in cases (Study Confirms Link 2004). One recent survey found that 48% of the 270 young MSM surveyed had sex with someone they met online (Garafalo et al. 2007). Only 54% of the sample used condoms regularly.
Behavioral interventions to increase condom use and promote other safer sex behavior have been shown to be effective (see Johnson et al. 2008 for a review) with stronger effects observed for interventions that teach interpersonal communication skills, such as condom use negotiation (Johnson et al. 2002; Reitmeijer et al. 2007). The information-motivation-behavioral skills (IMB) model is a commonly used and efficacious model for HIV prevention (e.g., see Carey et al. 1997; Fisher and Fisher 2000) and states that individuals need accurate prevention information, personal and social motivation, and the relevant behavioral skills in order to regularly engage in preventive behavior (Fisher et al. 2002). Although such interventions have been implemented across the US Hall et al. (2008) argued that “their reach must be considerably expanded to accelerate progress” (p. 528). The authors pointed out that, over a recent 1-year period, only about 8 and 15% of MSM had participated in group-level and individual-level interventions, respectively (Sanchez et al. 2006).
To date, most behavioral interventions have been delivered face-to-face (Johnson et al. 2003). Since use of the Internet for dating is related to risky sex, web-based interventions have been seen as a potentially more effective method of reaching those most at risk (Reitmeijer et al. 2007). Delivering an effective intervention via the web has many advantages. Importantly, it makes it possible to reach more people at lower cost, potentially increasing access to difficult-to-reach populations such as rural and minority MSM (Bowen 2005). Moreover, it affords individuals the opportunity to access the intervention privately and confidentially, on their own time, and potentially at critical “teaching opportunities,” such as when they are looking for new sex partners online.
To date only a small number of online safer sex interventions have been tested for efficacy. One popular online format involves public health counselors participating in chat rooms and answering questions about safer sex practices and testing when asked (e.g., McFarlane et al. 2005; Rhodes 2004). A literature search did not find any published record of randomized efficacy trials on this chat-based intervention and this type of one-on-one counseling has limitations (e.g., limited availability, personnel costs). These limitations are not present, however, in the case of multimedia psycho-educational interventions that are scalable, standardized and always available. Bowen and her colleagues (Bowen et al. 2007; Williams et al. 2008), for example, have developed a three-module intervention based on the IMB model which has been found to increase knowledge and self-efficacy and decrease risky sex in a sample of rural MSM over a short follow-up period. A second such intervention, a single-session condom promotion program for 18- to 24-year-olds (Bull et al. 2008), was recently tested in a randomized online study. Bull et al. (2008) were able to recruit a large number of participants, but condom use did not change significantly in the online intervention group.
The purpose of the present study was to evaluate the effectiveness of a single session Internet-delivered multimedia safer sex intervention for young MSM. The goal of the project was to assess the impact of the intervention on self-reported sexual behavior at a 3 month follow-up. We hypothesized that, compared to those assigned to a control condition; those assigned to the experimental condition would report a greater reduction in unprotected sex. Given the strong emphasis on risk reduction in the experimental intervention, we further hypothesized that reductions would be observed in particular for the most risky sexual practices (e.g., receptive anal intercourse versus insertive oral intercourse), and among the most risky partners (i.e., those who were known to be HIV positive or whose HIV status was unknown).
Method
Pilot Testing
In order to evaluate the usability and acceptability of the intervention and the research questionnaires, pilot testing was conducted on a sample of 21 MSM (57% African American, 33% Hispanic, 23% non-Hispanic Caucasian) aged 18–28 (M = 24). Pilot testing procedures were approved by the Western Institutional Review Board (WIRB). The pilot study was conducted with participants recruited in New York, NY, using a desktop computer at the research offices of an organization that specializes in HIV-related research and intervention development and is well regarded in the gay community. Participants completed a battery of questionnaires, reviewed the entire HIV prevention intervention, completed questions to assess usability/acceptability, and participated in a brief semi-structured interview with a study research assistant. They were paid $80 for their time. Feedback on the intervention was positive. No participant reported becoming upset during the intervention or finding any content offensive. Participants had no trouble answering the questionnaires, but found them too long. As a result of feedback during pilot testing, the questionnaire battery was shortened and minor content revisions were made.
Participants
The online intervention was designed for MSM at higher risk of contracting HIV: younger MSM, including minority MSM, who were having unsafe sex. Eligible participants were men aged 18–39 years whose own HIV status was negative or unknown and who had engaged in unprotected sex (oral or anal) with a man within the last 3 months; had access to a Windows-based computer with audio capabilities, Internet service, and Internet Explorer; were willing to provide an active email address for study-related contact; read and understood English; resided in the US; and had not participated in another psychosocial HIV intervention study in the past year.
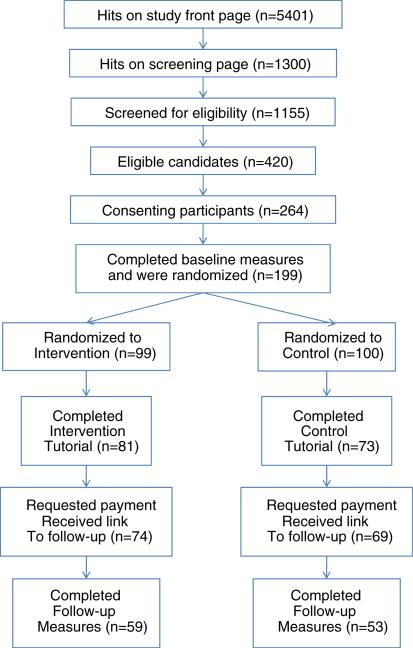
Participants were recruited through banner advertisements posted on same-sex community websites (see Table 1 for more details) and profiles of the study were posted on www.migente.com, www.blackplanet.com, and www.amigos.com. As shown in Fig. 1, the study front page received 5,401 hits during the enrollment period, from 6/20/2006 to 11/16/2006.
Table 1.
Summary of advertising locations and parameters for study recruitment
| Site | Dates | Impressions | Ad clicks | Cities | Regions |
|---|---|---|---|---|---|
| OutinAmerica.com | 6/30/06 | 735,000 | 1,134 | 17 large- and medium-sized cities | N/A |
| Gay.com (PlanetOut Inc.) | 8/15/06–9/15/06 | 9,506,286 | 4,762 | Atlanta | Southern CA |
| Baltimore | AZ | ||||
| Chicago | NM | ||||
| Washington, DC | TX | ||||
| Detroit | |||||
| Gay.com (PlanetOut Inc.) | 9/29/06–11/16/06 | 3,474,298 | Unknown | Los Angeles | Southern CA |
| Miami | AZ | ||||
| New York | NM | ||||
| Philadelphia | TX | ||||
| San Diego | |||||
| San Francisco | |||||
| Manhunt.net | 10/11/06–11/27/06 | 155,771 | 703 | Washington, DC | DE |
| GA | |||||
| MI |
Fig. 1.
Flow diagram showing the number of hits and participants at each stage of the present study
One hundred ninety-nine individuals completed baseline measures and were randomized. Of those, 143 participants completed the intervention (i.e., landed on the last page) and were sent a link to the follow-up measures. Of those, a final N = 112 completed the follow-up measures.
Procedures
The Western Institutional Review Board reviewed and approved all study procedures. The study website was hosted on an SSL server with 128 bit encryption. This server was accessible via the Internet, but the data were stored on a separate server not accessible via the Internet or available to the public. Identifiable information (e.g., name and mailing address) was encrypted and stored on a third server. Users were required to use Microsoft Explorer version 5 or higher (the study site was not compatible with Safari or Firefox). Users were informed of the technical requirements on the study home page. In order to detect users who might attempt to participate multiple times, IP addresses were collected, but cookies were not.
All study participation was completed online. Potential participants viewed a welcome page with a brief description of the study and payment procedures. Informed consent was obtained over the website. Participants read the consent form and then clicked a button (either “I consent” or “I do not consent”). Participants were able to e-mail or call the study research assistant for more information or technical assistance. To ensure participants would be correctly pre/post-matched, all users were automatically assigned a unique user key in the database upon their first visit to the study home page. After screening and consent, each participant registered his email address, and the database user key and email address became linked in the system. This email address was also used for authentication/login and to send the link for the follow-up assessment 3 months later.
Participants were required to complete the baseline assessment in one sitting, but were given 1 week to do so. Baseline questionnaires consisted of short answer text boxes and radio buttons. All participants were asked (but not required) to answer all of the questions. The sex frequency questionnaire, however, was structured so that participants were only shown questions relevant to sexual activities in which they reported having engaged. The baseline assessment took approximately 25 min to complete; the follow-up, 20 min. A page-by-page progress bar was not used.
After completing baseline questionnaires, participants were randomly assigned to complete either the experimental intervention or a control intervention that was not specifically focused on HIV risk. The computerized randomization algorithm used random number tables and was designed to produce a comparable racial and ethnic distribution between groups. Each tutorial took 1.5–2 h to complete and required participants to go through each section sequentially, clicking on each page. Participants were not required to complete the intervention in one sitting but were asked to complete it within 1 week. A “save and quit” function allowed participants to return to the intervention where they left off.
After completing their respective tutorials, participants were presented with a satisfaction questionnaire. Participants then provided a name and address for their first payment ($35). During the 3 month follow-up period, participants could return and view their respective tutorials without restriction.
To complete the follow-up, participants returned to the same site where they accessed the pretest and tutorial to authenticate/log in using the email address they registered with at the pretest. After authentication/login they were automatically redirected to a different site to complete the follow-up questionnaires. After completing the follow-up assessment, participants received a second payment ($50).
Experimental Intervention
The intervention website (now located at http://www.HotandSafeM4M.org) was based on the IMB theory of HIV risk reduction and consisted of seven brief motivational, informational and skills training modules. The format of the material was designed to engage younger men, including those from minority groups. Interactive exercises, multimedia presentation and audio clips of simulated peers were presented as well as didactic material and opportunities to test knowledge on HIV risk topics. The purpose of the intervention was to reduce risk of HIV and other sexually transmitted infections by increasing knowledge of risk factors (e.g., type of sex act, serostatus of partner, drug and alcohol use), providing skills training for safer behavior (e.g., communicating about serostatus and negotiating condom use), and increasing motivation for behavior change. The intervention incorporated several themes and strategies borrowed from Motivational Interviewing (Miller and Rollnick 2002), such as assessing and reflecting readiness to change, using decisional balance exercises to increase motivation for change, and building self-efficacy for change by identifying perceived barriers. Judgmental statements about any particular behaviors were avoided in order to reduce the risk of increasing resistance or defensiveness. An individual's freedoms to choose, as well as his responsibility for his own choices, were emphasized.
The experimental intervention began with an interactive assessment of HIV risk factors, offering targeted feedback based on individual responses. This was followed by a series of mini-assessments gauging readiness to change risky behaviors accompanied by interactive stage-based motivational exercises (e.g., “drag and drop” decisional balance and printable goal-setting exercises). Communication skills training included the topics of sexual rights, differences in communication styles, and sexual safety contracts. Information regarding correct condom use was followed by a true/false quiz about condom use myths. Triggers for risky behavior and alternatives for unsafe sex were presented through problem-solving exercises and audio narratives. Lastly, participants were given a chance to test their knowledge of HIV risk and learn up-to-date information through a quiz-like game. Additional themes in the intervention included the interaction of HIV risk and experiencing depression, trauma, childhood sexual abuse, intimate partner violence, or racism.
Control Intervention
The control intervention was a stress reduction training program, entitled eTranquility, originally developed for the general population. For the present study the content was customized for a younger MSM population by substituting representative photographs. The program consisted of a health-related rationale for stress reduction, description of physiological effects of stress and training in three types of relaxation exercises: diaphragmatic breathing, progressive muscle relaxation, and guided imagery. Audio recorded instructions were provided for all three types of relaxation.
Measures
Demographics
A basic demographics questionnaire was administered at pretest to assess each participant's age, education, and annual income. Comfort with a computer and mouse was rated on a Likert scale ranging from 1 very comfortable to 5 very uncomfortable.
Sexual Practices
At baseline and follow-up, participants reported, by serostatus, the number of male sex partners they had had in the preceding 90 days (Parsons et al. 2003). Then, participants were asked about the number of times they had engaged in various sexual activities with their male partner(s), by serostatus, over the preceding 90 days. For each activity, participants reported the total number of times and the number of times without a condom.
Satisfaction with Intervention
At follow-up, participants rated (on Likert scales ranging from 1 strongly disagree to 5 strongly agree) to what extent they agreed that the intervention was easy to use, attractive, and enjoyable.
Data Analytic Approach
Preliminary analyses were conducted to determine whether there were any baseline demographic differences between men who completed the follow-up assessment and those who did not and, among completers, between those randomly assigned to the control group and those assigned to the intervention group.
In evaluating the effects of the intervention, sexual practices were examined by the number of unprotected acts by type of act. These analyses were conducted for acts reported with all partners, regardless of their reported serostatus, and again for acts reported with partners of positive or unknown serostatus (i.e., excluding partners reportedly known to be seronegative). Raw numbers of unprotected acts were highly skewed. Extreme values three or more standard deviations above the mean were dropped, and the data were log transformed for analysis using multivariate analysis of variance (MANOVA) with repeated measures. The between-subjects variable was experimental condition. The within-subjects variable was time (baseline vs. follow-up). The dependent variables were unprotected anal intercourse in general (UAI), unprotected receptive anal intercourse (URAI), unprotected insertive anal intercourse (UIAI), unprotected receptive oral intercourse (UROI), and unprotected insertive oral intercourse (UIOI). Variables pertaining to satisfaction with the intervention were examined using independent-groups t-tests.
Results
Preliminary Analyses
Table 2 shows demographic data and baseline unprotected sexual practices for the 112 study completers. The mean age was 26.3 (SD = 5.7). Participants reported being very comfortable using a computer and mouse (M = 1.12, SD = 0.6).
Table 2.
Characteristics of participants completing follow-up (N = 112) at baseline
| % | |
|---|---|
| Ethnicity and race | |
| Hispanic/Latino | 15.2 |
| African American | 6.3 |
| Asian American | 5.4 |
| Hawaiian/Pacific islander | 0.9 |
| Native American | 7.1 |
| White | 80.4 |
| Other | 2.7 |
| Annual income | |
| Under $10,000 per year | 16.1 |
| $10,000–$20,000 per year | 19.6 |
| $21,000–$40,000 per year | 35.7 |
| $41,000–$60,000 per year | 20.5 |
| $61,000 or over per year | 8.1 |
| Highest grade completed | |
| <12th grade or GED | 2.7 |
| 12th grade or GED | 13.4 |
| 1 year college/tech school | 11.6 |
| 2 years college/tech school | 13.4 |
| >2 years college/tech school | 58.9 |
| Self-reported HIV status | |
| Negative | 83.9 |
| Positive | 0.0 |
| Unknown | 16.1 |
| UAI | |
| Any partner | 65.2 |
| Positive/unknown partner | 34.8 |
| UIAI | |
| Any partner | 44.6 |
| Positive/unknown partner | 18.8 |
| URAI | |
| Any partner | 51.8 |
| Positive/unknown partner | 26.8 |
| UIOI | |
| Any partner | 92.9 |
| Positive/unknown partner | 54.5 |
| UROI | |
| Any partner | 95.5 |
| Positive/unknown partner | 50.9 |
Baseline Comparison of Study Completers and Non-Completers
Two-sided Pearson chi-square tests revealed that, compared to those who completed the follow-up assessment (n = 112), those who did not (n = 87) were more likely to be African American, 14.9% versus 6.3%, χ2(1, N = 199) = 4.09, P = 0.043, and to report that their HIV status was unknown, 27.6% versus16.1%, χ2(1, N = 199) = 3.90, P = 0.048. There were no other frequency differences in race or ethnicity between completers and noncompleters, nor were there mean differences in age, income, education, or comfort using a computer and mouse. Two-sided Pearson chi-square tests were used to examine whether there were differences between completers and non-completers in prevalence of unprotected sexual activities; no differences were found.
Baseline Comparison of Experimental and Control Groups
Two-sided Pearson chi-square tests revealed that, compared to those in the control group (n = 53), those in the experimental group (n = 59) were more likely to be Asian American, 10.2% versus 0.0%, χ2(1, N = 112) = 5.70, P = 0.017. There were no other differences in race, ethnicity, or HIV status between groups, nor were there mean differences in age, income, education, or comfort with a computer. Two-sided Pearson chi-square tests were used to examine whether there were baseline differences between experimental and control groups in prevalence of unprotected sexual activities. Groups were equally likely to report UAI, URAI, UIAI, UROI, and UIOI, irrespective of partner serostatus. With regard to partners of unknown or positive serostatus, the experimental group was more likely to report UAI in general, 44.1% versus 24.5%, χ2(1, N = 112) = 4.70, P = 0.030; UIAI in particular, 28.8% versus 7.5%, χ2(1, N = 112) = 8.29, P = 0.004; and UIOI, 66.1% versus 41.5%, χ2(1, N = 112) = 6.81, P = 0.009.
Evaluating the Effects of the Intervention
Means and standard deviations for numbers of unprotected acts are shown in Table 3. Results of significance tests and effect sizes (partial η2) are shown in Table 4. Examining unprotected acts with all partners regardless of serostatus, there was a significant multivariate main effect for time. Inspection of the univariate tests indicated that, across groups, numbers of unprotected acts decreased from baseline to follow-up for both groups for all sexual practices. Examining unprotected acts with partners of positive or unknown serostatus, there was also a significant multivariate main effect for time. Inspection of the univariate tests indicated that numbers of unprotected acts with risky partners decreased for AI, RAI, IOI, and ROI, but not IAI. The multivariate main effect for time was qualified, however, by a significant multivariate group by time interaction. Numbers of unprotected acts with risky partners decreased more for the intervention group than for the control group for AI, IAI, IOI, and ROI, but not RAI.
Table 3.
Means and standard deviations for raw numbers of unprotected sex acts, by partner type
| Baseline |
Follow-up |
|||||||
|---|---|---|---|---|---|---|---|---|
| Control |
Intervention |
Control |
Intervention |
|||||
| M | SD | SD | SD | M | SD | M | SD | |
| With any partner regardless of serostatus | ||||||||
| UAI | 10.5 | 15.5 | 6.2 | 11.5 | 6.3 | 13.4 | 4.1 | 10.6 |
| UIAI | 3.3 | 6.9 | 3.4 | 7.6 | 1.9 | 4.6 | 2.1 | 6.1 |
| URAI | 6.0 | 9.4 | 2.9 | 6.2 | 3.0 | 6.9 | 2.0 | 5.5 |
| UIOI | 11.9 | 14.7 | 9.8 | 13.6 | 6.2 | 8.1 | 7.5 | 8.4 |
| UROI | 14.4 | 17.2 | 7.6 | 8.7 | 7.5 | 9.4 | 6.7 | 9.1 |
| With partner of positive/unknown serostatus | ||||||||
| UAI | 1.5 | 4.5 | 2.3 | 5.2 | 0.8 | 1.9 | 0.3 | 0.9 |
| UIAI | 0.2 | 0.8 | 1.0 | 2.6 | 0.2 | 0.5 | 0.2 | 0.9 |
| URA | 1.1 | 3.0 | 1.5 | 4.7 | 0.5 | 1.3 | 0.2 | 0.8 |
| UIOI | 2.2 | 4.1 | 3.5 | 6.3 | 1.5 | 2.9 | 1.2 | 2.3 |
| UROI | 3.0 | 6.8 | 3.0 | 5.4 | 1.4 | 2.8 | 0.9 | 2.3 |
Table 4.
Test statistics for unprotected sex acts, by partner type
| Time effect |
Group × time |
|||||||
|---|---|---|---|---|---|---|---|---|
| F | df | P | η 2 | F | df | P | η 2 | |
| With any partner regardless of serostatus | 3.10 | 5,101 | 0.012 | 0.133 | 1.42 | 5,101 | 0.224 | 0.066 |
| UAI | 12.64 | 1,105 | 0.001 | 0.107 | – | – | – | – |
| UIAI | 6.43 | 1,105 | 0.013 | 0.058 | – | – | – | – |
| URAI | 12.47 | 1,105 | 0.001 | 0.106 | – | – | – | – |
| UIOI | 6.69 | 1,105 | 0.011 | 0.060 | – | – | – | – |
| UROI | 11.76 | 1,105 | 0.001 | 0.101 | – | – | – | – |
| With partner of positive/unknown serostatus | 3.25 | 597 | 0.009 | 0.144 | 4.13 | 597 | 0.002 | 0.175 |
| UAI | 7.59 | 1,101 | 0.007 | 0.070 | 7.59 | 1,101 | 0.007 | 0.070 |
| UIAI | 3.37 | 1,101 | 0.069 | 0.032 | 7.24 | 1,101 | 0.008 | 0.067 |
| URAI | 4.79 | 1,101 | 0.031 | 0.045 | 1.35 | 1,101 | 0.248 | 0.013 |
| UIOI | 13.88 | 1,101 | <0.001 | 0.121 | 7.45 | 1,101 | 0.007 | 0.069 |
| UROI | 13.24 | 1,101 | <0.001 | 0.116 | 8.45 | 1,101 | 0.004 | 0.077 |
Satisfaction with the Intervention
There were no significant differences between the groups on ratings of the intervention's ease of use, M = 4.6 (SD = 0.6), attractiveness, M = 4.2 (SD = 0.7), and enjoyability, M = 4.0 (SD = 0.8).
Discussion
This online study examined the effects of a 90-min Internet-based safer sex intervention on sexual behavior of MSM. The results partially supported our hypotheses. Consistent with previous studies (e.g., Baker et al. 2003), participants in both the control and experimental groups reduced levels of risky sex from baseline to follow-up. We hypothesized that, compared to participants in the control group, those in the experimental group would report a greater reduction in unprotected sex. This was not evidenced without regard to partner serostatus. However, focusing specifically on unprotected sex with partners of positive or unknown serostatus, we found that, compared to the control group, the experimental group did in fact report significantly fewer unprotected acts. We also hypothesized that reductions would be observed for the most risky sexual practices, especially URAI. This was also not observed. Numbers of unprotected acts with risky partners decreased more for the intervention group than for the control group for all sexual practices, except URAI. One possible explanation is that perhaps both groups already knew that URAI with HIV-positive or serostatus-unknown partners was a particularly risky activity and mere completion of the baseline assessment was enough to reduce it. However, the intervention group showed greater reductions in other types of unprotected activities with riskier partners.
The additional benefit observed among participants who engaged in sexual behaviors with riskier partners was expected based on the intervention's strong emphasis on negotiated safety (e.g., discussing serostatus and a focus on reducing risk with HIV-positive and status-unknown partners). Discussing serostatus with a partner is an important risk-reduction strategy. An important effect of the intervention could be to impart to participants the skills or the motivation to reduce or eliminate sex with partners of positive or unknown status. Through discussion, a sexual partner whose serostatus was unknown at baseline may have been recategorized as known-negative at follow-up. Alternatively, participants may have increased their refusal of unprotected sex with partners whose acknowledged serostatus was unknown or positive. Unfortunately, our measures of sexual activities were not specific enough to discriminate between these possibilities. Nonetheless, the assessment of different types of sexual activities by partner serostatus was strength of the present study. Future studies should examine to what extent reductions in unprotected sexual behavior are due to increases in skills versus motivation and by what mechanism reductions with riskier partners in particular are achieved.
Given that the control intervention, a relaxation skills and stress management website for MSM, was devoid of targeted sexual risk-reduction information, it is noteworthy that, across all partner types, the control group reported a reduction in sexual risk behaviors comparable to that of the intervention condition. Mere completion of the baseline measures may have resulted in this effect. Participants in both groups completed a detailed assessment of sexual behavior, and research has shown that assessment itself can serve as an intervention. For example, Kypri et al. (2007) found that students who completed a 10-min online assessment of drinking patterns and associated problems reported significantly lower alcohol consumption and alcohol-related problems 12 months later as compared to those who did not complete an assessment. Presumably, completing a detailed assessment draws individuals’ attention to behaviors that they recognize as unsafe, motivating them to change their behavior. The effect of attention on participant behavior (i.e., the “Hawthorne Effect,” Roethlisberger and Dickson 1939) could also partially explain the change seen in the control group. It is also possible, though we would suspect less likely, that relaxation skills-acquisition by the control group conferred some benefit with regard to sexual risk reduction.
The results of the present study should be considered in light of its limitations. First, consistent with Internet research in general, the present study suffered from low rates of participation by minorities and those of lower socioeconomic status. Recent research has shown that minority groups, those with lower levels of education, and those over 65 continue to be less likely than other groups to use the Internet; however, those gaps are closing (Fox and Pew 2005). While recruiting for this study, we attempted to draw members of ethnic minority groups by targeting advertising to cities with higher percentages of African Americans and Latinos and by advertising on minority-specific Internet sites. Despite these efforts, the number of minority participants in our study remained low, as is common with Internet-based research. Reaching minorities is especially important in the area of HIV prevention research because minority MSM represent some of those at highest risk and in most need of preventative interventions. In order for the field of Internet-based intervention research to progress further, a more diverse audience must be accessed.
Another limitation of the present study was that it was designed in such a way so as to preclude intent-to-treat analysis (Lachin 2000). Those who completed the baseline measures were not provided a link to complete the follow-up measures unless they completed the tutorial to which they were assigned. Thus, no data are available that speak to whether or how the outcome variables would have changed over time among participants who completed only part of the intervention or no intervention at all. Moreover, because the intervention was delivered remotely, there is no reliable information about “dosage” and no assurance that the intervention was completed as intended. For example, although we do know that each enrolled participant clicked on all the pages of the tutorial to which he was assigned, we cannot know to what extent he was truly engaged with the material.
The brevity of the intervention may have limited its effectiveness. It is possible that a longer, more in depth intervention would be more effective; however, we felt that individuals would be more likely to participate in a shorter intervention. Future studies should explore the optimal length for online HIV prevention interventions, but this may be difficult to measure as individuals typically start, stop, and return later to online programs. While this is a limitation for research, the ability to leave and return when one is more motivated is a strength of web-based programs that is generally not easily accomplished with in-person interventions.
In addition to enrolling more minority participants, future studies should assess use of safer sex skills and strategies other than condom use. For example, frequency of conversations about serostatus could be assessed if the intervention specifically targets that behavior, as this one did. More information regarding the effectiveness of specific components of the intervention (e.g., motivational enhancement vs. skills training) would also be useful in addition to data regarding the interaction between individual characteristics and particular intervention components. This intervention attempted to educate young MSM about HIV risk factors including drug and alcohol misuse, mental health issues such as posttraumatic stress disorder and depression, and intimate partner violence. It may be that HIV prevention interventions need to be developed specifically for individuals with these issues. Despite its limitations, the present study provides important preliminary evidence that brief interventions delivered via the Internet can indeed affect HIV risk behavior.
Acknowledgments
Thank you to Miles Glew for all of his work developing the intervention.
This research was conducted with funding from the National Institute of Mental Health, Grant No. R43 MH066465.
Contributor Information
Kelly M. Carpenter, Talaria, Inc., 1121 34th Avenue, Seattle, WA 98122, USA
Susan A. Stoner, Talaria, Inc., 1121 34th Avenue, Seattle, WA 98122, USA
Aneke N. Mikko, Talaria, Inc., 1121 34th Avenue, Seattle, WA 98122, USA
Lynn P. Dhanak, Talaria, Inc., 1121 34th Avenue, Seattle, WA 98122, USA
Jeffrey T. Parsons, Hunter College, Graduate Center, City University of New York (CUNY), New York City, NY, USA
References
- Baker SA, Beadnell B, Stoner S, Morrison DM, Gordon J, Collier C, et al. Skills training versus health education to prevent STDs/HIV in heterosexual women: A randomized controlled trial utilizing biological outcomes. AIDS Education and Prevention. 2003;15:1–14. doi: 10.1521/aeap.15.1.1.23845. doi:10.1521/aeap.15.1.1.23845. [DOI] [PubMed] [Google Scholar]
- Bowen A. Internet sexuality research with rural MSM: Can we recruit and retain them? Journal of Sex Research. 2005;4:317–323. doi: 10.1080/00224490509552287. [DOI] [PubMed] [Google Scholar]
- Bowen AM, Horvath K, Williams ML. A randomized control trial of Internet-delivered HIV prevention targeting rural MSM. Health Education Research. 2007;22:120–127. doi: 10.1093/her/cyl057. doi:10.1093/her/cyl057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bull SS, McFarlane M, Lloyd L, Rietmeijer C. The process of seeking sex partners online and implications for STD/HIV prevention. AIDS Care. 2004;16:1012–1020. doi: 10.1080/09540120412331292426. doi:10.1080/09540120412331292426. [DOI] [PubMed] [Google Scholar]
- Bull S, Pratte K, Whitesell N, Rietmeijer C, McFarlane M. Effect of an Internet-based intervention for HIV prevention: The Youthnet trials. AIDS and Behavior, Electronic version. 2008 doi: 10.1007/s10461-008-9487-9. doi:10.1007/s10461-008-9487-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carey MP, Maisto SA, Kalichman SC, Forsyth AD, Johnson BT, Wright E. Enhancing motivation to reduce the risk of HIV infection for economically disadvantaged urban women. Journal of Consulting and Clinical Psychology. 1997;65:531–541. doi: 10.1037//0022-006x.65.4.531. doi:10.1037/0022-006X.65.4.531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention [14 August 2008];HIV incidence. 2008 from http://www.cdc.gov/hiv/topics/surveillance/incidence.htm.
- Elford J, Bolding G, Davis M, Sherr L, Hart G. The Internet and HIV study: Design and methods. BMC Public Health. 2004;4:39. doi: 10.1186/1471-2458-4-39. doi:10.1186/1471-2458-4-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fisher JD, Fisher WA. Theoretical approaches to individual-level change in HIV-risk behavior. In: Peterson J, DiClemente RJ, editors. HIV prevention handbook. Kluwer/Plenum Press; New York: 2000. pp. 3–55. [Google Scholar]
- Fisher JD, Fisher WA, Bryan AD, Misovich SJ. Information-motivation-behavioral skills model-based HIV risk behavior change intervention for inner-city high school youth. Health Psychology. 2002;21:177–186. doi:10.1037/0278-6133.21.2.177. [PubMed] [Google Scholar]
- Fox S, Pew Internet and American Life Project [8 May 2009];Digital divisions. 2005 from http://www.pewinternet.org/*/media//Files/Reports/2005/PIP_Digital_Divisions_Oct_5_2005.pdf.pdf.
- Garafalo R, Herrick A, Mustanski BS, Donenberg GR. Tip of the iceberg: Young men who have sex with men, the Internet, and HIV risk. American Journal of Public Health. 2007;97:1113–1117. doi: 10.2105/AJPH.2005.075630. doi:10.2105/AJPH.2005.075630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hall HI, Song R, Rhodes P, Prejean J, An Q, Lee LM, et al. Estimation of HIV incidence in the United States. Journal of the American Medical Association. 2008;300:520–529. doi: 10.1001/jama.300.5.520. doi:10.1001/jama.300.5.520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herbst JH, Sherba RT, Crepaz N, Deluca JB, Zohrabyan L, Stall RD, et al. A meta-analytic review of HIV behavioral interventions for reducing sexual risk behavior of men who have sex with men. Journal of Acquired Immune Deficiency Syndromes. 2005;39:228–241. [PubMed] [Google Scholar]
- Hoy-Ellis CP, Fredriksen-Goldsen KI. Is AIDS chronic or terminal? The perceptions of persons living with AIDS and their informal support partners. AIDS Care. 2007;19:835–843. doi: 10.1080/09540120701203360. doi: 10.1080/09540120701203360. [DOI] [PubMed] [Google Scholar]
- Johnson W, Diaz RM, Flanders WD, Goodman M, Hill AN, Holtgrave D, Malow R, McClellan WM. Behavioral interventions to reduce risk for sexual transmission of HIV among men who have sex with men. Cochrane Database of Systematic Reviews (Online : Update Software) 2008;3:CD001230. doi: 10.1002/14651858.CD001230.pub2. [DOI] [PubMed] [Google Scholar]
- Johnson WD, Hedges LV, Diaz RM. Interventions to modify sexual risk behaviors for preventing HIV infection in men who have sex with men. Cochrane Database of Systematic Reviews (Online : Update Software) 2003;1:CD001230. doi: 10.1002/14651858.CD001230. [DOI] [PubMed] [Google Scholar]
- Johnson WD, Semaan S, Hedges LV, Ramirez G, Mullen PD, Sogolow E. A protocol for the analytical aspects of a systematic review of HIV prevention research. Journal of Acquired Immune Deficiency Syndromes. 2002;30(S1):S62–S72. [PubMed] [Google Scholar]
- Kypri K, Langley JD, Saunders JB, Cashell-Smith ML. Assessment may conceal therapeutic benefit: Findings from a randomized controlled trial for hazardous drinking. Addiction (Abingdon, England) 2007;102:62–70. doi: 10.1111/j.1360-0443.2006.01632.x. doi:10.1111/j.1360-0443.2006.01632.x. [DOI] [PubMed] [Google Scholar]
- Lachin JM. Statistical considerations in the intent-to-treat principle. Controlled Clinical Trials. 2000;21:167–189. doi: 10.1016/s0197-2456(00)00046-5. doi:10.1016/S0197-2456(00)00046-5. [DOI] [PubMed] [Google Scholar]
- McFarlane M, Kachur R, Klausner JD, Roland E, Cohen M. Internet-based health promotion and disease control in the 8 cities: Successes, barriers and future plans. Sexually Transmitted Diseases. 2005;32(S10):S60–S64. doi: 10.1097/01.olq.0000180464.77968.e2. doi:10.1097/01.olq.0000180464.77968.e2. [DOI] [PubMed] [Google Scholar]
- Miller WR, Rollnick S. Motivational interviewing: Preparing people for change. 2nd ed. Guilford Press; New York: 2002. [Google Scholar]
- Parsons JT, Halkitis PN, Wolitski RJ, Gomez, the SUMS Team Correlates of sexual risk behaviors among HIV-positive men who have sex with men. AIDS Education and Prevention. 2003;15:383–400. doi: 10.1521/aeap.15.6.383.24043. doi:10.1521/aeap.15.6.383.24043. [DOI] [PubMed] [Google Scholar]
- Reitmeijer CA, Lloyd LV, McLean C. Discussing HIV serostatus with prospective sex partners: A potential HIV prevention strategy among high-risk men who have sex with men. Sexually Transmitted Diseases. 2007;34:215–219. doi: 10.1097/01.olq.0000233668.45976.a1. doi:10.1097/01.olq.0000233668.45976.a1. [DOI] [PubMed] [Google Scholar]
- Rhodes SD. Hookups or health promotion? An exploratory study of a chat room-based HIV prevention intervention for men who have sex with men. AIDS Education and Prevention. 2004;16:315–327. doi: 10.1521/aeap.16.4.315.40399. doi:10.1521/aeap.16.4.315.40399. [DOI] [PubMed] [Google Scholar]
- Roethlisberger FJ, Dickson WJ. Management and the worker. Harvard University Press; Cambridge, MA: 1939. [Google Scholar]
- Sanchez T, Finlayson T, Drake A, Behel S, Cribbin M, DiNenno E, et al. Human immunodeficiency virus (HIV) risk, prevention, testing behaviors—United States, National HIV Behavioral Surveillance System: Men who have sex with men, November 2003–April 2005. MMWR. Surveil-lance Summaries. 2006;55(SS-6):1–16. [PubMed] [Google Scholar]
- Study confirms the link between MSM and web: San Francisco officials use on-line Interventions. AIDS Alert. 2004;19(2):19–20. [PubMed] [Google Scholar]
- Vanable PA, Ostrow DG, McKirnan DJ, Taywaditep KJ, Hope BA. Impact of combination therapies on HIV risk perceptions and sexual risk among HIV-positive and HIV-negative gay and bisexual men. Health Psychology. 2000;19:134–145. doi: 10.1037//0278-6133.19.2.134. doi:10.1037/0278-6133.19.2.134. [DOI] [PubMed] [Google Scholar]
- Williams M, Bowen A, Ei S. An evaluation of the experiences of rural MSM who accessed an online HIV/AIDS health promotion intervention. Health Promotion Practice, Electronic Version. 2008 doi: 10.1177/1524839908324783. doi:10.1177/1524839908324783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolitski RJ, Valdiserri RO, Denning PH, Levine WC. Are we headed for a resurgence of the HIV epidemic among men who have sex with men? American Journal of Public Health. 2001;91:883–888. doi: 10.2105/ajph.91.6.883. doi:10.2105/AJPH.91.6.883. [DOI] [PMC free article] [PubMed] [Google Scholar]