Abstract
Contact hypersensitivity (CHS) is a delayed-type hypersensitivity that can be induced by haptens, such as 2,4-dinitrofluorobenzene (DNFB). Innate and adaptive immunities are both important for the development of CHS. To treat CHS-related diseases, such as allergic contact dermatitis, a disease prevalent in industrialized countries, ways of interfering with improper immune function during CHS responses need to be identified. Transforming growth factor-β-activated kinase-1 (TAK1), a member of mitogen-activated protein kinase kinase kinase family, is important for both innate and adaptive immunities. We thus hypothesized that the CHS response could be inhibited by interfering with TAK1 activity. Using a mouse model in which TAK1 deletion can be locally induced, we observed that TAK deficiency led to an impaired CHS response and was associated with defective T-cell expansion, activation and interferon (IFN)-γ production. In addition, we investigated the effect of deleting TAK1 specifically in dendritic cells (DC) on the CHS response. We found that when TAK1 is deficient in DC, the CHS response was abolished and hapten-elicited T-cell responses were defective. Collectively, this study demonstrates an essential role of TAK1 in the induction of CHS and suggests that targeting TAK1 could be a viable approach to treat CHS.
Keywords: CHS; DC; 2,4-dinitrofluorobenzene (DNFB); TAK1
Introduction
Allergic contact dermatitis is one of the most common occupational diseases in industrialized countries, and it has large socioeconomic impact.1, 2 Knowledge of the pathophysiology of human allergic contact dermatitis has been obtained mainly from studies using murine models of contact hypersensitivity (CHS) to strong haptens, such as 2,4-dinitrofluorobenzene (DNFB). With a single contact, DNFB is able to elicit a CHS response in the skin. In mouse models, CHS is induced in two phases.3 The first phase is the sensitization phase that is induced by painting a small area of abdominal or back skin with a hapten. During the sensitization phase, a hapten binds to endogenous proteins in the skin, alters the antigenicity of these proteins and activates professional antigen-presenting dendritic cells (DC) residing in the skin. Proteins with newly arisen antigenic specificities are processed by epidermal DCs, Langerhans cells and dermal DCs.4, 5 Activated hapten-bearing DCs migrate to the draining lymph nodes (DLN), where antigen-specific CD4 and CD8 T cells are primed.6 The second phase in the development of CHS is the elicitation phase, which is induced by epicutaneous hapten challenge 5 days after the initiation phase at a previously unexposed site, usually the ear skin. In this phase, T lymphocytes that were previously primed during the initiation phase are activated in the dermis and the epidermis in response to the challenge; they trigger an inflammatory process through interferon (IFN)-γ production and cytotoxicity toward keratinocytes.7, 8 Both DCs and T cells play critical roles in the development of CHS. Therefore, efficient ways of inhibiting DC and T-cell function to treat CHS need to be developed.
Transforming growth factor-β-activated kinase-1 (TAK1) is a serine/threonine kinase belonging to the mitogen-activated protein kinase kinase kinase family. Various stimuli can activate TAK1.9, 10 Once activated, TAK1 promotes downstream signaling molecules including NF-κB,11, 12 c-Jun N-terminal kinase MAPK and p38 MAPK.13 TAK1 is essential to control the survival, differentiation and function of innate and adaptive immune cells and thus also has an effect on related responses.9, 12, 14 Therefore, we hypothesize that we can inhibit the CHS response by interfering with TAK1 function.
In this study, we tested this hypothesis by disrupting TAK1 function both locally and specifically in DCs. We demonstrated that normal function of TAK1 during the initiation phase is required for the CHS response and corresponding T-cell activation, expansion and effector function. In addition, we showed that inhibiting TAK1 function specifically in DC is critical for the development of CHS and T-cell activation. Therefore, we have provided evidence that TAK1 is essential for the CHS response and that local or DC-specific targeting of TAK1 may be a viable approach to treat CHS and related delayed-type hypersensitivity diseases.
Materials and methods
Mice
TAK1fl/fl has been described previously.12 CD11c-Cre mice were kindly provided by B. Reizis (Columbia University, New York, USA). ER-Cre mice were kindly provided by T. Ludwig (Columbia University). All mice were on a C57BL/6 background and were kept under specific pathogen-free conditions in the animal care facility at the University of North Carolina at Chapel Hill. All mouse experiments were approved by the Institutional Animal Care and Use Committee of the University of North Carolina at Chapel Hill.
Hapten sensitization and elicitation of CHS
Mice were sensitized to DNFB (Sigma-Aldrich, St Louis, MO, USA) on day 1 by applying 25 µl 0.5% DNFB topically on dehaired back skin (sensitization phase). On day 6, sensitized mice were challenged topically with 10 µl 0.25% DNFB on the left ear (elicitation phase). To delete the TAK1 gene in ER-TAK1fl/fl mice, 50 µg tamoxifen (Sigma-Aldrich) was painted together with DNFB solution during the sensitization phase. Ear thickness was assessed with an electronic digital caliper (VWR, Radnor, PA, USA) before challenge and 48 h after challenge. The degree of the CHS response was determined by the increase in ear thickness 48 hours post-challenge.
Staining for surface markers and Foxp3
Lymphocytes were isolated from the auricular DLN. Various surface markers and intracellular Foxp3 were stained with cocktails of fluorescence-conjugated antibodies according to the manufacturer's protocols (eBioscience, San Diego, CA, USA).
Stimulation of cytokine production and intracellular cytokine staining
Lymphocytes were isolated from DLN and stimulated with 50 ng/ml phorbol myristate acetate (Sigma-Aldrich) and 1 µM of ionomycin (Sigma-Aldrich) for 4 h in the presence of 2 µg/ml Brefeldin A (Sigma-Aldrich). The cells were stimulated in Bruff's T-cell medium (Sigma-Aldrich) supplemented with 10% fetal bovine serum and 1% penicillin/streptomycin under typical cell culture conditions (37 °C, 5% CO2). Different surface markers and intracellular cytokines were stained with cocktails of fluorescence-conjugated antibodies as per the manufacturer's protocols (BD Bioscience, San Jose, CA, USA).
Flow cytometry analysis
Fluorescence-conjugated antibodies, including CD4-Pacific blue, CD8-PE-CY7, CD44-FITC, IFN-γ-FITC, IL-4-APC, CD62L-APC, Foxp3-PE and IL-17-PE, were purchased from eBioscience. Flow cytometry analysis of labeled cells was performed on an LSRII (Becton Dickinson, San Jose, CA, USA) or a CyAn (Beckman Coulter; Dako Cytomation, Fort Collins, CO, USA).
Statistical analysis
Data from at least three sets of samples were used for statistical analysis. Statistical significance was calculated by Student's t-test. A P value of less than 0.05 was considered significant.
Results
Local disruption of TAK1 inhibited the development of CHS
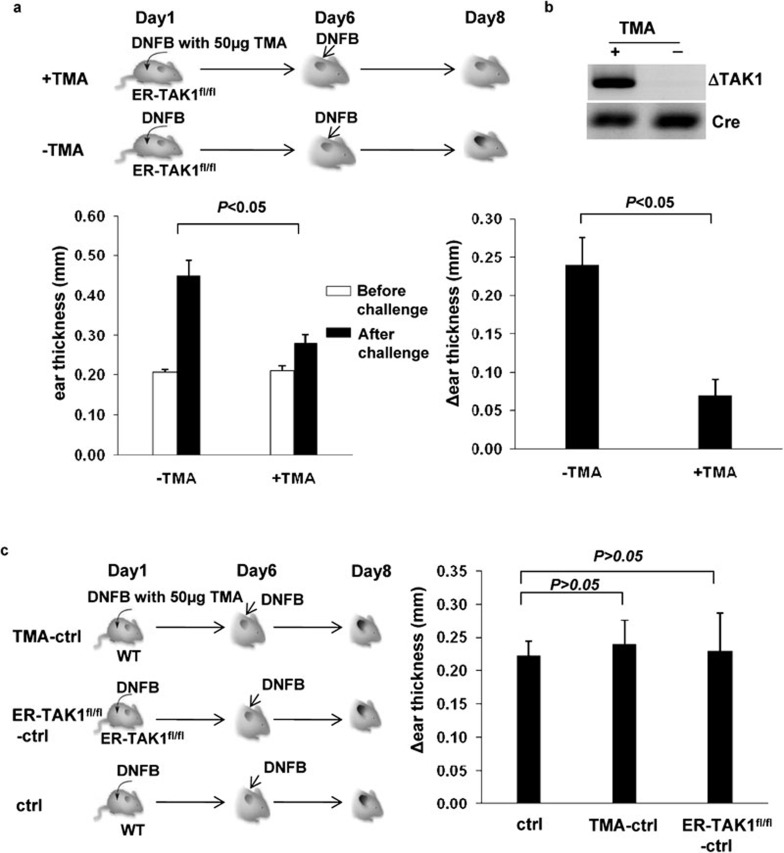
While TAK1 has been shown to be important for the generation and function of various cell types mediating innate and adaptive immunity,15 its role in the development of inflammatory diseases remains poorly understood. We hypothesized that TAK1 is critical in the development of the CHS response and that this response can be inhibited by interfering with TAK1 function. We thus investigated whether TAK1 is required for CHS induction by DNFB. We crossed mice bearing loxP-flanked TAK1 alleles12 with ER-Cre mice to generate ER-TAK1fl/fl mice. In ER-Cre mice, constitutively expressed Cre protein is activated only when tamoxifen is provided.16 Therefore, we can induce deletion of TAK1 in ER-TAK1fl/fl mice at any time by providing tamoxifen as described previously.17 We topically applied DNFB mixed with 50 µg tamoxifen to the dehaired back of ER-TAK1fl/fl mice to delete TAK1 during the sensitization phase of the CHS response (Figure 1a, top panel). Following DNFB treatment on the ear skin in the elicitation phase, a CHS response was elicited, and the degree of the response was assessed by measuring ear thickness. In response to this treatment, the ear thickness of mock-treated ER-TAK1fl/fl mice increased substantially, indicating severe skin inflammation. By contrast, the ears of tamoxifen-treated ER-TAK1fl/fl mice failed to swell (Figure 1a, lower panel). TAK1 deletion was detected in the skin of ER-TAKfl/fl mice treated with tamoxifen but not those treated with vehicle alone (Figure 1b). Therefore, local disruption of TAK1 during the initiation phase inhibited the development of CHS.
Figure 1.
Defective CHS response to DNFB in TMA-treated ER-TAK1fl/fl mice. (a) On day 1, ER-TAK1fl/fl mice were painted with DNFB mixed with (+) or without (−) TMA on their dehaired back skin. Mice were challenged with DNFB on the left ear skin on day 6. Ear thickness was measured before (open bar) and 48 h after (solid bar) the challenge and plotted (lower left panel). The changes in ear thickness (Δ ear thickness) were also calculated and plotted (lower right panel). Mean±SD values of four mice are shown, and the P value is indicated. (b) ER-TAK1fl/fl mice were painted with TMA (+) or not (−). The painted skin were excised and subjected to PCR analysis for TAK-deleted alleles (ΔTAK1) and Cre (served as internal control). (c) A CHS response was induced in indicated mouse strains with or without TMA as shown in the scheme (left panel). The ear thickness was measured before and after challenge as described in (a), and Δ ear thickness was calculated and plotted (right panel). Mean±SD values of three mice are shown, and the P value is indicated. CHS, contact hypersensitivity; DNFB, 2,4-dinitrofluorobenzene; TAK1, transforming growth factor-β-activated kinase-1; TMA, tamoxifen.
To confirm that the above finding was not due to a defect in the ER-TAK1fl/fl mouse itself or tamoxifen application, we elicited a DNFB-induced CHS response in ER-TAK1fl/fl mice without tamoxifen treatment and in wild-type mice with or without tamoxifen treatment. DNFB efficiently induced a CHS response in both ER-TAK1fl/fl mice and wild-type mice treated with tamoxifen (Figure 1c). Therefore, the defective CHS response observed in tamoxifen-treated ER-TAK1fl/fl mice resulted from the TAK1 deficiency.
T-cell activation, expansion and effector function require intact TAK1 during CHS response
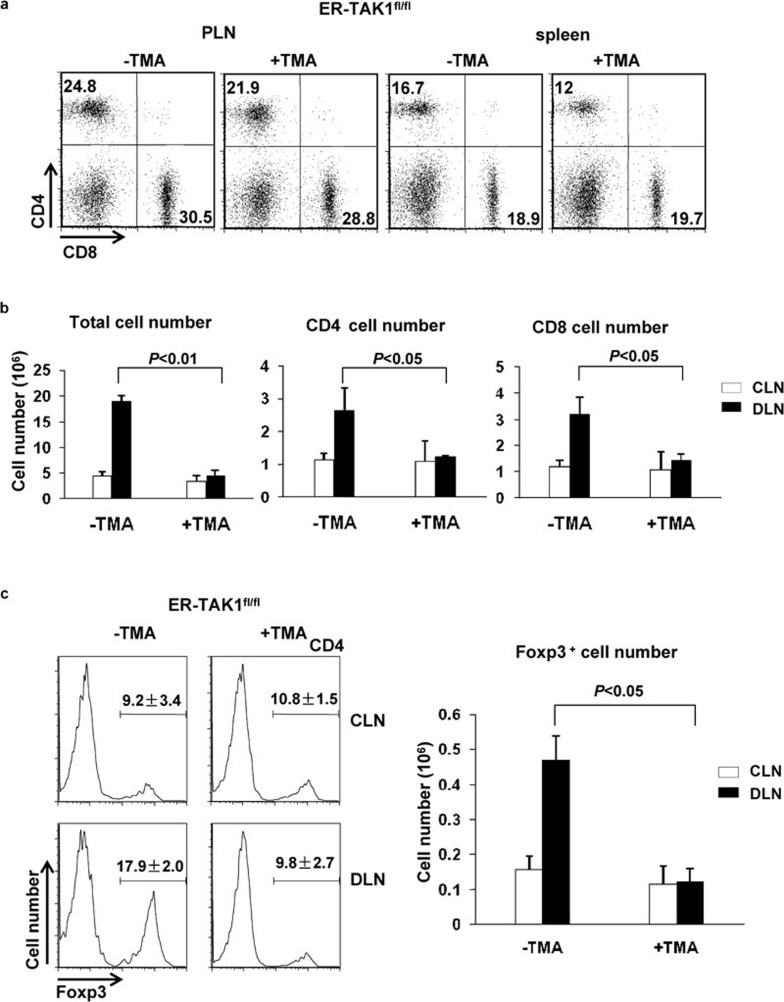
To elucidate the cellular mechanisms underlying the requirement of TAK1 for a CHS response, we investigated whether T-cell function was affected, as T cells are known to be the critical cell type mediating the CHS response.18 There was no significant difference in the percentages of CD4 and CD8 T cells from peripheral lymph nodes and spleens between tamoxifen and mock-treated ER-TAK1fl/fl mice, suggesting that application of 50 µg tamoxifen on skin did not cause general defect in T-cell numbers (Figure 2a). Auricular lymph nodes of both draining side (DLN) and non-draining side (control lymph node (CLN)) for DNFB-treated ears were collected, and the numbers of total lymphocytes in these lymph nodes were determined. The numbers of total lymphocytes, CD4 and CD8 T cells in CLN did not change upon DNFB treatment in both tamoxifen-treated and non-tamoxifen-treated ER-TAK1fl/fl mice (Figure 2b). However, the numbers of total lymphocytes, CD4 and CD8 T cells in DLN for DNFB-treated mice were increased compared with those in non-DNFB-treated ER-TAK1fl/fl mice (Figure 2b), consistent with the observed ear inflammation and swelling. By contrast, such an increase did not occur in tamoxifen-treated ER-TAK1fl/fl mice (Figure 2b). Similarly, we observed that the percentage and the numbers of Foxp3+ CD4 T cells increased in mock-treated but not in tamoxifen-treated ER-TAK1fl/fl mice (Figure 2c). Therefore, interfering with TAK1 function during the initiation phase abrogated the increase in T-cell numbers that is normally associated with inflammation during a CHS response.
Figure 2.
T cells failed to expand in TMA-treated ER-TAK1fl/fl mice during a CHS response. (a) Flow cytometry analysis of CD4 and CD8 T cells in PLN and spleens from ER-TAK1fl/fl mice with or without TMA treatment. (b) Forty-eight hours after challenge, the auricular lymph nodes of DLN (solid bar) and CLN (open bar) for DNFB-treated ears were collected and the numbers of total lymphocytes were counted and plotted. The numbers of total lymphocytes and CD4 and CD8 T cells were calculated and plotted based on the percentages of each population as determined by flow cytometry analysis. (c) Foxp3 expression was detected by intracellular staining and flow cytometry. Numbers above the bracketed lines indicate the percentage of Foxp3+ cells among the CD4 population (left panel). The absolute numbers of Foxp3+ cells from DLN (solid bar) and CLN (open bar) were calculated and plotted. Mean±SD values of four mice are shown, and the P value is indicated. CHS, contact hypersensitivity; CLN, control lymph node; DLN, draining lymph node; PLN, peripheral lymph node; TAK1, transforming growth factor-β-activated kinase-1; TMA, tamoxifen.
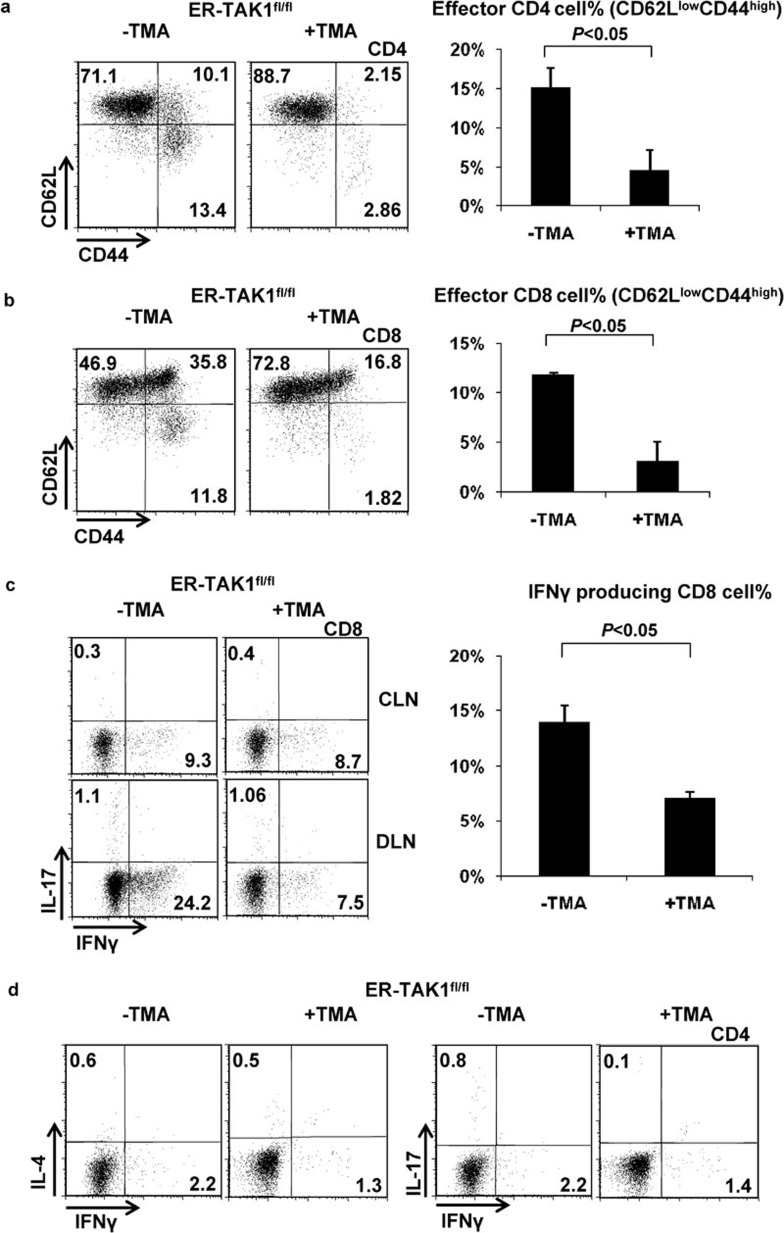
Hapten-specific CD8 T cells are recognized as the main effector cells that mediate CHS.19, 20 CD4 T cells cooperate with CD8 T cells21 and, in certain instances, mediate murine CHS responses to strong haptens.22 We further investigated whether T-cell activation and effector cytokine production were affected by TAK1 deletion during a CHS response. We found that while CD4 and CD8 T cells displayed an activated phenotype (CD62LlowCD44high) in mock-treated ER-TAK1fl/fl mice (Figure 3a and b), such activation did not occur in tamoxifen-treated ER-TAK1fl/fl mice (Figure 3a and b), suggesting that TAK1 is required for T-cell activation during the CHS response.
Figure 3.
Lack of activation and cytokine production of CD4 and CD8 T cells in TMA-treated ER-TAK1fl/fl mice. Flow cytometry analysis of CD62L and CD44 expression on CD4 (a) and CD8 (b) T cells in DLN from indicated mice 48 h after challenge (left panels). The percentages of the CD62Llow CD44high effector T-cell population were plotted (right panels). Mean±SD values of four mice are shown, and the P value is indicated. (c) IFN-γ and IL-17 production by CD8 cells in the DLN of indicated mice (left panels). The frequencies (%) of IFN-γ-producing CD8 cells obtained from four independent experiments are shown. Mean±SD values are shown and the P value is indicated. (d) IFN-γ, IL-4 and IL-17 production in CD4 cells in DLN from indicated mice were detected by intracellular staining. Representative results of four independent experiments are shown. CLN, control lymph node; DLN, draining lymph node; IFN, interferon; TAK1, transforming growth factor-β-activated kinase-1; TMA, tamoxifen.
The CHS response induced by DNFB is controlled by IFN-γ produced by CD8 T cells and, to a lesser extent, IFN-γ, IL-4 and IL-17 produced by Th1, Th2 and Th17 T cells, respectively. We assessed whether interfering with TAK1 function impacted cytokine production by T cells. Indeed, while a great number of IFN-γ-producing CD8 T cells was detected in mock-treated ER-TAK1fl/fl mice with ongoing CHS (Figure 3c), smaller numbers of IFN-γ-producing CD8 T cells were found in tamoxifen-treated ER-TAK1fl/fl mice (Figure 3c). Similarly, smaller percentages of IFN-γ-producing Th1 cells were found in tamoxifen-treated mice than in mock-treated ER-TAK1fl/fl mice (Figure 3d). Therefore, TAK1 is required for normal levels of cytokine expression in effector T cells during CHS response.
TAK1 function in DC is essential for CHS response
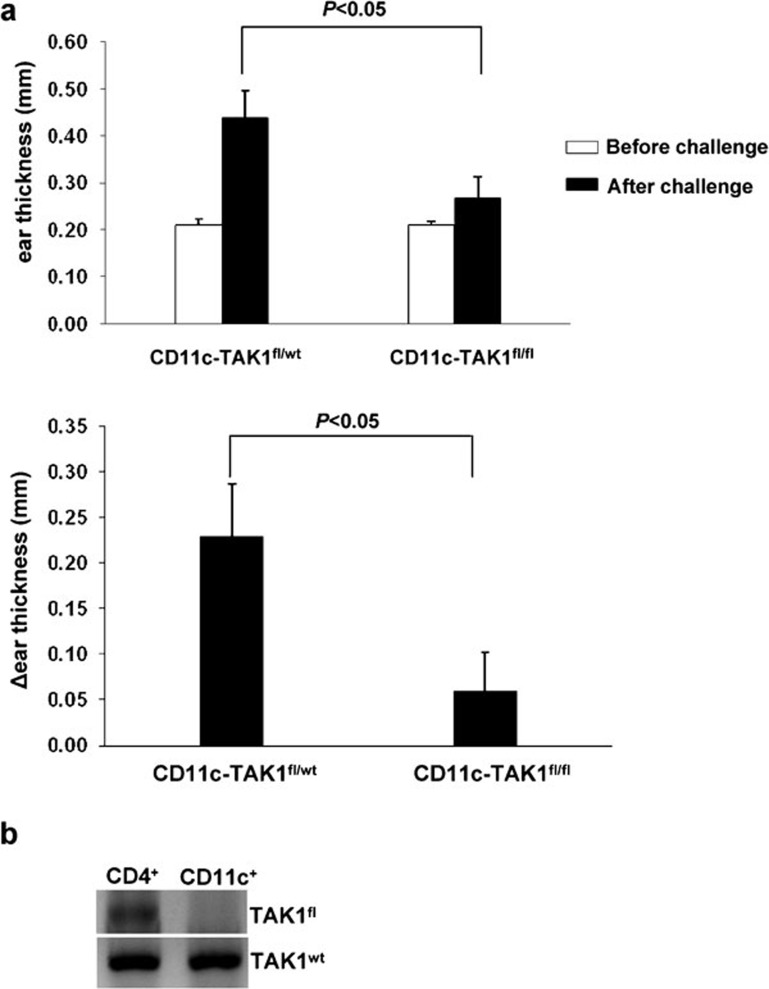
Hapten-induced T-cell activation and CHS requires intact function of innate cells, such as cutaneous DC.4, 23 We therefore hypothesized that the requirement of TAK1 in CHS response could be attributed, at least in part, to its essential role in regulating DC function. To test this hypothesis, we crossed TAK1fl/fl mice with CD11c-Cre mice to generate CD11c-TAK1fl/fl mice, which allowed for deletion of the TAK1 gene specifically in CD11c+ DC, and elicited a DNFB-induced CHS response in CD11c-TAK1fl/fl and CD11c-TAK1fl/wt mice. While a CHS response was efficiently induced in CD11c-TAK1fl/wt mice with ear swelling upon challenge, CD11c-TAK1fl/fl mice failed to develop CHS (Figure 4a). The floxed TAK1 allele was efficiently deleted in sorted CD11c+ cells but not in CD4+ cells (Figure 4b), indicating an efficient TAK1 deletion specifically in the DC population.
Figure 4.
Abolished CHS response in CD11c-TAK1fl/fl mice. (a) On day 1, the dehaired back skins of CD11c-TAK1fl/fl and CD11c-TAK1fl/wt mice were painted with DNFB. Mice were then challenged with DNFB on day 6. Before (open bar) and 48 h after (solid bar) challenge, ear thickness was measured and plotted (top panel). The Δ ear thickness was also calculated and plotted (lower panel). Mean±SD values of four mice are shown, and the P value is indicated. (b) CD11c+ and CD4+ cells were purified from CD11c-TAK1fl/wt mice. PCR analysis for the floxed-TAK allele (TAK1fl) and WT TAK1 allele (TAK1wt) (which served as an internal control) was performed. CHS, contact hypersensitivity; DNFB, 2,4-dinitrofluorobenzene; TAK1, transforming growth factor-β-activated kinase-1; WT, wild type.
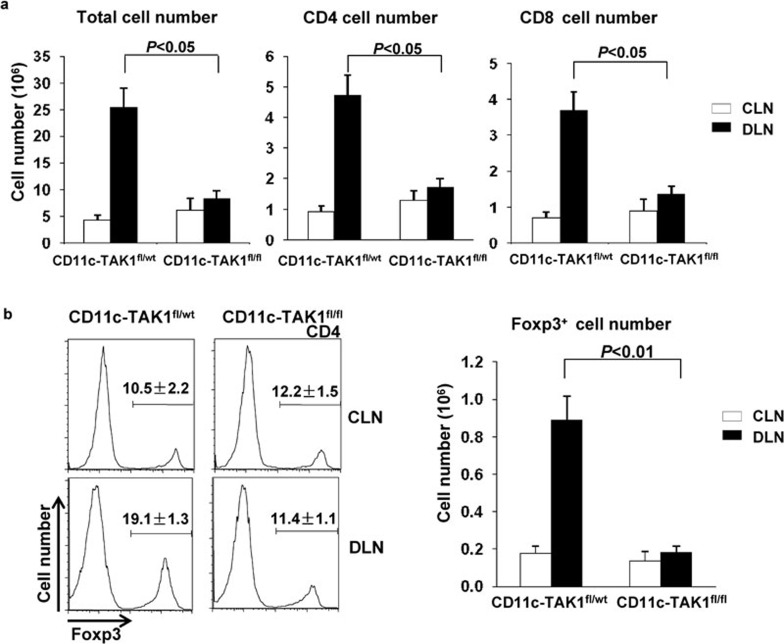
Intact TAK1 in DC is critical for T-cell function during CHS development
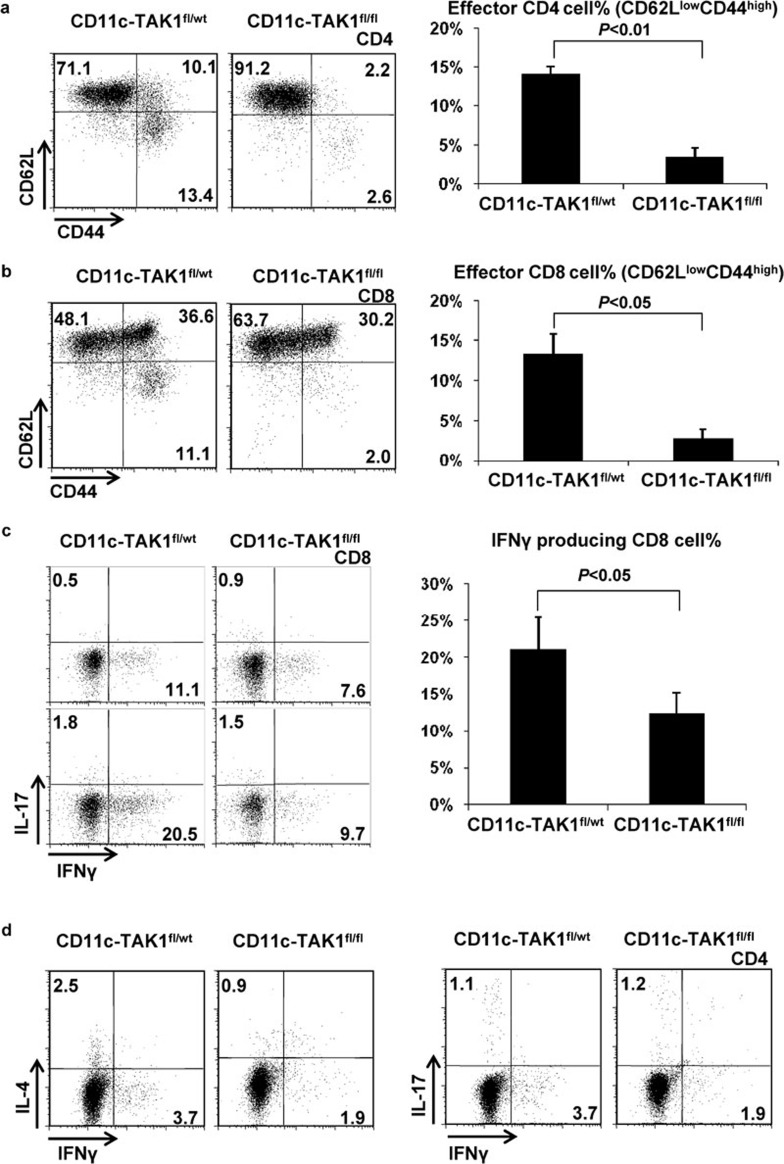
We further investigated whether T-cell function was affected in CD11c-TAK1fl/fl mice during CHS development. Our analysis revealed that the numbers of CD4, CD8 and Foxp3-expressing CD4 cells were elevated in CD11c-TAK1fl/wt mice with ongoing CHS responses. However, these increases were abolished in CD11c-TAK1fl/fl mice given the same treatment (Figure 5). Therefore, intact function of TAK1 in the CD11c+ DC population is important to promote T-cell expansion during CHS response. In addition, we observed that T-cell activation was abolished in CD11c-TAK1fl/fl mice following CHS induction. The percentages of activated (CD62LlowCD44high) CD4 and CD8 T cells of the DLN from CD11c-TAK1fl/wt mice increased significantly after CHS induction. However, such an increase did not occur in similarly treated CD11c-TAK1fl/fl mice (Figure 6a and b), suggesting an important role of TAK1 in DC for T-cell activation during CHS. Furthermore, we assessed the cytokine production of T cells in CD11c-TAK1fl/wt mice and CD11c-TAK1fl/fl mice undergoing a CHS response. Consistent with T-cell activation status, although a large percentage of IFN-γ-producing CD8 T cells were found in the DLN of CD11c-TAK1fl/wt mice, CD8 T cells from CD11c-TAK1fl/fl mice failed to increase IFN-γ production (Figure 6c). Similarly, CD4 T cells in CD11c-TAK1fl/fl mice did not produce elevated levels of IFN-γ upon CHS induction (Figure 6d).
Figure 5.
T cells failed to expand during the CHS response in CD11c-TAK1 fl/fl mice. (a) Forty-eight hours after challenge, lymphocytes from DLN (solid bar) and CLN (open bar) were collected from the indicated mouse strains, and the numbers of total lymphocytes were counted. CD4 and CD8 T-cell numbers were calculated and plotted based on the percentage of each population as determined by flow cytometry analysis and the total numbers of lymphocytes. (b) Foxp3 expression was detected by intracellular staining and flow cytometry. Numbers above the bracketed lines indicate the percentages of Foxp3+ cells among the CD4 population (left panels). The absolute numbers of Foxp3+ cells from DLN (solid bar) and CLN (open bar) were calculated and plotted (right panel). Mean±SD values of four mice are shown, and the P value is indicated. CHS, contact hypersensitivity; CLN, control lymph node; DLN, draining lymph node; TAK1, transforming growth factor-β-activated kinase-1.
Figure 6.
T-cell activation and effector function during the CHS response was abrogated in CD11c-TAK1fl/fl mice. Flow cytometry analysis of CD62L and CD44 expression on CD4 (a) and CD8 (b) T cells in DLN of indicated mice 48 h after challenge (left panels). The percentages of CD62Llow CD44high effector T cells were plotted (right panels). Mean±SD values of four mice are shown, and the P value is indicated. (c) IFN-γ and IL-17 production by CD8 cells in the DLN of indicated mice was assessed by flow cytometry (left panels). The frequencies (%) of IFN-γ-producing CD8 cells obtained from four independent experiments were plotted. Mean±SD values are shown, and the P value is indicated. (d) IFN-γ, IL-4 and IL-17 production in CD4 cells from DLN of the indicated mice was detected by intracellular staining. Representative results of four independent experiments are shown. DLN, draining lymph node; IFN, interferon; TAK1, transforming growth factor-β-activated kinase-1.
Collectively, this study demonstrated that intact function of TAK1 is critical for hapten-elicited activation and effector function of T cells and the development of a CHS response. Furthermore, this function of TAK1 can be ascribed at least in part to its critical role in regulating DC function.
Discussion
The relationship between TAK1 and immune function was originally revealed by studies on Drosophila.24 Subsequently, TAK1 was shown to be required for both innate and adaptive immunity in mammals.9, 12, 14 Previous studies have indicated that TAK1 is involved in the development of inflammatory diseases, such as rheumatoid arthritis.25, 26 Targeting TAK1 function may therefore be a viable approach to treating inflammatory diseases. CHS, a murine model for studying allergic contact dermatitis, is characterized as a classic T cell-mediated immune response.18 Whether TAK1 was functionally involved in CHS development was not previously addressed. Our current study shows for the first time that CHS induction and T-cell activation by DNFB are dependent on TAK1.
During the elicitation phase of CHS, re-exposure of sensitized mice to DNFB induces quantitative and qualitative alterations in T-lymphocyte responses. Quantitatively, T cells proliferate and increase in numbers in DLN.27 Qualitatively, T cells display an activated phenotype by downregulating CD62L expression and upregulating CD44 expression28 and producing IFN-γ.6 We found that interfering with TAK1 function affected T-cell function both quantitatively and qualitatively. First, T-cell numbers failed to increase in response to CHS response when TAK1 was disrupted (Figure 2b). Peripheral T-cell survival has been shown to be dependent on TAK1.12 However, the percentages of CD4 and CD8 T cells from peripheral lymph node, spleen and CLN did not decrease in tamoxifen-treated ER-TAK1fl/fl mice during a CHS response (Figure 2a and b), indicating that local administration of tamoxifen did not cause systemic depletion of T cells. Thus, the lack of T-cell expansion in DLN of mice with inhibited TAK1 is likely due to unresponsiveness to DNFB elicitation rather than to a defect in T-cell survival caused by TAK1 deletion. In agreement with this notion, our study showed that T cells failed to become activated or to produce IFN-γ when TAK1 was absent. Multiple mechanisms may account for this observation. The previously described requirement of TAK1 for T-cell function12 could explain our findings. In addition, defective innate function due to TAK1 disruption may also contribute to T-cell unresponsiveness.
The induction of a CHS response relies on the activation, maturation, antigen presentation and migration of innate immune cells.29 TAK1 may be important for these functions during the initiation of CHS. In ER-TAK1fl/fl mice, tamoxifen application on skin induced TAK1 deletion in various cell types, including stromal cells, but particularly in cutaneous DC, which are considered to play a central role in the initiation of responses to haptens.29 To specifically study the influence of TAK1 on DCs, we generated CD11c-TAK1fl/fl mice to knock out the TAK1 gene specifically in CD11c+ cells, which are mainly DC. Using this mouse model, we found that TAK1 function in DC is critical for the induction of CHS and T-cell responses (Figures 4a, 5a and 6). Although we have provided convincing genetic evidence to support the notion that TAK1 is essential for DC function during hapten-elicited CHS responses, the underlying mechanisms remain to be addressed. One possible explanation is that TAK1 plays an important role in the Toll-like receptor-induced NF-κB activation30, 31 that is critical for DC functions, including migration, survival and antigen processing and presentation.32 Given that the Toll-like receptor (TLR) are thought to be indispensable for CHS development,23 one mechanism by which TAK1 regulates DC function during CHS may be through a Toll-like receptor pathway. In addition, the migratory ability of DC might be affected by TAK1 deletion because the expression of chemokine ligands, including ccl2, ccl7 and ccl5, was strongly suppressed in TAK1 null cells.33 However, whether TAK1 deficiency affects the maturation, antigen presentation ability or cytokine production of DC warrants further study.
Regulatory T cells potently suppress innate and adaptive immune cells34 to dampen immune responses and maintain homeostasis. For example, regulatory T cells can be induced by foreign antigen35 to limit the inflammatory response in the skin.36 It is possible that the impaired CHS response we observed in mice with defective TAK1 function was due to increased immune suppression mediated by Foxp3-expressing regulatory T cells. However, our findings suggested that this may not be the case because the percentage and numbers of Foxp3+ cells in tamoxifen-treated ER-TAK1fl/fl mice and in CD11c-TAK1fl/fl mice failed to increase during the CHS response, unlike in the control mice (Figure 2c and 4b). This finding suggests that TAK1 is critically involved in CHS responses through a regulatory T cell-independent mechanism.
In conclusion, our study showed for the first time that TAK1 is critical for CHS development. Mechanistically, TAK1 is essential for the functions of both innate immunity mediated by DC and adaptive immunity mediated by T cells in the elicitation of a CHS response. Therefore, local or DC-specific targeting of a TAK1 deletion may serve as a viable approach to treating CHS-type immune diseases.
Acknowledgments
This work was supported by the National Institutes of Health (R00AI072956 to YYW), the Beijing Natural Science Foundation (7082054), the National Science and Technology Major Specific Project of the People's Republic of China (2009ZX09301-010 to WH) and the China Scholarship Council (YGZ).
The authors have no conflicting interests.
References
- Coenraads PJ, Goncalo M. Skin diseases with high public health impact. Contact dermatitis. Eur J Dermatol. 2007;17:564–565. doi: 10.1684/ejd.2007.0299. [DOI] [PubMed] [Google Scholar]
- Asano Y, Makino T, Norisugi O, Shimizu T. Occupational cobalt induced systemic contact dermatitis. Eur J Dermatol. 2009;19:166–167. doi: 10.1684/ejd.2008.0581. [DOI] [PubMed] [Google Scholar]
- Saint-Mezard P, Rosieres A, Krasteva M, Berard F, Dubois B, Kaiserlian D, et al. Allergic contact dermatitis. Eur J Dermatol. 2004;14:284–295. [PubMed] [Google Scholar]
- Martin SF, Jakob T. From innate to adaptive immune responses in contact hypersensitivity. Curr Opin Allergy Clin Immunol. 2008;8:289–293. doi: 10.1097/ACI.0b013e3283088cf9. [DOI] [PubMed] [Google Scholar]
- Jakob T, Ring J, Udey MC. Multistep navigation of Langerhans/dendritic cells in and out of the skin. J Allergy Clin Immunol. 2001;108:688–696. doi: 10.1067/mai.2001.118797. [DOI] [PubMed] [Google Scholar]
- Xu H, DiIulio NA, Fairchild RL. T cell populations primed by hapten sensitization in contact sensitivity are distinguished by polarized patterns of cytokine production: interferon gamma-producing (Tc1) effector CD8+ T cells and interleukin (IL) 4/IL-10-producing (Th2) negative regulatory CD4+ T cells. J Exp Med. 1996;183:1001–1012. doi: 10.1084/jem.183.3.1001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trautmann A, Akdis M, Schmid-Grendelmeier P, Disch R, Brocker EB, Blaser K, et al. Targeting keratinocyte apoptosis in the treatment of atopic dermatitis and allergic contact dermatitis. J Allergy Clin Immunol. 2001;108:839–846. doi: 10.1067/mai.2001.118796. [DOI] [PubMed] [Google Scholar]
- Akiba H, Kehren J, Ducluzeau MT, Krasteva M, Horand F, Kaiserlian D, et al. Skin inflammation during contact hypersensitivity is mediated by early recruitment of CD8+ T cytotoxic 1 cells inducing keratinocyte apoptosis. J Immunol. 2002;168:3079–3087. doi: 10.4049/jimmunol.168.6.3079. [DOI] [PubMed] [Google Scholar]
- Sato S, Sanjo H, Takeda K, Ninomiya-Tsuji J, Yamamoto M, Kawai T, et al. Essential function for the kinase TAK1 in innate and adaptive immune responses. Nat Immunol. 2005;6:1087–1095. doi: 10.1038/ni1255. [DOI] [PubMed] [Google Scholar]
- Shim JH, Xiao C, Paschal AE, Bailey ST, Rao P, Hayden MS, et al. TAK1, but not TAB1 or TAB2, plays an essential role in multiple signaling pathways in vivo. . Genes Dev. 2005;19:2668–2681. doi: 10.1101/gad.1360605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skaug B, Jiang X, Chen ZJ. The role of ubiquitin in NF-kappaB regulatory pathways. Annu Rev Biochem. 2009;78:769–796. doi: 10.1146/annurev.biochem.78.070907.102750. [DOI] [PubMed] [Google Scholar]
- Wan YY, Chi H, Xie M, Schneider MD, Flavell RA. The kinase TAK1 integrates antigen and cytokine receptor signaling for T cell development, survival and function. Nat Immunol. 2006;7:851–858. doi: 10.1038/ni1355. [DOI] [PubMed] [Google Scholar]
- Davis RJ. Signal transduction by the JNK group of MAP kinases. Cell. 2000;103:239–252. doi: 10.1016/s0092-8674(00)00116-1. [DOI] [PubMed] [Google Scholar]
- Schuman J, Chen Y, Podd A, Yu M, Liu HH, Wen R, et al. A critical role of TAK1 in B-cell receptor-mediated nuclear factor kappaB activation. Blood. 2009;113:4566–4574. doi: 10.1182/blood-2008-08-176057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Landstrom M. The TAK1–TRAF6 signalling pathway. Int J Biochem Cell Biol. 2010;42:585–589. doi: 10.1016/j.biocel.2009.12.023. [DOI] [PubMed] [Google Scholar]
- Shapiro-Shelef M, Lin KI, Savitsky D, Liao J, Calame K. Blimp-1 is required for maintenance of long-lived plasma cells in the bone marrow. J Exp Med. 2005;202:1471–1476. doi: 10.1084/jem.20051611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vooijs M, Jonkers J, Berns A. A highly efficient ligand-regulated Cre recombinase mouse line shows that LoxP recombination is position dependent. EMBO Rep. 2001;2:292–297. doi: 10.1093/embo-reports/kve064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nosbaum A, Vocanson M, Rozieres A, Hennino A, Nicolas JF. Allergic and irritant contact dermatitis. Eur J Dermatol. 2009;19:325–332. doi: 10.1684/ejd.2009.0686. [DOI] [PubMed] [Google Scholar]
- Vocanson M, Hennino A, Cluzel-Tailhardat M, Saint-Mezard P, Benetiere J, Chavagnac C, et al. CD8+ T cells are effector cells of contact dermatitis to common skin allergens in mice. J Invest Dermatol. 2006;126:815–820. doi: 10.1038/sj.jid.5700174. [DOI] [PubMed] [Google Scholar]
- Martin S, Lappin MB, Kohler J, Delattre V, Leicht C, Preckel T, et al. Peptide immunization indicates that CD8+ T cells are the dominant effector cells in trinitrophenyl-specific contact hypersensitivity. J Invest Dermatol. 2000;115:260–266. doi: 10.1046/j.1523-1747.2000.00038.x. [DOI] [PubMed] [Google Scholar]
- Traidl C, Sebastiani S, Albanesi C, Merk HF, Puddu P, Girolomoni G, et al. Disparate cytotoxic activity of nickel-specific CD8+ and CD4+ T cell subsets against keratinocytes. J Immunol. 2000;165:3058–3064. doi: 10.4049/jimmunol.165.6.3058. [DOI] [PubMed] [Google Scholar]
- Vocanson M, Hennino A, Chavagnac C, Saint-Mezard P, Dubois B, Kaiserlian D, et al. Contribution of CD4+ and CD8+ T-cells in contact hypersensitivity and allergic contact dermatitis. Expert Rev Clin Immunol. 2005;1:75–86. doi: 10.1586/1744666X.1.1.75. [DOI] [PubMed] [Google Scholar]
- Martin SF, Dudda JC, Bachtanian E, Lembo A, Liller S, Durr C, et al. Toll-like receptor and IL-12 signaling control susceptibility to contact hypersensitivity. J Exp Med. 2008;205:2151–2162. doi: 10.1084/jem.20070509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silverman N, Zhou R, Erlich RL, Hunter M, Bernstein E, Schneider D, et al. Immune activation of NF-kappaB and JNK requires Drosophila TAK1. J Biol Chem. 2003;278:48928–48934. doi: 10.1074/jbc.M304802200. [DOI] [PubMed] [Google Scholar]
- Hammaker DR, Boyle DL, Chabaud-Riou M, Firestein GS. Regulation of c-Jun N-terminal kinase by MEKK-2 and mitogen-activated protein kinase kinase kinases in rheumatoid arthritis. J Immunol. 2004;172:1612–1618. doi: 10.4049/jimmunol.172.3.1612. [DOI] [PubMed] [Google Scholar]
- Hammaker DR, Boyle DL, Inoue T, Firestein GS. Regulation of the JNK pathway by TGF-beta activated kinase 1 in rheumatoid arthritis synoviocytes. Arthritis Res Ther. 2007;9:R57. doi: 10.1186/ar2215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kimber I, Dearman RJ. Investigation of lymph node cell proliferation as a possible immunological correlate of contact sensitizing potential. Food Chem Toxicol. 1991;29:125–129. doi: 10.1016/0278-6915(91)90167-6. [DOI] [PubMed] [Google Scholar]
- Gerberick GF, Cruse LW, Miller CM, Sikorski EE, Ridder GM. Selective modulation of T cell memory markers CD62L and CD44 on murine draining lymph node cells following allergen and irritant treatment. Toxicol Appl Pharmacol. 1997;146:1–10. doi: 10.1006/taap.1997.8218. [DOI] [PubMed] [Google Scholar]
- Vocanson M, Hennino A, Rozieres A, Poyet G, Nicolas JF. Effector and regulatory mechanisms in allergic contact dermatitis. Allergy. 2009;64:1699–1714. doi: 10.1111/j.1398-9995.2009.02082.x. [DOI] [PubMed] [Google Scholar]
- Jiang Z, Zamanian-Daryoush M, Nie H, Silva AM, Williams BR, Li X. Poly(I-C)-induced Toll-like receptor 3 (TLR3)-mediated activation of NFkappa B and MAP kinase is through an interleukin-1 receptor-associated kinase (IRAK)-independent pathway employing the signaling components TLR3–TRAF6–TAK1–TAB2–PKR. J Biol Chem. 2003;278:16713–16719. doi: 10.1074/jbc.M300562200. [DOI] [PubMed] [Google Scholar]
- Irie T, Muta T, Takeshige K. TAK1 mediates an activation signal from Toll-like receptor(s) to nuclear factor-kappaB in lipopolysaccharide-stimulated macrophages. FEBS Lett. 2000;467:160–164. doi: 10.1016/s0014-5793(00)01146-7. [DOI] [PubMed] [Google Scholar]
- Zanoni I, Granucci F. Regulation of antigen uptake, migration, and lifespan of dendritic cell by Toll-like receptors. J Mol Med. 2010;88:873–880. doi: 10.1007/s00109-010-0638-x. [DOI] [PubMed] [Google Scholar]
- Thiefes A, Wolter S, Mushinski JF, Hoffmann E, Dittrich-Breiholz O, Graue N, et al. Simultaneous blockade of NFkappaB, JNK, and p38 MAPK by a kinase-inactive mutant of the protein kinase TAK1 sensitizes cells to apoptosis and affects a distinct spectrum of tumor necrosis factor [corrected] target genes. J Biol Chem. 2005;280:27728–27741. doi: 10.1074/jbc.M411657200. [DOI] [PubMed] [Google Scholar]
- Wan YY, Flavell RA. TGF-beta and regulatory T cell in immunity and autoimmunity. J Clin Immunol. 2008;28:647–659. doi: 10.1007/s10875-008-9251-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kretschmer K, Apostolou I, Hawiger D, Khazaie K, Nussenzweig MC, von Boehmer H. Inducing and expanding regulatory T cell populations by foreign antigen. Nat Immunol. 2005;6:1219–1227. doi: 10.1038/ni1265. [DOI] [PubMed] [Google Scholar]
- Dubois B, Chapat L, Goubier A, Papiernik M, Nicolas JF, Kaiserlian D. Innate CD4+CD25+ regulatory T cells are required for oral tolerance and inhibition of CD8+ T cells mediating skin inflammation. Blood. 2003;102:3295–3301. doi: 10.1182/blood-2003-03-0727. [DOI] [PubMed] [Google Scholar]