Abstract
Purpose
To determine the prevalence of follow-up and factors associated with completing an eye exam after a glaucoma public service announcement.
Design
Cross-sectional observational study
Participants
Individuals who participated in the Glaucoma EyeCare Program by calling a toll-free telephone number and receiving referral by meeting inclusion criteria.
Methods
The Glaucoma EyeCare Program uses public service announcements to encourage those at increased risk for glaucoma to obtain an eye exam. The program requires interested persons to dial a toll-free telephone number to collect demographic, medical, and socioeconomic information, and refers those at higher risk of glaucoma to an ophthalmologist for a free eye exam. The ophthalmologist completes an outcome form, which indicates whether the participant obtained an eye exam, and the results of this eye exam. We determined the factors associated with obtaining an eye exam.
Main Outcome Measures
Sociodemographic characteristics associated with obtaining an eye exam after referral through the Glaucoma EyeCare Program
Results
Ophthalmologists returned outcome forms for 24% (1514/6343) of participants. Of those with outcome forms, 671 (44.3%) had an eye exam, 756 (49.9%) did not make an appointment, and 87 (5.7%) made an appointment but did not complete the exam. A multivariate logistic regression model showed younger age, female gender, lack of health insurance, medical history of diabetes, and shorter distance to be associated with obtaining an eye exam.
Conclusion
Public service announcements encourage participants to have an eye exam. Multiple factors alter the success of obtaining an eye exam. Future studies are needed regarding the best method of decreasing the risk of undiagnosed glaucoma.
Glaucoma is the second leading cause of blindness worldwide.1 At least 50% of patients with glaucoma have not been diagnosed.2–4 Organizations have attempted to decrease the proportion of undiagnosed glaucoma by performing screening tests (such as frequency doubling technology perimetry) in the community.5,6 However public service announcements are another way of decreasing undiagnosed glaucoma. For example, public service announcements may highlight the risks of glaucoma, the need for eye exams, and encourage people at risk to have an eye exam. They also may have the advantage of reaching a larger audience when compared to screening tests because they utilize mass media, and don’t require interested participants to come to a particular location on a certain date for a screening test.
The Foundation of the American Academy of Ophthalmology established the EyeCare America program in 1985. The program uses public service announcements to educate its audience about the risks associated with various eye diseases and to publicize the availability of free ophthalmic care for those without insurance who are at greater risk for developing these diseases. It employs various forms of mass media including newspaper, television, radio, and Internet. The program also engages local celebrities to increase exposure. One subsection of EyeCare America is the Glaucoma EyeCare Program, whose mission is detection of undiagnosed glaucoma through eye exams by volunteer ophthalmologists.
We were interested in the proportion of participants who have an eye exam after the Glaucoma EyeCare Program identifies them as having a higher risk for the development of glaucoma and eligible for an eye exam. Glaucoma screenings with frequency doubling technology perimetry result in 40% to 70%5,6 of screening failures having an eye exam. To our knowledge, no study has reported the ability of public service announcements to encourage participants to have an eye exam and the factors associated with obtaining an eye exam. This information will provide guidance for designing and enhancing glaucoma public service announcements in the future to decrease the risk of undiagnosed glaucoma.
Methods
The Glaucoma EyeCare Program provided the authors with a de-identified database. The Institutional Review Board (IRB) of Legacy Health System approved this study.
Participants and data collection
The Glaucoma EyeCare Program uses nationwide public service announcements to encourage their audience to call a toll-free telephone number to determine whether callers are at increased risk for glaucoma and therefore eligible to receive a free glaucoma eye exam. Each public service announcement briefly discusses natural history and risk factors for glaucoma, often in conjunction with a real-life clinical vignette, and concludes with information on how to contact the program (see http://www.youtube.com/user/eyecareamerica for examples [accessed September 15, 2010]). During this portion of the telephone call, the program collects gender, age, ethnicity, medical insurance status, personal history of diabetes, home address, family history of eye problems, duration since their last eye exam, and calculates glaucoma risk score.
The glaucoma risk score survey questions are listed in Table 1 and are based on age, family history of glaucoma, and race. Two members of the Glaucoma EyeCare Program advisory committee, M. Roy Wilson and James F. Martone, created this scoring system in the 1980’s to be internally consistent with risk factors from then current prevalence studies.7–11 Another goal was to create a simple scoring system that was suitable for primary care medical providers and glaucoma patients (Personal communication-M. Roy Wilson and James F. Martone). The Glaucoma EyeCare Program considers a survey score of 4 or greater (≥4) as high risk, with a total range of possible scores from 0 to 10. For example, a 55-year-old African American caller with a brother who has glaucoma would be given a score of 9.
Table 1.
Telephone survey questions with associated score values
| 1. Family history | Score value |
| My parent or child has glaucoma | 2 |
| My brother or sister has glaucoma | 4 |
| My parent and brother or sister has glaucoma | 4 |
| There is no known glaucoma in my family | 0 |
| 2. Race | |
| I am white/Caucasian | 1 |
| I am Hispanic | 2 |
| I am black/African American | 3 |
| 3. Age | |
| I am younger than 40 years old | 0 |
| I am 40–49 years old | 1 |
| I am 50–59 years old | 2 |
| I am 60 or older | 3 |
A total score of 4 or greater (≥4) is considered high risk for glaucoma.
Any high risk participant is eligible for a free glaucoma eye exam if he or she is a United States citizen or legal resident; has not had an eye exam in 12 or more months; and does not belong to a health maintenance organization or Veterans Administration health plan. These exclusion criteria were incorporated based on Medicare restrictions and this information was included in the public service announcements. If eligible, the Glaucoma EyeCare Program provides the participant the name, office address, and telephone number of a volunteer ophthalmologist in their area and encourages them to call for an appointment. The Glaucoma EyeCare Program sends the participant’s information to the ophthalmologist and instructs the ophthalmologist to complete and return the outcome form after the visit, which includes whether the participant obtained an eye exam and the results of this exam. Information gathered from the telephone interview was used for data analysis.
Data Analysis
We include participants enrolled between January 15, 2006 and January 14, 2007. All statistical analyses were performed using SPSS® (v16.0, SPSS, Inc. Chicago, Illinois) statistical software. We created dichotomous variables for gender; ethnicity (white vs. other); insurance status (yes vs. no); family history of glaucoma; and medical history of diabetes. We included age and distance (between the participant and doctor’s office) as continuous variables.
We compared the characteristics of those included in the study (had an outcome form returned) to those excluded (did not have an outcome form returned) to evaluate selection bias. We compared characteristics of those who obtained an eye exam to those who did not obtain an eye exam to determine the factors related to obtaining an eye exam after a public service announcement. We used a chi-square test to evaluate the association of gender, race, insurance status, family history of glaucoma, and history of diabetes. We used a t-test to test the association of age and distance from the doctor’s office after confirming a normal distribution. We performed a multivariate logistic regression using an automated step-wise (Wald) selection procedure to select the factors most likely to be associated with obtaining an eye exam. Finally, we used a univariate logistic regression model to determine the association of glaucoma risk score with diagnosis of glaucoma, diagnosis of glaucoma suspect, and a combined diagnosis including glaucoma or glaucoma suspect.
We used the inverse probability weighting method12 to statistically weight and adjust for selection bias, resulting in differences between those included (had outcome forms returned) and excluded (no outcome forms) from the analysis. Briefly, this method creates statistical weighting using the inverse estimated probability of selection into the sample. Weighting creates up-regulation or down-regulation of the i-th individual to create a pseudosample that would have been observed if there were no differences between the included and excluded groups. We created fitted probabilities by using a logistic regression model with the dependent variable of outcome form returned (yes/no), and covariates with p values below 0.10.
Results
Participants
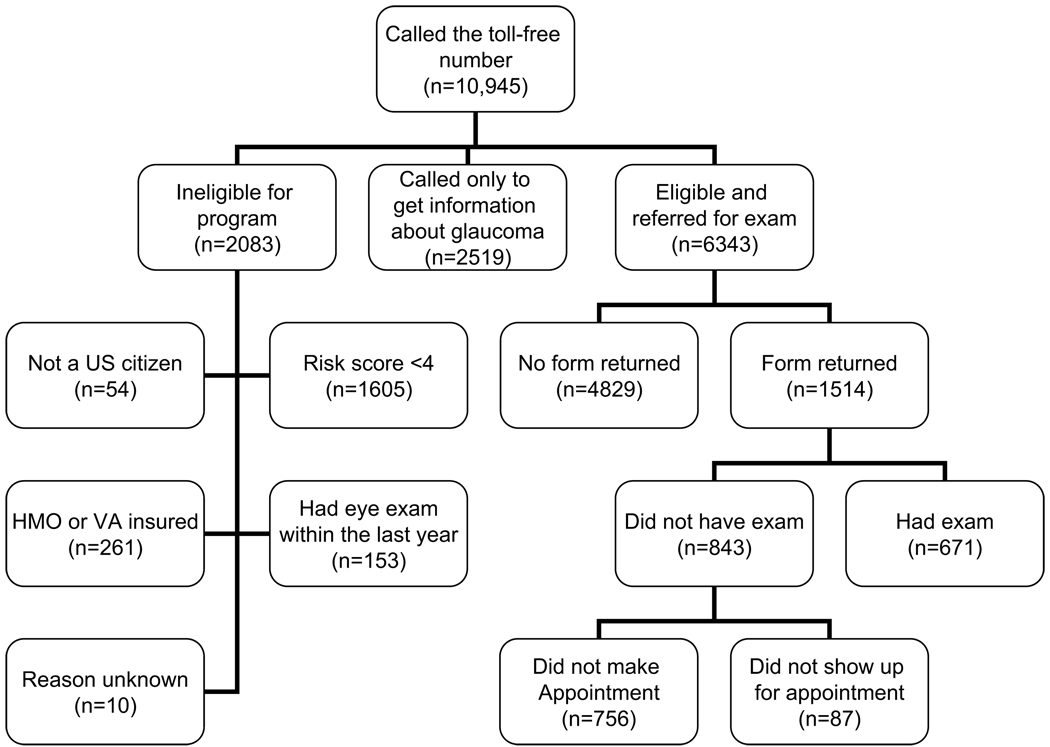
Figure 1 shows the total number of participants who called the toll-free telephone number, completed the telephone survey and received referral. Ten thousand nine hundred forty five (10,945) persons called the Glaucoma EyeCare toll-free phone number. Some callers (n=2519, 23%) did not want an eye exam but wanted more information regarding eye disease. Others were not eligible (n=2083, 19%). Of those not eligible, the reasons were: had a glaucoma risk score under 4 (n=1605); had health maintenance organization insurance or VA insurance (n=261); had a recent eye exam in the last 12 months (n=153); not United States citizens or resident (n=54); and unknown reason (n=10).
Figure 1.
Flowchart of Glaucoma EyeCare Program Participants (US= United States, HMO=Health Maintenance Organization, VA=Veterans Administration)
Of the 6343 persons referred, ophthalmologists returned 1514 (24%) outcome forms. A form was not returned for 4829 (76%) participants. Six hundred seventy one participants (n=671, 44.3%) obtained an eye exam after the referral generated from the public service announcement. Among those participants who did not have an eye exam, 756 (49.9%) did not make an appointment, and 87 (5.7%) made an appointment but did not come to the appointment.
Those referred (n=6343) had an average (+/− standard deviation) age of 62.3 (+/−11.7) years; were predominately female (65.8%); and were more likely to be uninsured (52.2%). They had a family history of glaucoma in 39.4%; had an average (+/−standard deviation) glaucoma score of 5.1 (+/−1.5); had a medical history of diabetes in 23.5%; and lived an average (+/−standard deviation) of 10.7 (+/−21.5) miles from the ophthalmologist’s office. Their ethnicities included 62.0% white, 27.0% African-American, 9.0% Hispanic, 0.9% Asian/Pacific islander, and 1.1% “other ethnicities”.
We explored the possibility of selection bias between those with and without outcome forms in Table 2. This table demonstrates differences between those with outcome forms returned (were included in the study) and those who did not have an outcome form returned (not included). We used the inverse probability weighting method13 to adjust for these differences. Based on the results of Table 2, we included as covariates: age, gender, insurance status, family history of glaucoma, and medical history of diabetes. The logistic regression model for creating weight included: dependent variable Y= outcome form returned (yes/no), intercept= −0.653, and covariates (β=beta coefficient) of age (β=−0.012), gender(β=0.221), insurance status(β=−0.301), family history of glaucoma(β=.032), and medical history of diabetes(β=0.121).
Table 2.
Sociodemographic characteristics for referred participants who did and did not have outcome forms returned
| Outcome Form Returned (n=1514) | Outcome Form Not Returned (n=4829) | p value* | |
|---|---|---|---|
| Age (mean +/− std) | 60.3 +/− 11.0 | 62.9 +/− 11.8 | <0.001 |
| < 40 | 43 (2.8) | 116 (2.4) | |
| 41–60 | 688 (45.4) | 1728 (35.8) | |
| 61–80 | 707 (46.7) | 2604 (53.9) | |
| >80 | 76 (5) | 381 (7.9) | |
| Gender (% female) | 1054 (69.6) | 3122 (64.7) | <0.001 |
| Ethnicity (white vs. Other) | 0.001 | ||
| White | 886 (58.5) | 3048 (63.1) | |
| African American | 420 (27.7) | 1290 (26.7) | |
| Hispanic | 172 (11.4) | 400 (8.3) | |
| Asian/Pac Islander | 9 (0.6) | 49 (1) | |
| Other | 27 (1.8) | 41 (0.8) | |
| Uninsured | 854 (56.4) | 2181 (45.2) | <0.001 |
| Family History of Glaucoma | 658 (43.5) | 1842 (38.1) | <0.001 |
| Glaucoma Score | 5.2 +/− 1.5 | 5.1 +/− 1.5 | 0.21 |
| Medical History of Diabetes | 381 (25.2) | 1109 (23.0) | 0.08 |
| Distance from ophthalmologist (miles) | 11.2 | 10.5 | 0.26 |
Compared groups using chi-square tests for dichotomous variables, and t-test for continuous variables.
Factors associated with obtaining an eye exam after referral resulting from public service announcement
Table 3 documents the factors associated with having an eye exam. Female gender, younger age, shorter distance from the doctor, not having insurance coverage, history of diabetes and family history of glaucoma increased the likelihood of having an eye exam based on univariate analysis. A multivariate regression analysis showed gender (p=0.01), insurance status (p<0.001), history of diabetes (p<0.001) and distance from the doctor (p<0.001) to be significantly associated with obtaining an eye exam. The results were similar when using statistical weighting except that younger age became significant.
Table 3.
Sociodemographic characteristics for those who did and did not see the doctor
| Had eye exam (n=671) |
Did not have eye exam (n=843) |
p value* |
p value** |
p value† |
|
|---|---|---|---|---|---|
| Age (mean +/− std) | 58.5 | 61.7 | <0.001 | 0.14 | 0.001 |
| < 40 | 13 (1.9) | 30 (3.6) | |||
| 41–60 | 355 (52.9) | 333 (39.5) | |||
| 61–80 | 289 (43.1) | 418 (49.6) | |||
| >80 | 14 (2.1) | 62 (7.4) | |||
| Gender (% female) | 492 (73.3) | 560 (66.4) | 0.005 | 0.01 | <0.001 |
| Ethnicity | 0.22 | 0.57 | 0.98 | ||
| White | 385 (57.4) | 498 (59.1) | |||
| African American | 197 (29.3) | 223 (26.4) | |||
| Hispanic | 73 (10.9) | 99 (11.7) | |||
| Asian/Pac Islander | 4 (0.6) | 5 (0.6) | |||
| Other | 12 (1.8) | 15 (1.8) | |||
| Uninsured | 478 (71.2) | 376 (44.6) | <0.001 | <0.001 | <.001 |
| Family History of Glaucoma | 329 (49) | 329 (39) | <0.001 | 0.10 | 0.36 |
| Glaucoma Score (mean +/− SD) | 5.3 +/−1.4 | 5.1 +/−1.5 | 0.14 | 0.88 | 0.47 |
| Medical History of Diabetes | 190 (28.3) | 191 (22.7) | 0.012 | 0.001 | <0.001 |
| Distance from the ophthalmologist office (miles) | 9 | 13 | <0.001 | <0.0001 | <0.001 |
Univariate logistic regression for those who had an eye exam and those who did not (younger age, female gender, not having health insurance, history of diabetes family history of glaucoma and shorter distance from the doctor were significant characteristics for seeing the doctor)
Results of a multivariate logistic regression model including all variables listed (female gender, not having health insurance, history of diabetes and shorter distance from the doctor were significant characteristics for seeing the doctor)
Results of a weighted multivariate logistic regression model including all variables listed (younger age, female gender, not having health insurance, history of diabetes and shorter distance from the doctor were significant characteristics for seeing the doctor)
Table 4 shows the diagnoses of participants who obtained an eye exam. Cataract (42.6%) was the most common diagnosis. A diagnosis of glaucoma or glaucoma suspect occurred in 18.5% of participants. Other common diagnoses included refractive error, and dry eyes. A normal eye exam was found in 5.8%. Glaucoma risk score was not significantly associated with a diagnosis of glaucoma (Odds Ratio=1.08, 95% confidence interval = 0.90–1.30, p=0.44), but was significantly associated with a diagnosis of glaucoma suspect (Odds Ratio=1.30, 95% confidence interval = 1.13–1.49, p<0.001) and a combined glaucoma or glaucoma suspect diagnosis (Odds Ratio= 1.22, 95% confidence interval =1.09–1.37, p<0.001).
Table 4.
Eye problems of participants who attained an eye exam (n=671 participants).
| Eye Problem* | n (%) |
|---|---|
| Cataract | 286 (42.6) |
| Refractive error | 97 (14.5) |
| Glaucoma suspect | 76 (11.3) |
| Dry eyes | 59 (8.8) |
| Glaucoma | 48 (7.2) |
| Normal eye exam | 39 (5.8) |
| Diabetic retinopathy | 38 (5.7) |
| Posterior capsular opacity | 24 (3.6) |
| Other retinal disease** | 22 (3.3) |
| Conjunctival and/or lid problem | 22 (3.3) |
| Amblyopia | 12 (1.8) |
| Macular degeneration (dry and/or wet) | 11 (1.6) |
| Other diseases† | 9 (1.3) |
| Vitreous opacities | 9 (1.3) |
| Traumatic injury | 4 (0.6) |
| Unknown diagnosis | 3 (0.4) |
Total does not add to 671 because some participants had multiple eye problems.
Other retinal diseases (some had multiple retinal problems) included: lattice degeneration (n=4), hypertensive retinopathy (n=4), retinal vein occlusion (n=4), chorioretinal scars from histoplasmosis (n=3), choroidal nevus (n=2), epiretinal membrane (n=2), macular hole (n=2), retinal detachment (n=2), and central serous chorioretinopathy.
Other diseases included corneal disease (n=4), strabismus (n=3), and optic atrophy (n=2).
Discussion
Organizations use public service announcements to promote health awareness of many issues from smoking cessation13 to colorectal cancer screening.14 To our knowledge, this is the first study exploring the effectiveness of nationwide public service announcements to encourage individuals at increased risk for glaucoma to have an eye exam. We were also interested in the factors associated with obtaining an eye exam among participants identified as being at increased risk for glaucoma. Results from our analysis show that participants are more likely to obtain an eye exam if they are female, uninsured, have a history of diabetes and live closer to the ophthalmologist’s office. Ophthalmologists diagnosed cataract, refractive error, glaucoma suspect, dry eyes, and glaucoma most commonly, with only a small proportion (5.8%) having a normal eye exam. This represents a large number of vision threatening conditions. We also found that a one-point increase in the glaucoma risk score- greater than or equal to the threshold score of 4 resulted in a 22% increase (Odds Ratio=1.22, p <0.001) in the risk of having a diagnosis of glaucoma suspect or glaucoma.
Factors associated with obtaining an eye exam after referral
One factor previously reported as a barrier to seeking follow up care is lack of health insurance,5,15,16 even when the care was provided free of charge.5 Our results may seem contradictory since participants were more likely to have an exam if they were uninsured. One explanation is that those with insurance had more flexibility to see an eye care provider outside of the Glaucoma EyeCare Program. This eye care provider may have an office location or an appointment time that is more convenient. Inability to take time away from work, co-payments, and insurance deductibles may have also discouraged those with insurance from obtaining an eye exam. Future studies should explore the reasons why those with insurance are less likely to have an eye exam after a public service announcement.
Female participants in the current study were more likely to have an eye exam. Others have previously reported gender differences in utilization of medical care.17–19 These studies suggested that women recognize symptoms of disease and have a greater interest in health maintenance than men. A study by Green, et al18 found that gender-related attitudinal and behavioral factors are more powerful predictors of health care utilization than health-related knowledge.
We also found that decreased distance between the participant and the ophthalmologist increased the likelihood of having an eye exam. Though in a practical sense the difference was small (9 miles for those who had an exam versus 13 miles for those who did not), it was statistically significant. Lack of adequate transportation has often been found to be a significant limiting factor in receiving follow up medical care.20,21 One solution may be to provide free transportation. However, this may not be sufficient as Quigley5 found that only 9% of participants cited lack of transportation as the reason they did not appear for follow-up. A second solution would be to increase the numbers of participating Glaucoma EyeCare Program providers in low utilization areas.
Participants with diabetes in our study were found to be more likely to follow up than those who did not. Diabetic patients are known to have a high prevalence of comorbidities and disabilities.22 Participants without diabetes in our study may have had less comorbidity and, consequently, they may also have felt that their overall health status was better and did not require an eye exam.
Surprisingly, family history was not found to be significant factor for increasing the likelihood of having an eye exam. As in many previous glaucoma prevalence studies23,24, our family history data was based solely on participant recall and this may have led to an underrepresentation of family history of glaucoma.
Effectiveness of Public Service Announcements
The advantage of utilizing public service announcements when compared to glaucoma screenings is that public service announcements facilitate exposure to a wide sector of the community through mass media advertising. The Glaucoma EyeCare Program used several proven methods to increase the effectiveness of public service announcements, including the incorporation of emotional appeals (Kean LG, Albada KF. The effectiveness of anti-smoking public service announcements: do emotional appeals work? Paper presentation: International Communication Association, New Orleans Sheraton, New Orleans, LA Online May 27, 2004), the highlighting of negative consequences of the disease25 and the use of celebrity spokespersons.26 In one year of this program, 10,945 people called the toll-free telephone number. Other programs, such as that launched by The Cancer Project, are known to have reached an audience in the millions using similar mass media outlets (www.cancerproject.org; accessed June 14, 2009). Similarly, over the last 20 years, the Glaucoma EyeCare Program may have impacted hundreds of thousands of people by raising awareness of glaucoma and its risk factors, and the need for an eye exam.
Although effective in reaching their intended audience, one limitation of recruitment through public service announcements is that they depend on high-risk participants to seek their own follow up care. Our study showed that 44% of participants presented for follow up care, which is similar to the 41% reported by Quigley5 in a glaucoma screening study, but lower than the 69% reported by Mansberger.6 Differences between public service announcements and glaucoma screening studies may account for some of the differences in results. For example, the Glaucoma EyeCare Program referred only those who were eligible via a telephone interview, while the glaucoma screening studies5,6 used an abnormal Frequency Doubling Technology result and a written detailed explanation to encourage participants to seek follow-up. This written visual representation of visual field loss may have encouraged follow up with an eye exam. The glaucoma screening studies contacted participants by telephone and mail after the initial screening to encourage follow-up.5,6 Perhaps additional follow-up mail or telephone calls would have increased the proportion of participants presenting for an eye exam after a public service announcement. Indeed, a major challenge in decreasing undiagnosed glaucoma lies in getting patients into the physician’s office. A recent study by Topouzis27 found that patients who had not visited an ophthalmologist in the previous 12 months were six times more likely to have undiagnosed glaucoma as those who had. Regardless of the method employed, increased awareness of glaucoma risk factors and of the importance of having an eye exam remains a key factor in providing treatment to those who need it. Overall, our results suggest that a similar proportion of participants obtain an eye exam after a public service announcement when compared to glaucoma screening studies. Future studies should examine methods of increasing the proportion of participants who obtain an eye exam after public service announcements and glaucoma screenings.
Limitations
In order to be included in our study population, participants must have been witness to one of the public service announcements. We acknowledge that this creates a selection bias for individuals with the means and opportunity to bear witness to a public service announcement. This limitation is inherent in the nature of our study and inevitable. A second possible source of selection bias could have arisen from a relatively low participation from participating providers. Some of our results were dependent on ophthalmologists returning the outcome forms and only 24% of outcome forms were returned. We do not know the reason for this low proportion, nor why differences were present between those with and without outcome forms. However, we found similar results after adjusting for this potential bias. It is also possible that the proportion of participants who obtained an eye exam was higher than the 41% reported in this study. This may have occurred if participants chose to see an eye care provider outside of the Glaucoma EyeCare Program.
Ophthalmologists reported a large number of vision threatening conditions. These results are similar to a previous community screening for glaucoma, which also showed a high proportion of cataract, glaucoma or glaucoma suspect diagnoses.6 However, these results should be treated with caution since our methods did not include a case definition for diagnoses such as cataract, and we were unable to scrutinize medical records to verify diagnoses. These methods would increase the validity of the proportion and type of eye disease found in this study. Also, we determined that the glaucoma risk score was associated with glaucoma suspects and a combined diagnosis that included either glaucoma or glaucoma suspects. It was not predictive of a glaucoma diagnosis. Determining the predictive value of the glaucoma risk score would require an analysis including all risk scores, not just those included in this study with a threshold score ≥4.
Additionally, our study is limited by the lack of set definitions for glaucoma and glaucoma suspect. Topouzis27 found that among a population of randomly selected participants, one out of three with undiagnosed glaucoma had visited an ophthalmologist in the previous year. These results are likely influenced by provider variability in relation to diagnostic protocols. Indeed the lack of a universal set of criteria for glaucoma diagnosis continues to present challenges. A panel of glaucoma experts was recently presented with clinical case scenarios and agreement on the appropriateness and inappropriateness of treatment glaucoma suspects was measured28. While the experts were in close agreement on appropriate and inappropriate treatment, they also agreed that for 35% of the scenarios they were uncertain. For the time being, standardized criteria for glaucoma diagnosis will remain elusive.
We cannot suggest public service announcements or community screenings as the preferred approach to decrease the risk of undiagnosed glaucoma. Each method has advantages and disadvantages, and each may reach different segments of the population. We need future studies comparing these approaches.
Acknowledgments
M. Roy Wilson, James F. Martone, and other members of the Glaucoma EyeCare Program advisory committee for their thoughtful input and development of the program.
Financial Support: NEI 5 K23 EY0155501-01 (SLM)
American Glaucoma Society (SLM)
H. Dunbar Hoskins, Jr., MD Center for Quality Eye Care and EyeCare America at the Foundation of the American Academy of Ophthalmology (SF, BAW, BL)
Good Samaritan Foundation (ZH, SLM)
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Presented in part at: The American Glaucoma Society meeting, Washington D.C. March 2008 and The Association for Research in Vision and Ophthalmology Annual -Conference, May 2009
Conflict of Interest: None of the authors has a conflicting relationship with the material presented.
References
- 1.Quigley HA, Broman AT. The number of people with glaucoma worldwide in 2010 and 2020. Br J Ophthalmol. 2006;90:262–267. doi: 10.1136/bjo.2005.081224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dielemans I, Vingerling JR, Wolfs RC, et al. The prevalence of primary open-angle glaucoma in a population-based study in the Netherlands: the Rotterdam Study. Ophthalmology. 1994;101:1851–1855. doi: 10.1016/s0161-6420(94)31090-6. [DOI] [PubMed] [Google Scholar]
- 3.Leske MC, Connell AM, Schachat AP, Hyman L Barbados Eye Study Group. The Barbados Eye Study: prevalence of open angle glaucoma. Arch Ophthalmol. 1994;112:821–829. doi: 10.1001/archopht.1994.01090180121046. [DOI] [PubMed] [Google Scholar]
- 4.Mitchell P, Smith W, Attebo K, Healey PR. Prevalence of open-angle glaucoma in Australia: the Blue Mountains Eye Study. Ophthalmology. 1996;103:1661–1669. doi: 10.1016/s0161-6420(96)30449-1. [DOI] [PubMed] [Google Scholar]
- 5.Quigley HA, Park CK, Tracey PA, Pollack IP. Community screening for eye disease by laypersons: the Hoffberger program. Am J Ophthalmol. 2002;133:386–392. doi: 10.1016/s0002-9394(01)01380-0. [DOI] [PubMed] [Google Scholar]
- 6.Mansberger SL, Edmunds B, Johnson CA, et al. Community visual field screening: prevalence of follow-up and factors associated with follow-up of participants with abnormal frequency doubling perimetry technology results. Ophthalmic Epidemiol. 2007;14:134–140. doi: 10.1080/09286580601174060. [DOI] [PubMed] [Google Scholar]
- 7.Klein BE, Klein R, Sponsel WE, et al. Prevalence of glaucoma: the Beaver Dam Eye Study. Ophthalmology. 1992;99:1499–1504. doi: 10.1016/s0161-6420(92)31774-9. [DOI] [PubMed] [Google Scholar]
- 8.Coffey M, Reidy A, Wormald R, et al. Prevalence of glaucoma in the west of Ireland. Br J Ophthalmol. 1993;77:17–21. doi: 10.1136/bjo.77.1.17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sommer A, Tielsch JM, Katz J, et al. Baltimore Eye Survey Research Group. Relationship between intraocular pressure and primary open angle glaucoma among white and black Americans. Arch Ophthalmol. 1991;109:1090–1095. doi: 10.1001/archopht.1991.01080080050026. [DOI] [PubMed] [Google Scholar]
- 10.Tielsch JM, Sommer A, Katz J, et al. Racial variations in the prevalence of primary open-angle glaucoma: the Baltimore Eye Survey. JAMA. 1991;266:369–374. [PubMed] [Google Scholar]
- 11.Mason RP, Kosoko O, Wilson MR, et al. National survey of the prevalence and risk factors of glaucoma in St. Lucia, West Indies. Part I. Prevalence findings. Ophthalmology. 1989;96:1363–1368. doi: 10.1016/s0161-6420(89)32708-4. [DOI] [PubMed] [Google Scholar]
- 12.Haneuse S, Schildcrout J, Crane P, et al. Adjustment for selection bias in observational studies with application to the analysis of autopsy data. Neuroepidemiology. 2009;32:229–239. doi: 10.1159/000197389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Shadel WG, Fryer CS, Tharp-Taylor S. Uncovering the most effective active ingredients of antismoking public service announcements: the role of actor and message characteristics. Nicotine Tob Res. 2009;11:547–552. doi: 10.1093/ntr/ntp045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cooper CP, Gelb CA, Jameson H, et al. Developing English and Spanish television public service announcements to promote colorectal cancer screening. Health Promot Pract. 2005;6:385–393. doi: 10.1177/1524839905278759. [DOI] [PubMed] [Google Scholar]
- 15.Anderson RM, Wolf FM, Musch DC, et al. Conducting community-based, culturally specific, eye disease screening clinics for urban African Americans with diabetes. Ethn Dis. 2002;12:404–410. [PubMed] [Google Scholar]
- 16.Ngan R, Lam DL, Mudumbai RC, Chen PP. Risk factors for noncompliance with follow-up among normal-tension glaucoma suspects. Am J Ophthalmol. 2007;144:310–311. doi: 10.1016/j.ajo.2007.04.005. [DOI] [PubMed] [Google Scholar]
- 17.Green CA, Pope CR. Gender, psychosocial factors and the use of medical services: a longitudinal analysis. Soc Sci Med. 1999;48:1363–1372. doi: 10.1016/s0277-9536(98)00440-7. [DOI] [PubMed] [Google Scholar]
- 18.Ladwig KH, Martin-Mittag B, Formanek B, Dammann G. Gender differences of symptom reporting and medical health care utilization in the German population. Eur J Epidemiol. 2000;16:511–518. doi: 10.1023/a:1007629920752. [DOI] [PubMed] [Google Scholar]
- 19.van Wijk CM, Kolk AM. Sex differences in physical symptoms: the contribution of symptom perception theory. Soc Sci Med. 1997;45:231–246. doi: 10.1016/s0277-9536(96)00340-1. [DOI] [PubMed] [Google Scholar]
- 20.Gwira JA, Vistamehr S, Shelsta H, et al. Factors associated with failure to follow up after glaucoma screening: a study in an African American population. Ophthalmology. 2006;113:1315–1319. doi: 10.1016/j.ophtha.2006.04.017. [DOI] [PubMed] [Google Scholar]
- 21.Hoffmann RL, Rohrer WM, III, South-Paul JE, et al. The effects of barriers on health related quality of life (HRLQ) and compliance in adult asthmatics who are followed in an urban community health care facility. J Community Health. 2008;33:374–383. doi: 10.1007/s10900-008-9108-6. [DOI] [PubMed] [Google Scholar]
- 22.Kalyani RR, Saudek CD, Brancati FL, Selvin E. The association of diabetes, comorbidities, and A1C with functional disability in older adults: results from the National Health and Nutrition Examination Survey (NHANES), 1999–2006. Diabetes Care. 2010;33:1055–1060. doi: 10.2337/dc09-1597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mitchell P, Rochtchina E, Lee AJ, Wang JJ. Bias in self-reported family history and relationship to glaucoma: the Blue Mountains Eye Study. Ophthalmic Epidemiol. 2002;9:333–345. doi: 10.1076/opep.9.5.333.10335. [DOI] [PubMed] [Google Scholar]
- 24.Tielsch JM, Katz J, Sommer A, et al. Family history and risk of primary open angle glaucoma: the Baltimore Eye Survey. Arch Ophthalmol. 1994;112:69–73. doi: 10.1001/archopht.1994.01090130079022. [DOI] [PubMed] [Google Scholar]
- 25.Fishbein M, Hall-Jamieson K, Zimmer E, et al. Avoiding the boomerang: testing the relative effectiveness of antidrug public service announcements before a national campaign. Am J Public Health. 2002;92:238–245. doi: 10.2105/ajph.92.2.238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Cram P, Fendrick AM, Inadomi J, et al. The impact of a celebrity promotional campaign on the use of colon cancer screening: the Katie Couric effect. Arch Intern Med. 2003;163:1601–1605. doi: 10.1001/archinte.163.13.1601. [DOI] [PubMed] [Google Scholar]
- 27.Topouzis F, Coleman AL, Harris A, et al. Factors associated with undiagnosed open-angle glaucoma: the Thessaloniki Eye Study. Am J Ophthalmol. 2008;145:327–335. doi: 10.1016/j.ajo.2007.09.013. [DOI] [PubMed] [Google Scholar]
- 28.Appropriateness of Treating Glaucoma Suspects RAND Study Group. For which glaucoma suspects is it appropriate to initiate treatment? Ophthalmology. 2009;116:710–716. doi: 10.1016/j.ophtha.2008.12.065. [DOI] [PMC free article] [PubMed] [Google Scholar]