Abstract
Background
Psychological distress contributes to the development of hypertension in young adults. This trial assessed the effects of a mind–body intervention on blood pressure (BP), psychological distress, and coping in college students.
Methods
This was a randomized controlled trial (RCT) of 298 university students randomly allocated to either the Transcendental Meditation (TM) program or wait-list control. At baseline and after 3 months, BP, psychological distress, and coping ability were assessed. A subgroup of 159 subjects at risk for hypertension was analyzed similarly.
Results
Changes in systolic BP (SBP)/diastolic BP (DBP) for the overall sample were −2.0/−1.2 mm Hg for the TM group compared to +0.4/+0.5 mm Hg for controls (P = 0.15, P = 0.15, respectively). Changes in SBP/DBP for the hypertension risk subgroup were −5.0/−2.8 mm Hg for the TM group compared to +1.3/+1.2 mm Hg for controls (P = 0.014, P = 0.028, respectively). Significant improvements were found in total psychological distress, anxiety, depression, anger/hostility, and coping (P values < 0.05). Changes in psychological distress and coping correlated with changes in SBP (P values < 0.05) and DBP (P values < 0.08).
Conclusions
This is the first RCT to demonstrate that a selected mind–body intervention, the TM program, decreased BP in association with decreased psychological distress, and increased coping in young adults at risk for hypertension. This mind–body program may reduce the risk for future development of hypertension in young adults.
Hypertension affects ~33% of US adults.1 College age individuals with mild blood pressure (BP) elevation are three times more likely to develop hypertension within 30 years than normotensives.2
Psychological distress such as anxiety, depression, and anger/hostility have been found to contribute to the development of hypertension.3 In young adults, affective distress was associated with the development of hypertension over 15 years.4 The risk for hypertension associated with anxiety, depression, and anger/hostility is similar to traditional predictors of hypertension such as obesity and physical inactivity.5 Studies also have indicated that positive coping strategies may moderate the effect of stressful events on BP while negative coping may have a detrimental effect.6,7
College students are particularly prone to psychological distress,8 caused by interpersonal and social problems, pressures to succeed academically, financial strains, and uncertain futures.9,10,11 Previous controlled studies on the Transcendental Meditation (TM) program, one of the most widely used mind–body approaches for reducing psychological distress, has shown significant reductions in BP,12,13 anxiety,14,15 depression,15 and improved coping ability16 in students and adults.
To further investigate the effectiveness of the TM program on BP, psychological distress, and coping, we conducted a randomized controlled trial (RCT) in college students. To our knowledge, this is the first RCT to evaluate the efficacy of a mind–body intervention on BP and psychological factors in young adults.
Methods
Study design
This was a single-blind RCT comparing stress reduction with the TM program to wait-list controls on change in BP, psychological distress, and coping in young adults. The present study reports on both the overall sample and a subgroup at risk for hypertension. The field site was American University (Washington, DC). The administrative and data-coordinating center was the Center for Natural Medicine and Prevention at Maharishi University of Management Research Institute (Maharishi Vedic City, IA). The institutional review boards of both institutions approved the study. The trial was conducted from January 2006 to May 2007.
Study participants
The subjects were 298 students from American University and other surrounding colleges, including Georgetown and University of District of Columbia. Inclusion criteria included enrollment in an undergraduate or graduate program through August 2006. Students were excluded if they had a history of hypertension, hypoglycemia, chronic fainting, coronary heart disease, or current BP above 140/90 mm Hg or below 90/60 mm Hg.
Subjects were included in a high-risk subgroup if they had one or more of the following risk factors for hypertension: systolic BP (SBP) >130, diastolic BP (DBP) >85,17 family history of hypertension,18 overweight, or obesity defined as body mass index ≥25.19,20
Study protocol
Interested participants were scheduled for small group informational sessions presented by the research staff and TM instructional staff. After providing written informed consent, students underwent baseline testing.
Students were then randomized to experimental or control groups, using the random blocks method21 stratifying on gender (male/female) and self-reported attention deficit hyperactivity disorder status (yes, no), to either (a) immediate instruction in the TM program or (b) wait list/delayed start condition. (The attention deficit hyperactivity disorder stratification was for the purpose of a separate substudy.)
The treatment group allocations were concealed by the study statistician, with individual treatment group assignments revealed to the project manager only when study participants completed baseline testing. Subjects were post-tested after ~3 months. All assessments were administered by research staff who were masked to treatment condition. Thus, this was a single-blind design. After post-test evaluation, wait-list participants were offered TM instruction.
Outcome measures
The primary outcome for the study was casual BP. Secondary outcomes were psychological distress (total mood disturbance, anxiety, depression, anger/hostility) and coping ability (global constructive thinking).
BP was measured in a seated position, with an automated BP monitor (model #UA-787; A&D Medical, Albany, GA) using standard clinical trial technique.22 Three readings were taken in both pre- and post-testing sessions. The first BP reading was taken after an adaptation period of 5 min in which subjects were seated comfortably not practicing any formal relaxation technique. Thereafter, a 1-min adaptation period was used between the first, second, and third readings. The last two were averaged for the study score.
Family history of hypertension was determined by self-report and body mass index by a ratio of weight and height (BMI = weight in kilograms/(height in meters × height in meters)).
Psychological distress was measured with the Profile of Mood States total mood disturbance main scale and tension/anxiety, depression/dejection, and anger/hostility subscales.23 These scales were selected because of the association of these constructs with BP.5 Internal consistency coefficients range from 0.90 to 0.95.23
Coping was measured using the Constructive inking Inventory global constructive thinking main scale, which measures constructive and destructive thinking patterns underlying coping ability.24,25 Previous research has shown that global constructive thinking is sensitive to mind–body intervention.16 The global constructive thinking scale includes emotional and behavioral coping items, with higher scores indicating more positive, healthy coping. Internal consistency is reported to be 0.90.26
Intervention
The TM technique is the principal mind–body modality of the Maharishi Vedic Approach to Health, a comprehensive traditional system of natural health care derived from the ancient Vedic tradition.27 The TM technique is a simple, natural, and easy-to-learn procedure that allows the ordinary thinking process to become more quiescent and a unique psychophysiologic state of “restful alertness” to be gained.28 This distinctive state of restful alertness,28,29 is characterized by decreased respiration rates, sympathetic tone and hypothalamic–pituitary–adrenal axis activity,30,31 and high electroencephalography coherence.32 The program is practiced twice a day for 20 min while sitting comfortably with eyes closed.33 Students who learned the TM technique were taught by certified instructors, according to the standardized format offered in the United States by Maharishi Vedic Education Development Corporation33 and used in previous trials.34,35
The TM technique was taught in a seven-step course33 as follows: (i) group introductory lecture on potential benefits and previous research (90 min); (ii) group preparatory lecture, discussing the mechanics and origin of the TM technique (90 min); (iii) personal interview (10 min); (iv) personal instruction session (90 min); (v–vii) group “verification and validation of the practice” sessions on 3 consecutive days following personal instruction, verifying correctness of TM practice, and providing the understanding of the mechanics of the TM technique.
After the seven-step course, students were invited to attend individual meetings with the TM instructor to verify the mechanics of practice and maintain regularity. These meetings were held weekly for the first month, then monthly thereafter (30 min each). Weekly (group) knowledge meetings were also available.
Adherence
Adherence to the TM program was measured via self-report at post-testing among those who had received TM instruction. Participants were asked to describe the regularity of their practice of the TM technique over the preceding week (not at all, less than once/day, once a day, or twice a day). Participants reporting having practiced at least once a day were considered adherent.
Power analysis
Based on previously published data,13 we estimated pre/post-test differences between TM and control groups of −4.4 (s.d. = 8.1) mm Hg for SBP and −3.9 (s.d. = 7.5) mm Hg for DBP. Calculations using SAS Proc Power (SAS, Cary, NC) indicated 90% power to detect significant differences in BP change at the 0.05 level between groups among the whole sample, and 80% power to detect significant differences between groups in the high-risk subsample.
Statistical methods
Differences between the treatment groups on demographic and baseline variables was examined using t-tests for continuous variables and χ2-tests for categorical variables, and by multivariate analysis of variance to assess multivariate differences across all variables. To investigate treatment effects on change in outcome variables from baseline and post-test, analysis of covariance (ANCOVA) was performed in the overall sample and in the hypertension risk subgroup on all eligible subjects with baseline and post-test data. In these analyses, the independent variable was TM program vs. the wait-list control condition. Baseline score of the dependent variable was a prespecified covariate; other baseline factors were not used in the primary analyses to statistically adjust estimated treatment effects. Additional ANCOVA were performed covarying also for baseline variables on which there were significant differences between the treatment groups, in order to assess the potential influence of such differences on the treatment outcomes. To investigate relationships in change among the outcome variables, partial correlations controlling for baseline scores for each pair of variables were calculated by multiple regression analysis. All analyses are reported as two-tailed.
Results
Baseline variables
Of the 298 participants (average age = 25.5 years), 117 (40%) were men; 62% were Caucasian, 16% African American, 7% Asian American, 4% Hispanic, and 11% were of other ethnicities or declined to report race/ethnicity. Average SBP/DBP was 117/76 mm Hg.
Table 1 shows baseline data for the 207 students who completed both BP baseline and post-testing by group. Multivariate analysis of variance showed no significant differences between groups on baseline variables (F(17,173) = 0.78; P = 0.72).
Table 1.
Baseline comparisons by treatment groups for students completing 3-month post-testing (N = 207)
| Variable | Mean ± s.d. | P value | |
|---|---|---|---|
| TM (n = 93) | Control (n = 114) | ||
| Age | 25.4 ± 9.2 | 26.2 ± 9.9 | 0.57 |
| Gender, % male | 38.7% | 43.0% | 0.54 |
| Graduate students, % | 33.3% | 27.2% | 0.34 |
| Undergraduates, % | 64.5% | 71.1% | 0.32 |
| Weight, kg | 68.0 ± 12.3 | 70.6 ± 16.1 | 0.21 |
| BMI ≥25 | 22.5% | 31.5% | 0.16 |
| Current smoking, y/n | 10.8% | 12.3% | 0.73 |
| Family history of hypertension | 26.9% | 23.7% | 0.60 |
| Alcohol usage, drinks/week | 4.3 ± 5.2 | 4.2 ± 6.4 | 0.91 |
| SBP, mm Hg | 116.7 ± 12.8 | 117.9 ± 13.7 | 0.50 |
| DBP, mm Hg | 74.7 ± 8.4 | 76.6 ± 8.7 | 0.12 |
| SBP/DBP >130/85 mm Hg | 23.7% | 24.6% | 0.88 |
| Total psychological distress | 45.2 ± 36.0 | 40.1 ± 33.2 | 0.30 |
| Anxiety subscale | 13.6 ± 6.8 | 12.1 ± 6.4 | 0.12 |
| Depression subscale | 13.7 ± 12.1 | 12.9 ± 11.2 | 0.64 |
| Anger/hostility subscale | 11.2 ± 9.0 | 9.9 ± 8.0 | 0.27 |
| Coping ability | 95.3 ± 17.5 | 101.5 ± 15.9 | 0.009 |
BMI, body mass index; DBP, diastolic blood pressure; SBP, systolic blood pressure; TM, Transcendental Meditation.
Pre/post-test changes
ANCOVA, covarying for the baseline score of the dependent variable for the 207 subjects who completed baseline and post-test, indicated a mean reduction in SBP for the TM group of −2.0 mm Hg compared to +0.4 mm Hg for wait-list controls (P = 0.15). DBP change was −1.2 mm Hg for the meditation group compared to +0.5 mm Hg for controls (P = 0.15).
The TM group compared to controls showed improvement in total psychological distress (P = 0.004), anxiety (P = 0.003), depression (P = 0.012), and anger/hostility (P = 0.06), sub-scales, and coping ability (P = 0.003) (see Table 2).
Table 2.
Pre/post-test changes in the transcendental Meditation group compared to controls
| Variable | Adjusted mean change ± s.e.m. | P value | |
|---|---|---|---|
| TM (n = 93) | Control (n = 114) | ||
| SBP, mm Hg | −2.0 ± 1.2 | 0.4 ± 1.1 | 0.15 |
| DBP, mm Hg | −1.2 ± 0.9 | 0.5 ± 0.8 | 0.15 |
| Total psychological distress | −18.9 ± 3.2 | −6.1 ± 2.9 | 0.004 |
| Anxiety | −3.7 ± 0.7 | −1.0 ± 0.6 | 0.003 |
| Depression | −5.2 ± 1.0 | −1.9 ± 0.9 | 0.012 |
| Anger/hostility | −3.2 ± 0.8 | −1.0 ± 0.8 | 0.06 |
| Coping ability | 6.0 ± 1.1 | 1.5 ± 1.0 | 0.003 |
Means are adjusted by covarying for the baseline score on each outcome variable. DBP, diastolic blood pressure; SBP, systolic blood pressure; TM, Transcendental Meditation.
Additional BP analysis, covarying for both baseline score of the dependent variable and baseline coping ability indicated a change in SBP for the TM group of −2.0 ± 1.2 mm Hg vs. +0.4 ± 1.1 mm Hg for controls (P = 0.14) and a change in DBP for the TM group of −1.4 ± 0.9 mm Hg vs. +0.6 ± 0.8 mm Hg for controls (P = 0.10).
Hypertension risk subgroup
Baseline variables
A total of 159 subjects met the inclusion criteria for this subgroup. Of these, 112 completed baseline and post-testing were included in these analyses. Average SBP/DBP was 122/79 mm Hg. In terms of inclusion criteria for this subgroup, 45% had BP >130/85, 46% had at least one family member with hypertension, and 50% had a body mass index ≥25 (see Table 3). Multivariate analysis of variance showed no significant differences between groups on baseline variables (F(17,86) = 0.82; P = 0.67).
Table 3.
Baseline comparisons of hypertension risk subgroup by treatment groups (N = 112)
| Variable | Mean ± s.d. | Mean ± s.d. | P value |
|---|---|---|---|
| TM (n = 48) | Control (n = 64) | ||
| Age | 27.7 ± 10.3 | 29.4 ± 11.2 | 0.42 |
| Gender, % male | 37.5% | 40.6% | 0.74 |
| Graduate students, % | 37.5% | 29.7% | 0.39 |
| Undergraduates, % | 58.3% | 68.8% | 0.26 |
| Weight, kg | 73.0 ± 13.6 | 75.5 ± 18.6 | 0.44 |
| BMI ≥25 | 42.6% | 54.8% | 0.21 |
| Current smoking y/n | 10.4% | 10.9% | 0.93 |
| Family history of hypertension | 52.1% | 42.2% | 0.30 |
| Alcohol usage, drinks/week | 4.1 ± 5.7 | 3.1 ± 4.6 | 0.30 |
| SBP mm Hg | 122.5 ± 13.4 | 121.2 ± 15.9 | 0.65 |
| DBP mm Hg | 78.3 ± 8.3 | 79.3 ± 9.4 | 0.56 |
| SBP/DBP >130/85 mm Hg% | 16.7% | 28.1% | 0.16 |
| Total psychological distress | 47.0 ± 38.7 | 39.0 ± 33.7 | 0.25 |
| Anxiety | 13.8 ± 7.1 | 12.4 ± 6.6 | 0.31 |
| Depression | 15.2 ± 12.8 | 12.1 ± 11.0 | 0.17 |
| Anger/hostility | 11.6 ± 9.4 | 9.4 ± 8.3 | 0.19 |
| Coping ability | 94.0 ± 17.8 | 100.8 ± 16.4 | 0.041 |
DBP, diastolic blood pressure; SBP, systolic blood pressure; TM, Transcendental Meditation.
Pre/post-test changes
Findings indicated significant reductions for the TM group vs. controls in both SBP (−5.0 mm Hg vs. +1.3 mm Hg; P = 0.014) and DBP (−2.8 mm Hg vs. +1.2 mm Hg; P = 0.028).
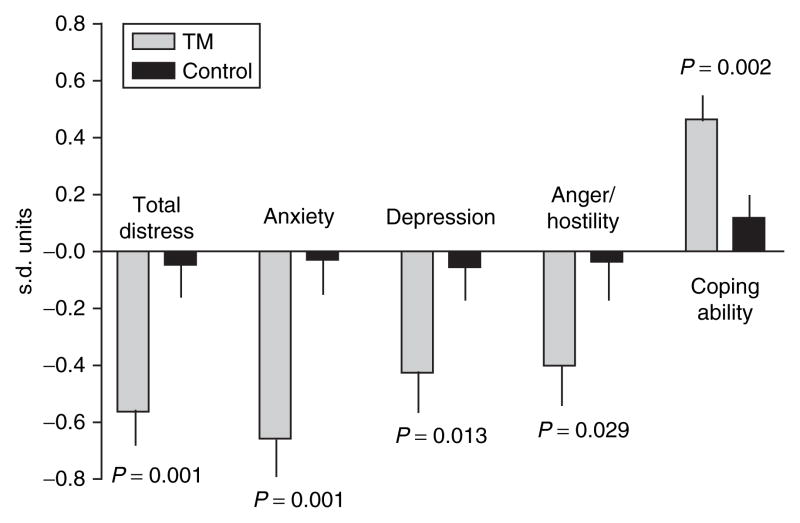
Significant improvement was found in total psychological distress (P = 0.001) and anxiety (P = 0.001), depression (P = 0.013), and anger/hostility (P = 0.029) subscales, and coping ability (P = 0.002) (see Table 4). Changes in psychological distress and coping for both groups are shown in s.d. units in Figure 1.
Table 4.
Pre/post-test changes comparing the transcendental Meditation group to controls in the hypertension risk subgroup
| Variable | Adjusted mean change ± s.e.m. | P value | |
|---|---|---|---|
| TM (n = 48) | Control (n = 64) | ||
| SBP (mm Hg) | −5.0 ± 1.9 | 1.3 ± 1.7 | 0.014 |
| DBP (mm Hg) | −2.8 ± 1.4 | 1.2 ± 1.2 | 0.028 |
| Total psychological distress | −21.8 ± 4.2 | −1.6 ± 3.6 | 0.001 |
| Anxiety | −4.7 ± 0.9 | −0.2 ± 0.8 | 0.001 |
| Depression | −5.4 ± 1.4 | −0.7 ± 1.2 | 0.013 |
| Anger/hostility | −3.8 ± 1.1 | −0.5 ± 1.0 | 0.029 |
| Coping ability | 8.2 ± 1.5 | 1.9 ± 1.3 | 0.002 |
Means are adjusted by covarying for the baseline score on each outcome variable. DBP, diastolic blood pressure; SBP, systolic blood pressure; TM, Transcendental Meditation.
Figure 1.
Three-month pre/post-test change in psychological distress and coping comparing the TM group to controls in the hypertension risk subgroup. TM, Transcendental Meditation.
Additional analyses for BP in the high-risk sample, covarying for both baseline score of the dependent variable and baseline coping ability, continued to indicate significant reductions for the TM group vs. controls in both SBP (−5.3 ± 2.0 mm Hg vs. +1.6. ± 1.7 mm Hg; P = 0.01) and DBP (−3.3 ± 1.4 mm Hg vs. +1.4 ± 1.2 mm Hg; P = 0.013). Two-factor ANCOVA on the entire sample, with treatment and level of BP risk (high vs. low) as grouping factors, covarying for baseline dependent variable and coping ability, showed significant interactions between treatment and level of BP risk for SBP (P = 0.01) and DBP (P = 0.018), indicating that BP treatment effects were specific to the high-risk subgroup.
Associations between outcome variables
Reduction in SBP was associated with change in total psychological distress (partial r = 0.19; P = 0.043), anxiety (r = 0.21; P = 0.029), depression (r = 0.21; P = 0.027), and coping ability (r = −0.21; P = 0.026). Reduction in DBP was associated with change in anxiety (partial r = 0.17; P = 0.08) and coping ability (r = −18; P = 0.06).
In addition, change in psychological distress scales and coping ability showed significant negative correlations with each other (partial r values range from −0.44 to −0.68; P values < 0.01).
Adherence to TM practice
Of the 93 participants who had received TM instruction and completed post-testing, 64% of the entire sample and 67% of the hypertension risk subgroup reported practicing the TM technique regularly. There was no significant difference between the entire sample and high-risk subgroup with regard to the proportion of TM subjects who were regular in their practice (χ2(1) = 0.365; P = 0.55). An additional 15% in the entire sample and 13% in the subgroup reported some practice of the technique.
Comparison among completers and attriters at baseline
Across groups, there were no significant differences between subjects who completed post-testing (n = 207) and those who did not complete post-testing (n = 91) on any of the primary or secondary outcome variables at baseline, either in the whole sample or in the high-risk subgroup. Also no significant differences between the TM group and control group among subjects who did not complete post-testing were observed on any of the primary or secondary outcome variables at baseline, either in the entire sample or in the high-risk subsample.
Discussion
Results of this RCT in a general population of college students indicated nonsignificant reductions of −2.0 mm Hg in SBP and −1.2 mm Hg in DBP in the TM group compared to increases of 0.4 mm Hg in SBP and 0.5 mm Hg in DBP in the control group. These BP reductions in the overall sample may have been limited by the relatively low baseline BP levels. However, findings in this sample showed significant improvement in psychological distress and coping ability. Analysis of the hypertension risk subgroup indicated significant reductions of −5.0 mm Hg in SBP and −2.8 mm Hg in DBP in the TM group compared to increases of 1.3 mm Hg in SBP and 1.2 mm Hg in DBP in the control group. Thus, net reductions of −6.3 mm Hg in SBP and −4.0 mm Hg in DBP for the TM group relative to the control group were observed. Decreased psychological distress and increased coping ability were also found for the TM group compared to controls in the high-risk sample. Reductions in BP were significantly correlated with reductions in psychological distress and increased coping.
Recent meta-analyses of RCTs in predominantly prehypertensive and hypertensive subjects showed that practice of the TM program produced an average SBP/DBP reduction of about −5.0/−3.0 mm Hg.12,13 The net reductions −6.3 mm Hg in SBP and −4.0 in DBP for the TM group relative to the control group in the high-risk subgroup in this study are consistent with previous findings in high-BP samples. Based upon a risk prediction scoring formula for the onset of hypertension from Framingham study data, the net reductions in BP for the TM group are associated with a 52% lower risk for onset of hypertension over a 4-year period.20
Regression analyses further showed that the changes in SBP and DBP were significantly correlated with changes in psychological distress, including anxiety and depression, and coping ability. These findings are congruent with a biobehavioral model of high BP.36 According to this model, psychological distress leads to hyperactivation of the sympathetic nervous system and hypothalamic–pituitary–adrenocortical axis.37 This, in turn, leads to acute and chronic elevations in BP. Thus the reductions in psychological distress factors may have contributed to lower BP. Reductions in sympathetic nervous system and hypothalamic–pituitary–adrenocortical activation with TM practice reported in previous studies suggest central nervous system and neuroendocrine pathways for the effects of the psychological distress changes on BP observed in the current trial.38
Another element in this model is the buffering effect of coping mechanisms. According to the biobehavioral stress model, external stressors (such as financial concerns and work/school stress) induce negative affect (in the form of anxiety, depression, and anger), which in turn adversely impact BP.5,36,39,40 The influence of external stressors on negative affect and BP may be moderated by positive coping mechanisms (employed by constructive thinkers). Previous research has shown that high global constructive thinkers appraise external stressors as less threatening and produce less negative affective and cognitive responses to laboratory stressors, with lower levels of physiological arousal.26 In the present study, coping ability correlated with BP and psychological distress factors. Thus improved coping ability may have contributed to lower BP via its effects on moderating/reducing psychological distress factors.
Study strengths and limitations
There were several important methodological strengths, including the use of random assignment, the use of assessors masked to treatment condition to reduce demand characteristics, and a sizable racially diverse subject sample, which lends confidence in the generalizability of the findings to the college student population.
A limitation is that about 30% of the pretest sample was unavailable for post-testing. This concern is mitigated by the fact that across groups completers did not differ from non-completers on any baseline entry characteristics. Also there were no differences between groups on baseline primary and secondary outcomes in noncompleters.
It is unlikely that baseline differences between the treatment arms in the high-risk subsample could have contributed to the observed BP reduction. ANCOVA results for BP were very similar, regardless of whether baseline coping ability, which was significantly different between groups, was included as a covariate. Differences on other baseline variables were relatively small (~0.1 s.d. on BP and 0.2 s.d. on total psychological distress) and are therefore unlikely to have affected the results substantially.
Future randomized trials of the TM program in college students should evaluate longer-term intervention periods to assess long-term effects on BP and psychological distress.
In conclusion, this is the first RCT to demonstrate that a selected mind–body intervention, the TM program, significantly decreased BP in association with improved psychological distress and coping ability in young adults at risk for hypertension. In addition, there were improvements in mental health in the general student sample and trends toward reduction of BP. Practice of this mind–body intervention may be an effective method to reduce psychological distress, BP, and the risk for prospective development of hypertension in high-risk young adults.
Acknowledgments
This study was funded by the Abramson Family Foundation, David Lynch Foundation, Howard and Alice Settle, Ramani and Louise Ayer, and other private donors. This study was supported, in part, by a Specialized Center of Research Grant from the National Institutes of Health -National Center for Complementary and Alternative Medicine (1P50AT00082). The authors are grateful to Mario Orsatti, Linda Mainquist, Laura Alcorn, Linda Heaton, Dr Diane Prather-Huff, Marilyn Ungaro, Kris Schumann, and Sarah Weisberg for their assistance in the study and the preparation of the manuscript. Transcendental Meditation and TM are service marks registered in the US patent and trademark office, licensed to Maharishi Vedic Development Corporation and used under sublicense.
Footnotes
Disclosure: R.H.S. is a consultant to Maharishi Health Technologies, LLC. Other authors declared no conflict of interest.
References
- 1.Rosamond W, Flegal K, Furie K, Go A, Greenlund K, Haase N, Hailpern SM, Ho M, Howard V, Kissela B, Kittner S, Lloyd-Jones D, McDermott M, Meigs J, Moy C, Nichol G, O’Donnell C, Roger V, Sorlie P, Steinberger J, Thom T, Wilson M, Hong Y American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics—2008 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation. 2008;117:e25–146. doi: 10.1161/CIRCULATIONAHA.107.187998. [DOI] [PubMed] [Google Scholar]
- 2.Andersson OK, Lingman M, Himmelmann A, Sivertsson R, Widgren BR. Prediction of future hypertension by casual blood pressure or invasive hemodynamics? A 30-year follow-up study. Blood Press. 2004;13:350–354. doi: 10.1080/08037050410004819. [DOI] [PubMed] [Google Scholar]
- 3.Rozanski A, Blumenthal JA, Davidson KW, Saab PG, Kubzansky L. The epidemiology, pathophysiology, and management of psychosocial risk factors in cardiac practice: the emerging field of behavioral cardiology. J Am Coll Cardiol. 2005;45:637–651. doi: 10.1016/j.jacc.2004.12.005. [DOI] [PubMed] [Google Scholar]
- 4.Yan LL, Liu K, Matthews KA, Daviglus ML, Ferguson TF, Kiefe CI. Psychosocial factors and risk of hypertension: the Coronary Artery Risk Development in Young Adults (CARDIA) study. JAMA. 2003;290:2138–2148. doi: 10.1001/jama.290.16.2138. [DOI] [PubMed] [Google Scholar]
- 5.Rutledge T, Hogan BE. A quantitative review of prospective evidence linking psychological factors with hypertension development. Psychosom Med. 2002;64:758–766. doi: 10.1097/01.psy.0000031578.42041.1c. [DOI] [PubMed] [Google Scholar]
- 6.Kobasa SC, Maddi SR, Kahn S. Hardiness and health: a prospective study. J Pers Soc Psychol. 1982;42:168–177. doi: 10.1037//0022-3514.42.1.168. [DOI] [PubMed] [Google Scholar]
- 7.Clark AM, Hartling L, Vandermeer B, McAlister FA. Meta-analysis: secondary prevention programs for patients with coronary artery disease. Ann Intern Med. 2005;143:659–672. doi: 10.7326/0003-4819-143-9-200511010-00010. [DOI] [PubMed] [Google Scholar]
- 8.D’Zurilla TJ, Sheedy CF. Relation between social problem-solving ability and subsequent level of psychological stress in college students. J Pers Soc Psychol. 1991;61:841–846. doi: 10.1037//0022-3514.61.5.841. [DOI] [PubMed] [Google Scholar]
- 9.Landow M. College Students: Mental Health and Coping Strategies. Hauppauge, NY: Nova Science; 2006. [Google Scholar]
- 10.Seligman ME, Schulman P, Tryon AM. Group prevention of depression and anxiety symptoms. Behav Res Ther. 2007;45:1111–1126. doi: 10.1016/j.brat.2006.09.010. [DOI] [PubMed] [Google Scholar]
- 11.Petruzzello S. Physical activity and mental health in college students. In: Landow M, editor. College Students: Mental Health and Coping Strategies. Nova Science; Hauppauge, NY: 2006. pp. 41–57. [Google Scholar]
- 12.Rainforth MV, Schneider RH, Nidich SI, Gaylord-King C, Salerno JW, Anderson JW. Stress reduction programs in patients with elevated blood pressure: a systematic review and meta-analysis. Curr Hypertens Rep. 2007;9:520–528. doi: 10.1007/s11906-007-0094-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Anderson JW, Liu C, Kryscio RJ. Blood pressure response to transcendental meditation: a meta-analysis. Am J Hypertens. 2008;21:310–316. doi: 10.1038/ajh.2007.65. [DOI] [PubMed] [Google Scholar]
- 14.Eppley KR, Abrams AI, Shear J. Differential effects of relaxation techniques on trait anxiety: a meta-analysis. J Clin Psychol. 1989;45:957–974. doi: 10.1002/1097-4679(198911)45:6<957::aid-jclp2270450622>3.0.co;2-q. [DOI] [PubMed] [Google Scholar]
- 15.Sheppard WD, Staggers F, Johns L. The effects of a stress management program in a high security government agency. Anxiety Stress Coping. 1997;10:341–350. [Google Scholar]
- 16.So KT, Orme-Johnson DW. Three randomized experiments on the holistic longitudinal effects of the Transcendental Meditation technique on cognition. Intelligence. 2001;29:419–440. [Google Scholar]
- 17.Vasan RS, Larson MG, Leip EP, Kannel WB, Levy D. Assessment of frequency of progression to hypertension in non-hypertensive participants in the Framingham Heart Study: a cohort study. Lancet. 2001;358:1682–1686. doi: 10.1016/S0140-6736(01)06710-1. [DOI] [PubMed] [Google Scholar]
- 18.Wang NY, Young JH, Meoni LA, Ford DE, Erlinger TP, Klag MJ. Blood pressure change and risk of hypertension associated with parental hypertension: the Johns Hopkins Precursors Study. Arch Intern Med. 2008;168:643–648. doi: 10.1001/archinte.168.6.643. [DOI] [PubMed] [Google Scholar]
- 19.Israeli E, Korzets Z, Tekes-Manova D, Tirosh A, Schochat T, Bernheim J, Golan E. Blood-pressure categories in adolescence predict development of hypertension in accordance with the European guidelines. Am J Hypertens. 2007;20:705–709. doi: 10.1016/j.amjhyper.2007.01.020. [DOI] [PubMed] [Google Scholar]
- 20.Parikh NI, Pencina MJ, Wang TJ, Benjamin EJ, Lanier KJ, Levy D, D’Agostino RB, Sr, Kannel WB, Vasan RS. A risk score for predicting near-term incidence of hypertension: the Framingham Heart Study. Ann Intern Med. 2008;148:102–110. doi: 10.7326/0003-4819-148-2-200801150-00005. [DOI] [PubMed] [Google Scholar]
- 21.Stommel M, Wills C. Clinical Research: Concepts and Principles for Advanced Practice Nurses. Lippincott Williams & Wilkins; Philadelphia, PA: 2003. p. 480. [Google Scholar]
- 22.Multiple Risk Factor Intervention Trial Research Group. Multiple risk factor intervention trial. Risk factor changes and mortality results. JAMA. 1982;248:1465–1477. [PubMed] [Google Scholar]
- 23.McNair DM, Lorr M, Drooppleman LF. Manual for the Profile of Mood States. San Diego, CA: Education and Testing Service; 1971. [Google Scholar]
- 24.Epstein S. Cognitive-experiential self-theory of personality. In: Millon T, Lerner MJ, Weiner IB, editors. Comprehensive Handbook of Psychology, Personality and Social Psychology. Wiley & Sons; Hoboken, NJ: 2003. pp. 159–184. [Google Scholar]
- 25.Ghorbani N, Watson PJ. Validity of Experiential and Reflective Self-knowledge Scales: relationships with basic need satisfaction among Iranian factory workers. Psychol Rep. 2006;98:727–733. doi: 10.2466/pr0.98.3.727-733. [DOI] [PubMed] [Google Scholar]
- 26.Katz L, Epstein S. Constructive thinking and coping with laboratory-induced stress. J Pers Soc Psychol. 1991;61:789–800. doi: 10.1037//0022-3514.61.5.789. [DOI] [PubMed] [Google Scholar]
- 27.Nader T, Rothenberg S, Averbach R, Charles B, Fields JZ, Schneider RH. Improvements in chronic diseases with a comprehensive natural medicine approach: a review and case series. Behav Med. 2000;26:34–46. doi: 10.1080/08964280009595751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Jevning R, Wallace RK, Beidebach M. The physiology of meditation: a review. A wakeful hypometabolic integrated response. Neurosci Biobehav Rev. 1992;16:415–424. doi: 10.1016/s0149-7634(05)80210-6. [DOI] [PubMed] [Google Scholar]
- 29.Wallace RK. Physiological effects of transcendental meditation. Science. 1970;167:1751–1754. doi: 10.1126/science.167.3926.1751. [DOI] [PubMed] [Google Scholar]
- 30.Dillbeck MC, Orme-Johnson DW. Physiological differences between Transcendental Meditation and rest. American Psychologist. 1987;42:879–881. [Google Scholar]
- 31.Infante JR, Torres-Avisbal M, Pinel P, Vallejo JA, Peran F, Gonzalez F, Contreras P, Pacheco C, Roldan A, Latre JM. Catecholamine levels in practitioners of the transcendental meditation technique. Physiol Behav. 2001;72:141–146. doi: 10.1016/s0031-9384(00)00386-3. [DOI] [PubMed] [Google Scholar]
- 32.Travis F, Wallace RK. Autonomic and EEG patterns during eyes-closed rest and transcendental meditation (TM) practice: the basis for a neural model of TM practice. Conscious Cogn. 1999;8:302–318. doi: 10.1006/ccog.1999.0403. [DOI] [PubMed] [Google Scholar]
- 33.Roth R. Maharishi Mahesh Yogi’s Transcendental Meditation. Primus; Washington, DC: 2002. pp. 90–102. [Google Scholar]
- 34.Schneider RH, Staggers F, Alxander CN, Sheppard W, Rainforth M, Kondwani K, Smith S, King CG. A randomised controlled trial of stress reduction for hypertension in older African Americans. Hypertension. 1995;26:820–827. doi: 10.1161/01.hyp.26.5.820. [DOI] [PubMed] [Google Scholar]
- 35.Paul-Labrador M, Polk D, Dwyer JH, Velasquez I, Nidich S, Rainforth M, Schneider R, Merz CN. Effects of a randomized controlled trial of transcendental meditation on components of the metabolic syndrome in subjects with coronary heart disease. Arch Intern Med. 2006;166:1218–1224. doi: 10.1001/archinte.166.11.1218. [DOI] [PubMed] [Google Scholar]
- 36.Schwartz AR, Gerin W, Davidson KW, Pickering TG, Brosschot JF, Thayer JF, Christenfeld N, Linden W. Toward a causal model of cardiovascular responses to stress and the development of cardiovascular disease. Psychosom Med. 2003;65:22–35. doi: 10.1097/01.psy.0000046075.79922.61. [DOI] [PubMed] [Google Scholar]
- 37.Julius S, Nesbitt S. Sympathetic overactivity in hypertension: A moving target. J Hypertens. 1996;9:113S–120S. doi: 10.1016/0895-7061(96)00287-7. [DOI] [PubMed] [Google Scholar]
- 38.Walton KG, Schneider RH, Nidich SI, Salerno JW, Nordstrom CK, Bairey Merz CN. Psychosocial stress and cardiovascular disease Part 2: effectiveness of the Transcendental Meditation program in treatment and prevention. Behav Med. 2002;28:106–123. doi: 10.1080/08964280209596049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Andersen BL. Biobehavioral outcomes following psychological interventions for cancer patients. J Consult Clin Psychol. 2002;70:590–610. doi: 10.1037//0022-006X.70.3.590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Weinrich S, Weinrich M, Hardin S, Gleaton J, Pesut DJ, Garrison C. Effects of psychological distress on blood pressure in adolescents. Holist Nurs Pract. 2000;15:57–65. doi: 10.1097/00004650-200010000-00008. [DOI] [PubMed] [Google Scholar]