Abstract
Purpose
To assess the impact of change in visual field (VF) on change in health related quality of life (HRQoL) at the population level.
Design
Prospective cohort study
Participants
3,175 Los Angles Latino Eye Study (LALES) participants
Methods
Objective measures of VF and visual acuity and self-reported HRQoL were collected at baseline and 4-year follow-up. Analysis of covariance was used to evaluate mean differences in change of HRQoL across severity levels of change in VF and to test for effect modification by covariates.
Main outcome measures
General and vision-specific HRQoL.
Results
Of 3,175 participants, 1430 (46%) showed a change in VF (≥1 decibel [dB]) and 1651, 1715 (54%) reported a clinically important change (≥5 points) in vision-specific HRQoL. Progressive worsening and improvement in the VF were associated with increasing losses and gains in vision-specific HRQoL for the composite score and 10 of its 11 subscales (all Ptrends<0.05). Losses in VF > 5 dB and gains > 3 dB were associated with clinically meaningful losses and gains in vision-specific HRQoL, respectively. Areas of vision-specific HRQoL most affected by greater losses in VF were driving, dependency, role-functioning, and mental health. The effect of change in VF (loss or gain) on mean change in vision-specific HRQoL varied by level of baseline vision loss (in visual field and/or visual acuity) and by change in visual acuity (all P-interactions<0.05). Those with moderate/severe VF loss at baseline and with a > 5 dB loss in visual field during the study period had a mean loss of vision-specific HRQoL of 11.3 points, while those with no VF loss at baseline had a mean loss of 0.97 points Similarly, with a > 5 dB loss in VF and baseline visual acuity impairment (mild/severe) there was a loss in vision-specific HRQoL of 10.5 points, whereas with no visual acuity impairment at baseline there was a loss of vision-specific HRQoL of 3.7 points.
Conclusion
Both losses and gains in VF produce clinically meaningful changes in vision-specific HRQoL. In the presence of pre-existing vision loss (VF and visual acuity), similar levels of visual field change produce greater losses in quality of life.
Approximately 314 million people worldwide are visually impaired, and about 82% of those 314 million are over the age of 50 years.1 The prevalence of visual impairment in the United States (U.S.) adult population over the age of 50 years ranges from 14.3% to 20.5%.2 Visual impairment can lead to disability,3 and as the number of older individuals increases in the U.S., the prevention and management of vision-related disability has become a major public health4 and clinical priority.5
Using health-related quality of life (HRQoL) as a measure of disability, researchers have noted that both visual field loss and visual acuity impairment are associated with increased disability. Population6–9 and multi-center clinically based studies10 consistently seem to indicate that worse visual impairment correlates with poorer HRQoL. Furthermore, individuals with higher levels of visual impairment are at increased risk for poorer outcomes such as falls and falls with injury,11 motor vehicle accidents,12 inability to drive,13 social dependence,14 and increased mortality.15, 16
Most studies, however, have evaluated the impact of prevalent visual impairment on HRQoL rather than the impact of change in visual impairment or the joint effect of both visual field (VF) loss and visual acuity impairment on HRQoL. The Los Angeles Latino Eye Study (LALES),17 a prospective cohort study among Latino adults, offers the unique opportunity to test these hypotheses in a population-based sample. The central focus of this report was to further our current understanding of visual impairment on HRQoL by evaluating the impact of VF changes on HRQoL and to test whether pre-existing levels of vision loss modify this association. These results may provide important evidence-based knowledge necessary to tailor both public health and clinical interventions aimed toward preventing or delaying vision-related disability or toward increasing awareness of vision-related disability, especially for those with VF loss, which is often an irreversible condition.
Material and Methods
Study Population
Details of the study design and data collection have been described previously.17 Briefly, a census of all residential households from 6 census tracts in La Puente, California, was completed to identify individuals eligible for the study; men and women ≥ 40 years of age and self-described as Latino were included. Home interviews and clinic examinations were carried out between February 2000 and May 2003 and were repeated after 4 years between January 2004 and May 2008. Informed consent was obtained for each participant, and institutional review board ethics committee approval was obtained from the Los Angeles County/University of Southern California Medical Center institutional review board (approval No. 969004 and 041004).
Data Collection
Demographics, history of medical conditions,18 insurance, and degree of acculturation were collected via computer-assisted, in-person interviews in the preferred language (English or Spanish) of each individual. Operational definitions were based on variables described in the Hispanic Health and Nutrition Examination Survey.19, 20 Acculturation was measured using the short-form Cuellar Acculturation Scale, with scores ranging from 1(low level) to 5 (high level).21
Visual Field
Testing was performed separately in each eye with the Humphrey Automated Field Analyzer II (Swedish Interactive Thresholding Algorithm [SITA] Standard 24-2 program) (Carl Zeiss Meditec, Dublin, CA) and repeated for any abnormal results. Results of the second test were confirmed as visual field loss (VFL) by two ophthalmologists. Results are reported as the average depression (or elevation) of the measured visual field compared to an age-adjusted normal reference expressed as mean deviation (MD) in decibels (dB), which has favorable test-retest reliability.22 Individuals who did not show reliable tests (4%) were excluded from the analysis.
Baseline VFL was categorized into four severity levels: none (MD>−2 dB), mild (MD ≤ −2 dB and ≥ −6 dB), moderate (MD<−6 dB and ≥−12 dB), and severe (MD <−12 dB) based on previous studies.7, 23
Change in VF was calculated as the difference between follow-up and baseline measurements in the better and worse eye, separately. Negative values indicate loss in VF while positive values indicate improvement. Change in VF was normally distributed and modeled as both a continuous and a categorical variable. Although previous clinical trials suggest that a loss in VF ≥ 3 dB is considered substantial,24 there are no established categories for interpreting the magnitude of change in VF at the population level. Therefore, we initially created and tested 2 dB intervals. The extreme categories for both loss and gain were then collapsed to increase the sample size within these strata. The final categories were as follows: a) −33 to −5.1 dB; b) −5 to −3.1 dB; c) −3 to −1.1 dB; d) −1 to +1 dB; e) +1.1 to +3 dB; and f) +3.1 to +35 dB. Values of between −1 dB to +1 dB were considered as no change.25 Similar quantitative results were noted for 1 dB intervals; however, limited sample sizes in some categories produced unstable estimates.
Visual Acuity
Visual acuity was measured as presenting binocular distance visual acuity as previously described.17 Briefly, each participant was measured with the presenting correction (if any) at 4 meters using modified Early Treatment Diabetic Retinopathy Study distance charts trans-illuminated with a chart illuminator (Precision Vision, La Salle, IL). Visual acuity was scored as the total number of lines read correctly and then converted to a logarithm of the minimum angle of resolution (logMAR) score.
Baseline visual acuity was modeled as a categorical variable as follows: no visual impairment (< 20/40 in both eyes), mild visual impairment (between 20/40 and 20/63 in at least one eye), and moderate/severe visual impairment (20/80 or worse in one or both eyes) according to previously published reports.26
Change in visual acuity over the 4-year interval was modeled as a 3-level categorical variable, considered clinically important26, 27: no change, ≥2 line improvement, and ≥2 line loss, which is considered clinically important.
Health-Related Quality of Life Assessment
General HRQoL
The Medical Outcomes Study 12-Item Short-Form Health Survey (SF-12, version 1) was used to calculate the standard U.S. norm-based Physical Component Summary (PCS) and Mental Component Summary (MCS) scores, 28 with larger scores representing better HRQoL.29 The PCS and MCS are scored on a T-score metric with the mean equal to 50 and standard deviation (SD) equal to 10 in the U.S. general population.29
Change in SF-12 score was calculated by subtracting baseline from 4-year follow-up scores. Negative values indicate loss in HRQoL while positive values indicate improvement. Changes in SF-12 scores were normally distributed and modeled as continuous variables.
Vision-specific HRQoL
Vision-specific HRQoL was assessed by the National Eye Institute Visual Function Questionnaire-25,30, 31 administered before a vision test. The questionnaire measures the impact of vision status on generic health domains such as emotional well-being and social functioning, as well as task-oriented domains related to daily visual functioning. It contains 12 vision-specific subscales: general health, general vision, near and distance vision activities, ocular pain, vision-related social function, vision-related role function, vision-related mental health, vision-related dependency, driving difficulties, color vision, and peripheral vision. Each subscale consists of 1 to 4 items. The standard recommended algorithm was used to calculate scale scores that range from 0 to 100.30 Higher scores represent better HRQoL. Eleven of the 12 subscale scores (excluding general) were averaged to yield a composite score.30
Baseline vision-specific HRQoL composite score was not normally distributed and therefore categorized into three levels by tertiles as follows: low (median=71.3, range= 2.6–81.3 ), medium (median=87.1, range=81.4–90.5), high (median=93.6, range=90.6–100). Change in vision-specific HRQoL composite scores and subscales was calculated by subtracting scores at baseline from scores at 4-year follow-up; negative values indicated loss in HRQoL and positive values indicated improvement. Change in subscales and composite scores was normally distributed and modeled as both continuous and categorical variables. Categories were defined as loss [< −1 point], no change [−1 to 1 points], or improvement [>1 point]; and a minimally important difference was defined as a ≥5 point change [loss or gain].7, 26
Statistical Analyses
Covariates were compared across baseline VFL severity categories using analysis of variance and Pearson’s chi-square. Wilcoxon ranked-sum test was used to quantify change in VFL and HRQoL during the 4-year study period. Since change in VF was measured in the better and worse eye separately and binocular change in VF was not available at the time of this study, it was of interest to understand whether better and worse eye changes in VF were associated and whether the effects on HRQoL were comparable. For the first analysis Pearson’s correlation coefficient (continuous change in VF) and Kappa statistic (categorical change in VF) were used. For the second, an iterative, locally weighted, least squares method to generate lines of best fit (LOWESS fit line32 was employed.
Analysis of covariance was used to model mean differences of change in HRQoL scores across severity levels of change in VF and to adjust for covariates that resulted in a change in effect of ≥10%.33 Since none of the baseline covariates confounded the association between change in visual field and change in HRQoL, the main results are presented for the unadjusted model. Linear trends using F tests were calculated. Standard diagnostic procedures showed no substantial departure from model assumptions. Proportions of individuals with a clinically important change in vision-specific HRQoL were compared across severity levels of change in VF using Pearson chi-square and tests for trend.
Based on previous results from a clinical trial suggesting that age and baseline visual field status modifies the impact of the intervention on visual field progression 24 we tested for interaction between change in visual field and covariates based on biological plausibility (age, and baseline visual field loss). Furthermore, we have previously shown that baseline central visual acuity and change in visual acuity has significant impact on HRQoL.27 Therefore, it was important to examine any interactions with these covariates. Interaction was evaluated by generating multiplicative interaction terms (dummy variables) and introducing each interaction in a separate model adjusted for the main effect. Analysis of covariance and corresponding F-tests were used to evaluate statistical significance.
All hypothesis testing was two-sided, assuming a 0.05 significance level. All analysis was conducted using Stata 10.0 software (Stata Corporation, College Station, TX).
Results
A total of 7,789 participants were identified as eligible for the study; 6,357 (82%) completed the eye examination and 6,131 (79%) completed both the eye examination and the in-home interview. At the 4-year follow-up, 4,658/6,100 living eligible participants (76%) completed the eye examination; of these, 3,625 (78%) completed the in-home interview. The final analysis cohort included 3,175 participants with complete information regarding change in VF and HRQoL. A comparison of participants who completed the follow-up examination (n=4658) versus those who did not (n=1442) has been reported previously34 and in brief showed that those participants who completed the exam were more likely to be female (60% vs. 56%, P<0.003) and slightly older (54.7 vs. 53.1, P<0.001), less likely to be married (67% vs. 71%, P=.01), more likely to have health insurance (67% vs. 54%, P<0.001), more likely to have ≥2 co-morbidities (41% vs. 34%, P<0.001), and more likely to report any ocular disease (13% vs.11%, P=0.01). There was no differential drop-out by country of birth, acculturation, employment, income level, or self-report of health as excellent or very good.
Table 1 (available at http://aaojournal.org) shows that as the severity of baseline visual field loss increased (none to severe) participants were more likely to be older and female, to have worse visual acuity and worse VFL in the worse seeing eye, to have been diagnosed with an eye disease, and to have received specific eye disease treatment.
This population showed a very small but significant improvement in VF after 4 years in both the better (median difference [interquartile range] = 0.08 [1.8] dB, P =.04) and worse eye (0.01 [2.1] dB, P=0.03). Overall, 1430 (46%) showed a change in VF >1 dB in the better eye (loss=22%, gain= 24%) and 52% in the worse eye (loss=28%, gain=24%).
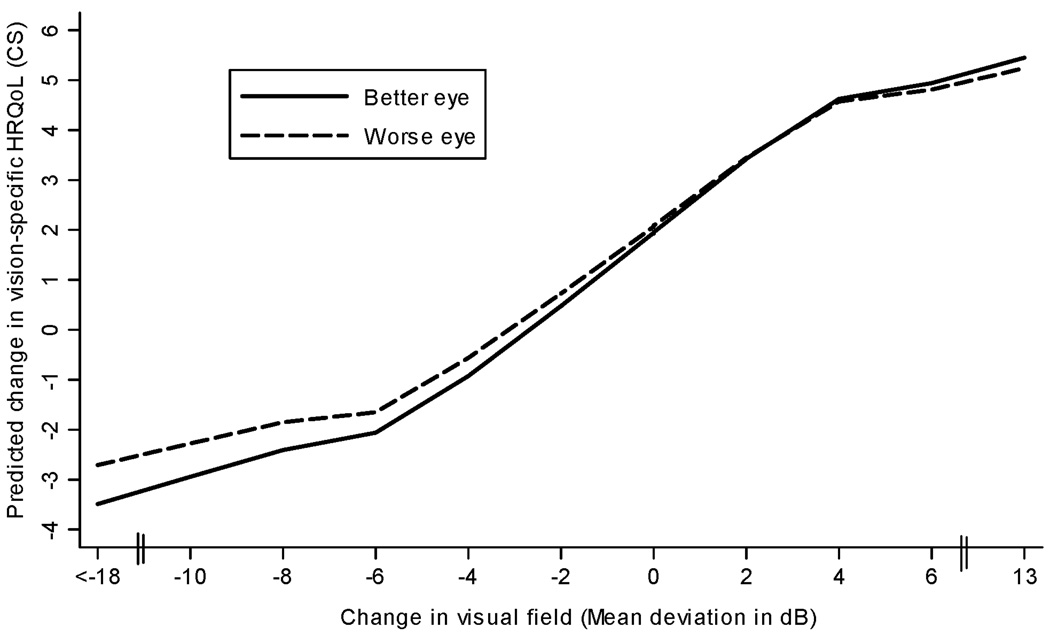
There was a small mean difference between better and worse eye change in VF (mean difference [SD] =0.18 dB [2.6], P=0.0001). Change in VF in the better and worse eye were linearly associated (Pearson’s correlation rho=0.72, P=<0.0001) and severity levels were in good agreement (agreement 68%, kappa=0.50, P<0.0001). LOWESS plots depicting the association between change in VF and vision-specific HRQoL were similar between the better and worse eye (Figure 1). Therefore, all remaining results are presented in the better eye.
Figure 1.
Locally weighted, least squares plot (LOWESS) depicting the relationship between change in visual field (mean deviation in decibels) and predicted change in vision-specific health related quality of life (HRQoL) in the better and worse seeing eye. Vision-specific HRQoL was measured using the National Eye Institute Visual Function Questionnaire-25 composite score (CS).
On average, there was a small loss in vision-specific HRQoL composite score (mean change; 95% confidence interval [CI] = −2.0; −2.1, −1.5, P<0.0001). Overall, 699 (22%) showed a ≥5 point loss and 1016 (32%) a ≥5 point gain in vision-specific HRQoL composite score.
A small loss in general HRQoL (SF-12) physical component score (mean change; 95% CI= −0.55; −0.87, −0.23, P =0.0008) and gain in the mental component score (mean change; 95%CI=1.6; 1.2,2.0, P <0.0001) were noted.
Association between 4-year change in VF and mean change in HRQoL
For the composite score and all vision specific subscales, except ocular pain, as change in VF transitioned from levels of greater loss (< −5.0 dB) to levels of greater gain (> 3.0 to 25 dB), average vision-specific HRQoL scores improved (all Ptrends<0.05) (Table 2). With progressive worsening of visual field loss the greatest losses were present in the driving, dependency, and role-function subscales. With improvement in the visual field, the greatest gains were present in role-function, peripheral vision, and mental health subscales. Change in VF was not associated with change in general HRQoL physical or mental summary component scores, based on the SF-12 instrument (both Ptrends>0.30).
Table 2.
Change in Health-Related Quality of Life Across Levels of Change in Visual Field, n=3175.
| Change in Visual Field (MD expressed in dB) | |||||||
|---|---|---|---|---|---|---|---|
| Worsened | Stable | Improved | |||||
| < −5.0 n=92 3% |
−5.0 to −3.1 n=91 3% |
−3.0 to −1.1 n=500 16% |
−1 to 1 n=1745 54% |
1.1 to 3 n=603 19% |
> 3.0 n=144 5% |
||
| Change in HRQoLa | |||||||
| mean (SD) | |||||||
| Ptrend | |||||||
| Vision-specific HRQoLb | |||||||
| Composite Scorec | −4.5 (17.5) | −.96 (14.1) | .85 (13.0) | 2.1 (11.4) | 2.9 (12.1) | 5.2 (15.7) | <.001 |
| General Vision | −6.1 (21.9) | 1.9 (18.3) | .32 (17.4) | .53 (18.2) | .96 (19.6) | 2.3 (18.1) | 0.01 |
| Near Vision | −2.1 (24.4) | 3.6 (20.4) | 1.8 (19.5) | 1.8 (20.1) | 3.4 (20.4) | 5.4 (21.7) | 0.04 |
| Distance Vision | −4.3 (21.8) | −2.5 (21.4) | −1.9 (17.6) | .02 (17.2) | .59 (19.2) | 3.9 (21.8) | 0.002 |
| Peripheral Vision | −2.4 (27.5) | 0.0 (25.5) | 2.4 (21.7) | 1.1 (19.2) | 3.3 (23.0) | 7.1 (24.1) | 0.002 |
| Color Vision | −2.4 (22.8) | −1.1 (20.7) | 1.1 (15.8) | .88 (15.1) | 1.7 (16.1) | 4.5 (21.2) | 0.01 |
| Ocular Pain | 3.2 (26.9) | 0.0 (23.3) | 2.7 (21.8) | 3.1 (19.7) | 3.1 (19.5) | 5.8 (24.5) | 0.45 |
| Driving Difficultiesd | −13.2 (29.6) | −4.4 (20.9) | −1.5 (16.9) | .16 (15.0) | .30 (15.1) | 2.4 (22.3) | <.001 |
| Dependency | −8.8 (30.5) | −3.7 (26.6) | 1.1 (21.0) | 3.4 (18.1) | 4.8 (18.1) | 3.4 (27.3) | <.001 |
| Mental Health | −5.6 (28.8) | −1.9 (26.4) | 1.1 (22.4) | 4.2 (20.3) | 4.6 (21.1) | 6.5 (27.8) | <.001 |
| Role Function | −7.6 (27.5) | −.41 (26.3) | 1.1 (23.7) | 2.1 (19.4) | 2.5 (21.6) | 8.2 (26.2) | <.001 |
| Social Function | −2.5 (22.9) | −1.5 (16.9) | 1.1 (16.4) | 1.2 (13.1) | 2.4 (15.4) | 4.4 (18.1) | 0.002 |
| General HRQoLe | |||||||
| PCS | −2.1 (11.3) | −1.1 (10.3) | −.19 (09.9) | −.68 (08.8) | −.18 (09.5) | −.33 (09.4) | 0.37 |
| MCS | 2.5 (13.9) | 1.9 (11.9) | .88 (12.6) | 1.5 (10.6) | 1.7 (11.5) | 2.4(11.7) | 0.59 |
Abbreviations: MD, mean deviation; dB, decibel; NEI VFQ-25, National Eye Institute Visual Function Questionnaire; HRQoL, health-related quality of life; SF-12, Medical Outcomes Study 12-Item Short-Form Health Survey; PCS, physical component summary; MCS, mental component summary.
Change: difference between 4-year follow-up and baseline HRQoL; negative values= worsened, positive values = improved.
Measured with NEI VFQ-25. General health sub-scale not included because general health was measured with SF-12.
Composite score : unweighted average of 24 of the 25 items (general health item not included).
Scores were generated for participants who reported that they were currently driving or had driven in the past, (n=2,279).
Measured with SF-12.
Minimal clinically important differences (MCID) in vision-specific HRQoL
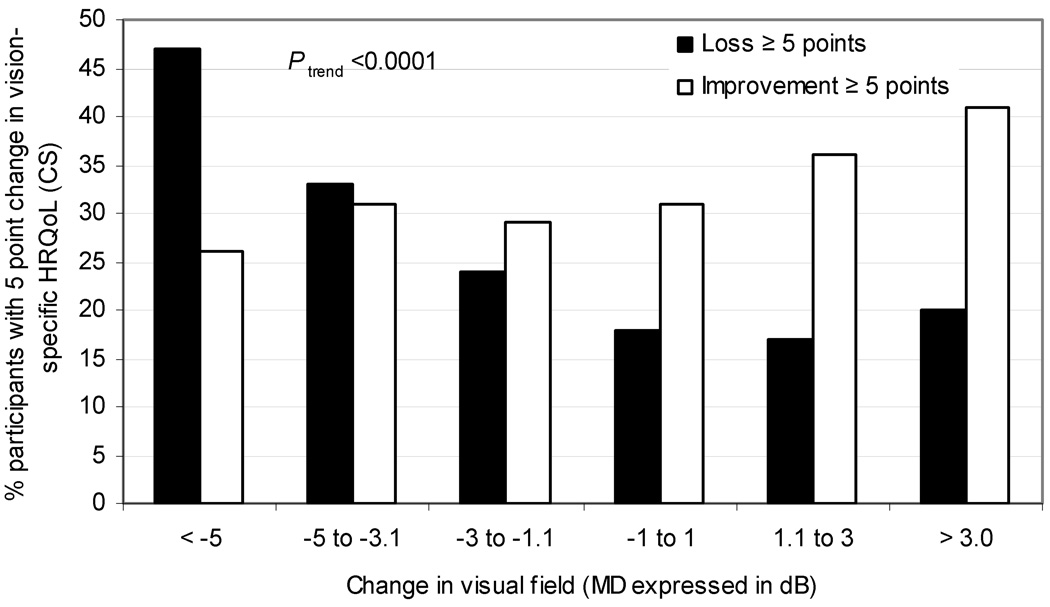
As expected, larger changes in VF (< −5 and > 3 db) were associated with MCID (≥ 5 points) for the composite score and most areas of vision-specific HRQoL (9 of 12 subscales). Certain areas of vision-specific HRQoL were sensitive to MCID with losses in visual field and others with gains in visual field. For example, only extreme losses in VF (> −5 dB) were associated with clinically meaningful changes for the driving difficulty subscale, while only gains (> 3db) in VF were associated with clinically meaningful changes in the peripheral vision subscale. Most importantly, smaller losses in VF (−5 to −3.0) approached MCID in the driving difficulty subscale [−4.4]; and smaller gains (1.1 to 3 db) approached MCID in the dependency [4.8] and mental health [4.6] subscales (see Table 1 available at http://aaojournal.org). However, some individuals experienced MCID in vision-specific HRQoL (loss or gain) across all levels of change in VF, Ptrend <0.0001, (Figure 2).
Figure 2.
Proportion of individuals with a ≥ 5 point change in vision-specific health related quality of life (HRQoL) composite score (CS) across decreasing levels of change in visual field (mean deviation in decibel). Vision-specific HRQoL was measured using the National Eye Institute Visual Function Questionnaire-25 CS. A five-point change in vision-specific HRQoL was considered a minimal clinically important difference.
The impact of visual field change on vision-specific quality of life across covariates
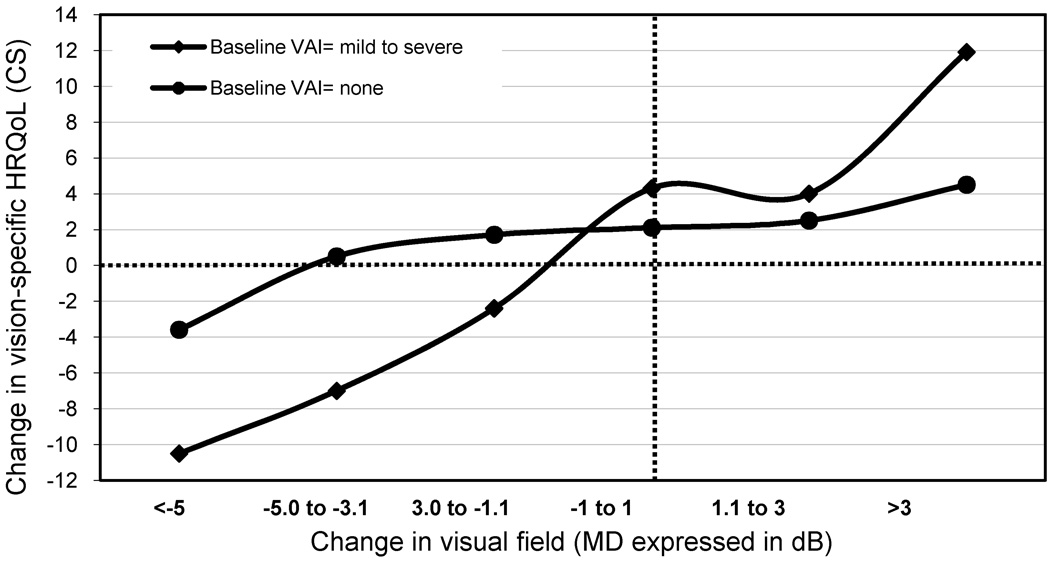
There was a statistically significant variation of the effect of losses in VF on losses in vision-specific HRQoL composite score across the following levels of covariates: (1) baseline visual field loss (moderate/severe vs. no visual field loss; P-interaction=0.0002), (2) baseline visual acuity impairment (mild/severe vs. no impairment; P-interaction=0.04), as illustrated in Figure 3, (3) change in visual acuity (≥ 2 line loss vs. no loss; P-interaction <0.0001), and (4) gender (males vs. females; P-interaction= 0.0002). No statistically significant interaction was found between change in VF and age (P-interaction=0.14).
Figure 3.
LOWESS plots depicting the relationship between change in vision-specific health related quality of life (HRQoL) across levels of mean change in visual field [Mean deviation (MD) expressed in decibels (dB)], by severity of impairment in baseline visual acuity (VAI). The figure shows that the effect of change in visual field on vision-specific HRQoL varies by levels of VAI (mild to severe vs. none). The crossing of lines suggests interaction between change in visual field and VAI on their effect in producing a change in vision-specific HRQoL. The intersection of the two broken lines (----) represents the point where there is no change in visual field and no change in vision-specific quality of life.
These effects were most evident with changes in visual field that were more extreme, for example losses in visual field > 5 dB produced greater losses in vision-specific HRQoL if the participants were visually impaired at baseline (visual field and visual acuity), if they experienced a 2 lines loss in visual acuity during the 4-year study period, or if the participants were male. For example, moderate/severe VF loss at baseline together with a > 5 dB mean loss in VF resulted in a mean loss of vision-specific HRQoL of 11.3 points, whereas no VF loss at baseline together with a > 5 dB mean loss in VF resulted in a mean loss of only −0.97 points in vision-specific HRQoL. Similarly, mild/severe baseline visual acuity impairment and a > 5 dB mean loss in VF resulted in a mean loss of vision-specific HRQoL of 10.5 points, whereas no visual acuity impairment at baseline and a > 5 db loss in VF resulted in a loss of vision-specific HRQoL of only 3.7 points.
Discussion
In this Latino adult, population-based cohort, changes in visual field (loss and gain) were associated with changes in vision-specific HRQoL. This linear trend was apparent for most subscales but was strongest for vision-related dependency, driving difficulties, peripheral vision, mental health, and role-function. The impact of VF loss on vision-specific HRQoL loss was most evident among those with pre-existing vision loss (in visual fields or central visual acuity).
During the 4-year follow-up, approximately half of the LALES population experienced a change in visual field (loss=22%, gain=24%). Plausible reasons for worsening in VF include the presence of eye diseases that may commonly produce visual field loss, such as cataract, glaucoma, diabetic macular edema, neovascular macular degeneration; while specific treatment for cataract (lens extraction), macular edema (laser and anti-VEGF injections), neovascular macular degeneration (injections of anti-VEGF drugs) most likely explain improvement in VF. Overall, 35% of the cohort was diagnosed with at least one of these eye disease at baseline, and the prevalence varied by whether there was a loss or gain in visual field (loss=48.2%, gain=31.7%, no change=31.4%). Additionally, 4.6% reported receiving at least one eye disease-specific treatment (loss=8.4%, gain=4.2%, no change=3.4%) in the past 4 years which could explain, in part, why some individuals had an improvement in visual fields.
These longitudinal results further support previous cross-sectional findings showing a positive linear association between VFL and loss in vision-specific HRQoL.7–9, 35–37 The present results are also consistent with earlier studies showing that all-cause7 and disease-specific38,39 VFL significantly affects most areas of vision-specific HRQoL. We do not show effects of change in VF on general HRQoL, unlike an earlier study from the LALES population.7 This previous cross-sectional study evaluated baseline inter-individual differences in VF, while the current study measures intra-individual change. Therefore, it is possible that the LALES population did not experience a large enough change in VF to impact change in general HRQoL during the 4-year study period. This is consistent with a clinical trial showing a positive association between vision restoration training and gains in vision-specific but not general HRQoL.36
Individuals with VFL commonly report difficulties in completing important daily tasks such as reading,40 walking and maintaining their balance,41 and driving.42 In this study, losses in VF had a strong effect on driving (i.e., driving in difficult conditions), dependency (i.e., dependency on others to get things done), role-functioning (i.e., endurance), and mental health (i.e., feeling frustrated because of eye sight). While we are not aware of other observational cohort studies evaluating the effect of change in VF on different aspects of change in vision-specific HRQoL, these results are in agreement with previous cross-sectional studies.7, 9, 4We were interested in determining the amount of change in VF needed to produce a MCID43 in vision-specific HRQoL since statistically significant differences are not always equivalent to clinically important ones. The MCID for HRQoL has been defined as a difference large enough to have an implication for the patient’s treatment, care, and/or disease monitoring.44 The data suggest that losses greater than 5 dB and gains greater than 3 dB are necessary to produce MCID in vision-specific HRQoL. These results are consistent with reports from other areas of HRQoL research, indicating that the magnitude of change in HRQoL can vary by the direction of change in the exposure.45–47 Importantly, the data also show that some areas of vision-related HRQoL (driving difficulties, dependency, and mental health) were sensitive to smaller changes in VF, which addresses the issue of understanding how severe visual loss must be before disability is first detected.48 These results can be used by clinicians to inform treatment decisions for patients with progressive VFL.
Our findings show that the presence of pre-existing visual field loss, worsening in visual acuity over the 4-year study period, and male gender increase the impact of visual field loss on worsening in vision-specific HRQoL. Mean declines in HRQoL were greater among individuals who experienced visual field loss with the above-mentioned covariates than what would be expected based only on additive effects, thus suggesting interaction. The underlying mechanisms explaining these joint effects on HRQoL need further study.
Although the most common and best understood application of health related quality of life measures has been in the context of clinical trials, it has been advocated as a useful measure in the clinical setting.49 The ultimate goal of using such measures in the clinic is to focus on the patient’s perception of the impact of a disease and its treatment on specific areas of HRQoL, as well as on the disease itself. Examples of how HRQoL could be used in the clinical setting include facilitating patient-provider communication, prioritizing health problems, identifying patient preferences for treatment and monitoring changes or response to treatment.50 The challenge of using HRQoL measures during the clinical encounter has been the general lack of training received by undergraduate and postgraduate students on how to use them and on how to interpret the results50; as well as finding user-friendly ways to incorporate them into a busy clinical practice.50 More importantly, while some clinical trials in ophthalmology have utilized measures of HRQoL, rarely have they been used in clinical practice, and thus their utility in patient management using an evidence-based approach has not been well established. 50 The results of this study strongly suggest that change (both worsening and improvement) in the visual field impacts vision specific HRQoL and support the use of this measure as an aid for clinicians in the management of patients with eye diseases (such as cataract, glaucoma) that impact the visual field.
Strengths of this study include objective measurements of vision, large number of participants with clinically important changes (≥5 points) in vision-specific HRQoL assuring stability in multivariable models, and assessing the effect of both losses and gains in VF on HRQoL. Although HRQoL is a self-reported outcome subject to measurement error, we used validated measures of HRQoL that have been evaluated in different racial/ethnic groups, including Latinos. 26, 46, 47, 51,52 We tested for the confounding effects by all covariates measured at baseline and found than none changed the effect of VF on quality of life by more than 10% and thus were not included in the final model. Limitations include having only one measure of change in VF (at 4-year follow-up); therefore, transient forms of VFL could not be distinguished from permanent forms. Since visual field fluctuations of 3 dB or more at a single time point could occur because of temporary ophthalmic conditions, such as cataract development and extraction, it is important to make these distinctions.24 After the 8-year follow-up visit of LALES is completed this issue will be better addressed. Other sources of visual impairment, such as depth perception, contrast sensitivity and location of visual field loss, were not included in this analysis but may also have contributed to changes in HRQoL. Lastly, results of the impact of change in VF on HRQoL are reported only in the better eye. While VF data was collected for both eyes, the results for the better eye were highly correlated with the worse eye and the results for the better eye had a slightly stronger effect on vision-specific HRQoL, consistent with a previous study.30 Although the effect of monocular change in visual field on HRQoL may have been over or underestimated by not having evaluated binocular changes,53,54 cross-sectional results from the LALES population revealed no statistically significant differences between monocular and binocular visual field loss on HRQoL, (Aghaian, E. Visual Field Loss and Health Related Quality of Life. Invest Ophthalmol Vis Sci, 2007, 48, ARVO E-Abstract, 4329). Although a future analysis will include binocular change in VF for the LALES population,48 binocular fields are not readily available in clinical practice and their utility as a metric for disability has not been well established.45, 49
In summary, changes in VF over time are associated with clinically important changes in vision-specific HRQoL in a population-based sample. The impact of this effect on certain areas of quality of life depended on whether visual field worsened or improved. Finally, the impact of progressive visual field loss was greater depending on the presence and level of pre-existing visual field loss and impairment of visual acuity. Finally, these results are important because they can inform both public policy for the development of community-based screening and prevention programs and individual physicians and their patients when managing conditions that are associated with progressive reversible (e.g., cataract) and irreversible (e.g., glaucoma) visual field loss.
Supplementary Material
Acknowledgments
Financial Support: National Institutes of Health Grants NEI U10-EY-11753 and EY-03040 and an unrestricted grant from the Research to Prevent Blindness, New York, NY, and Pfizer Inc. Rohit Varma is a Research to Prevent Blindness Sybil B. Harrington Scholar. The sponsors or funding organizations had no role in the design or conduct of this research.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
See Appendix for members of the Los Angeles Latino Eye Study Group
Meeting presentation: partial results from this manuscript were presented at the 2010 Association for Research and Vision (ARVO) annual meeting, Ft. Lauderdale, Florida on May 6, 2010.
Financial Disclosure: The authors have no proprietary or commercial interest in any materials discussed in the manuscript.
References
- 1.World Health Organization. Visual impairment and blindness. [Accessed March 15, 2010];2009 May; Fact sheet no. 282.. Available at: www.who.int/mediacentre/factsheets/fs282/en/print.html.
- 2.Bailey RN, Indian RW, Zhang X, et al. Centers for Disease Control and Prevention. Visual impairment and eye care among older adults-five states, 2005. MMWR Morb Mortal Wkly Rep. 2006;55:1321–1325. [PubMed] [Google Scholar]
- 3.McNeil JM, Binette J. Prevalence of disabilities and associated health conditions among adults--United States, 1999. MMWR Morb Mortal Wkly Rep. 2001;50:120–125. [PubMed] [Google Scholar]
- 4.Centers for Disease Control and Prevention. Vision Health Initiative (VHI) [Accessed March 15, 2010]; Available at: http://www.cdc.gov/visionhealth/
- 5.Agency for Healthcare Research and Quality. Vision rehabilitation: care and benefit plan models. [Accessed March 15, 2010]; Available at: http://www.ahrq.gov/clinic/vision/vision1.htm#definitionandgoals.
- 6.Ivers RQ, Mitchell P, Cumming RG. Visual function tests, eye disease and symptoms of visual disability: a population-based assessment. Clin Experiment Ophthalmol. 2000;28:41–47. doi: 10.1046/j.1442-9071.2000.00236.x. [DOI] [PubMed] [Google Scholar]
- 7.McKean-Cowdin R, Varma R, Wu J, et al. Los Angeles Latino Eye Study Group. Severity of visual field loss and health-related quality of life. Am J Ophthalmol. 2007;143:1013–1023. doi: 10.1016/j.ajo.2007.02.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Freeman EE, Munoz B, West SK, et al. Glaucoma and quality of life: the Salisbury Eye Evaluation. Ophthalmology. 2008;115:233–238. doi: 10.1016/j.ophtha.2007.04.050. [DOI] [PubMed] [Google Scholar]
- 9.McKean-Cowdin R, Wang Y, Wu J, et al. Los Angeles Latino Eye Study Group. Impact of visual field loss on health-related quality of life in glaucoma: the Los Angeles Latino Eye Study. Ophthalmology. 2008;115:941–948. doi: 10.1016/j.ophtha.2007.08.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mills RP, Janz NK, Wren PA, Guire KE CIGTS Study Group. Correlation of visual field with quality-of-life measures at diagnosis in the Collaborative Initial Glaucoma Treatment Study (CIGTS) J Glaucoma. 2001;10:192–198. doi: 10.1097/00061198-200106000-00008. [DOI] [PubMed] [Google Scholar]
- 11.Patino CM, McKean-Cowdin R, Azen SP, et al. Los Angeles Latino Eye Study Group. Central and peripheral visual impairment and the risk of falls and falls with injury. Ophthalmology. 2010;117:199–206. doi: 10.1016/j.ophtha.2009.06.063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.McGwin G, Jr, Xie A, Mays A, et al. Visual field defects and the risk of motor vehicle collisions among patients with glaucoma. Invest Ophthalmol Vis Sci. 2005;46:4437–4441. doi: 10.1167/iovs.05-0750. [DOI] [PubMed] [Google Scholar]
- 13.Ang GS, Eke T. Lifetime visual prognosis for patients with primary open-angle glaucoma. Eye (Lond) 2007;21:604–608. doi: 10.1038/sj.eye.6702284. [DOI] [PubMed] [Google Scholar]
- 14.Freeman EE, Gange SJ, Munoz B, West SK. Driving status and risk of entry into long-term care in older adults. Am J Public Health. 2006;96:1254–1259. doi: 10.2105/AJPH.2005.069146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lee DJ, Gomez-Marin O, Lam BL, Zheng DD. Glaucoma and survival: the National Health Interview Survey 1986–1994. Ophthalmology. 2003;110:1476–1483. doi: 10.1016/S0161-6420(03)00408-1. [DOI] [PubMed] [Google Scholar]
- 16.Lee DJ, Gomez-Marin O, Lam BL, Zheng DD. Visual impairment and unintentional injury mortality: the National Health Interview Survey 1986–1994. Am J Ophthalmol. 2003;136:1152–1154. doi: 10.1016/s0002-9394(03)00573-7. [DOI] [PubMed] [Google Scholar]
- 17.Varma R, Paz SH, Azen SP, et al. Los Angeles Latino Eye Study Group. The Los Angeles Latino Eye Study: design, methods, and baseline data. Ophthalmology. 2004;111:1121–1131. doi: 10.1016/j.ophtha.2004.02.001. [DOI] [PubMed] [Google Scholar]
- 18.Linn BS, Linn MW, Gurel L. Cumulative illness rating scale. J Am Geriatr Soc. 1968;16:622–626. doi: 10.1111/j.1532-5415.1968.tb02103.x. [DOI] [PubMed] [Google Scholar]
- 19.Solis JM, Marks G, Garcia M, Shelton D. Acculturation, access to care, and use of preventive services by Hispanics: finding from HHANES 1982–84. Am J Public Health. 1990;80 suppl:11–19. doi: 10.2105/ajph.80.suppl.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Marks G, Garcia M, Solis JM. Health risk behaviors of Hispanics in the United States: findings from HHANES, 1982–84. Am J Public Health. 1990;80 suppl:20–26. doi: 10.2105/ajph.80.suppl.20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cuellar I, Harris LC, Jasso R. An acculturation scale for Mexican American normal and clinical populations. Hisp J Behav Sci. 1980;2:199–217. [Google Scholar]
- 22.Gillespie BW, Musch DC, Guire KE, et al. CIGTS Study Group. The Collaborative Initial Glaucoma Treatment Study: baseline visual field and test-retest variability. Invest Ophthalmol Vis Sci. 2003;44:2613–2620. doi: 10.1167/iovs.02-0543. [DOI] [PubMed] [Google Scholar]
- 23.Cello KE, Nelson-Quigg JM, Johnson CA. Frequency doubling technology perimetry for detection of glaucomatous visual field loss. Am J Ophthalmol. 2000;129:314–322. doi: 10.1016/s0002-9394(99)00414-6. [DOI] [PubMed] [Google Scholar]
- 24.Musch DC, Gillespie BW, Lichter PR, et al. CIGTS Study Investigators. Visual field progression in the Collaborative Initial Glaucoma Treatment Study: the impact of treatment and other baseline factors. Ophthalmology. 2009;116:200–207. doi: 10.1016/j.ophtha.2008.08.051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Strouthidis NG, Scott A, Viswanathan AC, et al. Monitoring glaucomatous visual field progression: the effect of a novel spatial filter. Invest Ophthalmol Vis Sci. 2007;48:251–257. doi: 10.1167/iovs.06-0576. [DOI] [PubMed] [Google Scholar]
- 26.Globe DR, Wu J, Azen SP, et al. Los Angeles Latino Eye Study Group. The impact of visual impairment on self-reported visual functioning in Latinos: the Los Angeles Latino Eye Study. Ophthalmology. 2004;111:1141–1149. doi: 10.1016/j.ophtha.2004.02.003. [DOI] [PubMed] [Google Scholar]
- 27.Varma R, Wu J, Chong K, et al. Los Angeles Latino Eye Study Group. Impact of severity and bilaterality of visual impairment on health-related quality of life. Ophthalmology. 2006;113:1846–1853. doi: 10.1016/j.ophtha.2006.04.028. [DOI] [PubMed] [Google Scholar]
- 28.Ware J, Jr, Kosinski M, Keller SD. A 12-item short-form health survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34:220–233. doi: 10.1097/00005650-199603000-00003. [DOI] [PubMed] [Google Scholar]
- 29.Ware JE, Jr, Kosinski M, Keller SD. SF-12: How to Score the SF-12 Physical and Mental Health Summary Scales. 2nd ed. Boston, MA: New England Medical Center Hospital Health Institute; 1995. pp. 21–28. [Google Scholar]
- 30.Mangione CM, Lee PP, Gutierrez PR, et al. National Eye Institute Visual Function Questionnaire Field Test Investigators. Development of the 25-item National Eye Institute Visual Function Questionnaire. Arch Ophthalmol. 2001;119:1050–1058. doi: 10.1001/archopht.119.7.1050. [DOI] [PubMed] [Google Scholar]
- 31.Mangione CM, Lee PP, Pitts J, et al. NEI-VFQ Field Test Investigators. Psychometric properties of the National Eye Institute Visual Function Questionnaire (NEI-VFQ) Arch Ophthalmol. 1998;116:1496–1504. doi: 10.1001/archopht.116.11.1496. [DOI] [PubMed] [Google Scholar]
- 32.Cleveland WS. Robust locally weighted regression and smoothing scatterplots. J Am Stat Assoc. 1979;74:829–836. [Google Scholar]
- 33.Hosmer DW, Jr, Lemeshow S. Applied Logistic Regression. 2nd ed. New York: Wiley; 2000. pp. 189–216. [Google Scholar]
- 34.Varma R, Chung J, Foong AW, et al. Los Angeles Latino Eye Study Group. Four-year incidence and progression of visual impairment in Latinos: the Los Angeles Latino Eye Study. Am J Ophthalmology. 2010;149:713–727. doi: 10.1016/j.ajo.2009.12.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Gutierrez P, Wilson MR, Johnson C, et al. Influence of glaucomatous visual field loss on health-related quality of life. Arch Ophthalmol. 1997;115:777–784. doi: 10.1001/archopht.1997.01100150779014. [DOI] [PubMed] [Google Scholar]
- 36.Gall C, Mueller I, Gudlin J, et al. Vision- and health-related quality of life before and after vision restoration training in cerebrally damaged patients. Restor Neurol Neurosci. 2008;26:341–353. [PubMed] [Google Scholar]
- 37.Rubin GS, Bandeen-Roche K, Huang GH, et al. SEE Project Team. The association of multiple visual impairments with self-reported visual disability: SEE Project. Invest Ophthalmol Vis Sci. 2001;42:64–72. [PubMed] [Google Scholar]
- 38.Gall C, Lucklum J, Sabel BA, Franke GH. Vision- and health-related quality of life in patients with visual field loss after postchiasmatic lesions. Invest Ophthalmol Vis Sci. 2009;50:2765–2776. doi: 10.1167/iovs.08-2519. [DOI] [PubMed] [Google Scholar]
- 39.Parrish RK, II, Gedde SJ, Scott IU, et al. Visual function and quality of life among patients with glaucoma. Arch Ophthalmol. 1997;115:1447–1455. doi: 10.1001/archopht.1997.01100160617016. [DOI] [PubMed] [Google Scholar]
- 40.Nelson P, Aspinall P, O'Brien C. Patients' perception of visual impairment in glaucoma: a pilot study. Br J Ophthalmol. 1999;83:546–552. doi: 10.1136/bjo.83.5.546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Geruschat DR, Turano KA. Estimating the amount of mental effort required for independent mobility: persons with glaucoma. Invest Ophthalmol Vis Sci. 2007;48:3988–3994. doi: 10.1167/iovs.06-1193. [DOI] [PubMed] [Google Scholar]
- 42.Haymes SA, LeBlanc RP, Nicolela MT, et al. Glaucoma and on-road driving performance. Invest Ophthalmol Vis Sci. 2008;49:3035–3041. doi: 10.1167/iovs.07-1609. [DOI] [PubMed] [Google Scholar]
- 43.Jaeschke R, Singer J, Guyatt GH. Measurement of health status: ascertaining the minimal clinically important difference. Control Clin Trials. 1989;10:407–415. doi: 10.1016/0197-2456(89)90005-6. [DOI] [PubMed] [Google Scholar]
- 44.Wyrwich KW, Bullinger M, Aaronson N, et al. Clinical Significance Consensus Meeting Group. Estimating clinically significant differences in quality of life outcomes. Qual Life Res. 2005;14:285–295. doi: 10.1007/s11136-004-0705-2. [DOI] [PubMed] [Google Scholar]
- 45.Cella D, Hahn EA, Dineen K. Meaningful change in cancer-specific quality of life scores: differences between improvement and worsening. Qual Life Res. 2002;11:207–221. doi: 10.1023/a:1015276414526. [DOI] [PubMed] [Google Scholar]
- 46.D'Antonio LL, Zimmerman GJ, Cella DF, Long SA. Quality of life and functional status measures in patients with head and neck cancer. Arch Otolaryngol Head Neck Surg. 1996;122:482–487. doi: 10.1001/archotol.1996.01890170018005. [DOI] [PubMed] [Google Scholar]
- 47.Wells GA, Tugwell P, Kraag GR, et al. Minimum important difference between patients with rheumatoid arthritis: the patient's perspective. J Rheumatol. 1993;20:557–560. [PubMed] [Google Scholar]
- 48.Ramulu P. Glaucoma and disability: which tasks are affected, and at what stage of disease? Curr Opin Ophthalmol. 2009;20:92–98. doi: 10.1097/ICU.0b013e32832401a9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Higginson IJ, Carr AJ. Measuring quality of life: using quality of life measures in the clinical setting. BMJ. 2001;322:1297–1300. doi: 10.1136/bmj.322.7297.1297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Fitzpatrick R, Fletcher A, Gore S, et al. Quality of life measures in health care. I: Applications and issues in assessment. BMJ. 1992;305:1074–1077. doi: 10.1136/bmj.305.6861.1074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Baker RS, Bazargan M, Calderon JL, Hays RD. Psychometric performance of the National Eye Institute Visual Function Questionnaire in Latinos and non-Latinos. Ophthalmology. 2006;113:1363–1371. doi: 10.1016/j.ophtha.2006.01.073. [DOI] [PubMed] [Google Scholar]
- 52.Broman AT, Munoz B, Rodriguez J, et al. The impact of visual impairment and eye disease on vision-related quality of life in a Mexican-American population: Proyecto VER. Invest Ophthalmol Vis Sci. 2002;43:3393–3398. [PubMed] [Google Scholar]
- 53.Nelson-Quigg JM, Cello K, Johnson CA. Predicting binocular visual field sensitivity from monocular visual field results. Invest Ophthalmol Vis Sci. 2000;41:2212–2221. [PubMed] [Google Scholar]
- 54.Jampel HD, Friedman DS, Quigley H, Miller R. Correlation of the binocular visual field with patient assessment of vision. Invest Ophthalmol Vis Sci. 2002;43:1059–1067. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.