Abstract
Background
The Clock-in-the-Box is a rapid (2 minute) cognitive screening tool. The purpose of this study was a) to compare the Clock-in-the-Box with the Mini-Mental State Exam (MMSE) and neuropsychological tests, b) to determine Clock-in-the-Box score normative values by age and education group, and c) to determine if the Clock-in-the-Box score is associated with measures of physical function.
Methods
Community-dwelling older participants in the Boston-area were recruited for a prospective, longitudinal study in which they completed a variety of cognitive and functional assessments.
Results
At baseline, participants (n=798; mean age (±SD)=78.2 (±5.5) years; 14 (±3) mean years of education) completed in-home assessments of cognition – the Clock-in-the-Box and MMSE; measures of independent function - Activities of Daily Living and Instrumental Activities of Daily Living; and measures of physical function - Short Physical Performance Battery. Mean MMSE score was 27.1 (±1.6; range 0–30 – 0 worst) and mean Clock-in-the-Box was 6.2 (±1.6; range 0–8 – 0 worst). Performance on the Clock-in-the-Box was correlated (Spearman) with the MMSE (r=0.49, p<.001) and neuropsychological measures (r=0.37–0.50; p<.001). Higher Clock-in-the-Box score was significantly associated with no difficulty in Activities of Daily Living (χ2=39.6, p=<.001) and Instrumental Activities of Daily Living (χ2=35.5, p=<.001). Additionally, higher Clock-in-the-Box scores were associated with higher scores on the Short Physical Performance Battery (F=5.4, p<.001).
Conclusion
The Clock-in-the-Box is a brief cognitive screening test that is correlated with the MMSE, neuropsychological tests, and measures of independent and physical function in community-dwelling older adults.
Keywords: cognition, aged, function, dementia, screening, neuropsychological testing
Introduction
As the population ages and life-expectancy rises, the prevalence of age-associated diseases and syndromes, such as dementia, will likely increase. Currently in the United States, 40 million people are ≥65 years of age and this population will double by 2040, with the largest growth in those over 85 years old.(1) At age 65, the lifetime risk for Alzheimer's Disease is 9.1% for men and 17.2% for women and this risk increases with advancing age.(2) With the growing older population and increased age-associated dementia risk, the prevalence of Alzheimer's Disease and other cognitive impairments will increase in the future. Because dementia is costly and debilitating for patients and families, improved methods of screening for cognitive impairment are necessary.
Screening for cognitive dysfunction is challenging in the clinical setting, because of the complexity and training necessary to complete the cognitive assessment, the psychometric properties of the cognitive screening tests, and the limited time available for screening in a busy clinical practice.(3–5) For example, the Mini-Mental State Exam (MMSE) is a widely-used screening and monitoring instrument that requires 7–10 minutes to administer.(6, 7) The MMSE evaluates orientation, memory, attention, language, and visuospatial function, but does not assess executive function.(8) While memory loss is a requirement for the diagnosis of dementia, independent functioning may be most linked to executive functions(9) and executive dysfunction may precede the memory disturbance of dementia.(10, 11)
The Clock Drawing Test is a useful screening test(12), because of the inclusion of executive function components. The Clock-in-the-Box test was developed as an enhancement to the traditional Clock Drawing Test(13, 14) by including two specific modifications to strengthen the planning and working memory components: a) instructions are provided in written form to the examinee and b) the response is to be provided in a predetermined location on the response form. The Clock-in-the-Box reduces verbal administration cues, requiring the participant to read a page containing four written instructions, and return the instructions prior to completing the task on the response page.
The purpose of this analysis was to compare performance on the Clock-in-the-Box to the MMSE and measures of function in a community-dwelling, older population. We hypothesized that a) performance on the Clock-in-the-Box would be well correlated with MMSE and neuropsychological test performance and b) that the Clock-in-the-Box would be associated with measures of function including Activities of Daily Living (ADL), Instrumental Activities of Daily Living (IADL), and the Short Physical Performance Battery (SPPB). As a secondary objective, we sought to describe the psychometric properties by developing age and education normative scores for the Clock-in-the-Box.
Methods
Study participants
The Maintenance Of Balance, Independent Living, Intellect, and Zest in the Elderly (MOBILIZE) Boston study is a prospective longitudinal cohort study of community-dwelling seniors. Details of the study recruitment and design have been previously published elsewhere.(15) Briefly, from June 2005-March 2007, 816 participants were recruited via door-to-door visits by study staff. Inclusion criteria for participation in the MOBILZE study included age over 70 years, English-speaking, and living within a 5-mile radius of the Hebrew SeniorLife in Boston. Participation in the study included a 3-hour in-home interview in which trained research assistants administered cognitive testing and surveys and a later follow-up outpatient visit for functional assessment. The results from the baseline home visit were used for the present analysis. This study excluded individuals scoring < 18 (n = 7) on the MMSE and participants unable to complete the Clock-in-the-Box because of physical or vision limitations (n=11). Thus, 798 participants completed the Clock-in-the-Box, MMSE, and neuropsychological testing at baseline in the MOBILIZE Boston study.
Brief Description of Tools
Mini Mental State Examination
The MMSE is a widely-used and well-validated cognitive screening test that is scored on a 30-point scale, with low scores indicating worse performance. While many cutoff values for MMSE have been used, traditionally a cutoff of <24 signifies cognitive impairment and scores <18 indicate moderate – severe cognitive impairment.(16) Using a cutoff score of <24 in an outpatient general medical practice, the MMSE is reported to have sensitivity of 69% and specificity of 99% for dementia.(17) Education and age biases exist with the MMSE, with higher scores correlated to younger age and increasing education.(7)
Clock-in-the-Box
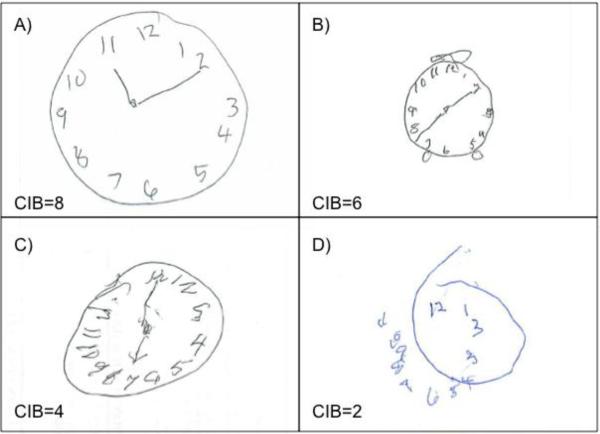
The Clock-in-the-Box is a clock drawing task with a strengthened working memory and planning component. The participant was given a sheet with four typed directions (“1. In the blue box on the next page, 2. Draw a picture of a clock, 3. Put in all the numbers, 4. Set the time to ten after eleven.”) After acknowledgement that the directions have been read and understood, the participant returned the instructions and was given the response sheet, which has a colored box in each of the quadrants (yellow, red, green and blue). The blue box is oriented in the right, lower quadrant. The participant was not allowed to refer to the directions and no additional hints or clues were provided. In the case of visual limitation or illiteracy, the administrator read the instructions to the participant, but the participant needed to see the stimulus sheet to complete the task. The Clock-in-the-Box was scored on eight criteria (one point each; range 0–8; lower scores indicate poorer performance) including: drawing located in the blue box, object resembles a clock, number inclusion, number order, number spacing, correct time, clock of appropriate size, and hand origin and length. Prior work demonstrated that the Clock-in-the-Box takes approximately 2-minutes and has high agreement (93%) and weighted kappa (k=0.72, p<.0001) between a trained interviewer and a neuropsychologist scoring.(18). Figure 1 illustrates sample clock drawings at different scoring levels.
Figure 1. Sample Clock Drawing.
The four panels (A, B, C, and D) display Clock-in-the-Box scores of 8, 6, 4, and 2, display. Panel A) represents a Clock-in-the-Box score of 8 because the clock was drawn in the blue box (not shown), the circle is large enough to accommodate the numbers, all numbers are present in the correct order and appropriately spaced, as well as the time is correct with hands originating from near the center. Panel B) represents a clock score of 6, with two points deducted for the incorrect time and completion in an incorrect (yellow) box. Panel C) resembles a clock, is appropriate size to accommodate all of the numbers, was drawn in the blue box, and has appropriate hand origin and length. Points were not given because the number 12 is repeated, the number 3 is not legible, the spacing is not uniform, and the time is incorrect. Panel D) represents a score of 2 because it resembles a clock and was drawn in the correct box. Points were not given for number inclusion, number order (3 is repeated), the numbers are not evenly spaced, the circle is not completed, no time is indicated and no hands are drawn.
Neuropsychological Assessment
A brief neuropsychological battery was administered by trained interviewers. The measures included Trailmaking A, Trailmaking B, the Hopkins Verbal Learning Test - Revised, phonemic fluency, and semantic fluency. Trailmaking A is a measure of psychomotor speed in which the participant is asked to connect circled numbers in order.(19) Trailmaking B is a test of executive function that involves shifting attentional abilities.(19) Performance is based on completion time for both Trailmaking Test A and B. The Hopkins Verbal Learning Test-Revised (HVLT), a 12 item verbal learning and recall measure(20) was also administered. HVLT subscales were calculated in accordance with the manual and included: the number of items recalled in the initial three learning trials (immediate recall) and the number of spontaneously recalled items (delayed recall). Fluency tasks assess generative language and lexical knowledge by requiring the participant to spontaneously generate words belonging to a specific category (semantic)(21) or beginning with a specific letter (phonemic).(21)
Activities of Daily Living
The Activities of Daily Living (ADL) assessment is a self-reported survey of ability to perform general daily tasks, e.g. bathing, dressing, transferring, continence, and eating.(22) ADLs were scored on a three point scale with 0 — representing no difficulty, 1 – some difficulty, and 2 — a lot of difficulty. For this analysis, we compared those with no difficulty in any ADL (intact ADL) to those with some difficulty in ≥1 ADL, because of extreme skew in ADL performance (e.g. very few participants were highly impaired).
Instrumental Activities of Daily Living
The Instrumental Activities of Daily Living (IADL) assessment evaluates the ability to complete more complex daily tasks.(23) Because of the focus on physical function, the MOBILIZE study evaluated participants' level of difficulty performing 4 mobility-related IADL tasks: shopping, preparing meals, and light and heavy housework. The same scoring scale for ADLs was applied to IADLs.
Short Physical Performance Battery
The SPPB assesses balance, mobility, and lower extremity function using three timed measures. The participant is asked to rise from a seated position five consecutive times without assistance from the upper extremities, maintain balance while standing, and complete a 4m walk. The SPPB is scored on a scale of 0–12 (0—worst physical performance). Lower scores correlate with increased risk for nursing home admission, disability, and mortality.(24) Forty patients did not complete the SPPB performed at a follow-up visit and were not included in the analysis of SPPB. There was no difference among these patients with respect to age, sex, education, or MMSE (results not shown)
Other Covariates
Through participant interview, information about demographics, living status, and comorbidity was collected. As provided by the participant, we recorded the highest educational year completed. To improve clinical utility, we divided the population into those with less than 12 years of education, high school, college, and graduate school.
Statistical Analysis
All statistical analyses were completed with Stata 9.2 (Stata, Inc. College Station, TX). The normal distribution was assessed for all variables using a histogram. When comparing MMSE and Clock-in-the-Box, three analyses were performed to compare the MMSE and Clock-in-the-Box: a) a Spearman correlation, b) a partial correlation with age and education adjustment, and c) an ANOVA. The neuropsychological tests were compared to the Clock-in-the-Box using a Spearman correlation. The association between performance on the Clock-in-the-Box and ADL and IADL function was examined with a Chi-square test. The association between Clock-in-the-Box performance and physical performance on the SPPB was assessed with ANOVA.
Results
Characteristics of the study population are presented in Table 1. The average age was 78.2 ±5.5 years, with a nearly 2:1 female: male ratio. The MOBILIZE study was reflective of the demographic composition of greater Boston with self-identified race of white (78%), black (16%), and other (6%). This was an educated population, with an average of 14 grades completed. High average MMSE and Clock-in-the-Box scores (27.1 ±1.6 and 6.2 ±1.6, respectively) indicated a generally cognitively intact population. As a community-dwelling elderly cohort, most scores on ADL, IADL, and SPPB tests indicated a relatively high level of function.
Table 1.
Characteristics of the MOBILIZE Boston Study
| Variable | Mean (SD) n (%)a (N=798) |
|---|---|
| Age, mean (SD), y | 78.2 (5.5) |
| Sex, n (%) | |
| Female | 513 (64) |
| Race, n (%) | |
| White | 622 (78) |
| Black | 126 (16) |
| Other | 50 (6) |
| Education, mean (SD), grades | 14.2 (3.1) |
| Charlson comorbidity, mean (SD) | 3.1 (1.6) |
| Marital status, n (%) | |
| Married / Living with partner | 344 (43) |
| Average MMSE Score, mean (SD) | 27.1 (2.6) |
| Average Clock-in-the-Box Score, mean (SD) | 6.2 (1.6) |
| ADL, n (%) | |
| No difficulty in any ADL (intact) | 612 (77) |
| Little/some difficulty in ≥1 ADL | 122 (15) |
| Much difficulty/inability ≥1 ADL | 64 (8) |
| IADL, n (%) | |
| No difficulty in any IADL (intact) | 472 (59) |
| Little/some difficulty in ≥1 IADL | 153 (19) |
| Much difficulty/inability ≥1 ADL | 172 (22) |
| Short Physical Performance Battery, mean (SD) | 9.3 (2.5) |
Percentages may not equal 100 as calculated values were rounded to whole numbers.
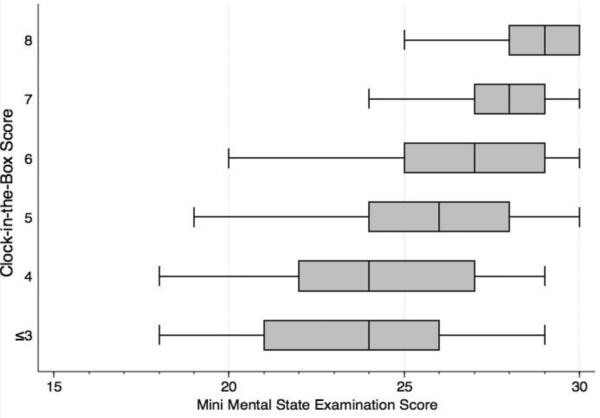
Performance on the MMSE and Clock-in-the-Box were correlated (r=0.49, 95%CI 0.44–0.55, p<.001). Taking into account age and education, MMSE and Clock-in-the-Box were correlated (r=0.42, p<.001). Figure 2 depicts the distribution of the MMSE stratified by score level. In general, the MMSE and Clock-in-the-Box decline at similar rates through the dynamic range of the MMSE (20–30). The ANOVA demonstrates a significant association (F=68.9 df(5), p<.001) with increasing MMSE and increasing Clock-in-the-Box score. As described in Table 2, the Clock-in-the-Box was also highly correlated with performance on the neuropsychological tests.
Figure 2. Clock-in-the-Box performance and Mini Mental State Examination.
The median, 25th, and 75th percentile are displayed in the box and the range is displayed with the bars.
Table 2.
Correlation of the Clock in the Box and Neuropsychological Tests
| Test | Range | Correlation with the CIB (r) | 95% Confidence Interval | p-value |
|---|---|---|---|---|
| Trailmaking A | 19 – 300 sec | −0.39 | −0.33, −0.45 | <.0001 |
| Trailmaking B | 34–300 sec | −0.50 | −0.44, −0.55 | <.0001 |
| HVLT Immediate Recall | 3 – 36 words | 0.43 | 0.38, 0.49 | <.0001 |
| HVLT Delayed Recall | 0 – 12 words | 0.45 | 0.40, 0.51 | <.0001 |
| Phonemic Fluency | 0 – 87 words | 0.37 | 0.31, 0.43 | <.0001 |
| Semantic Fluency | 4 – 35 words | 0.40 | 0.34, 0.46 | <.0001 |
CIB – Clock-in-the-Box; HVLT – Hopkins Verbal Learning Test, sec - seconds
The normative Clock-in-the-Box values for age and education are displayed in Table 3. As with the MMSE, age and education impact performance, such that higher Clock-in-the-Box or MMSE scores correlate to younger age and increasing years of education. However, the association appears stronger for education than age. Across the age range of 70 to >85, the Clock-in-the-Box changed by less than one point (median 0.7 points, range 0.4–1.1). With respect to education, the change from <HS to beyond college was about 1.5 points (median 1.7, range 1.5–2.1) for each age category. There was no effect of gender on clock in the box performance.
Table 3.
Clock-in-the-Box Score norms for age & education
| Education |
||||
|---|---|---|---|---|
| Age (years) | <High School Mean(SD) | High School Mean(SD) | College Mean(SD) | Graduate School Mean(SD) |
| 70–74 | 5.2 (1.9) | 6.3 (1.7) | 6.6 (1.2) | 7.1 (1.1) |
| 75–79 | 5.1 (1.9) | 6.3 (1.6) | 6.4 (1.3) | 6.6 (1.4) |
| 80–84 | 4.6(1.9) | 5.8 (1.5) | 5.9 (1.6) | 6.7 (1.2) |
| ≥85 | 4.9 (1.3) | 5.4 (1.3) | 5.8 (1.7) | 6.5 (1.5) |
The association between Clock-in-the-Box score and performance on the Clock-in-the-Box relative to performance on measures of functional status is displayed in Table 4. Better performance on the Clock-in-the-Box was significantly associated with the percentage of participants with intact ADLs (X2=39.6, p=<.001) such that 88% of those with Clock-in-the-Box = 8 reported intact ADLs, whereas for people scoring ≤3 on the Clock-in-the-Box, only 59% reported intact ADLs. Similarly, this significant trend was also observed when examining the IADLs: lower Clock-in-the-Box score was associated with a lower percentage of people reporting intact IADLs. SPPB scores illustrated the trend observed with ADL and IADLs; Mean SPPB scores ranged from 8.1 with a Clock-in-the-Box ≤3 to 10.0 with a Clock-in-the-Box=8.
Table 4.
Functional Status (Activities of Daily Living, Independent Activities of Daily Living, Short Physical Performance Battery) by Clock-in-the-Box Score
| Clock-in-the-Box Score | Intact ADL n/N (%) | Intact IADL n/N (%) | SPPB* Mean (SD) |
|---|---|---|---|
| ≤3 | 25/42 (59.5) | 20/42 (47.6) | 8.1 (2.7) |
| 4 | 34/54 (63.0) | 27/54 (50.0) | 8.7 (2.4) |
| 5 | 76/114 (66.7) | 60/114 (52.6) | 8.0 (3.0) |
| 6 | 144/180 (80.0) | 110/180 (61.1) | 9.5 (2.4) |
| 7 | 177/232 (76.3) | 133/231 (57.6) | 9.6 (2.3) |
| 8 | 156/176 (88.6) (χ2=39.6, p=<.001) | 122/176 (69.3) (χ2=35.5, p=<.001) | 10.0 (1.9) (F=5.4, p<.001) |
Abbreviations: ADL, Activities of Daily Living; IADL, Independent Activities of Daily Living; SPPB, Short Physical Performance Battery
Forty patients were unable to complete the SPPB and were not included in this analysis.
Discussion
This study evaluated performance of a rapid cognitive screening assessment, the Clock-in-the-Box, in a ethnically-diverse, community-dwelling older population and found that performance on the Clock-in-the-Box was correlated with the MMSE, neuropsychological tests, and was significantly associated with functional measures. Consistent with most cognitive tests, there were educational and age-associated changes in the Clock-in-the-Box performance. However, in a busy clinical setting, screening with a cognitive assessment such as the Clock-in-the-Box could provide valuable information about cognition in a short time.
In addition to the time benefit, the Clock-in-the-Box may have some advantages over traditional cognitive screening tests, because of the executive function screening. Prior work has determined that measures of executive function are perhaps more important for independent function relative to measures of memory and orientation.(9) Additionally, measures of executive function have been related to gait and balance in older patients (9, 25) Consistent with this concept, recent studies with the Clock-in-the-Box in diabetic(26) and cardiac surgery(18) patients found better Clock-in-the-Box performance was associated with improved glycemic control and return to home, respectively. Thus, our finding that the Clock-in-the-Box was associated with functional outcomes has face validity.
Consistent with all cognitive tests, the Clock-in-the-Box is limited by patient factors that may affect performance. Similar to the MMSE, the Clock-in-the-Box is associated with differential performance based on education and age. By publishing normative data for this community-dwelling population of older patients, primary care providers will be able to use the Clock-in-the-Box and compare performance in their patients. Inevitably, a cognitive test that requires reading and writing will be associated with educational level. As less education has been identified as an independent risk factor in the development of dementia,(27) memory may be the area most affected by age and education biases.(28) Higher rates of false positives (i.e. lower scores) are observed for individuals with less education(29) and the most accurate portrayal of an individual's cognitive function may be best understood in the context of education-matched controls. Consequently, existence of documented education bias means that neither the MMSE nor the Clock-in-the-Box should be used alone to diagnose dementia, although they can serve as valuable screening tools that indicate when further testing is necessary.
There are strengths to this work. The MOBILIZE study was a large-scale, prospective, observational study, evaluating 798 older adults who are representative of the local sex, ethnic, and racial distributions in people ≥70 years in the Boston area. As a community-dwelling population, participants were generally cognitively and physically functional. The comparison to both other cognitive screening measures, as well as, neuropsychological tests increases the face validity that the Clock-in-the-Box is capturing a snapshot of cognitive function and is suitable as a screening measure. These factors improve external validity (generalizability), especially to physicians who care for older patients in primary care practices.
This study also has limitations. First, individuals scoring <18 on the MMSE were excluded from this project. Thus, the population was relatively cognitively intact. Future studies should be directed toward more cognitively impaired populations to determine if the MMSE and Clock-in-the-Box correlation observed in this population still stands in advanced stages of dementia. Because memory impairment is a fundamental component of the definition of both dementia and mild cognitive impairment, further comparison of the Clock-in-the-Box with neuropsychological measures of memory is required. Additionally, more thorough comparison of Clock-in-the-Box score to patients with a diagnosis of dementia would be helpful. Secondly, the Clock-in-the-Box measure is scored on a 0 to 8 scale and likely has floor and ceiling effects, like all cognitive screening tools and some neuropsychological tests. The floor effects in this study are likely minimized by the exclusion of participants with a MMSE score <18. Future studies of participants with lower performance will likely improve understanding of the functional and cognitive effects of low Clock-in-the-Box scores. The ceiling effects of the MMSE limit the variability at higher levels of Clock-in-the-Box performance. While the ceiling effects may limit the utility of correlation coefficients as a measure of comparison, the neuropsychological tests used in this study were selected to minimize ceiling effects. Third, the Clock-in-the-Box is a cognitive screening test and at this time, its use should be limited to screening patients who may benefit from further cognitive assessment for diagnosis or management. Fourth, standardized training on administration and scoring would provide a sound basis for implementation of the Clock-in-the-Box into clinical practice and future studies. Finally, this study did not measure cognitive performance longitudinally. Thus, further studies of the Clock-in-the-Box are required to determine if there are changes in Clock-in-the-Box performance with aging, re-testing, or pathologic cognitive impairments.
Due to the importance of assessing early decline or change in cognitive function, the Clock-in-the-Box may be useful as a screening tool in a busy clinical setting. The Clock-in-the-Box takes 2 minutes to administer and was correlated with cognitive screening and neuropsychological measures. In this study, we published normative values of Clock-in-the-Box based on age and education, as well as describing the association of functional performance with Clock-in-the-Box score. Thus, the Clock-in- the-Box may be a rapid and effective screening measure for evaluating early cognitive decline and monitoring change in cognition in the primary care setting, but additional cognitive assessment would be required to diagnose dementia.
The Clock-in-the-Box is a brief (2-minute) cognitive screening instrument that was well correlated with performance on other cognitive screening instruments and neuropsychological tests in a large cohort study of community-dwelling elders.
The Clock-in-the-Box was associated with measures of independent function
The article reports age and education normative values for the Clock-in-the-Box
Cognitive screening instruments alone are insufficient to diagnose dementia
Acknowledgements
The MOBILIZE Boston Study is funded by NIH/NIA under grant number P01AG004390. The authors acknowledge the MOBILIZE Boston research team and study participants for the contribution of their time, effort, and dedication. Ms. Chester was funded by an Einstein Research Fellowship. Dr. Rudolph is funded by a VA Rehabilitation Career Development Award. Additional Support provided by the American Federation for Aging Research, the Boston MSTAR, and NIH grants (AG038027-01 AG023480, AG08812, and AG029861). The Clock-in-the-Box was developed by Dr. Grande with contributions from Drs. Milberg and McGlinchey. All were VA employees at the time.
Funding: Ms. Chester was funded by an Einstein Research Fellowship. Dr. Rudolph is funded by a VA Rehabilitation Career Development Award. Additional Support provided by the American Federation for Aging Research, the Boston MSTAR, and NIH grants (AG038027-01 AG023480, AG08812, and AG029861). The Data for this project was collected by the Hebrew SeniorLife / Harvard Research Nursing Home-MOBLIZE Boston Project (AG004390).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest: The Authors have no conflict of interests. The Clock-in-the-Box was developed by Dr. Grande with contributions from Drs. Milberg and McGlinchey. All were VA employees at time.
References
- 1.National Population Projections. US Census Bureau; 2008. Projections of the Population by Selected Age Groups and Sex for the United States: 2010 to 2050. Released. Based on Census 2000. [Google Scholar]
- 2.Plassman BL, Langa KM, Fisher GG, et al. Prevalence of dementia in the United States: the aging, demographics, and memory study. Neuroepidemiology. 2007;29(1–2):125–32. doi: 10.1159/000109998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chodosh J, Petitti DB, Elliott M, et al. Physician recognition of cognitive impairment: evaluating the need for improvement. J Am Geriatr Soc. 2004;52(7):1051–9. doi: 10.1111/j.1532-5415.2004.52301.x. [DOI] [PubMed] [Google Scholar]
- 4.Valcour VG, Masaki KH, Curb JD, Blanchette PL. The detection of dementia in the primary care setting. Arch Intern Med. 2000;160(19):2964–8. doi: 10.1001/archinte.160.19.2964. [DOI] [PubMed] [Google Scholar]
- 5.Boise L, Camicioli R, Morgan DL, et al. Diagnosing dementia: perspectives of primary care physicians. Gerontologist. 1999;39(4):457–64. doi: 10.1093/geront/39.4.457. [DOI] [PubMed] [Google Scholar]
- 6.Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12(3):189–98. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 7.Crum RM, Anthony JC, Bassett SS, Folstein MF. Population-based norms for the Mini-Mental State Examination by age and educational level. JAMA. 1993;269(18):2386–91. [PubMed] [Google Scholar]
- 8.Nys GM, van Zandvoort MJ, de Kort PL, et al. Restrictions of the Mini-Mental State Examination in acute stroke. Arch Clin Neuropsychol. 2005;20(5):623–9. doi: 10.1016/j.acn.2005.04.001. [DOI] [PubMed] [Google Scholar]
- 9.Royall DR, Palmer R, Chiodo LK, Polk MJ. Declining executive control in normal aging predicts change in functional status: the Freedom House Study. J Am Geriatr Soc. 2004;52(3):346–52. doi: 10.1111/j.1532-5415.2004.52104.x. [DOI] [PubMed] [Google Scholar]
- 10.Binetti G, Magni E, Padovani A, et al. Executive dysfunction in early Alzheimer's disease. J Neurol Neurosurg Psychiatry. 1996;60(1):91–3. doi: 10.1136/jnnp.60.1.91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lafleche G, Albert M. Executive function deficits in mild Alzheimer's disease. Neuropsychology. 1995;9(3):313–20. [Google Scholar]
- 12.Shulman KI. Clock-drawing: is it the ideal cognitive screening test? Int J Geriatr Psychiatry. doi: 10.1002/1099-1166(200006)15:6<548::aid-gps242>3.0.co;2-u. [DOI] [PubMed] [Google Scholar]
- 13.Grande LJ, Milberg WP, Rudolph JL, et al. A timely screening for executive functions and memory. J Int Neuropsychol Soc. 2005;11(S1):9–10. [Google Scholar]
- 14.Grande LJ, Rudolph JL, Milberg WP, et al. Detecting cognitive impairment in individuals at risk for cardiovascular disease: the “Clock-in-the-Box” screening test. Int J Geriatr Psychiatry. 2011 doi: 10.1002/gps.2635. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Leveille SG, Kiel DP, Jones RN, et al. The MOBILIZE Boston Study: design and methods of a prospective cohort study of novel risk factors for falls in an older population. BMC Geriatr. 2008;8:16. doi: 10.1186/1471-2318-8-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pasqualetti P, Moffa F, Chiovenda P, et al. Mini-mental state examination and mental deterioration battery: analysis of the relationship and clinical implications. J Am Geriatr Soc. 2002;50(9):1577–81. doi: 10.1046/j.1532-5415.2002.50416.x. [DOI] [PubMed] [Google Scholar]
- 17.Tangalos EG, Smith GE, Ivnik RJ, et al. The Mini-Mental State Examination in general medical practice: clinical utility and acceptance. Mayo Clin Proc. 1996;71(9):829–37. doi: 10.4065/71.9.829. [DOI] [PubMed] [Google Scholar]
- 18.Harrington MB, Kraft M, L.J. G, Rudolph JL. Preoperative cognitive status is independently associated with cognitive status after cardiac surgery. Am J Crit Care. 2010 doi: 10.4037/ajcc2011275. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Trailmaking Tests A and B. War Department Adjutant General's Office; Washington, DC: 1944. [Google Scholar]
- 20.Brandt J, Benedict RHB. Hopkins Verbal Learning Test-Revised (HVLT) Psychological Assessment Resources, Inc; Lutz, FL: 1991. [Google Scholar]
- 21.Benton AL, Hamsher K. Multilingual aphasia examination. University of Iowa; Iowa City: 1976. [Google Scholar]
- 22.Katz S, Ford AB, Moskowitz RW, et al. Studies of Illness in the Aged. The Index of Adl: A Standardized Measure of Biological and Psychosocial Function. JAMA. 1963;185:914–9. doi: 10.1001/jama.1963.03060120024016. [DOI] [PubMed] [Google Scholar]
- 23.Lawton MP, Brody EM. Assessment of older people: self-maintaining and instrumental activities of daily living. Gerontologist. 1969;9(3):179–86. [PubMed] [Google Scholar]
- 24.Guralnik JM, Simonsick EM, Ferrucci L, et al. A short physical performance battery assessing lower extremity function: association with self-reported disability and prediction of mortality and nursing home admission. J Gerontol. 1994;49(2):M85–94. doi: 10.1093/geronj/49.2.m85. [DOI] [PubMed] [Google Scholar]
- 25.Kuo HK, Lipsitz LA. Cerebral white matter changes and geriatric syndromes: is there a link? J Gerontol A Biol Sci Med Sci. 2004;59(8):818–26. doi: 10.1093/gerona/59.8.m818. [DOI] [PubMed] [Google Scholar]
- 26.Munshi M, Grande L, Hayes M, et al. Cognitive dysfunction is associated with poor diabetes control in older adults. Diabetes Care. 2006;29(8):1794–9. doi: 10.2337/dc06-0506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Schmand B, Lindeboom J, Hooijer C, Jonker C. Relation between education and dementia: the role of test bias revisited. J Neurol Neurosurg Psychiatry. 1995;59(2):170–4. doi: 10.1136/jnnp.59.2.170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ganguli M, Snitz BE, Lee CW, et al. Age and education effects and norms on a cognitive test battery from a population-based cohort: the Monongahela-Youghiogheny Healthy Aging Team. Aging Ment Health. 2010;14(1):100–7. doi: 10.1080/13607860903071014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Anthony JC, LeResche L, Niaz U, et al. Limits of the `Mini-Mental State' as a screening test for dementia and delirium among hospital patients. Psychol Med. 1982;12(2):397–408. doi: 10.1017/s0033291700046730. [DOI] [PubMed] [Google Scholar]