Abstract
Background:
Cerebral vasospasm is a preventable cause of death and disability in patients who experience aneurysmal subarachnoid hemorrhage (SAH). The aim of this study is to investigate the incidence of cerebral vasospasm following traumatic SAH and its relationship with different brain injuries and severity of trauma.
Methods:
This cross-sectional study was conducted from October 2006 to March 2007 in department of Neurosurgery in Al-Zahra Hospital. Consecutive head-injured patients who had SAH on the basis of an admission CT scan were prospectively evaluated. The severity of the trauma was evaluated by determining Glasgow Coma Scale (GCS) score on admission. Transcranial Doppler ultrasonography evaluations were performed at least 48 hours after admission and one week thereafter. Vasospasm in the MCA and ACA was defined by mean flow velocity (FV) of more than 120 cm/sec with a Lindegaard index (MVA/ICA FV ratio) higher than 3. Basilar artery vasospasm was defined by FV higher than 85 cm/sec.
Results:
Seventy seven patients with tSAH were enrolled from whom 13 were excluded. The remaining were 52 (81.2%) men and 12 (18.7%) women, with a mean age of 37.89 years. Trauma was severe in 11 (17.2%), moderate in 13 (20.3%), and mild in 40 (62.5%) patients. From all, 27 patients (42.1%) experienced at least one vasospasm during the study period and MCA vasospasm was the most common in the first and second weeks (55.5%).
Conclusions:
Traumatic SAH is associated with a high incidence of cerebral vasospasm with a higher probability in patients with severe TBI.
Keywords: Cerebral Vasospasm, Subarachnoid Hemorrhage, Trauma, Traumatic Brain Injury
Cerebral arterial vasospasm has long been recognized as a major cause of disability and long-term neurological deficits following aneurysmal as well as traumatic Subarachnoid Hemorrhage (SAH). While symptomatic vasospasm with neurological deterioration occurs in 20-30% of patients, radiographic vasospasm can be seen in up to 70%. The underlying pathogenic mechanisms and best management of delayed cerebral vasospasm are incompletely understood. Despite maximal therapy, nearly 50% of patients with symptomatic vasospasm will progress to cerebral infarction and 15-20% will develop a disabling stroke or death.1–3
Although several studies have been conducted on SAH with aneurysmal origin, less attention has been paid to the significance of vasospasm after traumatic SAH (tSAH). Therefore, there are not much data available on the incidence, time course, predictors, and management of vasospasm following tSAH. SAH has been reported in up to 60% of patients who have sustained traumatic brain injuries (TBI) and a significant predictor of death in patients with severe TBI.4–8 It has been shown that the incidence of vasospasm after tSAH is similar to that following aneurysm rupture.9–11 It is proposed that tSAH is a predictor of poor outcome because it may induce vasospasm and secondary cerebral ischemia.4 The aim of the present study was to investigate the incidence of cerebral vasospasm following tSAH and its relationship with different brain injuries and severity of trauma.
Methods
This cross-sectional study was conducted from October 2006 to March 2007 in department of Neurosurgery in Al-Zahra Hospital (Isfahan University of Medical Sciences). Consecutive head-injured patients who had SAH on the basis of an admission CT scan were prospectively evaluated. Patients who had received sedative drugs before evaluating Glasgow Coma Scale (GCS) score, those who underwent neurosurgery before Transcranial Doppler ultrasonography (TCD), those who had received anticoagulation drugs (e.g. heparin, warfarin), and those with penetrating head injury were excluded from the study. The severity of the trauma was evaluated by determining GCS score on admission, after resuscitation measures, and then was categorized to mild (13 to 15), moderate (9 to 12), and severe (less than 9). Calculated sample size was 64 considering estimated prevalence of 40%, confidence interval 95% and d = 0.3.
For diagnosing cerebral vasospasm, TCD evaluations were performed using MultiDop®X4 (DWL, Sipplingen, Germany) with a 2MHz pulse-waved and range-gated transducer, according to the technique described by Aaslid et al.12 The middle and anterior cerebral arteries (MCA and ACA) were insonated through the temporal acoustic window and basilar artery (BA) was assessed through the foramen magnum. Internal carotid arteries (ICAs) were insonated extracranially via the submandibular approach. Both sides were evaluated in four cardiac cycles. In every patient, TCD recordings were performed twice; once in the first week (at least 48 hours after admission) and once, one week after the first TCD recording. Vasospasm in the MCA and ACA was defined by mean flow velocity (FV) of more than 120 cm/sec with a Lindegaard index (MVA/ICA FV ratio) higher than 3, according to Aaslid et al 13 and Lindegaard et al.14 The severity of vasospasm in the MCA and ACA was categorized to severe (FV ≥ 200), moderate (150 ≤ FV < 200), and mild (120 < FV < 150). BA vasospasm was defined by a FV higher than 85 cm/sec.15
The Ethics Committee of Isfahan University of Medical Sciences approved the study protocol. Data were recorded according to the usual clinical practice and patient privacy was maintained at all times. Independent Sample t test and Chi-square test were used for statistical analysis and a p value of less than 0.05 was considered statistically significant. Analyses were done using SPSS for windows (version 16.0).
Results
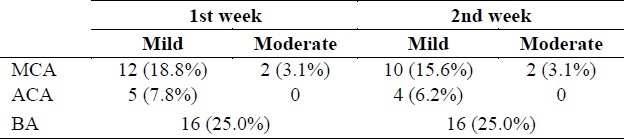
During the study period, 77 consecutive patients with tSAH were prospectively evaluated. Five patients died before the second TCD and eight patients did not participate for the second TCD. Therefore, 64 patients’ data were considered for analyses. Patients included 52 (81.3%) men and 12 (18.8%) women, with a mean age of 37.8 years (SD = 19.1, from 6 to 79). The mean GCS score was 12.0 (SD = 3.1, from 4 to 15). Trauma was severe in 11 (17.2%), moderate in 13 (20.3%), and mild in 40 (62.5%) patients. From all, 27 patients (42.1%) experienced at least one vasospasm during the study period and MCA vasospasm was the most common in the first and second weeks (15.27% and 55.5% respectively). In all patients, severity of vasospasm was limited to mild and moderate and sever vasospasm was not seen in any of them. (Table 1)
Table 1.
Vasospasm in the first and second weeks
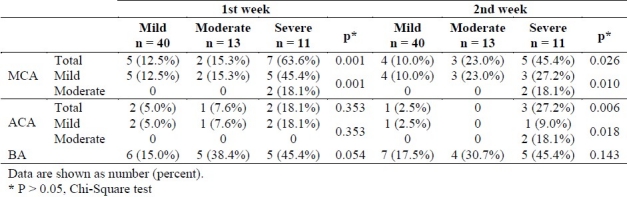
As presented in table 2, there was a relationship between the severity of trauma and the occurrence of vasospasm in MCA, ACA, and BA in the first and second weeks. But, the relationships were statistically significant only for MCA in both weeks, ACA in the second week, and slightly for BA in the first week. Also, relationship was found between the severity of trauma and the severity of vasospasm in MCA in both weeks (r = 0.381 and 0.336, p < 0.05) and in ACA in the second week (r = 0.278, p < 0.05).
Table 2.
Vasospasm in the first and second weeks in relation to severity of trauma
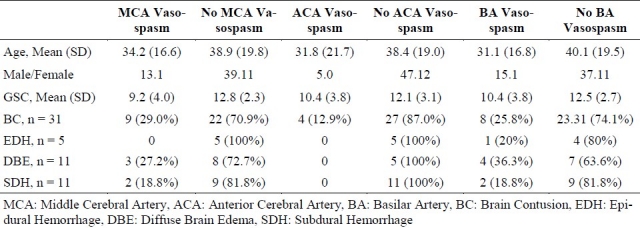
There was no relationship between the occurrence of vasospasm and sex or age. (p > 0.05) Regarding findings of CT on admission, there was not any significant relationship between various brain injuries and the occurrence of vasospasm (p > 0.05). The only difference between groups was that the mean of GCS scores were lower in patients with MCA and BA vasospasm compared to no vasospasm (p < 0.05). (Table 3)
Table 3.
Vasospasm in relation to sex, age, and brain injuries
Discussion
Compared to SAH of aneurysmal origin, trauma is the most common cause of SAH.6 Evidence showed that the incidence of vasospasm and also poor outcomes in patients with TBI increased with the presence of SAH. While vasospasm is thought to contribute to secondary brain damage by causing ischemia or by adding intensity to existing ischemia, in head injury, there are other factors which themselves may induce ischemia (e.g. edema, systemic hypoxia, and hypotension). Therefore, vasospasm plays an important role in head injury by contributing to already existing or impending ischemia.4,16–18
However, little researches have been devoted to the importance of vasospasm following tSAH. With the development of the TCD technique with good sensitivity and excellent specificity in recent years, post-traumatic cerebral vasospasm has been more often recognized. Vasospasm has been reported in 5-59% of patients following tSAH.4 In present study, we included patients with mild, moderate, and severe trauma while only patients with severe trauma (GCS < 9) have been included in most of the previous reports.4 However, we found a relationship between the severity of trauma and the occurrence of vasospasm that was significant for MCA and ACA vasospasm (p < 0.05), and slightly significant for BA vasospasm (p = 0.054). These findings are in contrast to some previous reports19–21 but similar to other ones.22,23 These various results may be related to differences in patient selection, radiologist expertise, and definition of vasospasm among the studies.
It is likely that the mechanisms involved in vasospasm following tSAH are similar to those identified in aneurysmal SAH. Several studies reported a significant correlation between the amount of SAH on CT scan and the incidence of vasospasm in head injured patients.11,20,23,24 TSAH is associated with poor outcome which is consistent with this finding that post-traumatic vasospasm's outcomes are predictive. Presence of SAH, however, does not always lead to vasospasm 23,25 and it seems that other mechanisms in head injury like mechanical stretching and pulling forces and release of vasoactive substances from damaged parenchyma are also involved in the pathogenesis of post-traumatic vasospasm.4
Few studies have examined CT findings and vasospasm after trauma. In the study by Zubkov et al vasospasm was independently predicted in patients with severe SAH, sub-dural hematoma, and intraventricular hemor rhage on CT scans. Their study primarily included patients with severe head injury.23 In another study by Oertel et al, with enrollment of patients with mild to severe TBI, only SAH was significantly related to the development of vasospasm, although intracerebral hematomas or contusions revealed a trend.22 But, in present study there was no significant relationship between various brain injuries and the occurrence of vasospasm. Also, some studies have showed that patients with vasospasm are significantly younger than those without vasospasm20,22 but, present results did not support this finding. As mentioned above, these different results are probably due to the different patient population, criteria for vasospasm detection, and also limited sample size of present study. The sample size of present study was not enough for analyzing above mentioned associations in patients with severe (n = 11) or moderate to severe (n = 24) TBI. Moreover, in some previous studies, serial TCD has been done to detect vasospasm which was not possible in current investigation. However, the time points for evaluation of vasospasm in present study were according to the peak in the frequency of vasospasm during 3rd to 5th day after the trauma.20 According to some reports,20,21 and also as present results showed, MCA FV after elevation since the third day post-trauma, remained constant for about two weeks. Indeed, the presence of vasospasm did not significantly alter (without treatment) within about two weeks after trauma. Anyway, more investigations are needed to clarify this issue.
Conclusions
In conclusion, traumatic SAH is associated with a high incidence of cerebral vasospasm with a higher probability and severity in patients with more severe TBI. More studies on the predictors and treatments of vasospasm following TBI/tSAH are required.
Authors’ Contributions
BA came up with the idea and supervised the project scientifically. AGh determined the diagnostic methodology, did TCDs, and diagnosed vasospasm. DSh wrote the proposal, managed the project, determined the GCSs, and prepared the draft of the report. HSh and AA helped in finding cases, data gathering, and also preparing the draft of the report. All authors have read, edited, and approved the content of the final manuscript.
Acknowledgments
The authors would like to appreciate the kind assistance and financial support provided by the Vice Chancellor for Research of Isfahan University of Medical Sciences. Also, we are thankful to Dr. Ali Gholamrezaei (Isfahan University of Medical Sciences) who helped us in editing this report.
Footnotes
Conflict of Interests:
Authors have no conflict of interest.
References
- 1.Crowley RW, Medel R, Kassell NF, Dumont AS. New insights into the causes and therapy of cerebral vasospasm following subarachnoid hemorrhage. Drug Discov Today. 2008;13(5-6):254–60. doi: 10.1016/j.drudis.2007.11.010. [DOI] [PubMed] [Google Scholar]
- 2.Mayberg MR, Batjer HH, Dacey R, Diringer M, Haley EC, Heros RC, et al. Guidelines for the management of aneurysmal subarachnoid hemorrhage. A statement for healthcare professionals from a special writing group of the Stroke Council, American Heart Association. Circulation. 1994;90(5):2592–605. doi: 10.1161/01.cir.90.5.2592. [DOI] [PubMed] [Google Scholar]
- 3.Haley EC, Jr, Kassell NF, Torner JC. The international cooperative study on the timing of aneurysm surgery. The North American experience. Stroke. 1992;23(2):205–14. doi: 10.1161/01.str.23.2.205. [DOI] [PubMed] [Google Scholar]
- 4.Zurynski YA, Dorsch NW. A review of cerebral vasospasm. Part IV. Post-traumatic vasospasm. J Clin Neurosci. 1998;146(2):146–54. doi: 10.1016/s0967-5868(98)90028-5. [DOI] [PubMed] [Google Scholar]
- 5.Mattioli C, Beretta L, Gerevini S, Veglia F, Citerio G, Cormio M, et al. Traumatic subarachnoid hemorrhage on the computerized tomography scan obtained at admission: a multicenter assessment of the accuracy of diagnosis and the potential impact on patient outcome. J Neurosurg. 2003;98(1):37–42. doi: 10.3171/jns.2003.98.1.0037. [DOI] [PubMed] [Google Scholar]
- 6.Eisenberg HM, Gary HE, Jr, Aldrich EF, Saydjari C, Turner B, Foulkes MA, et al. Initial CT findings in 753 patients with severe head injury. A report from the NIH Traumatic Coma Data Bank. J Neurosurg. 1990;73(5):688–98. doi: 10.3171/jns.1990.73.5.0688. [DOI] [PubMed] [Google Scholar]
- 7.Kakarieka A, Schakel EH, Fritze J. Clinical experiences with nimodipine in cerebral ischemia. J Neural Transm Suppl. 1994;43:13–21. [PubMed] [Google Scholar]
- 8.Morris GF, Bullock R, Marshall SB, Marmarou A, Maas A, Marshall LF. Failure of the competitive N-methyl-Daspartate antagonist Selfotel (CGS 19755) in the treatment of severe head injury: results of two phase III clinical trials. The Selfotel Investigators. J Neurosurg. 1999;91(5):737–43. doi: 10.3171/jns.1999.91.5.0737. [DOI] [PubMed] [Google Scholar]
- 9.Harders A, Kakarieka A, Braakman R. Traumatic subarachnoid hemorrhage and its treatment with nimodipine.German tSAH Study Group. J Neurosurg. 1996;85(1):82–9. doi: 10.3171/jns.1996.85.1.0082. [DOI] [PubMed] [Google Scholar]
- 10.Martin NA, Doberstein C, Zane C, Caron MJ, Thomas K, Becker DP. Posttraumatic cerebral arterial spasm: transcranial Doppler ultrasound, cerebral blood flow, and angiographic findings. J Neurosurg. 1992;77(4):575–83. doi: 10.3171/jns.1992.77.4.0575. [DOI] [PubMed] [Google Scholar]
- 11.Sander D, Klingelhofer J. Cerebral vasospasm following post-traumatic subarachnoid hemorrhage evaluated by transcranial Doppler ultrasonography. J Neurol Sci. 1993;119(1):1–7. doi: 10.1016/0022-510x(93)90185-2. [DOI] [PubMed] [Google Scholar]
- 12.Aaslid R, Markwalder TM, Nornes H. Noninvasive transcranial Doppler ultrasound recording of flow velocity in basal cerebral arteries. J Neurosurg. 1982;57(6):769–74. doi: 10.3171/jns.1982.57.6.0769. [DOI] [PubMed] [Google Scholar]
- 13.Aaslid R, Huber P, Nornes H. Evaluation of cerebrovascular spasm with transcranial Doppler ultrasound. J Neurosurg. 1984;60(1):37–41. doi: 10.3171/jns.1984.60.1.0037. [DOI] [PubMed] [Google Scholar]
- 14.Lindegaard KF, Nornes H, Bakke SJ, Sorteberg W, Nakstad P. Cerebral vasospasm after subarachnoid haemorrhage investigated by means of transcranial Doppler ultrasound. Acta Neurochir Suppl (Wien) 1988;42:81–4. doi: 10.1007/978-3-7091-8975-7_16. [DOI] [PubMed] [Google Scholar]
- 15.Sviri GE, Newell DW, Lewis DH, Douville C, Ghodke B, Chowdhary M, et al. Impact of basilar artery vasospasm on outcome in patients with severe cerebral vasospasm after aneurysmal subarachnoid hemorrhage. Stroke. 2006;37(11):2738–43. doi: 10.1161/01.STR.0000244765.29502.85. [DOI] [PubMed] [Google Scholar]
- 16.Maas AI, Steyerberg EW, Butcher I, Dammers R, Lu J, Marmarou A, et al. Prognostic value of computerized tomography scan characteristics in traumatic brain injury: results from the IMPACT study. J Neurotrauma. 2007;24(2):303–14. doi: 10.1089/neu.2006.0033. [DOI] [PubMed] [Google Scholar]
- 17.Servadei F, Murray GD, Teasdale GM, Dearden M, Iannotti F, Lapierre F, et al. Traumatic subarachnoid hemorrhage: emographic and clinical study of 750 patients from the European brain injury consortium survey of head injuries. Neurosurgery. 2002;50(2):261–9. doi: 10.1097/00006123-200202000-00006. [DOI] [PubMed] [Google Scholar]
- 18.Abraszko R, Zurynski Y, Dorsch N. The importance of traumatic subarachnoid haemorrhage. J Clin Neurosci. 1996;3(1):21–5. doi: 10.1016/s0967-5868(96)90078-8. [DOI] [PubMed] [Google Scholar]
- 19.Soustiel JF, Bruk B, Shik B, Hadani M, Feinsod M. Transcranial Doppler in vertebrobasilar vasospasm after subarachnoid hemorrhage. Neurosurgery. 1998;43(2):282–93. doi: 10.1097/00006123-199808000-00061. [DOI] [PubMed] [Google Scholar]
- 20.Soustiel JF, Shik V, Feinsod M. Basilar vasospasm following spontaneous and traumatic subarachnoid haemorrhage: clinical implications. Acta Neurochir (Wien) 2002;144(2):137–44. doi: 10.1007/s007010200016. [DOI] [PubMed] [Google Scholar]
- 21.Weber M, Grolimund P, Seiler RW. Evaluation of posttraumatic cerebral blood flow velocities by transcranial Doppler ultrasonography. Neurosurgery. 1990;27(1):106–12. doi: 10.1097/00006123-199007000-00015. [DOI] [PubMed] [Google Scholar]
- 22.Oertel M, Boscardin WJ, Obrist WD, Glenn TC, McArthur DL, Gravori T, et al. Posttraumatic vasospasm: the epidemiology, severity, and time course of an underestimated phenomenon: a prospective study performed in 299 patients. J Neurosurg. 2005;103(5):812–24. doi: 10.3171/jns.2005.103.5.0812. [DOI] [PubMed] [Google Scholar]
- 23.Zubkov AY, Lewis AI, Raila FA, Zhang J, Parent AD. Risk factors for the development of post-traumatic cerebral vasospasm. Surg Neurol. 2000;53(2):126–30. doi: 10.1016/s0090-3019(99)00178-0. [DOI] [PubMed] [Google Scholar]
- 24.Taneda M, Kataoka K, Akai F, Asai T, Sakata I. Traumatic subarachnoid hemorrhage as a predictable indicator of delayed ischemic symptoms. J Neurosurg. 1996;84(5):762–8. doi: 10.3171/jns.1996.84.5.0762. [DOI] [PubMed] [Google Scholar]
- 25.Vajramani GV, Chandramouli BA, Jayakumar PN, Kolluri S. Evaluation of posttraumatic vasospasm, hyperaemia, and autoregulation by transcranial colour-coded duplex sonography. Br J Neurosurg. 1999;13(5):468–73. [PubMed] [Google Scholar]


