Abstract
BACKGROUND:
Patients have a major role in the control and treatment of type 2 diabetes. So, knowledge of different aspects of this disease especially diet therapy is very important for these patients. This study was conducted to determine the effectiveness of the Health Belief Model (HBM) on nutrition education in type 2 diabetic patients.
METHOD:
Eighty eight type 2 diabetic patients attending Iranian Diabetes Association seminars were randomly selected to participate in the study (44 in intervention group and 44 in control group). The intervention was consisted of two educational sessions each one for 80 minutes. Data were collected by a validated and reliable questionnaire (58 questions) before intervention and one month after intervention.
RESULTS:
After intervention, knowledge scores increased in the intervention group compared to the control group (Mean differences in the intervention and test group: 22.68 ± 15.90 vs - 2.27 ± 17.30, P < 0.001). Perceived susceptibility increased significantly in the intervention group compared to the control group (27.5 ± 18.5 vs 3.9 ± 17.2, P < 0.001). The result was the same for perceived severity, perceived threatened and perceived benefits (P < 0.001). In contrast perceived barriers reduced in the intervention group compared to the control diet (-14.7 ± 13.3 vs 0.9 ± 13.9, P < 0.001). In the intervention group, behavior grades increased more than control group (34.61 ± 14.93 vs -0.23 ± 8.52, P < 0.001).
CONCLUSION:
The efficacy of the health belief model in nutritional education to the diabetic patients was confirmed in the present study.
Keywords: Type 2 diabetes mellitus, nutritional behavior, Health Belief Model, nutritional education
Diabetes is a clustering of common metabolic disorders resulting in hyperglycemia. In the USA, diabetes mellitus is the major cause of end-stage renal disease, non traumatic amputation in lower limps and adult blinding. It is expected that diabetes remain the most common cause of death in the coming decades.1
According to a community based study 10.8% of the population in the older onset diabetes group had low vision and 2.7% had legal blindness.2
Cardiovascular diseases are responsible for 75% of death among diabetic patients in industrial countries and 50% of patients with diabetes have retinopathy.3
In Iran, it is said that 7.7% of adults aged 25-64 years (2 million) have diabetes and 16.8% (4.4 million) of Iranian adults had impaired fasting glucose.4
Diet is a key factor in controlling diabetes. Diet therapy is a necessary component of the treatment and may result in lower costs of the disease.5 Since the patients have a major role in the control and treatment of type 2 diabetes, it is important to provide them with self-management education and diet therapy.6 The importance of education depends upon its behavioral impact. Health Belief Model is recommended for nutrition education to increase the impact of educational programs.7 A major feature of this model holds that the patients have choices and are able to make suitable decisions regarding their health. This model suggests that whether or not individuals take action to protect their health depends on whether they believe that they are susceptible to an ill health condition; that the occurrence of that condition would have serious consequences; and that they have a course of action to avoid the condition and benefits of taking the action outweigh the costs.8
The components of this model are perceived as severity, susceptibility, threatened, benefits and barriers. Moreover, this model is more suitable than other models for nutrition education.8,9 Some researches also mentioned the beneficiary of applying this model in different health education programs.10,11 Anyhow, we are not aware of any study on the effects of nutritional education based on this model on the knowledge, attitude and practice of diabetic patients.
This study was conducted to determine the effectiveness of nutrition education on the knowledge of diabetic patients using health belief model.
Methods
In this semiexperimental study, 88 type 2 diabetic patients attending Iranian Diabetes Association seminars were randomly selected and divided into two groups of intervention and control (44 patients in each group). To control potential confounding factors, the two groups were matched. Inclusion criteria included age of 30 to 60 years, not to be illiterate, at least one year attendance in Iranian Diabetes Association seminars, regular followups and no sever and chronic complications of diabetes. Those patients who were not willing to participate or continue the study were excluded. The intervention was consisted of two educational sessions, each 80 minutes. Data were collected using a questionnaire with 58 questions in four sections including demographic data, nutritional knowledge, health belief models components, and nutritional practice. Validity and reliability of the questionnaire was assessed by the standard methods (the details will be reported in a forthcoming paper) .
The questionnaire was completed before and after intervention. The educational intervention was executed in 4 sessions each 40 minutes.
Nutritional education was based on the nutritional recommendations of the world health organization and American Diabetes Association.12 The patients learned about food exchange list. One month after intervention, patients were evaluated by completing the questionnaire. The knowledge section consisted of questions about dietary planning, energy intake, number of meals, and some information about healthy food for diabetic patients. Practice was assessed by food records. The components of HBM were perceived as severity, susceptibility, threatened, benefits and barriers. Data were analyzed by SPSS (version 13.0, Chicago IL). Student's t test was used to compare the values between the two groups before and after intervention. The mean differences of variables were compared by paired t test. P values less than 0.05 were considered significant.
Results
Mean of age was 47.1 ± 6.7 years for the intervention group and 49.9 ± 7.5 years for the control group.
There was no significant difference between the two groups regarding age and diabetes duration.
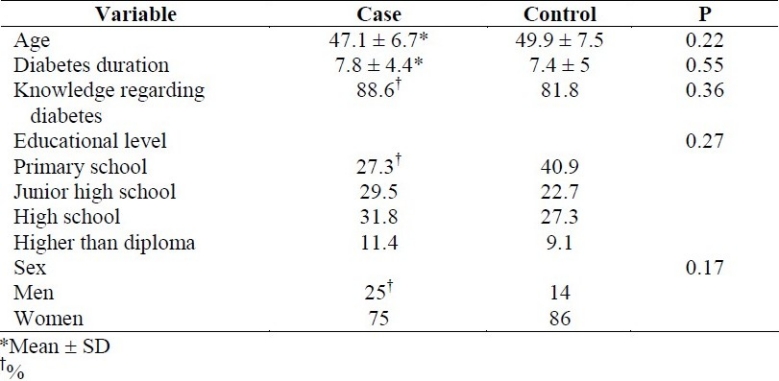
Most of the participants in both groups were women. The two groups were matched in sex, educational level and knowledge background. Demographic characteristics of the patients are presented in Table 1.
Table 1.
Demographic characteristics of diabetic patients in the case and control groups.
Before the intervention, patients were in the moderate level of the perceived susceptibility, severity, threat, benefits and barriers. There was no significant difference between the two groups regarding the components of the health belief model. After the intervention, the values of the mentioned variables increased significantly in the case group and showed a significant differences compared to the control group (p < 0.001). Table 2 shows the mean and standard deviation of the components of the health belief model in the two groups before and after intervention as well as the mean differences.
Table 2.
Mean ± SD of the Health Belief Model components in diabetic patients in the case and control groups and the mean differences.
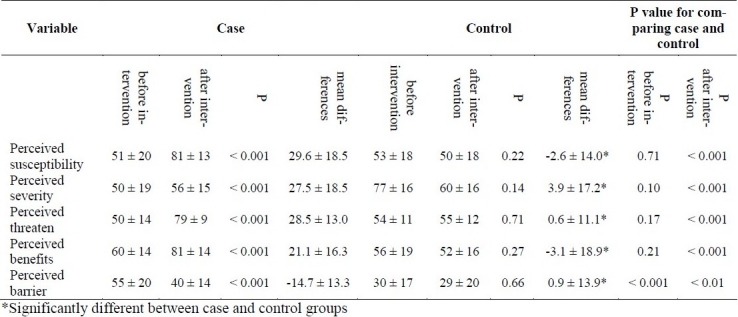
After intervention, perceived susceptibility increased significantly in the case group vs. control group (mean differences in case and control groups: 29.6 ± 18.5 vs. -2.6 ± 14.0 respectively, p < 0.001). The results was the same regarding the perceived severity (mean differences in case and control groups: 27.5 ± 18.5 vs. 3.9 ± 17.2 respectively, p < 0.001), perceived threatened (mean differences in case and control groups: 28.5 ± 13.0 vs. 0.6 ± 11.1, respectively, p < 0.001) and perceived benefits (mean differences in case and control groups: 21.1 ± 16.3 vs. -3.1 ± 18.9 respectively, p < 0.001). Perceived barriers reduced significantly after intervention in the case group compared to the control group (p < 0.001).
Table 3 compares the means of nutritional knowledge and practice before and after the intervention in the two groups and the mean differences.
Table 3.
Mean ± SD of the nutritional knowledge and practice in type2 diabetes before and after intervention in the case and control groups and the mean differences.

There was no significant difference in the knowledge scores of the two groups before the intervention but after the intervention, the knowledge scores of the case group were significantly higher than the control group (p < 0.001). Also, there were increases in the knowledge and practice scores in the case group, compared to the control (p < 0.001).
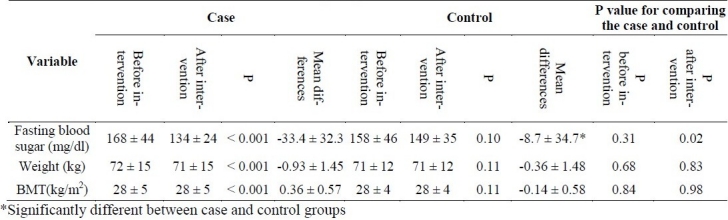
Table 4 shows the mean of the metabolic variables before and after educational intervention in the two groups. Fasting blood glucose, weight and body mass index of the two groups were not significantly different before the intervention. But after the intervention, there was a significant difference in fasting blood glucose of the two groups and it reduced significantly in the case group compared to the control group (p < 0.001). However, there was no significant difference between the two groups in weight and BMI.
Table 4.
Mean ± SD of the metabolic indices in diabetic patients before and after intervention in the case and control groups and the mean differences.
Discussion
The results of the present study showed that nutritional education could increase patients’ knowledge and reduce their fasting blood glucose.
Before the intervention, mean of knowledge scores was in the moderate level for both groups. The nutritional knowledge grades in other studies were also in the moderate grades.13 Heidari et al14 reported the grade of 68% in nutritional knowledge of diabetes before intervention, which significantly increased after the intervention. One study in Iran15 and another in Spain16 showed a significant increase in the patients’ knowledge.
The components of the health belief model were in the moderate stage in the present study. In other studies also the attitude of patients was in the moderate stage.17–20 After the intervention, in the present study, the mean values of the health belief model increased in the case group compared to the controls. This means that patients in the case group see the danger of poor adherence to the diet (the increase of perceived susceptibility) and feel the benefits of adherence to the diet (the increase of perceived benefits), and this makes them follow the diet. The main benefits of dieting for patients were mentioned as controlling their fasting blood sugar and weight, and lowering the costs of disease.
In a study by Aghamolayee et al,21 the mean values of the perceived susceptibility, severity, benefits and behavior increased after intervention and the perceived barriers reduced in the intervention group.
Brekke et al22 reported that unavailability of healthy food and lack of healthy recipes in restaurants were barriers of adherence to the diet. Polly et al23 found a significant relationship between perceived barriers and glycemic control. Vijan et al24 mentioned the high costs, life-style and lack of family support as the barriers of adherence to the diet.
Nutritional practice of the patients in both groups was poor before the intervention, but after the intervention, it increased significantly. In other studies also the practice scores increased after educational intervention.17,21 In the present study, matching the case and control groups reduced the common biases of this kind of studies.
In conclusion, health belief model improved the knowledge, attitude and practice of patients and the most increased variables were perceived susceptibility and severity. Therefore, the present study confirms the efficacy of the health belief model in nutrition education.
Authors’ Contributions
GHSH, MHE and AK designed the study, collected and analyzed the data and wrote the manuscript. LA helped with manuscript preparation.
All authors have read and approved the content of the manuscript.
Footnotes
Conflict of interest: Authors have no conflicts of interest.
References
- 1.Eknoyan G. Obesity, diabetes, and chronic kidney disease. Curr Diab Rep. 2007;7(6):449–453. doi: 10.1007/s11892-007-0076-5. [DOI] [PubMed] [Google Scholar]
- 2.Idil A, Caliskan D, Ocaktan E. The prevalence of blindness and low vision in older onset diabetes mellitus and associated factors: a community-based study. Eur J Ophthalmol. 2004;14(4):298–305. doi: 10.1177/112067210401400404. [DOI] [PubMed] [Google Scholar]
- 3.Targher G, Bertolini L, Zenari L, Lippi G, Pichiri I, Zoppini G, et al. Diabetic retinopathy is associated with an increased incidence of cardiovascular events in type 2 diabetic patients. Diabet Med. 2008;25(1):45–50. doi: 10.1111/j.1464-5491.2007.02327.x. [DOI] [PubMed] [Google Scholar]
- 4.Esteghamati A, Gouya MM, Abbasi M, Delavari A, Alikhani S, Alaedini F, et al. Prevalence of diabetes and impaired fasting glucose in the adult population of Iran: national survey of risk factors for noncommunicable diseases of Iran. Diabetes Care. 2008;31(1):96–8. doi: 10.2337/dc07-0959. [DOI] [PubMed] [Google Scholar]
- 5.Skamagas M, Breen TL, LeRoith D. Update on diabetes mellitus: prevention, treatment, and association with oral diseases. Oral Dis. 2008;14(2):105–14. doi: 10.1111/j.1601-0825.2007.01425.x. [DOI] [PubMed] [Google Scholar]
- 6.Standards of medical care for patients with diabetes mellitus. Diabetes Care. 2003;26(Suppl 1):S33–S50. doi: 10.2337/diacare.26.2007.s33. [DOI] [PubMed] [Google Scholar]
- 7.Lynch L, Happell B. Implementation of clinical supervision in action: part 2: implementation and beyond. Int J Ment Health Nurs. 2008;17(1):65–72. doi: 10.1111/j.1447-0349.2007.00512.x. [DOI] [PubMed] [Google Scholar]
- 8.Janz N, Champion V, Strecher V. The health belief model. In: Glanz K, Rimer B, LF, editors. Health behavior and health education. San Francisco: Jossey-Bass; 2002. pp. 45–66. [Google Scholar]
- 9.Spikmans FJ, Brug J, Doven MM, Kruizenga HM, Hofsteenge GH, Van Bokhorst-Vander Schueren MA. Why do diabetic patients not attend appointments with their dietitian? J Hum Nutr Diet. 2003;16(3):151–8. doi: 10.1046/j.1365-277x.2003.00435.x. [DOI] [PubMed] [Google Scholar]
- 10.Daddario DK. A review of the use of the health belief model for weight management. Medsurg Nurs. 2007;16(6):363–6. [PubMed] [Google Scholar]
- 11.Chang LC, Hung LL, Chou YW, Ling LM. Applying the health belief model to analyze intention to participate in preventive pulmonary tuberculosis chest X-ray examinations among indigenous nursing students. J Nurs Res. 2007;15(1):78–87. doi: 10.1097/01.jnr.0000387601.24908.45. [DOI] [PubMed] [Google Scholar]
- 12.Mahan LK, Escott-Stump S. 11 th ed. Philadelphia: Saunders; 2003. Krause's food, nutrition and diet therapy. [Google Scholar]
- 13.Nojoumi M, Najmabadi SH, Shakiba V, Danayei D. The study of nutritional knowledge of type 2 diabetic patients attending to Rasoul Akram Hospital in 2003. Journal of Iran University of Medical Sciences. 2005;12(47):197–204. [Google Scholar]
- 14.Heidari GH, Moslemi S, Montazerifar F, Heidari M. The effect of nutrition education on the knowledge,Attitude and practice of type 2 diabetic patients. Tabibe Shargh. 2002;4(4):207–13. [Google Scholar]
- 15.Borzou SR, Biabangardi Z. The effect of diet therapy on the blood glucose level of non-insulin dependent diabetes attending to the Rasht health care center. Journal of Zanjan University of Medical Sciences. 1999;26, 27:65–70. [Google Scholar]
- 16.Giral GA, Magana MA, Arriazu EC, Elviro BT, Aguado MG, Sandua SM. Diet based on rations.Practical teaching for type II diabetics. Rev Enferm. 1998;21(236):11–4. [PubMed] [Google Scholar]
- 17.Khabazian A, Rezaei N. The effect of education on the nutritional knowledge, attitude and practice in diabetic patients. Tolue Behdasht. 2003;2(2&3):57. [Google Scholar]
- 18.Hawthorne K, Tomlinson S. Pakistani moslems with type 2 diabetes mellitus: effect of sex, literacy skills, known diabetic complications and place of care on diabetic knowledge, reported self-monitoring management and glycaemic control. Diabet Med. 1999;16(7):591–7. doi: 10.1046/j.1464-5491.1999.00102.x. [DOI] [PubMed] [Google Scholar]
- 19.Daniel M, Messer LC. Perceptions of disease severity and barriers to self-care predict glycemic control in aboriginal persons with type 2 diabetes mellitus. Chronic Dis Can. 2002;23(4):130–8. [PubMed] [Google Scholar]
- 20.Burnet D, Plaut A, Courtney R, Chin MH. A practical model for preventing type 2 diabetes in minority youth. Diabetes Educ. 2002;28(5):779–95. doi: 10.1177/014572170202800519. [DOI] [PubMed] [Google Scholar]
- 21.Aghamolayee T, Eftekhar H, Mohammad K. The application of health belief model in changing the behavior in diabetic patients. Payesh. 2005;4(4):263–9. [Google Scholar]
- 22.Brekke HK, Sunesson A, Axelsen M, Lenner RA. Attitudes and barriers to dietary advice aimed at reducing risk of type 2 diabetes in first degree relatives of patients with type 2 diabetes. J Hum Nutr Diet. 2004;17(6):513–21. doi: 10.1111/j.1365-277X.2004.00566.x. [DOI] [PubMed] [Google Scholar]
- 23.Polly RK. Diabetes health beliefs, self-care behaviors, and glycemic control among older adults with non-insulin dependent diabetes mellitus. Diabetes Educ. 1992;18(4):321–7. doi: 10.1177/014572179201800411. [DOI] [PubMed] [Google Scholar]
- 24.Vijan S, Stuart NS, Fitzgerald JT, Ronis DL, Hayward RA, Slater S, et al. Barriers to following dietary recommendations in type 2 diabetes. Diabet Med. 2005;22(1):32–8. doi: 10.1111/j.1464-5491.2004.01342.x. [DOI] [PubMed] [Google Scholar]


