Abstract
Carney triad (CT) describes the association of paragangliomas (PGLs) with gastrointestinal stromal tumours (GISTs) and pulmonary chondromas (PCH). A number of other lesions have been described in the condition including pheochromocytomas, oesophageal leiomyomas and adrenocortical adenomas; CT is a novel form of multiple endocrine neoplasia (MEN), a genetic condition with a female predilection. Inactivating mutations of the mitochondrial complex II succinate dehydrogenase (SDH) enzyme subunits SDHB, SDHC and SDHD have been found in familial and sporadic PGLs, and gain-of-function mutations of the oncogenes c-kit (KIT) and platelet-derived growth factor receptor A (PDGFRA) cause sporadic and familial GISTs. We recently reported an international series of patients with CT, 34 females and three males (median age of presentation 21 years) who did not carry SDHA, SDHB, SDHC, SDHD, KIT or PDGFRA gene mutations. Comparative genomic hybridization revealed a number of DNA copy number changes. The most frequent and greatest contiguous change was a deletion within the 1pcen13-q21 region, which harbours the SDHC gene. Another frequent change was loss of 1p. Although GISTs showed more frequent losses of 1p than PGLs, the pattern of chromosomal changes was similar in the two tumours despite their different tissue origin and histology; the findings were consistent with a common genetic aetiology of these two tumours in CT. In a separate condition, in which the association (or dyad) of GISTs with PGLs is inherited in an autosomal dominant manner (Carney–Stratakis syndrome, CSS), germline mutations of the SDHB, SDHC and SDHD genes (but not KIT or PDFGRA) were found; GISTs in this condition were caused by SDH deficiency. We conclude that CT is a novel MEN syndrome whose genetic defect remains elusive. CSS is caused by SDH defects, suggesting that sarcomas (GISTs) can be caused by defective mitochondrial oxidation, consistent with recent data implicating this enzyme in a variety of endocrine and other tumours. The above have clinical implications (i) for patients with GISTs that are cKIT- and PDGFRA-mutation negative: these tumours are usually resistant to treatment with currently available tyrosine kinase inhibitors and may be part of a syndrome such as CT or CSS; and (ii) for patients with an inherited PGL syndrome, family history should be explored to identify any other tumours in the family, and in particular other endocrine lesions and GISTs.
Introduction: Carney triad
Carney triad (CT) describes the association of paragangliomas (PGLs) with gastrointestinal stromal tumours (GISTs) and pulmonary chondromas (PCH) (Online Mendelian Inheritance in Man, OMIM, catalogue number 604287) [1]. The condition was first described as the ‘triad of gastric leiomyosarcoma, functioning extra-adrenal paraganglioma and pulmonary chondroma’ [2]. Initially, GISTs were thought to arise from the smooth muscle [2, 3] (hence the term ‘leiomyosarcoma’) but, later, they were shown to originate from the interstitial cells of Cajal (ICCs) [4, 5]. The condition was called ‘Carney triad’ [6], but it is in fact a multiple neoplasia syndrome affecting mostly females and predisposing to a variety of tumours including bilateral or unilateral adrenocortical adenomas (ACA) that are usually nonfunctioning [4, 7].
Although a few cases with family history of PGLs and GISTs were included within the original cohort patients with CT [4], it was recently recognized [8] that the dyad of ‘paraganglioma and gastric stromal sarcoma’ or the ‘Carney–Stratakis syndrome’ (CSS) which affects both males and females and is not associated with PCH [9] is a separate condition that is transmitted by autosomal dominant inheritance. The syndrome is listed in OMIM as a separate entity (OMIM#606864) and has been since reported in a number of kindreds [10] (see below).
Carney triad and CSS have been reported in all races and in several countries; there appears to be no specific ethnic or geographical predilection. The prevalence of the two syndromes is unknown; CSS is probably more frequent than CT (see below). Once the familial cases of CSS are removed from the original cohort of patients with CT, there appear to be no inherited cases of the triad. In the latest report [4], 77 nonfamilial cases of CT were reported; 66 female and 11 male. One-fifth of the patients had the three tumours; the remainder had two of the three, usually gastric GIST and PCH. ACAs were identified in one-eighth of the patients. Oesophageal leiomyoma was also suggested as an additional, probable component [4].
In the absence of patients with similarly affected relatives, can one consider CT a genetic disorder? The rarity of the individual components of this condition in the general population, their coexistence in affected individuals and the multiplicity and young age of tumour occurrence, all suggest a specific genetic defect. Positional cloning of the responsible gene(s), however, is hampered by the absence of inherited cases. We recently analysed DNA from 37 CT patients and/or their tumours for the coding sequence of the SDHB, SDHC, SDHD, KIT, and PDGFRA genes that have been involved in the pathogenesis of familial PGLs [10]. We also sequenced the gene coding for the SDH subunit A (SDHA), because polymorphisms of this gene had been potentially implicated in predisposition to PGLs [11]. In addition, we employed comparative genomic hybridization (CGH) to identify chromosomal loci associated with CT by comparing DNA extracted from peripheral blood cells to tumour DNA, or in the absence of the former, genetic material obtained from different tumours from the same patient [10].
There were no coding sequence mutations in any of the screened genes [10]. The most frequent and greatest contiguous change detected by tumour CGH studies was deletion of the 1cen-q21 chromosomal region involving the SDHC gene. Other alterations were also detected, including loss of the 1p region. Significantly, PGLs and GISTs in CT shared the same genetic alterations despite their different tissue origin. These data excluded known genes as the cause of CT and point to a common genetic aetiology for its component tumours.
Patients and candidate gene sequencing
We studied an international series of patients with CT; 34 females and three males, with a median age at presentation of 21 years (Table 1). CTRS2 and CTR04.01 were cases 3 and 1, respectively, in the reports by Carney et al. [2] and Carney [3]. CTR04.01 had a peripheral blood karyotype 46,XX, inv(9)(p11:q13), a variant found in the general population at a frequency of up to 1.5% and only rarely associated with phenotypic abnormalities [12]. CTR04.01 was developmentally normal but was born with complete and partial agenesis of the left and right external ear; she underwent left adrenalectomy for an ACA and subclinical Cushing syndrome at the age of 47 years. CTRS2 had multiple GIST metastases to the liver and elsewhere. CTR05.01, CTRS5T, CTR06.01, CTRS.13, CTRS21 and CTR08.03 are described in detail by Sigmund et al. [13], Cameron et al. (second case in that report) [14], Wintermark et al. [15], McLaughlin et al. [16], Grace et al. [6] and Convery et al. [17]. CTR06.01 had also ACA [15]. Patients CTRS21, CTRS23, CTRS42 and CTR07.03 and the archived specimens CT.1 to CT.24 were included in the last series on CT by Carney [4]; sample B177/B178 was from the proband with CT, parotid gland tumours and breast cancer; the patient also had a brother with Hirschprung disease. The family was reported by Scopsi et al. [18]. Finally, samples CTRS19 and CTRS41 were newly identified patients with CT that have not been reported. As mentioned above, there were no coding sequence mutations of the KIT, RET, SDHA, SDHB, SDHC, SDHD and PDGFRA genes in the germline and tumour DNA samples. A number of SDHA sequence variants were identified but they were relatively common polymorphisms (Table 2). There were no major deletions or other chromosomal rearrangements detected in any of the samples for the chromosomal loci of the candidate genes.
Table 1.
Patients with the triad of gastric leiomyosarcoma, functioning extra-adrenal paraganglioma and pulmonary chondroma (Carney triad)
| Patient | Id | Sex | Age | Tumours | Other | Reference |
|---|---|---|---|---|---|---|
| CTRS2 | 1 | F | 15 | GIST, PGL | Chest X-ray normal; metastatic GIST; multiple PGLs (mediastinal) | Case 3, Carney et al. [2] and Carney [3] |
| CTR04.01 | 2 | F | 12 | GIST, PGL, PCH | Peripheral blood karyotype is 46,XX,inv(9) (p11:q13); born with complete and partial agenesis of the left and right external ear, respectively; she has had multiple PGLs (neck) and PCHs and recurrent GIST; left adrenocortical adenomas (subclinical Cushing) | Case 1, Carney et al. [2] and Carney [3] |
| CTR05.01 | 3 | F | 17 | GIST, PGL, PCH | Multiple GISTs (one malignant); multiple PCH; one PGL (retroperitoneal) | Sigmund et al. [13] |
| CTRS.5T | 4 | F | 29 | GIST, PGL, PCH | Multiple GIST (metastatic); multiple PCH; one PGL (gastric); left adrenocortical tumour (nonfunctional) | Case 2, Cameron et al. [14] |
| CTRS.6 | 5 | F | 14 | GIST, PGL, PCH | Multiple GIST (metastatic) | |
| CTR06.01 | 6 | F | 18 | GIST, PGL, PCH | Multiple GIST (metastatic); PGL (neck and abdominal); left adrenocortical adenoma | Wintermark et al. [15] |
| CTRS.13 | 7 | F | 26 | GIST, PCH | GIST (malignant); multiple PCH | McLaughlin et al. [16] |
| CTRS.19 | 8 | F | 23 | GIST, PCH | GIST (multiple); multiple PCH | |
| CTRS.21 | 9 | F | 21 | GIST, PGL | GIST (multiple); PGL (cardiac) | Grace et al. [6] |
| CTRS.23 | 10 | F | 25 | GIST, PGL | GIST (metastatic); adrenocortical tumour | |
| CTRS.27 | 11 | F | 26 | GIST, PCH | GIST (multiple, gastric); lymphoma | |
| CTRS.41 | 12 | F | 12 | GIST, PGL | GIST (multiple, metastatic); PGL (para-aortic) | |
| CTRS.42 | 13 | F | 28 | GIST, PGL, PCH | GIST (multiple, metastatic); PGL; adrenocortical adenoma | Carney et al. [4] |
| CTR07.03 | 14 | F | 17 | GIST, PGL, PCH | GIST (multiple, metastatic); PGL; PCH (mutliple) | Carney et al. [4] |
| CTR08.03 | 15 | F | 21 | GIST, PGL, PCH | GIST (multiple, metastatic); PGL; PCH (mutliple) | Convey et al. [17] |
| CTR09.01 | 16 | F | 26 | GIST, PGL, PCH | GIST (multiple, metastatic); PGL (metastatic); PCH (mutliple) | |
| CTR10.01 | 17 | F | 21 | GIST, PGL | GIST (multiple, metastatic); PGL (nonfunctioning, abdominal); adrenocortical adenoma | |
| B177/B178 | 18 | F | 25 | GIST, PGL, PCH | GIST (metastatic), multiple PGLs (mediastinal) and PCHs; right ductal breast cancer at age 50 years | Scopsi et al. [18] |
| CT.1 | 19 | F | 19 | GIST, PGL, PCH* | ||
| CT.2 | 20 | F | 22 | GIST, PCH* | ||
| CT.3 | 21 | F | 21 | GIST, PCH* | ||
| CT.4 | 22 | F | 13 | GIST, PCH* | ||
| CT.6 | 23 | M | 21 | GIST, PCH* | ||
| CT.11 | 24 | F | 11 | GIST, PCH* | ||
| CT.12 | 25 | F | 26 | GIST, PCH* | ||
| CT.13 | 26 | F | 44 | GIST, PCH* | ||
| CT.14 | 27 | F | 19 | GIST, PCH* | ||
| CT.15 | 28 | M | 36 | GIST, PCH* | ||
| CT.16 | 29 | F | 17 | GIST, PCH* | ||
| CT.17 | 30 | F | 16 | GIST, PCH* | ||
| CT.18 | 31 | F | 9 | GIST, PCH* | ||
| CT.19 | 32 | F | 13 | GIST, PCH* | ||
| CT.20 | 33 | F | 7 | GIST, PGL* | ||
| CT.21 | 34 | F | 11 | GIST, PGL* | ||
| CT.22 | 35 | F | 11 | GIST, PCH* | ||
| CT.23 | 36 | F | 19 | GIST, PCH* | ||
| CT.24 | 37 | M | 30 | GIST, PGL* |
GIST, gastrointestinal stromal tumour (initially referred to as gastric leiomyosarcoma); PCH, pulmonary chondroma; PGL, paraganglioma.
DNA from samples CT.1 to CT.24 (patients 19 to 37) was obtained from archival material; these patients were included in Carney et al. [4].
Table 2.
SDHA polymorphic sequences
| Genomic region | Sequence | Frequency in CT (37) | Frequency in controls (45) |
|---|---|---|---|
| Promoter | -82 ins. T hom | 0 | 0 |
| -82 ins. T het | 11 | 10 | |
| Intron 1 | IVS1 +65 G>A* | 8 | 13 |
| IVS1 +65 A | 1 | 7 | |
| Intron 5 | IVS5-12 ins.C het | 1 | 1 |
| IVS5-12 ins.C hom | 0 | 0 | |
| Exon 6 | 684 T>C* | 11 | 8 |
| 684 C | 8 | 19 | |
| Exon 7 | 891 T>C | 11 | 12 |
| 891 C | 16 | 23 | |
| Exon 15 | 1932 G>A + 1969 G>A | 11 | 3 |
| 1932 A + 1969 A | 0 | 6 |
Het, heterozygous; hom, homozygous.
In these two polymorphisms, IVS1+65 G>A and 684 T>C, Fisher's exact test shows statistically significant higher frequency of the ‘mutant’ alleles G and T in the control population. The significance of this finding is unclear; it probably reflects an error in the existing publicly available information concerning the SDHA sequence and the frequency of its polymorphisms.
Tumour culture chromosome analysis and CGH results
Carney triad tumours, histological diagnoses, karyotypes and DNA copy number changes are reported elsewhere [10]. CGH was performed on a total of 41 tumours: 31 GIST, six PGL, three PCH and one ACA. For six of the tumours (five GIST, one PCH), primary culture karyotypes were obtained; with the exception of a polyclonal 46,XX, t(5;7)(q31:q11.2) abnormality detected in 2 of 30 cells from GIST CTRS9, there were no other abnormalities. Overall, 21 specimens showed no significant CGH changes; four were PGLs. Of the 41 GISTs, 17 (41.5%) showed no changes, a surprisingly large number given that almost 90% of sporadic GISTs have detectable chromosomal imbalances [10].
On the other hand, 10 of 15 benign tumours (75%) and five of six (83%) metastatic lesions showed chromosomal changes. Information was not available on the nature of tumour (benign versus metastatic) in the remaining lesions. There were more gains than losses in benign tumours (16 versus 12). The average number of alterations in benign tumours was 2.1 (range: 0–5). Amongst metastatic lesions, the average number of CGH changes was 3.8 (range, 0–6); gains were more frequent than losses (14 versus 12).
In total, 15 chromosomal regions showed gains in benign tumours. However, 11 were represented in only one sample each. Three chromosomal regions, 6 (6p and 6q), 15q and 17q, were involved in two cases (13%). Losses were identified on chromosomes 1p and 1q (61%) and 11p. In metastatic tumours, 15 chromosomal regions were involved in gains but only two regions, 15q and chromosome 4, showed gains in more than one sample.
Gains of five chromosomal regions that were present in at least one sample were identified in both benign and metastatic tumours. The latter showed more losses than the former; chromosome 1 losses were the most frequent (66%). The minimal region of losses harboured the SDHC locus; 1p33–36.4 also showed losses in both benign and malignant tumours (15%). Some other regions on chromosomes 3q, 11q, 16q and 17p had losses but those on 3q, 11q and 17p were detected in only one sample each. Loss of 16q was present in two metastatic lesions.
CGH, fluorescent in situ hybridization (FISH) and loss-of-heterozygosity (LOH) studies
Tumours that showed losses of 1q region by CGH (samples CTRS9, CTRS5T, CTRS6, CTRS7, CTRS10, CTRS13, CTRS19, CTRS21 and CTRS36) were subjected to interphase FISH, using the bacterial artificial chromosome (BAC) RP11 0338-B-10 containing the SDHC gene. FISH detected loss of the region in seven of the samples [10]. In these samples, 38–70% of cells showed only one signal of the probe used. In addition to these tumours, we also analysed three GISTs that were not included in the CGH analysis, but belonged to patients CTR07.07.03, CTR08.03 and CTR09.01; two also showed the loss of 1q21 region. Finally, LOH studies confirmed losses of the 1q21 region in these samples [10].
Array CGH was performed on a sample that showed minimal or no abnormalities in the previous analysis (CTRS2). The data are shown in Table 3. This sample was also selected because of the good quality of its DNA and the fact that it was obtained from a GIST excised from case 3 of the original reports of the syndrome by Carney et al. [2] and Carney [3] (Fig. 1). Although minimal changes were shown (confirming the lack of significant abnormalities upon the first CGH analysis), most of the single BAC changes were seen on chromosomal regions that were identified in other tumours (Table 2); chromosome 1 involvement included the 1p and 1q regions.
Table 3.
Array CGH analysis in sample CTRS2.
| Clone | Cyto Locn | Cy5 test log ratios | Cy3 test log ratios | DNA change | Comment |
|---|---|---|---|---|---|
| RP11-421C4 | 1p36.3–1p36.3 | 0.273 | -0.257 | Gain | Single BAC change |
| RP4-703E10 | 1p36.32–1p36.33 | 0.389 | -0.745 | Gain | Polymorphism |
| RP11-452O22 | 1q21.1–1q22 | 0.337 | -0.676 | Gain | Polymorphism |
| RP5-1016N21 | 1q42.13–1q43 | 0.225 | -0.204 | Gain | Single BAC change |
| RP11-91M15 | 3q11.2–3q11.2 | 0.209 | -0.326 | Gain | Single BAC change |
| RP5-963K6 | 4q35.2 | 0.432 | -0.431 | Gain | Single BAC change |
| RP11-90A9 | 5q14–5q14 | 0.414 | -0.366 | Gain | Single BAC change |
| RP1-304O5 | 6q12–6q13 | 0.455 | -0.266 | Gain | Single BAC change |
| RP11-89A20(E) | 7q11.23 | -0.288 | 0.239 | Loss | Single BAC change |
| RP11-18-L2 | 8p23.1 | 0.52 | -0.227 | Gain | Polymorphism |
| RP11-89C6 | 9p21.3–9p22 | 0.18 | -0.253 | Gain | Single BAC change |
| RP11-80F13 | 9q31.3–9q31.3 | -0.183 | 0.178 | Loss | Single BAC change |
| RP11-88B18 | 10q21.1–10q21.1 | -0.209 | 0.178 | Loss | Single BAC change |
| RP1-137E24 | 10q26.3 | 0.26 | -0.356 | Gain | Possible gain |
| RP11-108K14 | 10q26.3–10q26.3 | 0.236 | -0.274 | Gain | Possible gain |
| RP1-44H16 | 11p15.5 | 0.217 | -0.234 | Gain | Single BAC change |
| RP5-908H22 | 11p15.5 | 0.216 | -0.232 | Gain | Single BAC change |
| c197-2 | 17p13.3 | 0.189 | -0.196 | Gain | Possible gain |
| c197-4 | 17p13.4 | 0.229 | -0.302 | Gain | Possible gain |
| c197-9 | 17p13.5 | 0.371 | -0.424 | Gain | Possible gain |
| RP11-79F15 | 19p13.2–19p13.2 | -0.476 | 0.483 | Loss | Single BAC change |
| RP4-788L20 | 20p11.21–20p11.23 | 0.294 | -0.179 | Gain | Single BAC change |
| RP3-355C18 | 22q13.3–22q13.3 | 0.207 | -0.291 | Gain | Single BAC change |
| CTD-3018K1 | 22q13.33 | 0.477 | -0.392 | Gain | Single BAC change |
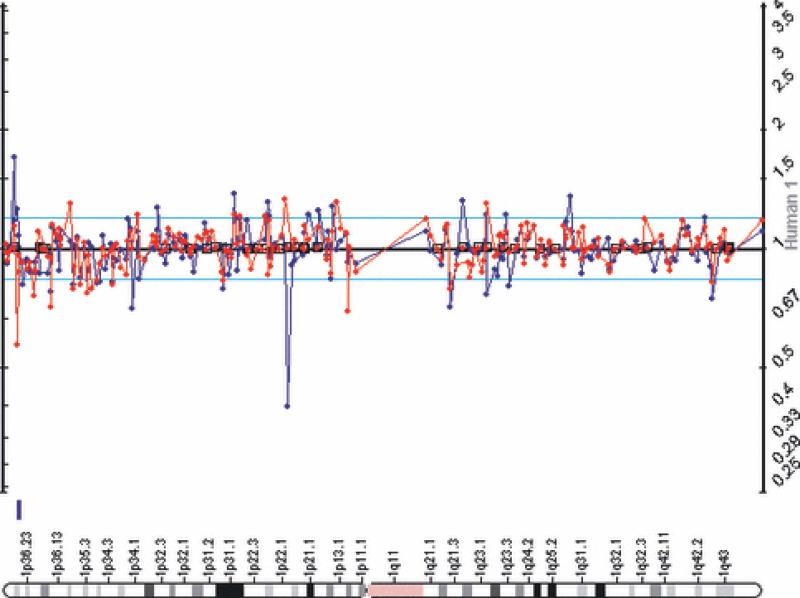
Figure 1.
Array CGH was performed on a sample that showed minimal or no abnormalities in the previous analysis, CTRS2 from case 3 of the original reports of the syndrome by Carney et al. [2] and Carney [3]. Table 3 lists the genome-wide changes; in this figure, chromosome 1 data showed involvement of the 1p and 1q regions.
Tumour type and CGH abnormalities
There were small differences between GISTs and PGLs in chromosomal involvement: 17q gains were detected only in PGLs (CTRS7 and CTRS19). There was only one PCH (out of the three investigated) that had CGH abnormalities (CTRS13); it demonstrated chromosome 6 gains, gains that were also detected in one adrenal tumour that was studied, a benign ACA (CTRS14). 1q losses were present in both the PCH and ACA tumours, as well as in three of the six PGLs; 1p losses were seen in two PGLs and five of the GISTs.
Summary of the findings in CT
This genetic investigation of 37 patients and 41 CT tumours is the most comprehensive ever performed in this disease. A total of five patients with CT who underwent genetic analysis has recently been reported in three case studies [19–21]. GISTs in these patients were negative for KIT or PDGFRA mutations [19–21]; one case (with multiple extra-adrenal paragangliomas) was also screened for SDHB, SDHC and SDHD mutations and none was found [19]. Three more cases of CT were included in another series; none had mutations in the screened genes and the CGH abnormalities were similar to those reported here [22]. Thus, to date, more than half of the known cases of CT worldwide have been screened for the genes that are linked with the sporadic or genetic forms of two of the individual tumours that comprise the syndrome (GIST and PGL) and no mutations have been found.
This suggests that other as yet unidentified gene(s) are responsible for CT. Further support to this notion is provided by the clinical and molecular analysis of KIT mutation-negative GISTs: KIT mutations are rare in childhood GISTs, tumours that occur predominantly in females, mostly during the second decade of life and with a gastric predilection [23] – all features of GISTs associated with CT [3, 4]. More recent studies show that KIT- and PPDFGRA mutation-negative GISTs have a distinct pattern of gene expression [24, 25].
The CGH results are consistent with the different genetic background of CT-associated GISTs and PGLs: In sporadic GISTs, the most common alterations are 14q, 22q and 1p losses, seen in 70%, 60% and 50% of the tumours respectively [24]. In the CT tumours we studied, 1p loss was seen relatively frequently (two PGLs and five GISTs) but 14q and 22q losses occurred in only one GIST each. 1q loss was by far the most frequent genetic abnormality in CT-associated GISTs and PGLs and was present in the single adrenal adenoma and one of three lung chondromas we studied.
In conclusion, the triad of PGL, GIST and PCH, a multiple neoplasia syndrome that includes adrenocortical and other endocrine tumours, is not due to SDH-inactivating or KIT and PDGFRA-activating mutations. Chromosome 1 and other copy number changes distinguished these tumours from their sporadic and other familial counterparts and point to a common, yet elusive, genetic cause of CT.
The dyad of ‘paraganglioma and gastric stromal sarcoma’ (CSS)
In 2002, we described a total of 12 patients, seven males and five females, in five unrelated families in which the PGL and GIST were inherited in an apparently autosomal dominant manner, with incomplete penetrance [8]. Paragangliomas were multicentric and gastric stromal sarcomas multifocal in all patients, supporting the inherited nature of this predisposition. The condition has been referred to as the dyad of ‘paraganglioma and gastric stromal sarcoma’ or the CSS (OMIM#606864) [1, 9].
We recently reported germline mutations of the SDHB, SDHC and SDHD genes in patients with the dyad and in their tumours [26, 27]: GISTs from the patients showed allelic losses around the SDHB and SDHC chromosomal loci pointing to a tumour-suppressor function of SDH subunits in these neoplasms. None of the patients had mutations of the PDGFRA or KIT genes.
GISTS and SDH deficiency: a new molecular pathway (and therapeutic target?) for GISTs
Although rare, GISTs are the most common mesenchymal tumours (5000 new cases per year in the United States) of the gastrointestinal tract with frequent occurrence in the muscular wall of the stomach (70%), small bowel (10–20%) and, at lower frequencies, in the oesophagus, omentum and mesentery [5, 28, 29]. The median age at diagnosis is around 60 years. The 5-year survival in patients with large tumour size and high mitotic index is less than 40%, indicating poor prognosis [29].
GISTs originate from stem cells with characteristics of the ICCs [5], the pacemaker cells which regulate peristalsis in the digestive tract. Similar to ICCs, up to 95% of GISTs express the receptor tyrosine kinase KIT whose immuno-histochemical detection (CD117) and that of the marker CD34 (haematopoietic progenitor cell antigen) is typical of the lesion [18]. In recent years it has been established that 75–80% of sporadic GISTs harbour somatic gain-of-function mutations in the KIT gene encoding the c-KIT protein; an additional 7% of sporadic GISTs harbour mutations in the functionally related PDGFRA gene [5, 27–29]. In both cases germline missense mutations or small in frame deletions generate constitutively activated tyrosine kinase receptors with ligand-independent autophosphorylation and downstream signalling. To date, germline KIT and PDGFRA mutations have also been identified in several families with familial GIST [5, 27–29]. Polyclonal diffuse hyperplasia of ICCs within the myenteric plexus is considered the primary effect of c-KIT constitutive activation [5]. Mutations in KIT and PDGFRA, either somatic or germline, are mutually exclusive events.
The existence of GISTs that lack detectable somatic mutations in either KIT or PDGFRA suggests that a different signalling pathway of tumourigenesis is likely to be involved in the pathogenesis of these neoplasms [24, 30]. The identification of germline loss-of-function mutation in the SDHB, SDHC and SDHD genes in the majority of the patients reported worldwide with the familial syndrome of ‘paraganglioma and gastric stromal sarcoma’ led to the uncovering of a new molecular aetiology for GISTs. These GISTs displayed clear losses of the wild type allele indicating a tumour suppressor role for the SDH enzyme in GISTs that are negative for KIT and PDGFRA mutations. These findings link mesenchymal tumours to the mitochondrial tumour suppressor gene pathway opening a new field of research and potentially identifying a new molecular target for GISTs that are not responsive to treatment with tyrosine kinase inhibitors [24, 30].
Conclusions – clinical implications
In summary, two new syndromes, CT and CSS, have entered the realm of multiple endocrine neoplasias in the last 5 years [31]. Both are linked to predisposition to PGLs and pheochromocytomas, and one is due to SDHB, SDHC and SDHD mutations that are becoming amongst the most frequently encountered genetic defects in a variety of endocrine tumours [32].
Although both CT and CSS are rare conditions, CSS is probably quite more frequent than what the current numbers indicate (so far, about 20 kindreds are known to us with the dyad or CSS). CSS may be particularly prevalent amongst young patients with GISTs that are negative for KIT and PDGFRA mutations.
Doctors who take care of patients with apparently ‘sporadic’ PGLs or GISTs should always obtain detailed medical and family histories as often these conditions have decreased penetrance and variable expression. A search for CT or CSS should always follow the detection of a KIT- or PDFGRA-mutation-negative GIST, especially in the younger patient.
Acknowledgements
This work was supported by NIH intramural project Z01-HD-000642-04 to Dr C.A. Stratakis, and, in part, by a Bench-to-Bedside Award from the Office of Rare Disorders (ORD) and the National Institute of Child Health & Human Development (NICHD), NIH, for the study of the ‘Genetics of inherited paragangliomas and gastric stromal tumors associated with adrenal and other tumors’.
References
- 1.Online Mendelian Inheritance in Man, OMIM (TM) McKusick-Nathans Institute for Genetic Medicine; Johns Hopkins University and National Center for Biotechnology Information, National Library of Medicine; Baltimore, MD: Bethesda, MD: [26 February 2007]. http://www.ncbi.nlm.nih.gov/omim/ [Google Scholar]
- 2.Carney JA, Sheps SG, Go VLW, Gordon H. The triad of gastric leiomyosarcoma, functioning extra-adrenal paraganglioma and pulmonary chondroma. N Engl J Med. 1977;296:1517–8. doi: 10.1056/NEJM197706302962609. [DOI] [PubMed] [Google Scholar]
- 3.Carney JA. The triad of gastric epithelioid leiomyosarcoma, pulmonary chondroma, and functioning extra-adrenal paraganglioma: a five-year review. Medicine (Baltimore) 1983;62:159–69. doi: 10.1097/00005792-198305000-00003. [DOI] [PubMed] [Google Scholar]
- 4.Carney JA. Gastric stromal sarcoma, pulmonary chondroma, and extra-adrenal paraganglioma (Carney triad): natural history, adrenocortical component, and possible familial occurrence. Mayo Clin Proc. 1999;74:543–52. doi: 10.4065/74.6.543. [DOI] [PubMed] [Google Scholar]
- 5.Kindblom LG, Remotti HE, Aldenborg F, Meis-Kindblom JM. Gastrointestinal pacemaker cell tumor (GIPACT): gastrointestinal stromal tumors show phenotypic characteristics of the interstitial cells of Cajal. Am J Pathol. 1998;152:1259–69. [PMC free article] [PubMed] [Google Scholar]
- 6.Grace MP, Batist G, Grace WR, Gillooley JF. Aorticopulmonary paraganglioma and gastric leiomyoblastoma in a young woman. Am J Med. 1981;70:1288–92. doi: 10.1016/0002-9343(81)90840-8. [DOI] [PubMed] [Google Scholar]
- 7.Perry CG, Young WF, Jr, McWhinney SR, et al. Functioning paraganglioma and gastrointestinal stromal tumor of the jejunum in three women: syndrome or coincidence. Am J Surg Pathol. 2006;30:42–9. doi: 10.1097/01.pas.0000178087.69394.9f. [DOI] [PubMed] [Google Scholar]
- 8.Carney JA, Stratakis CA. Familial paraganglioma and gastric stromal sarcoma: a new syndrome distinct from the Carney triad. Am J Med Genet. 2002;108:132–9. doi: 10.1002/ajmg.10235. [DOI] [PubMed] [Google Scholar]
- 9.Daum O, Vanecek T, Sima R, Michal M. Gastrointestinal stromal tumor: update. Klin Onkol. 2006;19:203–11. [Google Scholar]
- 10.Matyakhina L, Bei TA, McWhinney SR, et al. Genetics of Carney triad: recurrent losses at chromosome 1 but lack of germline mutations in genes associated with paragangliomas and gastrointestinal stromal tumors. J Clin Endocrinol Metab. 2007;92:2938–43. doi: 10.1210/jc.2007-0797. [DOI] [PubMed] [Google Scholar]
- 11.Baysal BE, Lawrence EC, Willett-Brozick JE, Ferrell RE. Sequence analysis of succinate dehydrogenase subunit A gene (SDHA) for paraganglioma tumor susceptibility. Am J Hum Genet. 2004;75:91. (Abstract 384) [Google Scholar]
- 12.Starke H, Seidel J, Henn W, et al. Homologous sequences at human chromosome 9 bands p12 and q13-21.1 are involved in different patterns of pericentric rearrangements. Eur J Hum Genet. 2002;10:790–800. doi: 10.1038/sj.ejhg.5200889. [DOI] [PubMed] [Google Scholar]
- 13.Sigmund G, Buitrago-Tellez CH, Torhorst J, Steinbrich W. Radiology of gastrointestinal stromal tumors (GIST) and a case of Carney syndrome. Rofo. 2000;172:287–94. doi: 10.1055/s-2000-121. [DOI] [PubMed] [Google Scholar]
- 14.Cameron S, Ramadori G, Fuzesi L, et al. Successful liver transplantation in two cases of metastatic gastrointestinal stromal tumors. Transplantation. 2005;80:283–4. doi: 10.1097/01.tp.0000164141.34293.6b. [DOI] [PubMed] [Google Scholar]
- 15.Wintermark P, Boubaker A, Gebhard S, et al. Adrenal mass in Carney triad. J Endocr Genet. 2001;2:229–40. [Google Scholar]
- 16.McLaughlin SJ, Dodge EA, Ashworth J, Connors J. Carney's triad. Aust N Z J Surg. 1988;58:679–81. doi: 10.1111/j.1445-2197.1988.tb07583.x. [DOI] [PubMed] [Google Scholar]
- 17.Convery RP, Grainger AJ, Bhatnagar NK, Scott D, Bourke SJ. Lung abscess complicating chondromas in Carney's syndrome. Eur Respir J. 1998;11:1409–11. doi: 10.1183/09031936.98.11061409. [DOI] [PubMed] [Google Scholar]
- 18.Scopsi L, Collini P, Muscolino G. A new observation of the Carney's triad with long follow-up period and additional tumors. Cancer Detect Prev. 1999;23:435–43. doi: 10.1046/j.1525-1500.1999.99047.x. [DOI] [PubMed] [Google Scholar]
- 19.Diment J, Tamborini E, Casali P, Gronchi A, Carney JA, Colecchia M. Carney triad: case report and molecular analysis of gastric tumor. Hum Pathol. 2005;36:112–6. doi: 10.1016/j.humpath.2004.10.003. [DOI] [PubMed] [Google Scholar]
- 20.Colwell AS, D'Cunha J, Maddaus MA. Carney's triad paragangliomas. J Thorac Cardiovasc Surg. 2001;121:1011–2. doi: 10.1067/mtc.2001.112820. [DOI] [PubMed] [Google Scholar]
- 21.Spatz A, Bressac-de-Paillerets B, Raymond E. Soft tissue sarcomas. Case 3. Gastrointestinal stromal tumor and Carney's triad. J Clin Oncol. 2004;22:2029–31. doi: 10.1200/JCO.2004.07.152. [DOI] [PubMed] [Google Scholar]
- 22.Agaimy A, Pelz AF, Corless CL, et al. Epithelioid gastric stromal tumours of the antrum in young females with the Carney triad: a report of three new cases with mutational analysis and comparative genomic hybridization. Oncol Rep. 2007;18:9–15. [PubMed] [Google Scholar]
- 23.Price VE, Zielenska M, Chilton-MacNeill S, Smith CR, Pappo AS. Clinical and molecular characteristics of pediatric gastrointestinal stromal tumors (GISTs). Pediatr Blood Cancer. 2005;45:20–4. doi: 10.1002/pbc.20377. [DOI] [PubMed] [Google Scholar]
- 24.Miselli F, Millefanti C, Conca E, et al. PDGFRA immunostaining can help in the diagnosis of gastrointestinal stromal tumors. Am J Surg Pathol. 2008;32:738–43. doi: 10.1097/PAS.0b013e31815c47e8. [DOI] [PubMed] [Google Scholar]
- 25.Gunawan B, Von Heydebreck A, Sander B, et al. An oncogenetic tree model in gastrointestinal stromal tumours (GISTs) identifies different pathways of cytogenetic evolution with prognostic implications. J Pathol. 2007;211:463–70. doi: 10.1002/path.2128. [DOI] [PubMed] [Google Scholar]
- 26.McWhinney SR, Pasini B, Stratakis CA, from the Carney Triad & Carney–Stratakis Dyad/Syndrome Consortium Mutations of the genes coding for the succinate dehydrogenase subunit genes in familial gastrointestinal tumors. N Engl J Med. 2007;357:1054–6. doi: 10.1056/NEJMc071191. [DOI] [PubMed] [Google Scholar]
- 27.Pasini B, McWhinney SR, Bei T, et al. Clinical and molecular genetics of patients with the Carney–Stratakis syndrome and germline mutations of the genes coding for the succinate dehydrogenase subunits SDHB, SDHC, and SDHD. Eur J Hum Genet. 2008;16:79–88. doi: 10.1038/sj.ejhg.5201904. [DOI] [PubMed] [Google Scholar]
- 28.Fletcher CD, Berman JJ, Corless C, et al. Diagnosis of gastrointestinal stromal tumors: a consensus approach. Hum Pathol. 2002;33:459–65. doi: 10.1053/hupa.2002.123545. [DOI] [PubMed] [Google Scholar]
- 29.Miettinen M, El-Rifai W, Sobin LH, Lasota J. Evaluation of malignancy and prognosis of gastrointestinal stromal tumors: a review. Hum Pathol. 2002;33:478–83. doi: 10.1053/hupa.2002.124123. [DOI] [PubMed] [Google Scholar]
- 30.Antonescu CR. Gastrointestinal stromal tumor (GIST) pathogenesis, familial GIST, and animal models. Semin Diagn Pathol. 2006;23:63–9. doi: 10.1053/j.semdp.2006.08.003. [DOI] [PubMed] [Google Scholar]
- 31.Alevizaki M, Stratakis CA. Multiple endocrine neoplasias 2008: advances and challenges for the future. J Intern Med 2009. 266:1–4. doi: 10.1111/j.1365-2796.2009.02108.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Pasini B, Stratakis CA. SDH mutations in tumourigenesis and inherited endocrine tumors: lessons from the phaeochromocytoma-paraganglioma syndromes. J Intern Med. 2009;266:19–42. doi: 10.1111/j.1365-2796.2009.02111.x. [DOI] [PMC free article] [PubMed] [Google Scholar]