Abstract
Background
Primary care providers are expected to provide lifestyle counseling, yet many barriers exist. Few studies report on adoption and implementation in routine practice. This study reports training, adoption, and implementation of an intervention to promote physical activity (PA) and dietary counseling in community health centers.
Methods
Providers (n = 30) and nurses (n = 28) from 9 clinics were invited to participate. Adopters completed CD-ROM training in stage-matched, patient-centered counseling and goal setting. Encounters were audio recorded. A subsample was coded for fidelity.
Results
Fifty-seven percent of providers and nurses adopted the program. Provider counseling was seen in 66% and nurse goal setting in 58% of participant (N = 266) encounters, although audio recordings were lower. Duration of provider counseling and nurse goal setting was 4.9 ± 4.5 and 7.3 ± 3.8 minutes, respectively. Most PA (80%) and diet (94%) goals were stage-appropriate. Although most providers discussed at least 1 behavioral topic, some topics (eg, self-efficacy, social support) were rarely covered.
Conclusions
A sizeable percentage of providers and nurses completed training, rated it favorably, and delivered lifestyle counseling, although with variable fidelity. With low implementation cost and limited office time required, this model has the potential to be disseminated to improve counseling rates in primary care.
Keywords: lifestyle counseling, primary care, exercise, diet, nutrition
Professional organizations1,2 and Healthy People 20103 recommend that primary care providers deliver brief counseling to promote physical activity (PA) and healthy eating in routine clinical encounters. Rates of such counseling are suboptimal4–7 due to barriers including lack of time, training, reimbursement, and standard easy-to-implement protocols, and low confidence to deliver counseling.8
Relatively few studies of dietary interventions in primary care have been published, but more have been done in the area of PA.8–10 Most primary care-based PA interventions have focused on the efficacy or effectiveness of the intervention,8 and researchers have called for more systematic investigation and reporting of other dimensions discussed in the RE-AIM model,11–13 including patient and primary care provider reach and representativeness, intervention adoption rates, and implementation fidelity.14 In addition, more trials that investigate lifestyle counseling that is integrated into routine care are needed,8,9 as are trials that use multidisciplinary models in which primary care providers recommend PA and make referrals to other health professionals and community resources to lessen time burdens.10 Finally, effective interventions for ethnically and racially diverse populations are needed.8,10,15
African American women are at increased risk for cardiovascular disease morbidity and mortality relative to white women.16 The high prevalence of cardiovascular disease risk factors, including hypertension, overweight, obesity, physical inactivity, high saturated fat diets, and diabetes, among African American women contribute to these health disparities.16 Lower socioeconomic status among African Americans is another important contributing factor.17,18 A greater appreciation of cultural factors that influence physical activity and dietary behaviors is needed to advance interventions in this area.19
Primary care centers are appealing settings for addressing lifestyle behaviors because of their broad reach. Community health care centers, in particular, may hold promise for eliminating disparities because they provide the largest proportion of comprehensive primary health care services to medically underserved and vulnerable populations. About 66% of health care center patients are minorities, 90% have incomes 200% below the federal poverty line, and 39% have no health insurance.20,21 Thus, they are able to reach underserved populations at risk.
The Heart Healthy and Ethnically Relevant (HHER) Lifestyle Program, reported in this paper, is responsive to many of these research gaps. Primary care provider counseling was incorporated into routine clinical visits; financially disadvantaged African American women were study participants; primary care provider reach, adoption, and implementation were tracked; and a multidisciplinary intervention model was used. In response to limitations to the literature described above, the purpose of this paper was to describe the training, adoption, and implementation of the HHER Lifestyle Program standard care intervention to promote PA and a low fat diet in primary care settings serving financially disadvantaged African American women. It is expected that describing adoption and implementation of behavior change counseling will provide useful but underreported information for others wishing to conduct primary care-based interventions.
Methods
Study Overview
The 4-year study began in 2004. The primary goal was to increase moderate intensity PA and reduce the intake of saturated and trans fat. The University partnered with 2 federally funded community health centers (Columbia, SC, and Orangeburg, SC) and worked with 9 clinics within them.
African American women over the age of 35 years who were patients of participating primary care providers and had clinic visits scheduled were sent letters inviting them to participate. We targeted women age 35 years and older because the prevalence of cardiovascular disease risk factors including hypertension, obesity, hyperlipidemia, and physical inactivity increases during this period; women are generally beyond child-bearing years; and our pilot work was conducted with this age population, thus providing us with more direct experience with this population Exclusion criteria included being functionally incapable of meeting the PA goals, blood pressure during the baseline assessment of ≥ 160/95 mmHg, myocardial infarction within the last 6 months, insulin dependent diabetes, pregnancy, or unable or willing to complete survey instruments. A total of 1623 letters were mailed between May 2005 and February 2007. Of these, 24 women returned a postcard requesting no further contact, 60 letters were returned as undeliverable, and 986 women were unable to be reached by telephone. Of the 553 women contacted by telephone, 88 immediately refused to answer questions, 13 were ineligible, 42 needed medical clearance to participate but did not receive it, 60 were eligible but did not complete a baseline visit, and 350 completed a baseline visit (conducted at the woman's home at least 1 week prior their scheduled clinic visit). Of those completing a baseline visit, 3 were ineligible, 34 needed medical clearance to participate but did not receive it, 47 were eligible but did not see their health care provider, and 266 women were ultimately enrolled into the study.
The standard care intervention was delivered to all study participants during a routine clinic visit. In the participating community health centers, the face-to-face patient encounter is delivered by a physician (MD or DO), nurse practitioner, or physician's assistant. These individuals are subsequently referred to as the “providers.” Ancillary support to the providers including obtaining the reason for the visit, documenting the patient's vital signs, verifying medication lists at the beginning of the visit, and assisting with various tasks at the conclusion of the visit (including patient education) is provided by registered and licensed practical nurses, subsequently referred to as the “nurses.” Providers were trained to deliver brief (2–4 minutes) counseling designed to increase their patient's readiness for change or actual behavioral change (depending on the patient's readiness for change) in the area of PA and diet using stage-matched,22 patient-centered counseling. Providers were trained to acknowledge and praise the patient's participation in the study, acknowledge her behavioral readiness for PA and dietary fat change, select at least 1 stage-appropriate behavioral topic for discussion for each behavior (eg, overcoming barriers, social support, goal setting), and state that a nurse would help the patient set goals for change. The use of empathy and open-ended questions was encouraged. Nurses were trained to engage participants in 5 to 10 minute stage-matched goal setting. Like providers, they were trained to acknowledge and praise the patient's participation in the study, acknowledge her behavioral readiness for PA and dietary fat change, select at least 1 stage-appropriate behavioral topic for discussion for each behavior, and assist the participant in selecting her own stage-appropriate goals for both behaviors. Examples of goals included making a list of the pros and cons of walking/eating a low fat diet (precontemplation or contemplation), beginning to trim visible fat from meats (preparation), and making a list of times when walking will be difficult and ways to still be able to walk during these times (action or maintenance). Following the standard care intervention, half of the participants were randomized to receive 12 months of telephone counseling delivered by HHER Lifestyle Program health educators or to a control group. Recruitment of participants and delivery of the standard care intervention are complete and are the focus of this paper.
This study was approved by the university institutional review board. An informed consent form was reviewed with each participant and signed before the baseline visit.
Training of Providers and Nurses
Our pilot study indicated that health care providers preferred flexible, self-paced training. Thus, we developed a CD-ROM that contained a video introduction, 5 training modules, and a video conclusion (content described in Table 1), along with a corresponding training manual. The CD-ROM was piloted with 2 physicians and 1 nurse outside the community health centers and was reviewed by an external consultant and modified appropriately.
Table 1.
Description of the CD-ROM modules
| Module | Content |
|---|---|
| Module 1 | • Importance of physical activity and low fat eating |
| • Epidemiology of cardiovascular disease | |
| • Risk factors for cardiovascular disease | |
| • Physical activity and nutrition basics | |
| • Current physical activity and dietary recommendations54,55 | |
| Module 2 | • Patient-centered counseling and goal setting |
| • Primary care provider's role in improving dietary and physical activity patterns of patients | |
| • Evidence supporting the efficacy of provider counseling | |
| • Professional organization recommendations for counseling | |
| • Training in the Transtheoretical Model (22) to guide counseling (primary care providers) and goal setting (nurses) | |
| • Because the intervention strategies are similar for precontemplation and contemplation and action and maintenance, providers and nurses were trained to view patients in 1 of 3 stages: Stage 1 (not ready for change), Stage 2 (beginning to change), or Stage 3 (making changes). Collapsing stages also made the intervention easier to remember and deliver. | |
| • Patient-centered counseling strategies (eg, empathy, active listening) | |
| • Strategies for effective goal setting (nurses) | |
| Module 3 | • How to deliver the HHER Lifestyle program protocol in clinics (logistics) |
| Module 4 | • Three videos demonstrating stage-matched, patient centered provider counseling for pseudo-patients in different stages of change |
| Module 5 | • One video demonstrating nurse goal setting |
| • Two text-based scripts of goal setting sessions |
Note. Knowledge-based posttests (10 items each) were administered after Modules 1–3.
The CD-ROM was evaluated with 16 items focused on the extent to which the training and stage-based counseling were expected to benefit their practice. All items were rated on a 5-point Likert scale (1 = strongly disagree, 5 = strongly agree).
Health Care Provider Adoption
All providers and nurses at targeted clinics were invited to attend a kick-off dinner or lunch. The purpose of this event was to introduce the study and study staff to community health care clinic staff, increase awareness of the need for provider counseling and nurse goal setting, and create interest and excitement in participating. At the end of the kick-off event, attendees received the training manual and CD-ROM. The training was approved for 7.5 continuing medical education credits and 7.2 continuing education units. Providers and nurses completed training on their own and submitted 3 knowledge-based posttest exams and a training evaluation.
As new providers and nurses joined the clinics, they were contacted by study staff and invited to join the study. Providers and nurses were tracked to report the percentage that adopted the program, ended their participation because they left the clinics, and withdrew from the study.
Measures of Implementation and Fidelity
Each week participating clinics received a fax containing HHER participants with clinic visits scheduled in the upcoming week. The fax contained the patient name, provider's name, and the patient's stage of change for PA and low fat eating. Stage of change was assessed during the home measurement visit (conducted by HHER study staff) to reduce burden for health care staff and to ensure it was collected accurately and in a uniform way across participants. Clinics faxed this list back to study staff at the end of the week and reported whether the participant was seen and received study counseling.
Providers and nurses were instructed to audio record the portion of the clinic visit devoted to the study for every participant. A nurse liaison(s) selected folders (color-coded based on stage of change) for study patients. The folders contained a stage-appropriate diet goal sheet in triplicate, a walking goal sheet in triplicate (nurse circled the patient's stage of change to direct goal selection), a local PA and dietary resource guide, 2 ethnically-tailored educational materials (walking and low fat), and information about reading food labels and the Dietary Approaches to Stop Hypertension (DASH) diet plan.23,24 The DASH diet plan emphasizes increasing intake of fruit, vegetables, and whole grains and reducing intake of fat and sodium. Nurses and providers also received a pocket-sized laminated counseling tool (folded in an accordion fashion) that contained a panel with the study steps, a panel with the counseling flowchart, 2 panels for easily assessing stage of change (one for PA and one for dietary fat, created for use in follow-up visits or with other participants), and a separate panel with suggestions for each stage of change (Stage 1 = precontemplation/contemplation, Stage 2 = preparation, and Stage 3 = action/maintenance)
Interaction time was assessed for all tapes, and 20% (which included the first audio-taped encounter for each provider) were evaluated to determine whether recommended practices were followed. Participant-provider and participant-nurse interactions were rated for the extent to which topics and approaches covered in training were demonstrated (listed in results section). Tapes were reviewed by 4 raters and were all trained by a coinvestigator (who was also one of the 4 raters) who reviewed tapes and ratings for each rater until at least 85% agreement was achieved. Interrater reliability coefficients (Kappa) of ratings ranged from .88 to .97.
Statistical Analyses
Means (standard deviations) were computed to describe participant characteristics and evaluation ratings that were on a continuous scale (eg, body mass index). Frequencies were computed to describe participant and provider characteristics that were categorical. Chi-square analyses examined whether adoption rates and counseling/goal setting rates differed by gender, type of practice, professional degree, or health center.
Results
Participant Characteristics
A total of 266 African American women were recruited into the study (250 from the Columbia center, 16 from the Orangeburg center). Participants averaged 51.2 (10.8) years of age. Close to half (46.2%) were employed full-time. Nearly a third of participants (32.3%) were married, with another 39.8% separated or divorced. A majority (70.3%) reported a household income of less than $30,000 per year, and the mean education was 13.1 (2.7) years. The most common health conditions were hypertension (61.6%), high cholesterol (34.8%), and type 2 diabetes (17.9%). The mean body mass index, 34.9 (9.2) kg/m2, was in the obese category. Almost one-fifth (19.1%) of participants reported current smoking.
Provider Adoption and Retention
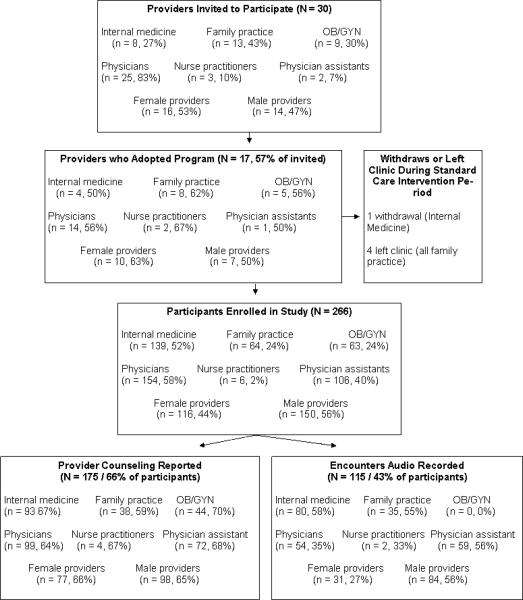
Thirty providers from 9 clinics were invited to participate (Figure 1). Seventeen providers (57%) agreed to participate and completed the required training. Adoption was unrelated to gender, type of practice, professional degree, or health center, P values > 0.10. Only 1 provider withdrew from the study, but 4 of the 17 trained providers (24%) left the clinic before the standard care portion of the study ended.
Figure 1.
Provider adoption and implementation of study protocol. The bottom 2 boxes report the number and percentage of encounters where provider counseling was reported (left side) and counseling was audio recorded (right side) relative to the total number of participants seen at that clinic type, by provider degree, and by provider gender.
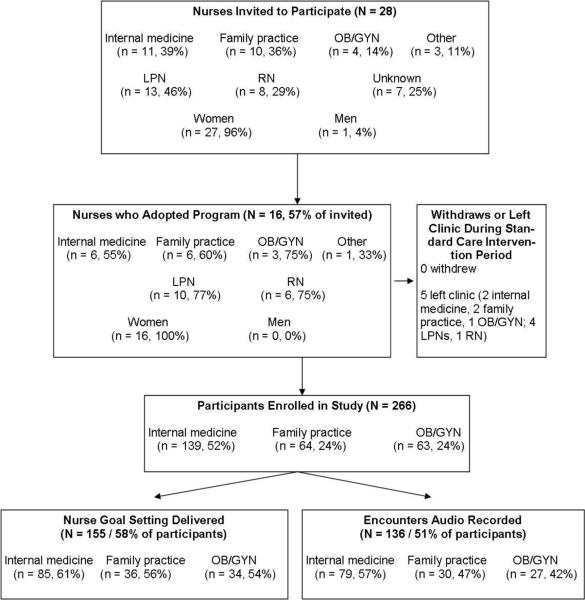
Nurse adoption and retention
Twenty-eight nurses from 8 clinics were invited to participate (Figure 2). Sixteen nurses (57%) agreed to participate and completed the required training. All adopters were women. Adoption was unrelated to type of practice. More nurses from the Columbia (76%) than the Orangeburg health center (27%) adopted the program (P = .01). We could not examine the association between professional degree and adoption because of missing information from nurses who did not enroll. No nurse withdrew from the study; however, 5 of the 16 trained (31%) left the clinic before the standard care intervention ended.
Figure 2.
Nurse adoption and implementation of study protocol. The bottom 2 boxes report the number and percentage of encounters where goal setting occurred (left side; as evidenced by completed goal setting sheets or an audio recording of encounter) and goal setting was audio recorded (right side) relative to the total number of participants seen by clinic type.
Provider and Nurse Evaluations—CD-ROM Training
Eleven of 17 providers and 15 of 16 nurses completed training evaluations. The mean rating across items was 4.14 (range: 3.64–4.45; α = .82) for providers and 4.14 (range: 3.87–4.38, α = .89) for nurses (Table 2). Providers were least likely to agree with statements that they had learned new information about PA and nutrition. They were most likely to agree with statements that stage-matched lifestyle counseling would benefit their practice and is something providers should do. Nurses were least likely to agree with statements that they learned new information about nutrition and that the amount of detail presented about PA and nutrition was about right. They were most likely to agree with statements that the video segments were useful. The average score on the 3 knowledge-based posttests was 91 ± 6% and 90 ± 7% for providers and nurses, respectively.
Table 2.
Provider and Nurse Evaluations of CD-ROM Training
| Item | Provider mean (SD) (N = 11) | Nurse mean (SD) (N = 15) |
|---|---|---|
| Learning stage-matched lifestyle counseling (goal setting) will benefit my practice | 4.36 (0.50) | 4.33 (0.49) |
| Stage-matched lifestyle counseling (goal setting) will be more effective than conventional lifestyle counseling. | 4.09 (0.70) | 4.27 (0.59) |
| I am confident that I can deliver stage-matched physical activity counseling (goal setting) to my patients. | 4.27 (0.65) | 4.07 (0.59) |
| I am confident I can deliver stage-matched dietary counseling (goal setting) to my patients. | 4.27 (0.65) | 4.07 (0.59) |
| I am confident I can implement the HHER Lifestyle Program in my practice. | 4.00 (0.45) | 4.00 (0.53) |
| I learned information about physical activity that I did not know before this training. | 3.64 (1.36) | 4.00 (0.76) |
| I learned information about nutrition that I did not know before this training. | 3.64 (1.29) | 3.93 (0.80) |
| The information I learned about physical activity will benefit my practice. | 4.27 (0.47) | 4.20 (0.56) |
| The information I learned about nutrition will benefit my practice. | 4.27 (0.47) | 4.00 (0.85) |
| The detail presented about physical activity was about right (providers) / Too much detail was presented about physical activity (nurses; ratings were reverse scored) | 4.18 (0.40) | 3.92 (0.95) |
| The detailed presented about nutrition was about right (providers) / Too much detail was presented about nutrition (nurses; ratings were reverse scored) | 4.09 (0.54) | 3.87 (1.06) |
| The video demonstrations of stage-matched counseling were helpful. | 4.18 (0.75) | 4.38 (0.51) |
| The video demonstration of stage-matched goal setting was helpful. | 4.18 (0.75) | 4.38 (0.51) |
| Lifestyle counseling is an activity providers should do / Lifestyle counseling is an important activity for nurses | 4.45 (0.52) | 4.33 (0.62) |
| CD ROM training is an effective way to learn about lifestyle counseling | 4.00 (0.63) | 4.20 (0.56) |
| I would recommend this training to a colleague. | 4.27 (0.47) | 4.33 (0.49) |
| Mean (SD) of the 16 items | 4.14 (0.37) | 4.14 (0.40) |
Note. 1 = strongly disagree; 2 = disagree; 3 = neutral; 4 = agree; 5 = strongly agree.
Intervention Implementation and Fidelity—Audio Recording and Duration of Counseling and Goal Setting
According to fax reports from clinics, 175 participants (66%) received provider counseling (3 received counseling after randomization), and rates did not differ by type of practice, provider gender, provider degree, or health center, P values > .10 (Figure 1). Only 115 audio tapes were submitted that documented provider counseling (43% of all participants). Internal medicine and family practice providers (P < .0001), male providers (P < .0001), and the physician assistant (P = .004) were the most likely to audio-record encounters. Recording did not differ by health center (P = .11). The average length of provider counseling was 4.57 ± 4.38 minutes.
A total of 136 audio tapes were submitted that documented nurse goal setting (51% of participants; Figure 2). In 7 of these cases, there was no trained nurse yet available at the clinic so the provider delivered the counseling and goal setting. PA goal sheets were submitted for 146 participants (55%), and diet goal sheets for 140 participants (53%). There was evidence of goal setting (audio tape or goal sheet) for 155 participants (58%). Type of clinic and health center were unrelated to audio recording and goal setting (P values > .10). The average length of goal setting was 7.20 ± 4.38 minutes.
Intervention Implementation and Fidelity—Stage-Appropriateness of Goals
Among participants with PA goal sheets (n = 146), 2.80 ± 2.54 goals were selected and 80% were stage appropriate. Among participants with diet goal sheets (n = 140), 4.56 ± 3.45 goals were selected and 94% were stage appropriate.
Intervention Implementation and Fidelity—Intervention Fidelity
Thirty-seven provider and 40 nurse audio tapes were reviewed and coded for whether recommended elements of the intervention were delivered (see Tables 3 and 4). Most providers explicitly acknowledged that their patient was enrolled in the study, and just over half summarized study goals. Providers rarely described the participant's stage of change for PA or diet. Most providers covered at least 1 behavioral topic, with benefits/barriers and pros/cons most common and self-reward, self-efficacy and social support least common. Empathy and encouragement were shown in most encounters, open-ended questions were used in over half of encounters, but in a lower percentage of encounters, providers asked their patients if they had any questions or recognized their patients' progress.
Table 3.
Percentage of Encounters Where Providers Discussed Recommended Counseling Topics or Demonstration of Counseling Skills (N = 37 Encounters Evaluated)
| Content area | Topic discussed/counseling skill demonstrated | % |
|---|---|---|
| Discussion of study | Acknowledged study participation | 81 |
| Summarized study goals | 51 | |
| Discussion of stage of change | Describes current physical activity stage of change | 14 |
| Describes current low fat diet stage of change | 11 | |
| Discussion of behavioral topics | Addressed at least 1 behavioral topic in relation to physical activity | 86 |
| Barriers and benefits | 57 | |
| Pros and cons of change | 43 | |
| Self-efficacy | 22 | |
| Social or environmental support | 27 | |
| Self-reward | 0 | |
| Past physical activity experiences | 54 | |
| Addressed at least 1 behavioral topic in relation to eating a low fat diet | 70 | |
| Barriers and benefits | 54 | |
| Pros and cons of change | 43 | |
| Self-efficacy | 16 | |
| Social or environmental support | 5 | |
| Self-reward | 3 | |
| Past low fat diet experiences | 32 | |
| Referral to nurse | Stated that provider was referring patient to nurse for goal setting | 49 |
| Facilitative communication | Asked if participant had questions | 30 |
| Provided empathy or encouragement | 73 | |
| Used open-ended questions | 57 |
Table 4.
Percentage of Encounters Where Nurses Discussed Recommended Counseling Topics or Demonstrated Counseling Skills (N = 40 Encounters Evaluated)
| Content area | Topic discussed/counseling skill demonstrated | % |
|---|---|---|
| Discussion of study | Introduces or summarizes study | 40 |
| Discussion of stage of change | Describes current physical activity and diet stage of change | 20 |
| Discussion of behavioral topics | Addressed at least 1 behavioral topic in relation to physical activity | 60 |
| Addressed at least 1 behavioral topic in relation to a low fat diet | 58 | |
| Past experiences | Asks participants about present/past physical activity and diet experiences | 20 |
| Goal setting | Reviews goal sheet and helps participant select physical activity goals | 83 |
| Reviews goal sheet and helps participant select dietary goals | 88 | |
| Self-efficacy | Assesses participant's physical activity goal self-efficacy | 23 |
| Assesses participant's diet goal self-efficacy | 15 | |
| Summary | Clarification of physical activity goals | 48 |
| Clarification of diet goals | 50 | |
| Emphasizes feasibility of goals | Discusses feasible and realistic progress in physical activity | 20 |
| Discusses feasible and realistic progress in diet | 13 |
In 40% of encounters, the nurse introduced or summarized the study. Like providers, few encounters involved discussing the participant's stage of change. Discussion of behavioral topics was common, although nurses rarely discussed the participants' past experiences and rarely assessed their confidence to meet goals. As expected, discussion regarding goal setting was noted in most encounters. Nurses clarified and repeated back goals at the end of the session in about half of the encounters, but they rarely emphasized the concept of starting slow and progressing.
Discussion
Despite professional mandates,1 primary care providers deliver PA and dietary counseling in routine clinical encounters at suboptimal levels.4–7 A sizeable number of studies have examined the efficacy of PA behavioral interventions in primary care settings,8–10,15,25,26 yet few address external validity.8 A recent review also found that very few studies reported on implementation dose and fidelity.14 Interventions will have a public health impact only if they are widely adopted and disseminated. Interventions that are moderately efficacious but reach large numbers have greater potential to improve health than highly efficacious interventions that reach small numbers.12,13,27,28 This paper described training, adoption, and implementation of a standard care intervention to promote PA and healthy eating in primary care settings.
There are several unique strengths of this study. The HHER Lifestyle Program targeted primary care providers and African American female patients from community health centers. Community health centers may be a more challenging setting to deliver lifestyle counseling as patients may only seek care for more serious or comorbid problems, leaving less time for such counseling. Financially disadvantaged African American women, with few exceptions,29–35 have not been the target of clinic-based PA and dietary interventions even though they experience disproportionate health burdens. All providers and nurses from selected clinics were invited to enroll in the study, thus allowing us to calculate adoption rates in and across clinics. Training was delivered via a self-paced CD-ROM which has potential for wider dissemination. The provider counseling and nurse goal setting was also integrated into routine clinical practice allowing us to test implementation in real world encounters, enhancing generalizability. In contrast, most primary care interventions have been delivered outside of the context of routine clinical visits.9 Encounters were audio recorded which allowed us to time length of counseling and examine protocol fidelity. Finally, by evaluating a standard care (vs. usual care) intervention, we were able to study variations in adoption rates of a recommended clinical practice in real-world settings.
This paper provides important and practically useful information regarding training providers and nurses from primary care settings to implement lifestyle counseling. The most commonly reported barriers to physical activity counseling by primary care providers include lack of time, limited patient receptiveness, lack of remuneration, and limited counseling skills.8 This study addressed a number of these issues by making the intervention easy and efficient to deliver and by training providers and nurses in counseling skills. Just over half of all health care providers invited to participate did so by satisfactorily completing training, and retention of providers was high. These rates of adoption and retention are substantial considering the study was not required and training was completed “on their own time.” Evaluations shed light on these findings. Both providers and nurses rated lifestyle counseling as an important activity that they “should do,” suggesting that health care providers may be responsive to lifestyle counseling if it is brief and easy to implement and if they can be trained at their convenience. The intervention did not require significant additional investments from the health care centers other than the time required to deliver the counseling and goal setting. If implemented outside of a research project, clinics would need to integrate the brief stage assessments into practice and provide the educational materials. Our counseling materials included a very brief stage assessment that providers could use on subsequent visits (not assessed) or with other patients. Nonetheless, the potential for disseminating this type of training and intervention is high. This study also provides data lacking in the literature, as the majority of studies have not reported the adoption rates by health care providers and typically rely on convenience samples of providers.8
There were notable challenges and limitations, however. First, although only 1 provider withdrew from the study, we experienced substantial organizational challenges with one of the health care centers such that a very small percentage of their patients were ultimately enrolled. The greater distance between the university and this center, combined with less organizational support and a transition in their clinic data system, may have contributed to communication challenges. Second, although OB/GYN providers reported comparable counseling rates, none of their study encounters were audio recorded, which prevented us from verifying counseling delivery or quality. OB/GYN providers expressed resistance to audio recording early on, and they saw the study as an additional burden on their time. PA and dietary counseling may not be as salient for these providers who may need to prioritize topics more closely related to their practice. Unfortunately, we did not collect information regarding reasons why providers and nurses did not audio record or implement the counseling or goal setting, nor do we know participants' receptivity to it. Finally, turnover of trained providers and nurses at the clinics was substantial. Turnover is a real-world challenge in community-health centers and could pose a challenge to implementing lifestyle counseling. Our mode of training (CD-ROM), however, was very accommodating to efficiently bringing new health care providers on board.
In this real-world, effectiveness trial, rates of counseling were fairly high. Almost two-thirds of patients received provider counseling, although provider counseling could only be verified in 43% of encounters (ie, not all counseling encounters were audio-taped). Nurse goal setting was delivered at similar rates. On average, providers spent 5 minutes and nurses spent 7 minutes delivering the intervention. There is evidence that brief encounters yield positive behavioral changes,1,9 particularly when they incorporate multiple health professionals (to spread the time burden) and community resources.36–39 For example, Ackermann et al found that training providers to deliver brief exercise advice and make referrals to community exercise programs, particularly for patients in the contemplation stage of change, enhanced physical activity participation relative to usual care.36 Behavioral changes in our trial will be the topic of a forthcoming paper (analyses are underway).
There were clear strengths and weaknesses in intervention implementation. In the majority of reviewed encounters, providers positively acknowledged participation in the study and addressed at least 1 behavioral topic. Providers were most likely to discuss barriers (cons) and benefits (pros) to change and past PA experiences. Providers demonstrated empathy and/or encouraged their patient in the majority of encounters. Nurses were rated most favorably in helping participants select appropriate goals and discussing behavioral topics. Indeed, the majority of goals selected by the participants were stage-appropriate. In terms of areas that could be improved, providers and nurses were rarely explicit in discussing with the patient her stage of change. Providers often did not ask if the patient had questions. Nurses generally did not assess whether goals selected were realistic. These topics could be emphasized more in training. In addition, a broader range of behavioral topics, tailored to the patient's stage and unique circumstances, could be emphasized. For example, concerns about safety, financial constraints, lack of transportation, role-strain, putting one's own needs last, acceptance of a larger body size, and health conditions have been shown to be barriers to physical activity in women, particularly African American women.40–49 Financial constraints, lack of availability of healthy food choices, and food insecurity have been shown to be major barriers to healthy eating in African American women.49–53 Lastly, self-efficacy and social support, both known to be strongly related to PA and dietary change, were rarely discussed.
In summary, primary care represents a key opportunity for providing PA and dietary counseling. Primary healthcare providers and nurses are expected to provide advice on healthy lifestyles, but struggle to find time to counsel patients and often lack the necessary training and support to do so effectively. We found that self-paced, CD-ROM training is acceptable, and posttest scores suggest that it is effective at increasing knowledge (unfortunately, pretests were not administered). Data on intervention fidelity also support the effectiveness of the training. The low cost and limited time required during the patient encounter greatly improve the likelihood of successfully incorporating an intervention into routine primary care. As such, the standard care intervention of the HHER Lifestyle Program represents a reasonable approach to overcoming many of the barriers to providing PA and dietary counseling in primary care settings.
Acknowledgments
We are especially grateful to all of the women who participated in this study. We also thank the providers and nurses at the Eau Claire Cooperative Health Center and Family Health Center, Inc. for their participation as well as their time and feedback regarding the study protocols. In addition, we thank Dr. Alice Ammerman from the University of North Carolina at Chapel Hill for providing consultation and feedback regarding the development of the nutrition training content. Finally, we acknowledge the substantial contributions of staff and investigators who have participated in HHER Lifestyle Program: Cheryl L. Addy, Tiffany N. Barker, Alisa Brewer, Shamika Brown, Elizabeth Mayer-Davis, Tina Devlin, Elizabeth Fallon, Elizabeth Fore, Monetha Gaskin, Desireé Hammond, Genova McFadden, Keri Noris, Lisa Wigfall, and Dawn Wilson. Intervention materials can be obtained by writing to the first author. This project was funded by a grant from the National Heart Lung and Blood Institute (HL073001).
References
- 1.Jacobson DM, Strohecker L, Compton MT, Katz DL. Physical activity counseling in the adult primary care setting: position statement of the American College of Preventive Medicine. Am J Prev Med. 2005;29(2):158–162. doi: 10.1016/j.amepre.2005.04.009. [DOI] [PubMed] [Google Scholar]
- 2.Fletcher GF. How to implement physical activity in primary and secondary prevention. A statement for healthcare-professionals from the Task Force on Risk- reduction, American Heart Association. Circulation. 1997;96(1):355–357. doi: 10.1161/01.cir.96.1.355. [DOI] [PubMed] [Google Scholar]
- 3.US Department of Health and Human Services . Healthy People 2010: Understanding and improving health. 2nd ed. US Government Printing Office; Washington, DC: 2000. [Google Scholar]
- 4.Ma J, Urizar GG, Jr, Alehegn T, Stafford RS. Diet and physical activity counseling during ambulatory care visits in the United States. Prev Med. 2004;39(4):815–822. doi: 10.1016/j.ypmed.2004.03.006. [DOI] [PubMed] [Google Scholar]
- 5.Glasgow RE, Eakin EG, Fisher EB, Bacak SJ, Brownson RC. Physician advice and support for physical activity: results from a national survey. Am J Prev Med. 2001;21(3):189–196. doi: 10.1016/s0749-3797(01)00350-6. [DOI] [PubMed] [Google Scholar]
- 6.Fallon EA, Wilcox S, Laken M. Health care provider advice for African American adults not meeting health behavior recommendations. Prev Chronic Dis. 2006;3(2):A45. [PMC free article] [PubMed] [Google Scholar]
- 7.Eaton CB, Goodwin M, Stange K. Direct observation of nutrition counseling in community family practice. Am J Prev Med. 2002;23(3):174. doi: 10.1016/s0749-3797(02)00494-4. [DOI] [PubMed] [Google Scholar]
- 8.Eakin EG, Smith BJ, Bauman AE. Evaluating the population health impact of physical activity interventions in primary care - are we asking the right questions? J Phys Act Health. 2005;2(2):197–215. [Google Scholar]
- 9.Smith BJ. Promotion of physical activity in primary health care: update of the evidence on interventions. J Sci Med Sport. 2004;7(1, Suppl):67–73. doi: 10.1016/s1440-2440(04)80280-9. [DOI] [PubMed] [Google Scholar]
- 10.Tulloch H, Fortier M, Hogg W. Physical activity counseling in primary care: who has and who should be counseling? Patient Educ Couns. 2006;64(1–3):6–20. doi: 10.1016/j.pec.2005.10.010. [DOI] [PubMed] [Google Scholar]
- 11.Glasgow RE, Lichtenstein E, Marcus AC. Why don't we see more translation of health promotion research to practice? Rethinking the efficacy-to-effectiveness transition. Am J Public Health. 2003;93(8):1261–1267. doi: 10.2105/ajph.93.8.1261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dzewaltowski DA, Estabrooks PA, Glasgow RE. The future of physical activity behavior change research: what is needed to improve translation of research into health promotion practice? Exerc Sport Sci Rev. 2004;32(2):57–63. doi: 10.1097/00003677-200404000-00004. [DOI] [PubMed] [Google Scholar]
- 13.Dzewaltowski DA, Glasgow RE, Klesges LM, Estabrooks PA, Brock ERE-AIM. evidence-based standards and a Web resource to improve translation of research into practice. Ann Behav Med. 2004;28(2):75–80. doi: 10.1207/s15324796abm2802_1. [DOI] [PubMed] [Google Scholar]
- 14.Breckon JD, Johnston LH, Hutchison A. Physical activity counseling content and competency: a systematic review. J Phys Act Health. 2008;5(3):398–417. doi: 10.1123/jpah.5.3.398. [DOI] [PubMed] [Google Scholar]
- 15.Wilcox S, Parra-Medina D, Thompson-Robinson M, Will J. Nutrition and physical activity interventions to reduce cardiovascular disease risk in health care settings: a quantitative review with a focus on women. Nutr Rev. 2001;59(7):197–214. doi: 10.1111/j.1753-4887.2001.tb07012.x. [DOI] [PubMed] [Google Scholar]
- 16.American Heart Association . Heart Disease and Stroke Statistics—2009 Update. American Heart Association; Dallas, TX: 2009. [Google Scholar]
- 17.Chu KC, Miller BA, Springfield SA. Measures of racial/ethnic health disparities in cancer mortality rates and the influence of socioeconomic status. J Natl Med Assoc. 2007;99(10):1092–100. 102–4. [PMC free article] [PubMed] [Google Scholar]
- 18.Sudano JJ, Baker DW. Explaining US racial/ethnic disparities in health declines and mortality in late middle age: the roles of socioeconomic status, health behaviors, and health insurance. Soc Sci Med. 2006;62(4):909–922. doi: 10.1016/j.socscimed.2005.06.041. [DOI] [PubMed] [Google Scholar]
- 19.Kumanyika SK, Whitt-Glover MC, Gary TL, et al. Expanding the obesity research paradigm to reach African American communities. Prev Chronic Dis. 2007;4(4):A112. [PMC free article] [PubMed] [Google Scholar]
- 20.Health Resources and Services Administration Bureau of Primary Health Care The Health Center Program: National Aggregate UDS Data; Table 3B: Patients by Race/Ethnicity/Language. 2007 [cited 2009 February 21]; Available from: http://bphc.hrsa.gov/uds/2007data/National/NationalT able3BUniversal.htm.
- 21.Health Resources and Services Administration Bureau of Primary Health Care The Health Center Program: National Aggregate UDS Data; Table 4: Patients by Socioeconomic Characteristics. 2007 [cited 2009 February 21]; Available from: http://bphc.hrsa.gov/uds/2007data/National/NationalT able4Universal.htm.
- 22.Prochaska JO, DiClemente CC, Norcross JC. In search of how people change. Applications to addictive behaviors. Am Psychol. 1992;47(9):1102–1114. doi: 10.1037//0003-066x.47.9.1102. [DOI] [PubMed] [Google Scholar]
- 23.Appel LJ, Moore TJ, Obarzanek E, et al. A clinical trial of the effects of dietary patterns on blood pressure. DASH Collaborative Research Group. N Engl J Med. 1997;336(16):1117–1124. doi: 10.1056/NEJM199704173361601. [DOI] [PubMed] [Google Scholar]
- 24.Conlin PR, Chow D, Miller ER, et al. The effect of dietary patterns on blood pressure control in hypertensive patients: results from the Dietary Approaches to Stop Hypertension (DASH) trial. Am J Hypertens. 2000;13(9):949–955. doi: 10.1016/s0895-7061(99)00284-8. [DOI] [PubMed] [Google Scholar]
- 25.Petrella RJ, Lattanzio CN. Does counseling help patients get active? Systematic review of the literature. Can Fam Physician. 2002;48:72–80. [PMC free article] [PubMed] [Google Scholar]
- 26.Eakin EG, Glasgow RE, Riley KM. Review of primary care-based physical activity intervention studies: effectiveness and implications for practice and future research. J Fam Pract. 2000;49(2):158–168. [PubMed] [Google Scholar]
- 27.Glasgow RE, Klesges LM, Dzewaltowski DA, Bull SS, Estabrooks P. The future of health behavior change research: what is needed to improve translation of research into health promotion practice? Ann Behav Med. 2004;27(1):3–12. doi: 10.1207/s15324796abm2701_2. [DOI] [PubMed] [Google Scholar]
- 28.Glasgow RE. Evaluation of theory-based interventions: The RE-AIM model. In: Glanz K, Rimer BK, Lewis FM, editors. Health behavior and health education theory, research, and practice. 3rd ed. Jossey-Bass; San Francisco, CA: 2002. pp. 530–544. [Google Scholar]
- 29.Rosamond WD, Ammerman AS, Holliday JL, et al. Cardiovascular disease risk factor intervention in low-income women: the North Carolina WISEWOMAN project. Prev Med. 2000;31(4):370–379. doi: 10.1006/pmed.2000.0726. [DOI] [PubMed] [Google Scholar]
- 30.Keyserling TC, Samuel-Hodge CD, Ammerman AS, et al. A randomized trial of an intervention to improve self-care behaviors of African-American women with type 2 diabetes: impact on physical activity. Diabetes Care. 2002;25(9):1576–1583. doi: 10.2337/diacare.25.9.1576. [DOI] [PubMed] [Google Scholar]
- 31.Keyserling TC, Ammerman AS, Atwood JR, et al. A cholesterol intervention program for public health nurses in the rural southeast: description of the intervention, study design, and baseline results. Public Health Nurs. 1999;16(3):156–167. doi: 10.1046/j.1525-1446.1999.00156.x. [DOI] [PubMed] [Google Scholar]
- 32.Keyserling TC, Ammerman AS, Davis CE, Mok MC, Garrett J, Simpson R., Jr. A randomized controlled trial of a physician-directed treatment program for low-income patients with high blood cholesterol: the Southeast Cholesterol Project. Arch Fam Med. 1997;6(2):135–145. doi: 10.1001/archfami.6.2.135. [DOI] [PubMed] [Google Scholar]
- 33.Ammerman AS, Keyserling TC, Atwood JR, Hosking JD, Zayed H, Krasny C. A randomized controlled trial of a public health nurse directed treatment program for rural patients with high blood cholesterol. Prev Med. 2003;36(3):340–351. doi: 10.1016/s0091-7435(02)00042-7. [DOI] [PubMed] [Google Scholar]
- 34.Ammerman AS, Haines PS, DeVellis RF, et al. A brief dietary assessment to guide cholesterol reduction in low-income individuals: design and validation. J Am Diet Assoc. 1991;91(11):1385–1390. [PubMed] [Google Scholar]
- 35.Ammerman AS, DeVellis BM, Haines PS, et al. Nutrition education for cardiovascular disease prevention among low income populations-description and pilot evaluation of a physician- based model. Patient Educ Couns. 1992;19(1):5–18. doi: 10.1016/0738-3991(92)90098-4. [DOI] [PubMed] [Google Scholar]
- 36.Ackermann RT, Deyo RA, LoGerfo JP. Prompting primary providers to increase community exercise referrals for older adults: a randomized trial. J Am Geriatr Soc. 2005;53(2):283–289. doi: 10.1111/j.1532-5415.2005.53115.x. [DOI] [PubMed] [Google Scholar]
- 37.Cifuentes M, Fernald DH, Green LA, et al. Prescription for health: changing primary care practice to foster healthy behaviors. Ann Fam Med. 2005;3(Suppl 2):S4–S11. doi: 10.1370/afm.378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Etz RS, Cohen DJ, Woolf SH, et al. Bridging primary care practices and communities to promote healthy behaviors. Am J Prev Med. 2008;35(5, Suppl):S390–S397. doi: 10.1016/j.amepre.2008.08.008. [DOI] [PubMed] [Google Scholar]
- 39.Reed J, Malvern L, Muthukrishnan S, Hardy R, King L. An ecological approach with primary-care counseling to promote physical activity. J Phys Act Health. 2008;5(1):169–183. doi: 10.1123/jpah.5.1.169. [DOI] [PubMed] [Google Scholar]
- 40.Wilcox S, Richter DL, Henderson KA, Greaney ML, Ainsworth BE. Perceptions of physical activity and personal barriers and enablers in African-American women. Ethn Dis. 2002;12(3):353–362. [PubMed] [Google Scholar]
- 41.Nies MA, Vollman M, Cook T. African American women's experiences with physical activity in their daily lives. Public Health Nurs. 1999;16(1):23–31. doi: 10.1046/j.1525-1446.1999.00023.x. [DOI] [PubMed] [Google Scholar]
- 42.Vrazel J, Saunders RP, Wilcox S. An overview and proposed framework of social-environmental influences on the physical-activity behavior of women. Am J Health Promot. 2008;23(1):2–12. doi: 10.4278/ajhp.06070999. [DOI] [PubMed] [Google Scholar]
- 43.Richter DL, Wilcox S, Greaney ML, Henderson KA, Ainsworth BE. Environmental, policy, and cultural factors related to physical activity in African American women. Women Health. 2002;36(2):91–109. doi: 10.1300/j013v36n02_07. [DOI] [PubMed] [Google Scholar]
- 44.Bopp M, Lattimore D, Wilcox S, et al. Understanding physical activity participation in members of an African American church: a qualitative study. Health Educ Res. 2007;22(6):815–826. doi: 10.1093/her/cyl149. [DOI] [PubMed] [Google Scholar]
- 45.Dutton GR, Johnson J, Whitehead D, Bodenlos JS, Brantley PJ. Barriers to physical activity among predominantly low-income African-American patients with type 2 diabetes. Diabetes Care. 2005;28(5):1209–1210. doi: 10.2337/diacare.28.5.1209. [DOI] [PubMed] [Google Scholar]
- 46.Sanderson B, Littleton M, Pulley L. Environmental, policy, and cultural factors related to physical activity among rural, African American women. Women Health. 2002;36(2):75–90. doi: 10.1300/j013v36n02_06. [DOI] [PubMed] [Google Scholar]
- 47.Wilbur J, Chandler P, Dancy B, Choi J, Plonczynski D. Environmental, policy, and cultural factors related to physical activity in urban, African American women. Women Health. 2002;36(2):17–28. doi: 10.1300/J013v36n02_02. [DOI] [PubMed] [Google Scholar]
- 48.Kumanyika S, Wilson JF, Guilford-Davenport M. Weight-related attitudes and behaviors of black women. J Am Diet Assoc. 1993;93(4):416–422. doi: 10.1016/0002-8223(93)92287-8. [DOI] [PubMed] [Google Scholar]
- 49.Casagrande SS, Whitt-Glover MC, Lancaster KJ, Odoms-Young AM, Gary TL. Built environment and health behaviors among African Americans: a systematic review. Am J Prev Med. 2009;36(2):174–181. doi: 10.1016/j.amepre.2008.09.037. [DOI] [PubMed] [Google Scholar]
- 50.Block JP, Scribner RA, DeSalvo KB. Fast food, race/ethnicity, and income: a geographic analysis. Am J Prev Med. 2004;27(3):211–217. doi: 10.1016/j.amepre.2004.06.007. [DOI] [PubMed] [Google Scholar]
- 51.Cassady D, Jetter KM, Culp J. Is price a barrier to eating more fruits and vegetables for low-income families? J Am Diet Assoc. 2007;107(11):1909–1915. doi: 10.1016/j.jada.2007.08.015. [DOI] [PubMed] [Google Scholar]
- 52.Hosler AS, Rajulu DT, Fredrick BL, Ronsani AE. Assessing retail fruit and vegetable availability in urban and rural underserved communities. Prev Chronic Dis. 2008;5(4):A123. [PMC free article] [PubMed] [Google Scholar]
- 53.Larson NI, Story MT, Nelson MC. Neighborhood environments: disparities in access to healthy foods in the U.S. Am J Prev Med. 2009;36(1):74–81. doi: 10.1016/j.amepre.2008.09.025. [DOI] [PubMed] [Google Scholar]
- 54.Pate RR, Pratt M, Blair SN, et al. Physical activity and public health. A recommendation from the Centers for Disease Control and Prevention and the American College of Sports Medicine. JAMA. 1995;273(5):402–407. doi: 10.1001/jama.273.5.402. [DOI] [PubMed] [Google Scholar]
- 55.US Department of Health and Human Services. US Department of Agriculture . Dietary Guidelines for Americans, 2005. 6th ed. U.S. Government Printing Office; Washington, DC: 2005. [Google Scholar]