Abstract
Introduction:
Psychosocial stress and impulsivity are each associated with smoking in adolescents. There is also evidence that stress can increase impulsive responding, and impulsive adolescent smokers attempting cessation are at greater risk of relapse. We performed a pilot investigation to examine stress-induced changes in response inhibition, inattention, and risk taking asrelated to smoking status and posttreatment smoking abstinence.
Methods:
Twelve adolescent smokers participating in a smoking cessation intervention and 15 adolescent nonsmokers completed a 2-session protocol assessing stress-related change in response inhibition and inattention (on the Conners’ Continuous Performance Test-II), risk taking (on the Balloon Analogue Risk Task), nicotine withdrawal symptoms, and self-reported stress.
Results:
At baseline, smokers had greater inattentive responding and risk taking when compared with nonsmokers. Stress exposure led to significant increases in stress, anger, and depression in all participants and also increased nicotine craving (on the Minnesota Nicotine Withdrawal Scale item) and impulsive responding in smokers. After covarying for baseline differences in impulsivity/risk taking, smokers who were not abstinent at the end of treatment experienced greater stress-induced risk taking when compared with those who were abstinent.
Conclusions:
In all, it appears that response inhibition and risk taking may be differentially altered by stress exposure in adolescent smokers and nonsmokers and that adolescent smoking cessation success may be associated with less risk taking in the face of stress.
Introduction
Despite declines, roughly one in nine adolescents was a daily tobacco smoker in 2008 (Johnston, O’Malley, Bachman, & Schulenberg, 2009). Adolescent smoking is associated with negative health effects (Department of Health and Human Services, 1994), other substance use (Lewinsohn, Rohde, & Brown, 1999), and psychiatric illness (Brown, Lewinsohn, Seeley, & Wagner, 1996). The majority of adolescent smokers want to quit smoking (Burt & Peterson, 1998), but the natural rates of cessation are often below 10% (e.g., Zhu, Sun, Billings, Choi, & Malarcher, 1999). While treatment improves cessation rates, these are usually still below 20% (Schepis & Rao, 2008). These data indicate the need for more effective adolescent cessation interventions. One way to improve treatment effectiveness could be to identify psychological constructs or situations that impede cessation.
Inattention (i.e., failure to sustain attention or vigilance), response inhibition (i.e., failure to prevent inappropriate responses), and risk taking (i.e., behavior with the potential for either harm or reward; Leigh, 1999) may be such factors. Among adolescents, smokers appear to have higher levels of inattention and risk taking and poorer response inhibition than nonsmokers (e.g., Fields, Collins, Leraas, & Reynolds, 2009; Lejuez et al., 2003; Reynolds et al., 2007). Furthermore, adolescent smokers with poorer response inhibition are less likely to achieve abstinence (Krishnan-Sarin et al., 2007), perhaps due to a heightened sensitivity to factors that prompt relapse. Stress may be one such factor. Nicotine abstinence appears to elevate stress levels (Parrott & Kaye, 1999), and stress levels have been linked back to relapse (McKee, Maciejewski, Falba, & Mazure, 2003). Furthermore, stress appears to decrease response inhibition (Swann, 2003; Tonissaar et al., 2008); stress also affects risk taking and inattention but in less straightforward ways (Porcelli & Delgado, 2009; van der Oord, Prins, Oosterlaan, & Emmelkamp, 2006).
To date, no studies have prospectively examined the roles of inattention, response inhibition, or risk taking on the relationship between stress and adolescent smoking. This study was a pilot examination of these relationships using a validated personalized stress imagery technique (Sinha, 2009). Participating adolescent smokers also entered a smoking cessation trial following completion of the stress induction paradigm, allowing for linking of data to cessation outcome. Finally, nonsmokers were included to test whether smoking status influenced stress-related inattention, response inhibition, and risk taking. We hypothesized that, following stress exposure, smokers would have more inattentive and response inhibition errors and take greater risks than nonsmokers. We also expected that smokers who were not abstinent at the end of the cessation trial would have greater stress-related increases in inattention, response inhibition, and risk taking.
Methods
Participants
Participants were high-school students taking part in a 4-week smoking cessation trial (Cavallo et al., 2007; Krishnan-Sarin et al., 2006). Smokers were eligible if they smoked ≥5 cigarettes daily and had urine cotinine levels ≥350 ng/ml (Graham Massey Analytical Labs). Nonsmokers denied smoking in the past six months, smoked ≤5 cigarettes lifetime, and had urine cotinine levels ≤30 ng/ml.
Fifteen nonsmokers (8 male and 7 female) and 12 smokers (9 male and 3 female) were included in analyses. One female smoker was excluded because of an adverse reaction to the stress induction. Smokers (17.2 ± 0.84) were older than nonsmokers (15.7 ± 1.10; p = .001), with no gender differences by smoking status. Abstinence among smokers was determined at the end of four weeks of treatment and defined as 7-day self-report confirmed by urine cotinine <100 ng/ml; 5 of 12 smokers were abstinent. Abstinent smokers were slightly older (17.4 ± 0.55; 4 males and 1 female) than nonabstinent smokers (17.0 ± 1.00), but no significant differences were observed in age or gender by cessation outcome.
Measures
NicAlert Semi-quantitative Cotinine Immunoassay Strips (Craig Medical) confirmed smoking status and are a reliable and valid measure of recent smoking in adolescents (Schepis et al., 2008).
Stress Visual Analogue Scale (VAS) assessed stress levels throughout the stress induction session. Participants reported their stress level by placing a mark on a 100-cm line with anchors ranging from “no sensation” to “strongest imaginable stress level of any kind.”
Minnesota Nicotine Withdrawal Scale (MNWS; Hughes & Hatsukami, 1986) assessed symptoms of nicotine withdrawal, including craving and negative affect (e.g., depression, anxiety and anger, frustration or irritability). It has adequate to good internal consistency (Toll, O’Malley, McKee, Salovey, & Krishnan-Sarin, 2007).
Conners’ Continuous Performance Test-II (CPT-II; Conners, 2000) assessed inattention (omission errors or failure to respond to target stimuli) and response inhibition (commission errors or response to infrequent nontarget stimuli). The CPT-II produces T-scores that are normed for age and gender; it is free from practice effects and appears to be reliable and valid (Conners, 2000).
Balloon Analogue Risk Task (BART; Lejuez et al., 2002) assessed risk taking as the mean number of pumps on balloon trials that do not burst (adjusted pumps), which is the most common outcome measure (e.g., White, Lejuez, & de Wit, 2008). The BART appears to be reliable and valid (Lejuez et al., 2003; White et al., 2008). Participants were not paid for their performance on the BART.
Procedures
Adolescents who expressed an interest in participation were screened for inclusion over the telephone. Eligible smokers, through participation in the cessation trial, signed assent/consent prior to participation; passive parental permission procedures were used (Krishnan-Sarin et al., 2006). Eligible nonsmokers and a parent/guardian met with study staff and signed consent or assent/permission forms prior to participation.
Baseline CPT-II and BART performance were obtained from smokers at an assessment visit. In that or a separate session, smokers participated in script development for the stress imagery paradigm. Nonsmokers completed the baseline CPT-II and BART trials and script development at a screening session. Two scripts were solicited from each participant: (a) one of the most stressful events they had experienced in the past year, and (b) a situation that they found relaxing. To avoid the confounding effects of tobacco use imagery, scripts did not involve tobacco use (Sinha, 2009; Sinha, Catapano, & O’Malley, 1999; Sinha et al., 2003).
All participants took part in a second (stress induction) session. First, they completed the VAS and MNWS and then listened to audiotapes describing their stressful experience. At the beginning of all tapes, participants were instructed to “Close your eyes and imagine the situation as if it is happening right now.” Participants then completed the VAS, MNWS, BART, and CPT-II and a VAS after CPT-II completion. Finally, participants listened to their relaxing script and completed a final VAS. All scripts were recorded by the same female research assistant, and each lasted 5 min (4:30 for the situation and 30 s for continued visualization).
After completion of the stress induction, smokers participated in the 4-week CM/CBT cessation protocol. Prior to quit day, all participants took part in a skill-building “Prep-to-Quit” session. Participants set a quit day within the next week at which point treatment began. All procedures were approved by the Human Investigation Committee of Yale University School of Medicine.
Data Analyses
Analysis of intervention fidelity, using the VAS and MNWS, was done using one-way analysis of variance (ANOVA), with Bonferroni corrections for multiple pairwise comparisons. Correlations were performed between age (Pearson) and gender (Spearman) and the outcome measures. Baseline and stress-related inattention, response inhibition, and risk taking were analyzed using one-way ANOVA, with separate analyses differing by between-subject factor (smoking status or abstinence status [smokers only]). For analyses of stress-related outcomes, the corresponding baseline variable was controlled for (i.e., for stress-related inattention, baseline inattention was a covariate) to isolate stress-induced effects.
Results
Baseline Assessment
Correlations indicated that inattentive (omission) errors and age were significantly related among the whole sample (r = .559; p = .004) and smokers (r = .678; p = .031); response inhibition (commission errors) and gender were correlated within the entire sample (ρ = .458; p = .021). Supplementary Table 1 (online only) captures all correlations. At baseline, smokers and nonsmokers differed on both inattention; F(1, 26) = 6.640, p = .017; partial η2 = .224; and risk taking; F(1, 26) = 5.111, p = .033; partial η2 = .176. Smokers were more inattentive (T-score = 51.48 ± 9.88) and risky (mean adjusted pumps = 40.13 ± 10.48) than nonsmokers (inattention T-score = 44.61 ± 2.71; mean adjusted pumps = 29.16 ± 13.72). Response inhibition (commission) errors did not differ by smoking status. Smokers who were abstinent and nonabstinent at the end of the cessation trial did not differ on any baseline measures (ps > .05).
Stress Induction Validity
Participants endorsed increases in stress on the VAS from preinduction (11.67 cm ± 15.67) to postinduction (31.0 cm ± 26.65; Bonferroni corrected p = .027); these stress levels had a nonsignificant decline to the end of the assessment battery (19.3 cm ± 18.70; Bonferroni corrected p = .108) and declined significantly after participants listened to their relaxing situation (7.24 cm ± 9.01; poststress to postrelaxation Bonferroni corrected p = .003; postassessment to postrelaxation Bonferroni corrected p = .005). Participants also evidenced significant increases in depression (p < .001), anger, frustration or irritability (p = .003), and anxiety (p = .043) on the MNWS from pre- to postinduction. These findings indicate that the stress induction was a valid manipulation, increasing stress levels across participants.
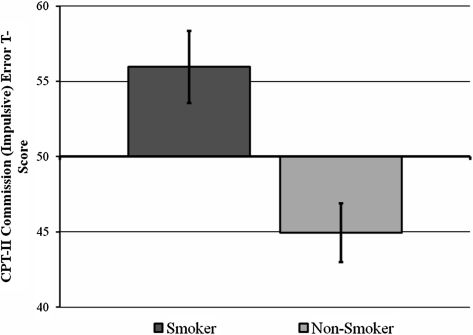
Stress-Related Differences by Smoking Status
After controlling for baseline performance differences between groups, poststress CPT-II commission (response inhibition) errors were found to differ by smoking status; F(1, 26) = 4.313, p = .050; partial η2 = .164. Smokers had higher levels of commission errors (T-score = 55.97 ± 10.70) than nonsmokers (T-score = 44.96 ± 12.38), which is illustrated in Figure 1. No stress-related differences by smoking status were observed for CPT-II inattentive errors or the BART (ps > .05).
Figure 1.
Smoking status and poststressor impulsive responding.
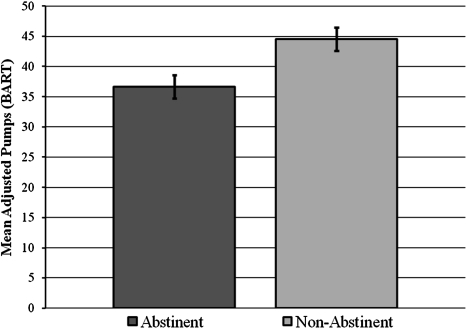
Differences Within Smokers by End-of-Treatment Abstinence
Controlling for baseline performance (end-of-treatment abstinent smokers: 40.20 ± 14.48; nonabstinent smokers: 40.08 ± 7.85), the only significant abstinence-related finding was on the BART; F(1, 11) = 9.835, p = .012, partial η2 = .522. At the poststressor assessment, smokers who were abstinent at the end of the smoking cessation trial engaged in fewer pumps (36.66 ± 13.25) than nonabstinent smokers (44.56 ± 7.53). This is illustrated in Figure 2. Poststressor levels of commission and omission errors and stress-related changes in MNWS symptoms and the VAS did not differ by end-of-treatment abstinence status (ps > .05).
Figure 2.
End-of-treatment abstinence and poststressor risk taking.
Discussion
In all, this pilot investigation supported several of the proposed hypotheses. First, smokers had higher levels of inattentive (omission) errors and engaged in greater levels of risk than nonsmokers at baseline. This is consistent with much of the established literature (e.g., Reynolds et al., 2007). We also found that smokers committed greater levels of response inhibition (commission) errors after stress exposure after controlling for baseline differences in commission errors and risk taking. This suggests that stress decreases response inhibition in smokers but not in nonsmokers. While previous research indicates decreased response inhibition after experimental stress exposure (see Sinha, 2001), this is the first study to demonstrate a difference by smoking status in adolescents. The results are also consistent with findings that greater perceived stress levels were significantly associated with greater risk taking among adolescents (Fields, Leraas, Collins, & Reynolds, 2009); however, the current study is the first prospective examination of these relationships in adolescents. Together, these results indicate that preventive interventions need to target decreasing stress and increasing nonimpulsive stress coping in adolescent smokers.
Most importantly, we found preliminary evidence that adolescent smokers who achieved abstinence in a cessation program that took place after the stress induction paradigm appeared to decrease their engagement in risk taking, while smokers who did not achieve abstinence increased their risk taking following stress exposure. This is notable in contrast to the finding by Shiffman (2005) that day-to-day changes in stressors did not predict smoking relapse. Perhaps our findings indicate that it is not stress exposure per se but one's reaction to stress exposure and any consequent increases in risk taking that increase smoking relapse risk (Sinha, 2001). That said, Shiffman's work examined adults and this examined adolescents, so developmental differences may also underlie discrepancies. Furthermore, nicotine withdrawal symptoms did not mediate this relationship as no significant interaction between nicotine withdrawal change (pre- to poststressor) and end-of-treatment abstinence was found. While in need of further study, these findings argue that addressing stress-related risk taking in adolescent smokers may help cessation attempts succeed.
Some limitations of this study should be noted. First, this is a pilot investigation with a small sample size, and hence, future replication with a larger sample size is warranted. Second, baseline CPT-II and BART performance were obtained on a different day than the stress induction session. This was done because of logistical issues, so some differences on the stress induction day could have been due to smoking or abstinence status; that said, controlling for baseline performance should have limited this. Finally, we did not control for gender in examining smoking status differences in response inhibition, despite a significant correlation. We did this because the CPT-II results are normed for gender and because of concerns about such analyses being underpowered. The current study, however, was strengthened by the use of a validated stress imagery paradigm by biochemical verification of smoking status and validated assessments of inattention, response inhibition, and risk taking.
These results indicate that stress-related increases in risk taking may mark increased risk for later cessation failure in adolescents. Given the small sample size, further investigations are needed that replicate these results and expand them to other developmental groups. In all, though, these findings provide evidence that intervention programs need to account for the relationships among stress, response inhibition, and risk taking to maximize their impact adolescent smoking rates.
Supplementary Material
Supplementary Table 1 can be found online at http://www.ntr.oxfordjournals.org
Funding
Preparation of this manuscript was supported by National Institutes of Health (NIH) grants R01 DA026450, P50 DA09421, and T32 DA07238 and the NIH Roadmap for Research Common Fund grants UL1-DE019586 and 1RL5 DA024858 that support the Interdisciplinary Research Consortium on Stress, Self-Control, and Addiction and Interdisciplinary Research Education.
Declaration of Interests
None declared.
Supplementary Material
Acknowledgments
None declared.
References
- Brown RA, Lewinsohn PM, Seeley JR, Wagner EF. Cigarette smoking, major depression, and other psychiatric disorders among adolescents. Journal of the American Academy of Child and Adolescent Psychiatry. 1996;35:1602–1610. doi: 10.1097/00004583-199612000-00011. doi:10.1097/00004583-199612000-00011. [DOI] [PubMed] [Google Scholar]
- Burt RD, Peterson AV., Jr. Smoking cessation among high school seniors. Preventive Medicine. 1998;27:319–327. doi: 10.1006/pmed.1998.0269. doi:10.1006/pmed.1998.0269. [DOI] [PubMed] [Google Scholar]
- Cavallo DA, Cooney JL, Duhig AM, Smith AE, Liss TB, McFetridge AK, et al. Combining cognitive behavioral therapy with contingency management for smoking cessation in adolescent smokers: A preliminary comparison of two different CBT formats. American Journal on Addictions. 2007;16:468–474. doi: 10.1080/10550490701641173. doi:10.1080/10550490701641173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conners CK. Conners’ Continuous PerformanceTest (CPT-II) computer program for Windows: Technical guide and software manual. North Tonawanda, NY: Multi-Health Systems; 2000. [Google Scholar]
- Department of Health and Human Services. Preventing tobacco use among young people: A report of the Surgeon General. (DHHS Publication No. CDC 89-8411) Washington, DC: U.S. Government Printing Office; 1994. [Google Scholar]
- Fields S, Collins C, Leraas K, Reynolds B. Dimensions of impulsive behavior in adolescent smokers and nonsmokers. Experimental and Clinical Psychopharmacology. 2009;17:302–311. doi: 10.1037/a0017185. doi:2009-17802-003 [pii]10.1037/a0017185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fields S, Leraas K, Collins C, Reynolds B. Delay discounting as a mediator of the relationship between perceived stress and cigarette smoking status in adolescents. Behavioural Pharmacology. 2009;20:455–460. doi: 10.1097/FBP.0b013e328330dcff. doi:10.1097/FBP.0b013e328330dcff. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hughes JR, Hatsukami D. Signs and symptoms of tobacco withdrawal. Archives of General Psychiatry. 1986;43:289–294. doi: 10.1001/archpsyc.1986.01800030107013. [DOI] [PubMed] [Google Scholar]
- Johnston LD, O’Malley PM, Bachman JG, Schulenberg JE. Monitoring the future national survey results on drug use, 1975–2008: Volume II, college students and adults ages 19-50. (NIH Publication No. 09-7403) Bethesda, MD: National Institute on Drug Abuse; 2009. [Google Scholar]
- Krishnan-Sarin S, Duhig AM, McKee SA, McMahon TJ, Liss T, McFetridge A, et al. Contingency management for smoking cessation in adolescent smokers. Experimental and Clinical Psychopharmacology. 2006;14:306–310. doi: 10.1037/1064-1297.14.3.306. doi:10.1037/1064-1297.14.3.306. [DOI] [PubMed] [Google Scholar]
- Krishnan-Sarin S, Reynolds B, Duhig AM, Smith A, Liss T, McFetridge A, et al. Behavioral impulsivity predicts treatment outcome in a smoking cessation program for adolescent smokers. Drug and Alcohol Dependence. 2007;88:79–82. doi: 10.1016/j.drugalcdep.2006.09.006. doi:10.1016/j.drugalcdep.2006.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leigh BC. Peril, chance, adventure: Concepts of risk, alcohol use and risky behavior in young adults. Addiction. 1999;94:371–383. doi: 10.1046/j.1360-0443.1999.9433717.x. [DOI] [PubMed] [Google Scholar]
- Lejuez CW, Aklin WM, Jones HA, Richards JB, Strong DR, Kahler CW, et al. The Balloon Analogue Risk Task (BART) differentiates smokers and nonsmokers. Experimental and Clinical Psychopharmacology. 2003;11:26–33. doi: 10.1037//1064-1297.11.1.26. [DOI] [PubMed] [Google Scholar]
- Lejuez CW, Read JP, Kahler CW, Richards JB, Ramsey SE, Stuart GL, et al. Evaluation of a behavioral measure of risk taking: The Balloon Analogue Risk Task (BART) Journal of Experimental Psychology: Applied. 2002;8:75–84. doi: 10.1037//1076-898x.8.2.75. [DOI] [PubMed] [Google Scholar]
- Lewinsohn PM, Rohde P, Brown RA. Level of current and past adolescent cigarette smoking as predictors of future substance use disorders in young adulthood. Addiction. 1999;94:913–921. doi: 10.1046/j.1360-0443.1999.94691313.x. doi:10.1046/j.1360-0443.1999.94691313.x. [DOI] [PubMed] [Google Scholar]
- McKee SA, Maciejewski PK, Falba T, Mazure CM. Sex differences in the effects of stressful life events on changes in smoking status. Addiction. 2003;98:847–855. doi: 10.1046/j.1360-0443.2003.00408.x. doi:10.1046/j.1360-0443.2003.00408.x. [DOI] [PubMed] [Google Scholar]
- Parrott AC, Kaye FJ. Daily uplifts, hassles, stresses and cognitive failures: In cigarette smokers, abstaining smokers, and non-smokers. Behavioural Pharmacology. 1999;10:639–646. doi: 10.1097/00008877-199911000-00010. [DOI] [PubMed] [Google Scholar]
- Porcelli AJ, Delgado MR. Acute stress modulates risk taking in financial decision making. Psychological Science. 2009;20:278–283. doi: 10.1111/j.1467-9280.2009.02288.x. doi:10.1111/j.1467-9280.2009.02288.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reynolds B, Patak M, Shroff P, Penfold RB, Melanko S, Duhig AM. Laboratory and self-report assessments of impulsive behavior in adolescent daily smokers and nonsmokers. Experimental and Clinical Psychopharmacology. 2007;15:264–271. doi: 10.1037/1064-1297.15.3.264. doi:10.1037/1064-1297.15.3.264. [DOI] [PubMed] [Google Scholar]
- Schepis TS, Duhig AM, Liss T, McFetridge A, Wu R, Cavallo DA, et al. Contingency management for smoking cessation: Enhancing feasibility through use of immunoassay test strips measuring cotinine. Nicotine and Tobacco Research. 2008;10:1495–1501. doi: 10.1080/14622200802323209. doi:10.1080/14622200802323209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schepis TS, Rao U. Smoking cessation for adolescents: A review of pharmacological and psychosocial treatments. Current Drug Abuse Reviews. 2008;1:142–155. doi: 10.2174/1874473710801020142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shiffman S. Dynamic influences on smoking relapse process. Journal of Personality. 2005;73:1715–1748. doi: 10.1111/j.0022-3506.2005.00364.x. doi:10.1111/j.0022-3506.2005.00364.x. [DOI] [PubMed] [Google Scholar]
- Sinha R. How does stress increase risk of drug abuse and relapse? Psychopharmacology (Berlin) 2001;158:343–359. doi: 10.1007/s002130100917. doi:10.1007/s002130050898. [DOI] [PubMed] [Google Scholar]
- Sinha R. Modeling stress and drug craving in the laboratory: Implications for addiction treatment development. Addiction Biology. 2009;14:84–98. doi: 10.1111/j.1369-1600.2008.00134.x. doi:10.1111/j.1369-1600.2008.00134.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sinha R, Catapano D, O’Malley S. Stress-induced craving and stress response in cocaine dependent individuals. Psychopharmacology (Berlin) 1999;142:343–351. doi: 10.1007/s002130050898. doi:10.1007/s002130050898. [DOI] [PubMed] [Google Scholar]
- Sinha R, Talih M, Malison R, Cooney N, Anderson GM, Kreek MJ. Hypothalamic-pituitary-adrenal axis and sympatho-adreno-medullary responses during stress-induced and drug cue-induced cocaine craving states. Psychopharmacology (Berlin) 2003;170:62–72. doi: 10.1007/s00213-003-1525-8. doi:10.1007/s00213-003-1525-8. [DOI] [PubMed] [Google Scholar]
- Swann AC. Neuroreceptor mechanisms of aggression and its treatment. Journal of Clinical Psychiatry. 2003;64(Suppl. 4):26–35. [PubMed] [Google Scholar]
- Toll BA, O’Malley SS, McKee SA, Salovey P, Krishnan-Sarin S. Confirmatory factor analysis of the Minnesota Nicotine Withdrawal Scale. Psychology of Addictive Behaviors. 2007;21:216–225. doi: 10.1037/0893-164X.21.2.216. doi:10.1037/0893-164X.21.2.216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tonissaar M, Herm L, Eller M, Koiv K, Rinken A, Harro J. Rats with high or low sociability are differently affected by chronic variable stress. Neuroscience. 2008;152:867–876. doi: 10.1016/j.neuroscience.2008.01.028. doi:10.1016/j.neuroscience.2008.01.028. [DOI] [PubMed] [Google Scholar]
- van der Oord S, Prins PJ, Oosterlaan J, Emmelkamp PM. The association between parenting stress, depressed mood and informant agreement in ADHD and ODD. Behaviour Research and Therapy. 2006;44:1585–1595. doi: 10.1016/j.brat.2005.11.011. doi:S0005-7967(05)00249-4 [pii]10.1016/j.brat.2005.11.011. [DOI] [PubMed] [Google Scholar]
- White TL, Lejuez CW, de Wit H. Test-retest characteristics of the Balloon Analogue Risk Task (BART) Experimental and Clinical Psychopharmacology. 2008;16:565–570. doi: 10.1037/a0014083. doi:2008-17521-013 [pii]10.1037/a0014083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu SH, Sun J, Billings SC, Choi WS, Malarcher A. Predictors of smoking cessation in U.S. adolescents. American Journal of Preventive Medicine. 1999;16:202–207. doi: 10.1016/s0749-3797(98)00157-3. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.