Abstract
Background
In order to determine the clinical usefulness of the MicroScan (Siemens Healthcare Diagnostics, USA) MICroSTREP plus antimicrobial panel (MICroSTREP) for testing antimicrobial susceptibility of β-hemolytic streptococci (BHS) and viridans group streptococci (VGS), we compared the accuracy of MICroSTREP with that of the CLSI reference method.
Methods
Seventy-five BHS and 59 VGS isolates were tested for antimicrobial susceptibility to ampicillin, penicillin, cefotaxime, meropenem, erythromycin, clindamycin, levofloxacin, and vancomycin by using MICroSTREP and the CLSI agar dilution method.
Results
The overall essential agreement with regard to minimum inhibitory concentrations (MICs) (within ±1 double dilution) between MICroSTREP and the CLSI reference method was 98.2%, and categorical agreement (CA) was 96.9%. For the BHS isolates, the CA for erythromycin was 96.0%, whereas that for cefotaxime, meropenem, levofloxacin, and vancomycin (for ampicillin, penicillin, and clindamycin; 98.7%) was 100%. For the VGS isolates, the CA for penicillin was 84.7% and that for erythromycin, clindamycin, and vancomycin (for meropenem, 86.5%; for ampicillin, 88.1%; and for cefotaxime and levofloxacin, 96.6%) was 100%. All categorical errors of penicillin and ampicillin in the VGS isolates were minor.
Conclusions
The accuracy of MICroSTREP is comparable to that of the CLSI reference method, suggesting that this panel can be effective for testing antimicrobial susceptibility of BHS and VGS.
Keywords: Antimicrobial susceptibility test, Streptococcus, MICroSTREP, MicroScan
INTRODUCTION
β-Hemolytic streptococcal isolates obtained from humans can be subdivided into large-colony and small-colony (<0.5 mm in diameter) formers. Large colony formers include Streptococcus pyogenes (Lancefield group A antigen), Streptococcus agalactiae (Lancefield group B antigen), and Streptococcus dysgalactiae subsp. equisimilis (Lancefield group C and G antigens) [1]. The small-colony-forming β-hemolytic strains with Lancefield group A, C, F, or G antigens are considered part of the viridans group streptococci (VGS). VGS also include Streptococcus mitis, Streptococcus oralis, Streptococcus mutans, Streptococcus salivarius, Streptococcus sanguinis, and Streptococcus bovis [1]. Although penicillin remains the drug of choice in the treatment of infections caused by large-colony-forming β-hemolytic streptococci (BHS), drug tolerance and clinical therapeutic failures have been reported [2]. Macrolides and lincosamides have been frequently used to prevent β-lactam allergies in patients. These agents are also used in empiric and preventive therapies for the treatment of BHS infections [3, 4]. However, recent studies have shown considerable changes in the susceptibility of BHS to erythromycin and clindamycin, although different resistance rates to these agents owing to geographical variation and investigators have been reported [5-7]. β-Lactam agents have been the treatment of choice for VGS infections; however, increase in the incidence of VGS with multidrug-resistance to penicillin and other agents, such as cephalosporins, macrolides, lincosamides, tetracycline, quinupristin-dalfopristin, and quinolones, has been reported [7, 8]. Moreover, CLSI has recommended that VGS isolated from normally sterile body sites should be tested for penicillin susceptibility by using a minimum inhibitory concentration (MIC) method and interpretive criteria [9]. Accurate susceptibility testing for BHS and VGS is required in order to guide appropriate antimicrobial therapy and to monitor further spread of resistant pathogens. Rising drug resistance of BHS and VGS has increased the need for accurate determination of antimicrobial susceptibility in a timely manner in clinical microbiology laboratories. Rapid reporting of the results of an antimicrobial susceptibility test (AST) has been shown to improve patient outcomes and reduce hospital costs [10, 11]. Because there are significant differences in the susceptibility of BHS and VGS to β-lactam agents, there are separate interpretive criteria for the susceptibility of the 2 groups of organisms to ampicillin, penicillin, cefotaxime, ceftriaxone, and cefepime [9].
Automated commercial susceptibility test systems for streptococci offer reliable AST results for MIC measurement and help accurately determine the antimicrobial susceptibility profile according to the Streptococcus group. However, most studies are focused on evaluating the AST performance of Streptococcus pneumoniae. To the best of our knowledge, no study has been conducted to evaluate the accuracy of the automated MicroScan (Siemens Healthcare Diagnostics, Sacramento, CA, USA) AST system for susceptibility testing of BHS and VGS. Therefore, this study was designed to evaluate the clinical usefulness of the MicroScan MICroSTREP plus antimicrobial panel (MICroSTREP) as a susceptibility testing system for BHS and VGS.
MATERIALS AND METHODS
1. Bacterial isolates
A total of 134 isolates of BHS (75 isolates) and VGS (59 isolates) were stocked from various clinical specimens obtained from January to December 2009 at Wonju Christian Hospital, Korea. Multiple isolates from the same patient were avoided. The predominant specimen sources were wounds (60, 44.8%), urinary tract (27, 20.1%), blood (13, 9.7%), and respiratory tract (11, 8.2%). The isolates were identified by on the basis of hemolytic patterns on 5% sheep blood agar, colony morphology, Gram staining, catalase reaction, and findings obtained by using the VITEK-2 GP identification system (bioMérieux, Marcy l'Étoile, France). The strains were stored in thioglycolate broth containing 20% glycerol at -70℃ until analysis. Thereafter, the frozen isolates were thawed, inoculated onto a 5% sheep blood agar plate, and incubated at 35℃ overnight. Pure isolates from 3 consecutive subcultures were tested for susceptibility. All 134 strains were tested using MICroSTREP and the CLSI reference method. Of the 134 isolates, BHS were S. agalactiae (61 isolates), S. pyogenes (9), and S. dysgalactiae (5), and VGS were S. mitis (34), Streptococcus anginosus (18), S. salivarius (3), S. sanguinis (2), and S. mutans (2).
2. Reference method
Susceptibility to penicillin, ampicillin, cefotaxime, erythromycin, clindamycin, levofloxacin (Sigma Chemical Co, St. Louis, MO, USA), meropenem (Yuhan, Seoul, Korea), and vancomycin (Daewoong Lilly, Seoul, Korea) was tested using the agar dilution method according to the recommendations of the CLSI [9]. Mueller-Hinton agar with 5% defibrinated sheep blood was used for the agar dilution test. Inocula were prepared by suspending colonies in tryptic soy broth to obtain approximately 104 colonies on inoculation using a Steers replicator (Craft Machine Inc, Chester, PA, USA). MIC was determined after 24 hr of incubation at 35℃. S. pneumoniae (ATCC 49619) was used as a control in the MIC determination. MIC was defined as the lowest concentration of an agent that yielded no growth or a mark-ed change in the appearance of the growth plate as compared to the growth control plate. The AST results obtained for the reference strains were consistently within the acceptable MIC range.
3. MicroScan MICroSTREP test
In the MicroScan MICroSTREP system, Renok hydrator/inoculator was used to deliver 115 µL of Mueller-Hinton broth with 3% lysed horse blood to each well. After inoculation with a 0.5 McFarland standard bacterial suspension, the panels were incubated at 35℃ in ambient air for 20-24 hr and read using the MicroScan WalkAway System (Siemens Healthcare Diagnostics).
4. Comparison of results
We analyzed essential agreement (EA) and categorical agreement (CA) between MICroSTREP and the CLSI reference method for each antibiotic tested. EA was defined as MIC of MICroSTREP and the CLSI reference method was within ±1 double dilution. CA was defined as interpretive category of MICroSTREP and the CLSI reference method was same. AST error rates were calculated and reported as follows: a very major error (VME) was recorded if an isolate was found to be susceptible on using MICroSTREP and resistant on employing the reference method; a major error (ME) was recorded if an isolate was found to be resistant on using MICroSTREP and susceptible on employing the reference method; and a minor error (MIE) was recorded if an isolate was judged intermediate on using MICroSTREP or the reference method and susceptible or resistant on employing the other method.
RESULTS
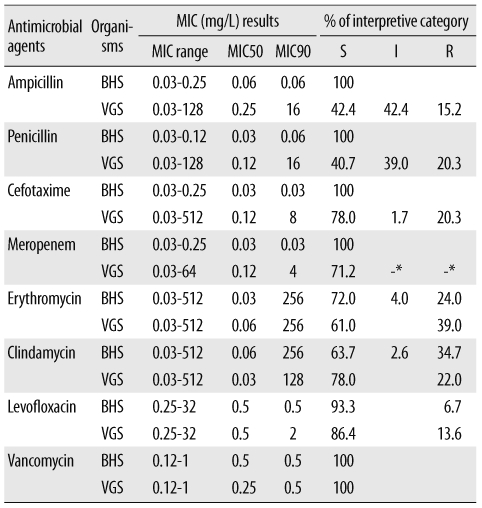
Using the agar dilution method, the VGS non-susceptibility rates were 57.6% for ampicillin (MIC ≥0.5 mg/L), 59.3% for penicillin (MIC ≥0.25 mg/L), 22.0% for cefotaxime (MIC ≥2 mg/L), 28.8% for meropenem (MIC >0.5 mg/L), 39.0% for erythromycin (MIC ≥0.5 mg/L), 22.0% for clindamycin (MIC ≥0.5 mg/L), and 13.6% for levofloxacin (MIC ≥4 mg/L). All BHS isolates were susceptible to ampicillin, penicillin, cefotaxime, and meropenem. Among the BHS isolates, the non-susceptibility rates for erythromycin, clindamycin, and levofloxacin were 28.0%, 37.3%, and 6.7%, respectively (Table 1).
Table 1.
Results of MIC ranges and interpretive category obtained by using the reference method for 134 BHS (75) and VGS (59) isolates
*Any interpretive category other than susceptible was classified as a nonsusceptible category when meropenem was tested for VGS.
Abbreviations: MIC, minimal inhibitory concentration; S, susceptible; I, intermediate; R, resistant; BHS, β-hemolytic streptococci; VGS, viridans group streptococci.
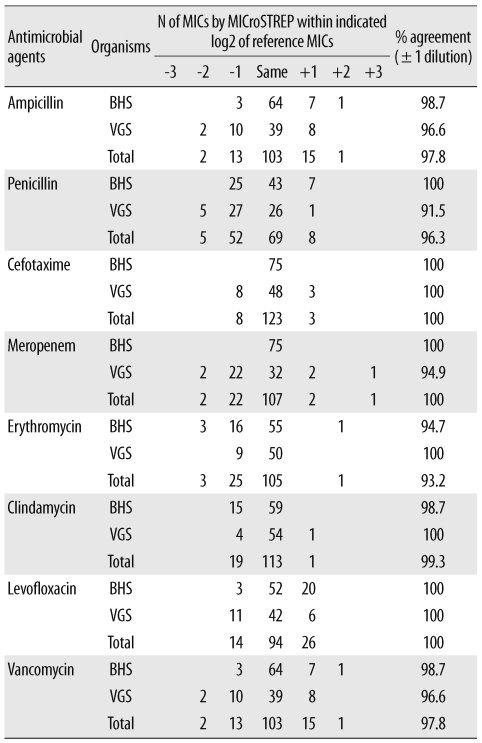
The overall EAs and CAs determined for MICroSTREP and the CLSI reference method were 98.2% and 96.9%, respectively (Tables 2 and 3). For the BHS isolates, the EAs for individual antimicrobial agents ranged from 94.7% (erythromycin) to 100% (penicillin, cefotaxime, meropenem, and levofloxacin), while the EA for ampicillin, clindamycin, and vancomycin was 98.7%. The CA for erythromycin was 96.0%; for cefotaxime, meropenem, levofloxacin, and vancomycin, 100%; and for ampicillin, penicillin, and clindamycin, 98.7%. For the VGS isolates, the EAs ranged from 91.5% (penicillin) to 100% (cefotaxime, erythromycin, clindamycin, and levofloxacin), and the EA for ampicillin and vancomycin was 96.6%. The CAs ranged from 84.7% (penicillin) to 100% (erythromycin, clindamycin, and vancomycin). The CAs for ampicillin and meropenem were 88.1% and 86.5%, respectively, and the CA for cefotaxime and levofloxacin was 96.6%.
Table 2.
Comparison of MICs determined by using MICroSTREP with MICs determined using the CLSI reference method for 134 BHS (75) and VGS (59) isolates
Abbreviations: MIC, minimal inhibitory concentration; MICroSTREP, MicroScan MICro-STREP plus antimicrobial panel; BHS, β-hemolytic streptococci; VGS, viridans group streptococci.
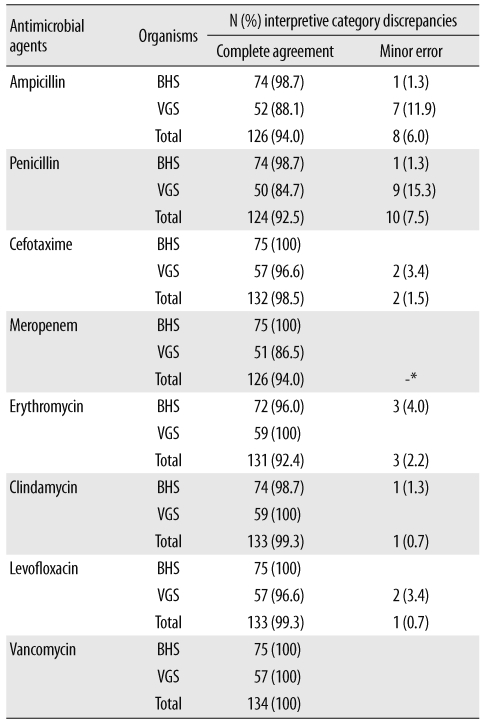
Table 3.
Interpretive category errors determined by comparing MICroSTREP and reference MICs for 134 BHS (75) and VGS (59) isolates
*Minor errors were not evaluated because any interpretive characteristic other than susceptibility was classified nonsusceptibility when meropenem was tested for VGS.
Abbreviations: MICroSTREP, MicroScan MICroSTREP plus antimicrobial panel; MIC, minimal inhibitory concentration; BHS, β-hemolytic streptococci; VGS, viridans group streptococci.
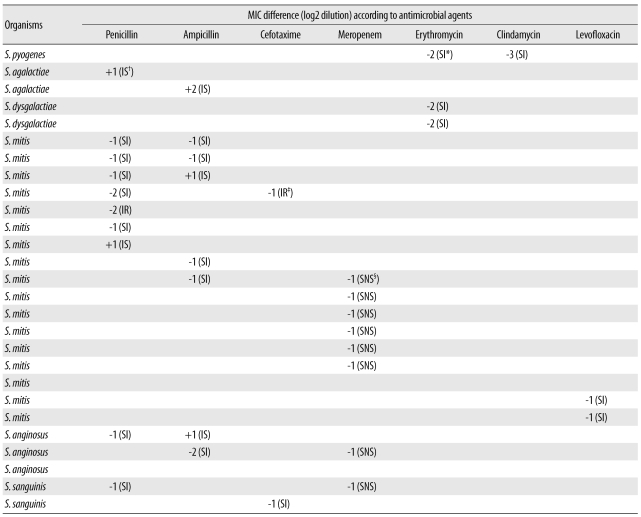
Of the total 134 isolates, all categorical errors were MIEs (Table 3). In the cases of 14 isolates for which MIEs were obtained for penicillin and/or ampicillin, MIEs for penicillin and ampicillin were obtained with 4 isolates (3 S. mitis isolates, 1 S. anginosus isolate); MIE only for penicillin was obtained with 6 isolates (4 S. mitis isolates, 1 S. anginosus isolate, and 1 S. agalactiae isolate); and MIE only for ampicillin was obtained with 4 isolates (2 S. mitis isolates, 1 S. anginosus isolate, 1 S. agalactiae isolate). The frequency of total MIEs obtained with BHS isolates was lower than that obtained with VGS isolates (Table 4).
Table 4.
Difference (log2 dilution) in MICs determined using MICroSTREP and reference method for 27 isolates showing categorical error by interpretive criteria
*judged susceptible using MICroSTREP and intermediate using the reference method; †judged intermediate using MICroSTREP and susceptible using the reference method; ‡judged intermediate using MICroSTREP and resistant using the reference method; §judged susceptible using MICroSTREP and non-susceptible using the reference method.
Abbreviations: MIC, minimal inhibitory concentration; MICroSTREP, MicroScan MICroSTREP plus antimicrobial panel; BHS, β-hemolytic streptococci; VGS, viridans group streptococci.
DISCUSSION
Healthcare professionals are faced with a variety of significant, fastidious organisms, including S. pneumoniae, BHS, and VGS, that are increasingly showing resistance to commonly used antimicrobial agents. Although, in the past, many laboratories may have chosen to screen VGS isolated from normally sterile body sites, e.g. cerebrospinal fluid, blood, and bone, to determine penicillin resistance, the rapid spread of multidrug-resistant strains requires a more aggressive approach. In addition, certain antimicrobials (penicillin, ampicillin, ertapenem, meropenem, and daptomycin) that may be used to treat VGS infections cannot be reliably tested using the disk diffusion method [9]. The CLSI also recommends the inclusion of penicillin (or ampicillin), cefepime (cefotaxime or ceftriaxone), erythromycin, clindamycin, and vancomycin in a routine, primary testing panel [9].
The accuracy and efficiency of AST dictates timely and appropriate decisions in choosing the antibiotic therapy. Automated systems with built-in expert systems can potentially increase the reproducibility and reliability of test results, and thus can be expected to improve the quality of patient care. In this study, penicillin-intermediate, and/or ampicillin-intermediate, and VGS isolates that were not susceptible to meropenem accounted for the bulk of the total MIEs. Despite the elevated frequency of MIEs obtained with VGS, the high EA values for penicillin, ampicillin, and meropenem suggest that these errors can be largely attributed to the MICs being close to the interpretive breakpoints (Table 4). In particular, all categorical errors for meropenem occurred when the MICroSTREP MIC was 2-fold dilution lower than the reference. The overall frequency of MIEs obtained with BHS was lower than that obtained with VGS, but MIEs for erythromycin and clindamycin were only detected with BHS. The highest MIE rates obtained for penicillin were similar to those reported by Guthrie et al. [12], who reported that penicillin was responsible for the highest MIE rate obtained with S. pneumoniae. When the reference MIC was close to a breakpoint value, 2 MIEs were observed for several isolates [13]. For most antibiotics, the MICroSTREP MICs tended to be lower than the reference MICs, which greatly contributed to the number of MIEs. The exceptions were the MIC results for ampicillin, levofloxacin, and vancomycin obtained with BHS: MICroSTREP reported higher MICs in these cases (Table 2). No VMEs or MEs were detected, and relatively few MIEs were observed. The only observed exceptions to the performance standards were categorical disagreement in cases of ampicillin, penicillin, and meropenem for VGS. The more the isolate population was concentrated near the MIC breakpoint level, the greater the possibility of categorical discrepancies between the results obtained using the testing instrument and the reference method. In contrast, the more the isolate population was distributed far away from MIC breakpoint level, the lesser the possibility of categorical discrepancies. Although diagnostic performance of the MIC testing system in BHS and VGS has not been reported, Jorgensen et al. [14] reported that MICroSTREP did not result in any VMEs or MEs and that high EA and CA values were achieved in testing with S. pneumoniae. The high EA and CA values obtained by using MICroSTREP satisfied the minimal performance criteria (CA, ≥90%; EA, ≥90%; VMEs, ≤1.5%; and MEs, ≤3%) of the Food and Drug Administration (FDA) [15]. The FDA suggested that 50% susceptible and 50% resistant distribution is desired to generate meaningful statistics regarding the performance characteristics of a method or system [15]. However, it was unlikely that sequentially collected isolates from clinical samples would be anything similar to the 50% susceptible and 50% resistant distribution suggested by the FDA.
The performance of MICroSTREP affirms the capability of the instrument as a reliable and efficient diagnostic tool for determining the appropriate antimicrobial agents for use against VGS and BHS infections. In conclusion, this instrument was able to decrease the turnaround time to results because of the reduced hands-on time required in comparison to that required in conventional laboratory methods.
Acknowledgement
This study was supported in part by Siemens Healthcare Diagnostics.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Uh Y, Hwang GY, Jang IH, Kwon O, Kim HY, Yoon KJ. Antimicrobial susceptibility patterns and macrolide resistance genes of β-hemolytic viridans group streptococci in a tertiary Korean hospital. J Korean Med Sci. 2007;22:791–794. doi: 10.3346/jkms.2007.22.5.791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gillespie SH. Failure of penicillin in Streptococcus pyogenes pharyngeal infection. Lancet. 1998;352:1954–1956. doi: 10.1016/s0140-6736(05)61327-x. [DOI] [PubMed] [Google Scholar]
- 3.Schuchat A. Group B streptococcal disease: from trials and tribulations to triumph and trepidation. Clin Infect Dis. 2001;33:751–756. doi: 10.1086/322697. [DOI] [PubMed] [Google Scholar]
- 4.Bisno AL, Gerber MA, Gwaltney JM, Jr, Kaplan EL, Schwartz RH. Practice guidelines for the diagnosis and management of group A streptococcal pharyngitis. Clin Infect Dis. 2002;35:113–125. doi: 10.1086/340949. [DOI] [PubMed] [Google Scholar]
- 5.Gordon KA, Beach ML, Biedenbach DJ, Jones RN, Rhomberg PR, Mutnick AH. Antimicrobial susceptibility patterns of β-hemolytic and viridans group streptococci: report from the SENTRY Antimicrobial surveillance program (1997-2000) Diagn Microbiol Infect Dis. 2002;43:157–162. doi: 10.1016/s0732-8893(02)00374-7. [DOI] [PubMed] [Google Scholar]
- 6.Jones RN, Sader HS. Update on the cefdinir spectrum and potency against pathogens isolated from uncomplicated skin and soft tissue infections in North America: are we evaluating the orally administered cephalosporins correctly? Diagn Microbiol Infect Dis. 2006;55:351–356. doi: 10.1016/j.diagmicrobio.2006.04.015. [DOI] [PubMed] [Google Scholar]
- 7.Hindler JF, Patel JB. Susceptibility test methods: fastidious bacteria. In: Murray PR, Baron EJ, et al., editors. Manual of clinical microbiology. 9th ed. Washington, DC: American Society for Microbiology Press; 2007. pp. 1193–1213. [Google Scholar]
- 8.Doern GV, Ferraro MJ, Brueggemann AB, Ruoff KL. Emergence of high rates of antimicrobial resistance among viridans group streptococci in the United States. Antimicrob Agents Chemother. 1996;40:891–894. doi: 10.1128/aac.40.4.891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Clinical and Laboratory Standards Institute. Performance standards for antimicrobial susceptibility testing; Twentieth informational supplement, M100-S20. Wayne, PA: Clinical and Laboratory Standards Institute; 2010. [Google Scholar]
- 10.Barenfanger J, Short MA, Groesch AA. Improved antimicrobial interventions have benefits. J Clin Microbiol. 2001;39:2823–2828. doi: 10.1128/JCM.39.8.2823-2828.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kerremans JJ, Verboom P, Stijnen T, Hakkaart-van Roijen L, Goessens W, Verbrugh HA, et al. Rapid identification and antimicrobial susceptibility testing reduce antibiotic use and accelerate pathogen-directed antibiotic use. J Antimicrob Chemother. 2008;61:428–435. doi: 10.1093/jac/dkm497. [DOI] [PubMed] [Google Scholar]
- 12.Guthrie LL, Banks S, Setiawan W, Waites KB. Comparison of MicroScan MICroSTREP, PASCO, and Sensititre MIC panels for determining antimicrobial susceptibilities of Streptococcus pneumoniae. Diagn Microbiol Infect Dis. 1999;33:267–273. doi: 10.1016/s0732-8893(98)00151-5. [DOI] [PubMed] [Google Scholar]
- 13.Mittman SA, Huard RC, Della-Latta P, Whittier S. Comparison of BD phoenix to Vitek 2, MicroScan MICroSTREP, and Etest for antimicrobial susceptibility testing of Streptococcus pneumoniae. J Clin Microbiol. 2009;47:3557–3561. doi: 10.1128/JCM.01137-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jorgensen JH, McElmeel ML, Crawford SA. Evaluation of the Dade MicroScan MICroSTREP antimicrobial susceptibility testing panel with selected Streptococcus pneumoniae challenge strains and recent clinical isolates. J Clin Microbiol. 1998;36:788–791. doi: 10.1128/jcm.36.3.788-791.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Food and Drug Administration. guidance for industry and FDA. Rockville, MD: Food and Drug Administration; 2007. Class II special controls guidance document: antimicrobial susceptibility test (AST) systems. [Google Scholar]