Abstract
BACKGROUND:
Dairy products intolerance is defined by existing of gastrointestinal symptoms following dairy product consumption. Its prevalence varies among different countries. This study is conducted to determine the frequencies and severities of intolerance symptoms in the consumption of different dairy products in Iranian students of Medical Sciences.
METHODS:
In this cross-sectional study, 1041 students from Isfahan University of Medical Sciences who apparently were healthy and had not used any drug before, participated.
The questionnaire included information about dairy product consumption and avoidance, severity of dairy intolerance symptoms included gas passing, flatulence, diarrhea and abdominal pain and coexistence of irritable bowel syndrome (IBS)
RESULTS:
The frequencies of dairy intolerance syndromes in milk, yoghurt, cheese and ice cream consumption were 51.1% (532), 16.6% (173), 11.7% (122) and 13.4% (140), respectively. Most severe symptoms for milk, yoghurt, cheese and ice cream intolerance were diarrhea (2.11 ± 0.08), gas passing (1.56 ± 0.09) and flatulence (1.49 ± 0.09), respectively. Fifty (9.4%) of symptomatic respondents never drank milk. Correlation coefficient between symptoms severity and the avoidance of consumption in milk intolerance was 0.38.
CONCLUSIONS:
Students tolerate other dairy products better in comparison with milk. In the present study, the phenomenon as irritable bowel syndrome was not strongly associated with the severity of all symptoms in dairy intolerant persons. Also, there were weak association between the severity of symptoms with dairy consumption and avoidance, but more studies are needed to evaluate calcium absorption and osteoporosis in symptomatic cases.
Keywords: Dairy Intolerance Symptoms, Irritable Bowel Syndrome, Iran, Symptom Severity
Dairy intolerance syndrome is defined by existing of gastrointestinal symptoms following dairy product consumption. There are many reasons for milk and dairy products intolerance syndrome. The most important of them are cow milk intolerance, cow milk allergy, lactose intolerance and lactase deficiency.
The prevalence of allergy to milk and milk proteins intolerance is about 2% to 15%. It is because of the inability to digest the milk proteins. The clinical signs of those are the same, but the immunological reactions are different.1
Lactase deficiency and lactose intolerance are the most prevalent causes of milk and dairy products intolerance.2 Dairy intolerance syndrome is composed of one or a group of symptoms together like stomachache, diarrhea, increase in gas passing and flatulence.3 It can be diagnosed by taking a good look at the medical history; the symptoms could be disappeared with a two week trial of lactose-free diet and they would recurrence after consumption of dairy products.3
The most important cause of lactose intolerance is primary lactase deficiency and can be stated that about 70% of the world adult population is lactase intolerant. The percentage varies according to ethnicity and is related to the amount of dairy products in the diet and genetic structure of ability to digest lactose in individuals.4,5 In the North European population in which consumption of dairy products in the diet is prominent, about 2% of the population has primary lactase deficiency. In contrast, about 50% to 80% of Spanish people, 60% to 80% of the black people, 100% of Asians and the Indians residing in the United States have this problem.6–8 The prevalence rate of milk intolerance according to subjective gastrointestinal symptoms has been reported 28.4% in Southern Iranian population who are older than 35 years.9 Another study objectively (on the basis of the low rise in blood glucose levels) found that 68% of Iranian cases who are younger than 25 years had lactose intolerance. Only 39% reported clinical symptoms related to lactose malabsorption.10
Milk and other dairy products intolerance cause gastrointestinal symptoms which are similar to those in irritable bowel syndrome (IBS). Both conditions are common, but it is contrasting to show a causative role between these two complaints.9,11
Above explanation shows the high prevalence of milk and dairy products intolerance syndrome in the world, especially in Asia. Since this may lead to avoidance of milk and dairy products consumption and less ingest of main minerals and protein intake, it may cause a major impact on public health. In spite of this fact, there is a few data available about the syndrome in Middle East and Iran and little has been published about the young adults, especially those who are studying in medical sciences university. Thus, these data can yield important information regarding development of interventional strategies to manage and optimize dairy consumption as a main source of calcium in young adults.
This study tried to assess the prevalence and severity of symptoms of dairy intolerance syndrome in Iranian students of Medical Sciences and also the relationship between the severities of symptoms with other factors including avoidance of using dairy products and the symptoms of irritable bowel syndrome.
Methods
This cross sectional study was done among the students of Isfahan University of Medical Sciences who are older than 18 years old. Samples were selected by convenience sampling method. They had not taken antibiotics or any other drugs especially laxatives, sorbitol or GI irritant at least three weeks before and did not have any diagnosed disease like celiac, intestinal parasites, cancer or systemic diseases including diabetes or renal function disorders. A self-report questionnaire was designed in the following domains:
A six-scaled question was used to assess the amount of milk and yoghurt consumption in the form of the numbers of milk glasses or yoghurt bowls in a week or on a day. Ordinal items related to this scale were consisting of: “almost never”, “1 to 3 times a month”, “1 to 3 times a week”, “4 to 7 times a week”, “2 times a day” and “more than 2 times a day”.
The severity of symptoms due to milk, yoghurt, ice cream and cheese consumption was assessed using a five-point question; with the score of 1 (mild symptoms) to 5 (sever symptoms). Symptoms included diarrhea, flatulence and bloating, increase in gas passing, stomachache and symptoms like headache, fatigue and calf senselessness.
The respondents were asked to answer the ordinal items related to avoidance of dairy products consumption due to somatic symptoms as follow: “seldom”, “sometimes”, “most of the times ”and “always ”.
Questions about irritable bowel syndrome (including the items of ROMEII criteria) 12 should have been answered by “yes” or “no”.
The pilot testing was done on fifty students to evaluate face validity of the tool. Finally, specialists and nutritionists approved the content and face validity of this tool. The study was accepted by Ethical Committee of Isfahan University of Medical Sciences.
The questionnaires were distributed by a trained team at the end of classes in different faculties. They explained the research project in each class and collected the questionnaires after 20 minutes. The final samples were composed of 1041 completed surveys. The study was undertaken for a period of 8 months, from May 2006 to December 2006.
In this study, dairy intolerance syndrome means to have at least one of these symptoms including flatulence and bloating, diarrhea, stomachache and increase in gas passing after consumption of different dairy products.6
Data were compiled and statistically analyzed with SPSS software (version 15.0). Mean ± SE was calculated to reveal the severity of symptoms. Cross-tabulation was used to determine the percentage of dairy intolerance syndrome and somatic symptoms in the symptomatic and total population. Mean symptom severity of dairy intolerance syndrome was created by adding up the scores of severity related to these four gastrointestinal symptoms and then dividing it into the number of existing symptoms. Spearman correlation was used to determine whether the severity of symptoms is associated with avoidance and amount of consumption as well as irritable bowel syndrome. Association between symptom severities for different kinds of dairy products was analyzed by Pearson correlation. P value of < 0.05 was considered significance throughout the study.
Results
Frequency and severity of somatic symptoms in milk consumers were more than other dairy products. Flatulence and bloating (36.5%) and stomachache (32.9%) had the highest ranks. Severe symptoms in yoghurt, cheese and ice cream consumers were fatigue (35.4%), flatulence (10%) and stomachache (10.2%), respectively (Table 1).
Table 1.
Frequencies and mean severities of seven somatic symptoms (n = 1041)
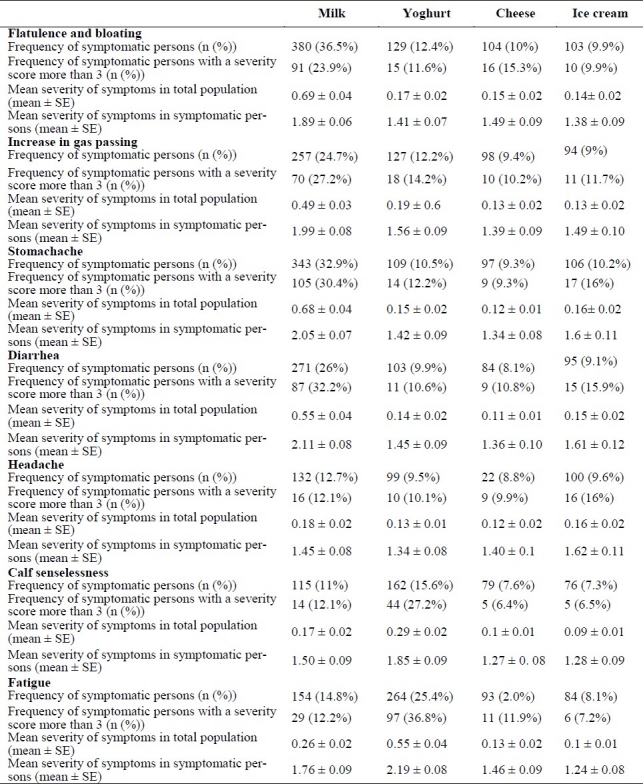
Having at least one of the seven somatic symptoms after milk, yoghurt, cheese and ice cream consumption had percentages of 53% (556), 32% ( 332), 14% (145) and 16% (165), respectively. Common somatic symptoms in dairy consumption differed in symptomatic students compared to the total population. Diarrhea (2.11 ± 0.08), fatigue (2.19 ± 0.08), headache (1.62 ± 0.11) and flatulence and bloating (1.49 ± 0.09) were the most common symptoms in the consumers of milk, yoghurt, ice cream and cheese (Table 1).
Table 2 shows the frequencies and severities of symptoms in subjects who had dairy intolerance syndrome. It was 532 (51.1%) in milk consumption compared to 173 (16.6%), 122 (11.7%) and 140 (13.4%) in ingestion of yoghurt, cheese and ice cream, respectively. The highest mean score of severity among all symptoms was seen in milk intolerance syndrome (1.91 ± 0.04) and then in ice cream (1.58 ± 0.08).
Table 2.
Mean severity of symptoms and percentage of avoiding dairy products in dairy intolerant respondents
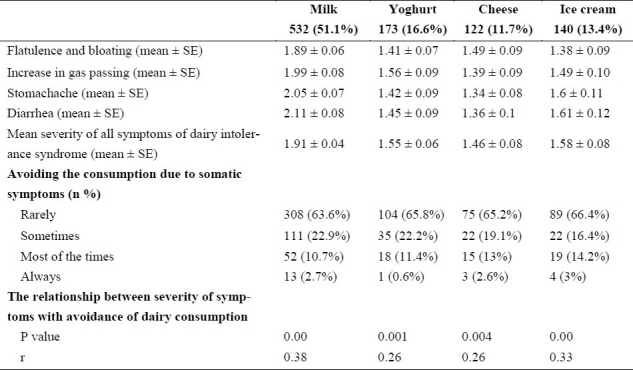
Three percent (3%) of ice cream intolerant persons stated to avoid it always due to somatic symptoms, while these were 2.7% for milk, 2.6% for cheese and only 0.6% stated permanent avoidance of yoghurt.
Severity of symptoms seemed to have significant association with avoidance of dairy products especially in milk(r = 0.38) and ice cream(r = 0.33) consumption (Table 2).
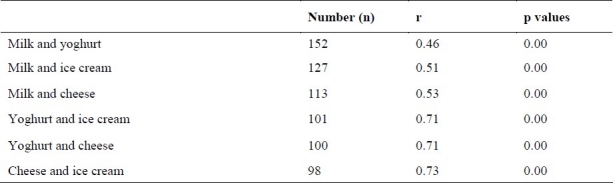
Symptoms of dairy intolerant persons were likely to have significant correlation in different kinds of dairy products. This association was notable in yoghurt, cheese and ice cream consumption, but it was less in milk consumption (Table 3).
Table 3.
Relation between severity of symptoms in dairy intolerant persons among different kinds of dairy products
The percentages of the amounts of milk and yoghurt consumption in the total population and milk intolerant persons are shown in table 4. Fifty (9.4%) of milk intolerant persons never drank milk. In addition, only 30.7% of respondents stated that they used milk once or more in a day. This rate was 27.2% in milk intolerant persons. Meanwhile, daily or more yoghurt consumptions in total population and milk intolerant ones were 56.1% and 54.4%, respectively.
Table 4.
Milk and yoghurt consumption in total population and in those with milk intolerance syndrome
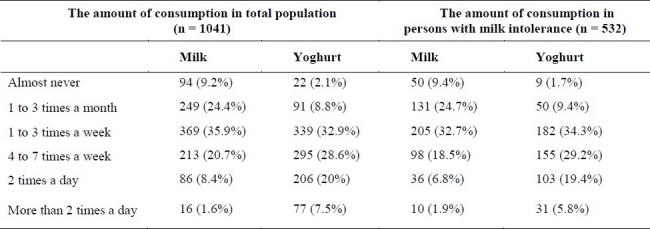
There was a reverse significant association between the amounts of milk consumption and the severity of symptoms like stomachache (r = -0.28), flatulence (r = -0.2), diarrhea (r = -0.17) as well as the whole symptoms (r = -0.19). No relationship was found between the amount of milk and yoghurt consumption and other symptoms in milk intolerant persons (p > 0.05).
Two hundred eighty persons (29.8 %, missing: 100, n = 941) stated that having an abdominal pain is relieved with stool passage and usually associated with a change in stool frequency and consistency with the onset of pain (i.e. IBS symptoms). In the present study, a significant association between irritable bowel syndrome and the severity of all symptoms in respondents with milk (r = -0.2) and ice cream (r = 0.17) intolerance syndrome was found. None of other dairy products correlated significantly with this complaint (p > 0.05).
The mean number of defecations per week was 8.18 ± 5.2 (n = 773) among the samples. No significant relationship was found between the number of defecations per week and severity of symptoms after different dairy product consumption (p > 0.05).
Discussion
Dairy intolerance syndrome is clinically defined as stomachache, flatulence and bloating, diarrhea and increase in gas passing induced by different dairy consumption.6 According to this study, 51.1% of our population had milk intolerance syndrome. Dairy intolerance syndrome was less than 20% for yoghurt, ice cream and cheese (as the highest to the lowest frequencies).
Dairy intolerance syndrome can cause other gut related symptoms like nausea, vomiting and constipation 13 as well as a range of systemic symptoms including muscle and joint pain, headache and lightheadedness, fatigue and loss of concentration.14 The prevalence of any of the above symptoms vary from 20% to 100%.6 The present study shows that the severities of flatulence and bloating, stomachache and diarrhea were more than other symptoms in milk consumers. Meanwhile, in yoghurt consumers, fatigue and calf senselessness were the prominent symptoms. Diarrhea, stomachache and headache were the most severe symptoms in ice cream consumers, but flatulence and bloating, excess gas and fatigue were prominent in cheese consumers. These results showed dairy consumption may cause the notable non-gastrointestinal symptoms, which can lead to dairy products abstinence.
The severities of symptoms in milk and ice cream consumers were more than other dairy products in those who had dairy intolerance syndrome. This may be due to unprocessed nature of these two products.
Dairy intolerance syndrome is not only caused by lactose maldigestion and hypolactasia, although the majority of cases do have one of these.2 The term dairy intolerance is used precisely by referring to the subjective symptoms, but lactose maldigestion is diagnosed definitely by different objective tests.
In a study in Iran, one hundred five Iranian cases, ranging in age from 4 months to 25 years old, were tested for lactose malabsorption. It has been reported that lactose maldigestion as evidenced by a small increase in the blood glucose (20mg/100ml) after an oral dose (2g/kg) of lactose were 68% among Iranian population. Only Thirty nine percent (39%) show clinical symptoms that are ordinarily associated with lactose intolerance.10 A survey on Iranian population who are older than 35 years showed that 28.4% of them had milk intolerance syndrome. It had been diagnosed by reporting gastrointestinal symptoms after milk ingestion.9 In a Malaysian study, after the consumption of lactose (50g), hypolactasia was diagnosed by two tests: the assessment of urinary galactose excretion and the calculation of galactose/creatinine ratio. Prevalence of hypolactasia in the three ethnics of Malays, Chinese and Indians respectively found to be 88% and 83%, 91% and 73%, 83% and 73% according to these two tests. Flatulence, stomachache and diarrhea were the prominent symptoms in these three groups, but stomachache was less common in Indians and it was attributed to the high threshold of pain and great consumption of milk in that society. The percentages of dairy intolerance syndrome were found to be 71% in Malays, 65% in Chinese and 53% in Indians based on somatic symptoms.15 In a study in China, 1168 healthy subjects between 3 and 13 years were recruited to assess hypolactasia by the expiratory H2 concentration after using lactose (25g/200mg) and milk (200cc + 14 gr of lactose + 50 gr of milk powder). The prevalence of hypolactasia was found to be 87% in both 7-8 year and 11-13 year old groups. Based on somatic symptoms, the prevalence of milk intolerance syndrome was 30% and 33% in these age groups. The children complained of excess gas, blooming, stomachache and flatulence (most to least frequently) after four hours under strict supervision.16 The prevalence of hypolactasia in European adults has been reported 4% in Denmark 4 and 50% in Italy,17 but its prevalence is more in Asian countries, so that it is 60% in Pakistan,18 98% in Thailand 19 and11% to 90% in Russia.20 It varies from 15% in the white population of American countries to 80% in the black population and 53% in Mexican-Americans.21 Therefore, this prevalence (51.1%) can be compared to other regions especially in Asian and Iranian ones.
To relieve the symptoms related to dairy intolerance, new methods have been suggested like using yoghurt and other dairy products containing bacteria with lactase 22,23 and also pharmaceutical 24,25 and non pharmaceutical26,27 treatments which delay the gastric emptying and intestinal transit time to expose lactose with intestinal lactase.
Symptoms of dairy maldigesters seemed strongly to be related in fermented dairy products (r ≥ 0.7) and there were weak association between symptoms induced by milk and these products, especially yoghurt (r = 0.46). In addition, fermented dairy products cause fewer symptoms and lactase non-persistent persons digest and tolerate them better than milk. After primary screening which was was done to select the Lactose malabsorbed (LM) subjects using the H2 breath test, an equivalent amount of lactose contained in yoghurt and fermented-then-pasteurized milk (FPM) was consumed by LM subjects. Breathing H2 excretion was significantly higher after ingestion of milk than after yoghurt consumption.28 However, several works emphasized that lactose ingestion was improved and symptoms were significantly reduced after consuming yoghurt compared to milk.29,30
In the present study, the irritable bowel syndrome was not strongly associated with the severity of all symptoms in dairy intolerant persons. In a Norwegian study, lactose malabsorption (LM) was not significantly higher in subjects with IBS compared to healthy volunteers and the results finally concluded that IBS and LM are unrelated disorders.31 Several other studies 32,33 showed similar findings which is comparable to the present survey. In contrast, some other studies found that lactose intolerance was more common among IBS subjects than healthy ones.9,34
In this study, permanent avoidance of using dairy products was seen more in ice cream (3%) and milk (2.7%). There was also a significant association between the severity of symptoms and avoidance of consumption especially in these ones. In addition, only, about one-third of respondents had at least daily milk consumption and less was seen in symptomatic cases. In contrast, more than 50% 0f older Americans reported that they had consumed milk at least 2 times per day during adolescence.35 These findings call for poor condition of milk intake and dietary restriction in this young population as well as intolerant persons which could cause harm to health. Recent studies indicate avoidance of milk consumption due to somatic symptoms can lead to inadequate calcium intake.4,36,37 In a study among Italian postmenopausal women, both bone mineral density and calcium intake were significantly lower in women with milk intolerance symptoms and also calcium intake was correlated inversely with the symptom score and positively with bone mineralization.4
Amounts of milk consumption had an inverse and low association with the severity of some symptoms. It has been reported that continued and divided milk ingestion reduces gastrointestinal symptoms, which has been due to a change in colonic flora and adaptation to milk consumption.3,13 But this weak association cannot confirm adaptation phenomenon.
According to the present study, the prevalence of milk intolerance syndrome in university students of 18-26 years old was about 51% and it was less than milk for other dairy products.
The severity of symptoms in milk consumers was more than other dairy products consumers. There was a strong correspondence between the symptoms of yoghurt, ice cream and cheese consumers suggesting the better tolerance of these products compared to milk consumption. There was a little relationship between the severity of symptoms and avoidance of dairy products. But, other researches showed avoidance of milk ingestion results in a decline in calcium intake. However, it was reported that adaptation can reduce the severity of symptoms, but weak association was seen between the severity of symptoms and the amount of milk consumption.
Conclusions
Using the self-reported questionnaire to assess symptoms of dairy intolerance syndrome and samples limited to the students of medical sciences are some pitfalls in this study. Using appropriate tests like hydrogen excretion and urine galactose as well as recruiting different age groups to determine exactly lactase deficiency and dairy intolerance syndrome are suggested to be considered in other works.
Dairy products are calcium resources that play an important role in daily diet. So, because of a high prevalence (50%) of dairy intolerance syndrome in Iranian young and educated samples as well as few milk ingestion and high prevalence of osteoporosis in Iranian people,38 more researches are needed to assess the association between this syndrome, avoidance of dairy consumption and calcium intake in the future.
Authors’ Contributions
The main idea was presented by PA. He also designed the study, supervised data collection, designed data analysis and helped in writing the article. PM designed the study, collected data and helped in writing the article. AS analyzed data and helped in writing the article. All authors have read and approved the content of final manuscript.
Footnotes
Conflict of Interests:
Authors have no conflict of interests.
References
- 1.Ewing WM, Allen PJ. The diagnosis and management of cow milk protein intolerance in the primary care setting. Pediatr Nurs. 2005;31(6):486–93. [PubMed] [Google Scholar]
- 2.Assa’ad AH. Gastrointestinal food allergy and intolerance. Pediatr Ann. 2006;35(10):718–26. doi: 10.3928/0090-4481-20061001-07. [DOI] [PubMed] [Google Scholar]
- 3.Heyman MB. Committee on Nutrition. Lactose intolerance in infants, children, and adolescents. Pediatrics. 2006;118(3):1279–86. doi: 10.1542/peds.2006-1721. [DOI] [PubMed] [Google Scholar]
- 4.Jackson KA, Savaiano DA. Lactose maldigestion, calcium intake and osteoporosis in African-, Asian-, and Hispanic-Americans. J Am Coll Nutr. 2001;20(2 Suppl):198S–207S. doi: 10.1080/07315724.2001.10719032. [DOI] [PubMed] [Google Scholar]
- 5.Srinivasan R, Minocha A. When to suspect lactose intolerance. Symptomatic, ethnic, and laboratory clues. (115-6, 122-3).Postgrad Med. 1998;104(3):109–11. doi: 10.3810/pgm.1998.09.577. [DOI] [PubMed] [Google Scholar]
- 6.Matthews SB, Waud JP, Roberts AG, Campbell AK. Systemic lactose intolerance: a new perspective on an old problem. Postgrad Med J. 2005;81(953):167–73. doi: 10.1136/pgmj.2004.025551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lloyd ML, Olsen WA. Disaccharide malabsorption. In: Haubrich WS, Schaffner F, Berk JE, editors. Bockus gastroenterology. 5th ed. Philadelphia: Saunders; 1995. pp. 1087–100. [Google Scholar]
- 8.Sahi T. Genetics and epidemiology of adult-type hypolactasia. Scand J Gastroenterol Suppl. 1994;202:7–20. doi: 10.3109/00365529409091740. [DOI] [PubMed] [Google Scholar]
- 9.Saberi-Firoozi M, Khademolhosseini F, Mehrabani D, Yousefi M, Salehi M, Heidary ST. Subjective lactose intolerance in apparently healthy adults in southern Iran: is it related to irritable bowel syndrome? Indian J Med Sci. 2007;61(11):591–7. [PubMed] [Google Scholar]
- 10.Sadre M, Karbasi K. Lactose intolerance in Iran. Am J Clin Nutr. 1979;32:1948–54. doi: 10.1093/ajcn/32.9.1948. [DOI] [PubMed] [Google Scholar]
- 11.Turnbull GK. Lactose intolerance and irritable bowel syndrome. Nutrition: The International Journal of Applied and Basic Nutritional Sciences. 2000;16(7):665–6. doi: 10.1016/s0899-9007(00)00339-7. [DOI] [PubMed] [Google Scholar]
- 12.Thompson WG, Longstreth GF, Drossman DA, Heaton KW, Irvine EJ, Müller-Lissner SA. Functional bowel disorders and functional abdominal pain. Gut. 1999;45(2 Suppl):II43–7. doi: 10.1136/gut.45.2008.ii43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jarvis JK, Miller GD. Overcoming the barrier of lactose intolerance to reduce health disparities. J Natl Med Assoc. 2002;94(2):55–66. [PMC free article] [PubMed] [Google Scholar]
- 14.Matthews SB, Campbell AK. Lactose intolerance and neuromuscular symptoms. The Lancet. 2000;356(9228):511. doi: 10.1016/S0140-6736(05)74183-0. [DOI] [PubMed] [Google Scholar]
- 15.Asmawi MZ, Seppo L, Vapaatalo H, Korpela R. Hypolactasia and lactose intolerance among three ethnic groups in Malaysia. Indian J Med Res. 2006;124(6):697–704. [PubMed] [Google Scholar]
- 16.Yang Y, He M, Cui H, Bian L, Wang Z. The prevalence of lactase deficiency and lactose intolerance in Chinese children of different ages. Chin Med J (Engl) 2000;113(12):1129–32. [PubMed] [Google Scholar]
- 17.Grant JD, Bezerra JA, Thompson SH, Lemen RJ, Koldovsky O, Udall JN., Jr Assessment of lactose absorption by measurement of urinary galactose. Gastroenterology. 1989;97(4):895–9. doi: 10.1016/0016-5085(89)91494-7. [DOI] [PubMed] [Google Scholar]
- 18.Miller MD, Ferris DG. Measurement of subjective phenomena in primary care research: the Visual Analogue Scale. Fam Pract Res. 1993;13(1):15–24. [PubMed] [Google Scholar]
- 19.Vesa TH, Korpela RA, Sahi T. Tolerance to small amounts of lactose in lactose maldigesters. Am J Clin Nutr. 1996;64(2):197–201. doi: 10.1093/ajcn/64.2.197. [DOI] [PubMed] [Google Scholar]
- 20.Khabarova YA, Torniainen ST, Nurmi HA, Järvelä IE, Isokoski MK, Mattila KJ. Prevalence of lactase persistent/non-persistent genotypes and milk consumption in a young population in north-west Russia. World J Gastroenterol. 2009;15(15):1849–53. doi: 10.3748/wjg.15.1849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Vesa TH, Marteau P, Korpela R. Lactose intolerance. J Am Coll Nutr. 2000;19(2 Suppl):165S–75S. doi: 10.1080/07315724.2000.10718086. [DOI] [PubMed] [Google Scholar]
- 22.Adolfsson O, Meydani SN, Russell RM. Yoghurt and gut function. Am J Clin Nutr. 2004;80(2):245–56. doi: 10.1093/ajcn/80.2.245. [DOI] [PubMed] [Google Scholar]
- 23.Hove H, Norgaard H, Mortensen PB. Lactic acid bacteria and the human gastrointestinal tract. Eur J Clin Nutr. 1999;53(5):339–50. doi: 10.1038/sj.ejcn.1600773. [DOI] [PubMed] [Google Scholar]
- 24.Peuhkuri K, Vapaatalo H, Nevala R, Korpela R. Influence of the pharmacological modification of gastric emptying on lactose digestion and gastrointestinal symptoms. Aliment Pharmacol Ther. 1999;13(1):81–6. doi: 10.1046/j.1365-2036.1999.00450.x. [DOI] [PubMed] [Google Scholar]
- 25.Szilagyi A, Salomon R, Seidman E. Influence of loperamide on lactose handling and oral-caecal transit time. Aliment Pharmacol Ther. 1996;10(5):765–70. doi: 10.1046/j.1365-2036.1996.45187000.x. [DOI] [PubMed] [Google Scholar]
- 26.McCray S. Nutritional support in gastroenterology, series #2. Lactose intolerance: considerations for the clinician. (24, 28, 31, 36, 38-9).Practical Gasteroenterology. 2003;XXVII(2):21–2. [Google Scholar]
- 27.Moore BJ. Dairy foods: are they politically correct? Nutr Today. 2003;38(3):82–90. [PubMed] [Google Scholar]
- 28.Varela-Moreiras G, Antoine JM, Ruiz-Roso B, Varela G. Effects of yoghurt and fermented-then-pasteurized milk on lactose absorption in an institutionalized elderly group. J Am Coll Nutr. 1992;11(2):168–71. [PubMed] [Google Scholar]
- 29.He T, Priebe MG, Zhong Y, Huang C, Harmsen HJM, Raangs GC, et al. Effects of yogurt and bifidobacteria supplementation on the colonic microbiota in lactose-intolerant subjects. J Appl Microbiol. 2008;104(2):595–604. doi: 10.1111/j.1365-2672.2007.03579.x. [DOI] [PubMed] [Google Scholar]
- 30.Rosado JL, Solomons NW, Allen LH. Lactose digestion from unmodified, low-fat and lactose-hydrolyzed yoghurt in lactose maldigesters. Eur J Clin Nutr. 1992;46(1):61–7. [PubMed] [Google Scholar]
- 31.Farup PG, Monsbakken KW, Vandvik PO. Lactose malabsorption in a population with irritable bowel syndrome: prevalence and symptoms.A case-control study. Scand J Gastroenterol. 2004;39(7):645–9. doi: 10.1080/00365520410005405. [DOI] [PubMed] [Google Scholar]
- 32.Vernia P, Marinaro V, Argnani F, Di Camillo M, Caprilli R. Self-reported milk intolerance in irritable bowel syndrome: what should we believe? Clin Nutr. 2004;23(5):996–1000. doi: 10.1016/j.clnu.2003.12.005. [DOI] [PubMed] [Google Scholar]
- 33.Vernia P, Ricciardi MR, Frandina C, Bilotta T, Frieri G. Lactose malabsorption and irritable bowel syndrome. Effect of a long-term lactose-free diet. Ital J Gastroenterol. 1995;27(3):117–21. [PubMed] [Google Scholar]
- 34.Bohmer CJ, Tuynman HA. The clinical relevance of lactose malabsorption in irritable bowel syndrome. Eur J Gastroenterol Hepatol. 1996;8(10):1013–6. doi: 10.1097/00042737-199610000-00015. [DOI] [PubMed] [Google Scholar]
- 35.Elbon SM, Johnson MA, Fischer JG. Milk consumption in older Americans. Am J Public Health. 1998;88(8):1221–4. doi: 10.2105/ajph.88.8.1221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Callegari C, Lami F, Levantesi F, Andreacchio AM, Tatali M, Miglioli M, et al. Post-menopausal bone density, lactase deficiency and milk consumption. J Hum Nutr Diet. 1990;3(3):159–64. [Google Scholar]
- 37.Corazza GR, Benati G, Di Sario A, Tarozzi C, Strocchi A, Passeri M, et al. Lactose intolerance and bone mass in postmenopausal Italian women. Br J Nutr. 1995;73(3):479–87. doi: 10.1079/bjn19950050. [DOI] [PubMed] [Google Scholar]
- 38.Hejazi J, Mohtadinia J, Kolahi S, Ebrahimi-Mamaghani M. Nutritional status among postmenopausal osteoporotic women in North West of Iran. Asia Pac J Clin Nutr. 2009;18(1):48–53. [PubMed] [Google Scholar]


