Abstract
Plasmodium vivax causes debilitating but usually non-lethal malaria in most of Asia and South America. Prevention of relapse after otherwise effective therapy for the acute attack requires a standard daily dose of primaquine administered over 14 days. This regimen has < 90% efficacy in Thailand, and is widely regarded as ineffective because of poor compliance over the relatively long duration of dosing. We evaluated the efficacy, safety, and tolerability of alternative primaquine dosing regimens combined with artesunate among 399 Thai patients with acute, symptomatic P. vivax malaria. Patients were randomly assigned to one of six treatment groups: all patients received artesunate, 100 mg once a day for 5 days. Groups 1–5 then received primaquine, 30 mg a day for 5, 7, 9, 11, and 14 days, respectively. Group 6 received primaquine, 30 mg twice a day for 7 days. The 28-day cure rates were 85%, 89%, 94%, 100%, and 96%, respectively. Treatment of P. vivax malaria with artesunate for 5 days followed by high-dose primaquine, 30 mg twice a day for 7 days, was highly effective, well-tolerated, and equivalent or superior to the standard regimen of primaquine therapy.
INTRODUCTION
Plasmodium vivax, the predominant species of malaria parasite, has a relapse mechanism that results in the reappearance of parasitemia arising from the pre-erythrocytic hepatic-stage hypnozoite.1 This parasite affects millions of persons living in tropical areas and is an important cause of morbidity in Central and South America and Asia.2 In Thailand, the current standard treatment for P. vivax malaria is chloroquine, 1,500 mg over 3 days, followed by primaquine, 15 mg a day for 14 days. The acute phase of a P. vivax infection has been successfully treated with chloroquine in Thailand3 but not in eastern Indonesia.4 Many studies in Thailand have demonstrated that the standard regimen of primaquine showed relatively high relapse rates.3–6 Because higher doses of primaquine showed good efficacy against relapse in Thailand,7–9 the observed poor efficacy of the standard regimen is often attributed to an intrinsic tolerance of primaquine by parasites in the region,4,10,11 such as the well-known tolerance of the Chesson strain of P. vivax from New Guinea.12
Primaquine, an 8-aminoquinoline, has been the drug of choice for radical cure of P. vivax malaria since 1950. Although therapeutic application of primaquine is restricted because of its reported adverse events,13–17 it is the only drug currently available to prevent relapse of P. vivax malaria. Numerous studies have shown relatively poor efficacy against relapse without supervision of compliance to the 14-day regimen. The regimen is widely viewed as impractical among malaria control officers. In light of the remarkably good safety and tolerability of a 30-mg regimen given for prophylaxis against malaria over prolonged periods,7,18 some workers suggested abbreviated, higher-dose regimens of primaquine may improve the effectiveness of primaquine against relapse.19
Artesunate, a sodium salt of the hemisuccinate ester of artemisinin, has proven efficacious for treatment of blood stage P. vivax malaria.7,17,18 Because chloroquine-resistant P. vivax malaria continues to develop and mixed infections with P. falciparum and P. vivax are not uncommon, especially in Southeast Asia,8,20,21 artesunate may be a possible alternative treatment for acute P. vivax malaria in the future. This strategy, a single treatment for P. falciparum and P. vivax malaria, avoids risks to patients that hinge upon correct species diagnosis, i.e., receiving ineffective chloroquine therapy for a dangerous drug-resistant infection with P. falciparum diagnosed as P. vivax malaria.
The use of artesunate in the studies reported here offered the important advantage of avoiding the confounding effects of a drug such as chloroquine with its relatively long plasma half-life.22–24 Lingering chloroquine in the blood suppresses relapse after ineffective primaquine therapy.25 The rapid excretion of artesunate enabled us to assess the efficacy of primaquine against relapse within 28 days.26 The objectives of this study were to determine the efficacy, safety, and tolerability of artesunate with selected regimens of primaquine and the parasite and fever clearance times.
PATIENTS AND METHODS
The study was reviewed and approved by the Ethics Committee of the Faculty of Tropical Medicine, Mahidol University (Bangkok, Thailand). Before enrollment in the study, written informed consent was obtained from all patients. The study was a randomized, open-label, prospective study. Patients admitted to the Bangkok Hospital for Tropical Diseases were recruited if they were slide-positive for P. vivax, 12–60 years of age, weighed more than 30 kg, and agreed to remain in the hospital for 28 days. Reasons for exclusion included pregnancy, history of antimalarial drug treatment within the preceding two weeks, mixed P. vivax and P. falciparum infections, unwillingness to remain hospitalized for 28 days, and a glucose-6-phosphate dehydrogenase (G6PD) deficiency.
All patients received artesunate, 600 mg over 5 days and were then randomly assigned into 1 of 6 groups. Groups 1–5 received 30 mg of primaquine daily over durations of 5, 7, 9, 11, and 14 days, respectively. Group 6 received primaquine, 30 mg twice a day (60 mg a day) for 7 days.
Laboratory tests included a complete blood count and blood chemistry (liver and renal function tests), and urinalysis was performed prior to treatment and repeated weekly until patients were discharged. Hematologic tests were performed using ADVIA 120 (Bayer, Leverkusen, Germany) and the biochemistry tests were performed using INTEGRA 400 (Roche, Basel, Switzerland). A qualitative test of G6PD activity was performed using a rapid fluorescent spot (Beutler) test.27–29 Thick and thin blood films were obtained from finger pricks and stained with Giemsa. Blood smears were examined every 12 hours from initiation of treatment until they were negative on two consecutive occasions; thereafter blood smears were examined daily until patients were discharged. Blood films were considered negative if no parasites were seen in 200 oil-immersion fields on a thick blood film. Parasitemias (asexual parasite/microliter of blood) were determined by counting the number per 200 leukocytes (thick film) or the number per 1,000 erythrocytes (thin film). Parasite clearance time was expressed in hours from the start of treatment until the parasite counts decreased below the level of detection for at least 24 hours.
Vital signs except blood pressure were measured every four hours. Blood pressure was measured daily. Monitoring of signs and symptoms of malaria and adverse events was performed daily for the first seven days of admission and weekly thereafter. All patients were closely monitored for the clinical signs of intravascular hemolysis and hemoglobinuria. Fever clearance time was defined as the time from the start of treatment until the oral temperature decreased below 37.5°C for at least 48 hours.
Patients with reappearance of parasitemia after treatment with any of the six regimens were treated with chloroquine (30 mg/kg) and primaquine (15 mg once a day for 14 days) as a standard treatment of the hospital. The patients with subsequent appearance of a sexual form of P. falciparum were treated with artesunate (600 mg) followed by mefloquine (25 mg/kg). Patients having recurrent parasitemia on or before day 14 were considered artesunate treatment failures, whereas recurrent parasitemia between days 15 and 28 were considered primaquine treatment failures. All patients with concurrent P. falciparum malaria were considered failures to treatment, excluded from the study, and not included in the analysis of the cure rate at 28 days.
The clinical efficacies among groups were estimated by comparing relapse rates observed after 28-day follow-up of patients in each groups. Descriptive statistics and statistical analysis were conducted using the Epi Info version 6.04 (USD Inc., Stone Mountain, GA) software package. All statistical tests were two-tailed and a significance level of 0.05 was used.
RESULTS
Three hundred ninety-nine patients with acute symptomatic P. vivax malaria infection were recruited into the study. The baseline demographic, clinical, and pre-treatment characteristic data were comparable (Table 1). Most patients reported recent travel to the Thailand-Myanmar border, where they presumably acquired their infections. There is no risk of malaria in Bangkok, and risk is low in most other areas of Thailand.
Table 1.
Baseline clinical and laboratory characteristics of patients in the study*
| Characteristic | Group 1 (n = 68) | Group 2 (n = 69) | Group 3 (n = 66) | Group 4 (n = 64) | Group 5 (n = 66) | Group 6 (n = 66) |
|---|---|---|---|---|---|---|
| Sex (M:F) | 42:26 | 46:24 | 46:19 | 44:21 | 41:21 | 37:29 |
| Mean (SD) age, years | 26.2 (9.4) | 24.5 (8.1) | 22.9 (5.8) | 23.7 (8.1) | 24.1 (8.2) | 23.7 (7.2) |
| Mean (SD) height, cm | 160.6 (8.4) | 159.2 (7.2) | 161.2 (7.1) | 160.4 (7.1) | 159.8 (6.6) | 159.0 (7.6) |
| Mean (SD) weight, kg | 53.6 (7.7) | 53.3 (7.9) | 53.0 (7.9) | 52.8 (8.5) | 52.8 (8.2) | 51.2 (7.2) |
| Fever, mean (SD) | ||||||
| Duration of fever before admission, days | 4.8 (3.6) | 4.2 (1.8) | 5.1 (4.7) | 5.2 (5.1) | 4.9 (3.1) | 4.8 (3.1) |
| Highest temperature, °C | 37.8 (1.0) | 38.0 (1.2) | 38.0 (1.0) | 37.8 (0.9) | 37.7 (0.8) | 37.9 (1.0) |
| No. of patients with | ||||||
| Splenomegaly | 0 | 2 | 1 | 1 | 3 | 3 |
| Hepatomegaly | 21 | 11 | 17 | 10 | 13 | 9 |
| First malaria attack | 37 | 28 | 32 | 28 | 38 | 37 |
| Geometric mean parasitemia (range)/μL | 6,410 (75–65,520) | 6,016 (63–48,500) | 5,993 (42–88,480) | 5,192 (22–41,680) | 5,616 (49–54,120) | 6,323 (105–54,120) |
| Laboratory results, mean (SD) | ||||||
| Hematocrit, % | 37.2 (5.6) | 35.6 (5.9) | 37.0 (6.4) | 37.6 (5.9) | 36.2 (5.6) | 36.5 (6.2) |
| White blood cell count/μL | 5.5 (1.6) | 5.5 (1.7) | 6.3 (2.1) | 6.6 (2.1) | 6.1 (1.8) | 5.6 (1.5) |
| Blood urea nitrogen, mg/dL | 14.9 (4.2) | 15.7 (4.6) | 14.4 (4.9) | 14.8 (4.4) | 15.4 (7.1) | 14.6 (4.9) |
| Serum creatinine, mg/dL | 0.8 (0.1) | 0.8 (0.1) | 0.8 (0.1) | 0.8 (0.1) | 0.8 (0.3) | 0.8 (0.1) |
| Total bilirubin, mg/dL | 1.5 (0.8) | 1.6 (1.1) | 1.7 (1.4) | 1.5 (1.0) | 1.5 (1.0) | 1.3 (0.6) |
| Serum AST, U/L | 34.3 (28.4) | 33.9 (21.7) | 39.2 (40.1) | 29.5 (19.1) | 31.5 (16.1) | 31.0 (15.2) |
| Serum ALT, U/L | 34.5 (48.4) | 35.8 (36.0) | 35.0 (37.8) | 30.1 (24.0) | 34.6 (35.0) | 32.6 (31.4) |
| Alkaline phosphatase, U/L | 117.4 (68.4) | 120.7 (55.1) | 123.9 (63.4) | 122.8 (61.0) | 127.2 (92.7) | 126.6 (62.7) |
| Albumin, g/dL | 3.7 (0.4) | 3.7 (0.4) | 3.7 (0.5) | 3.8 (0.5) | 3.7 (0.5) | 3.7 (0.4) |
For definition of groups, see Patients and Methods. AST = aspartate aminotransferase; ALT = alanine aminotransferase.
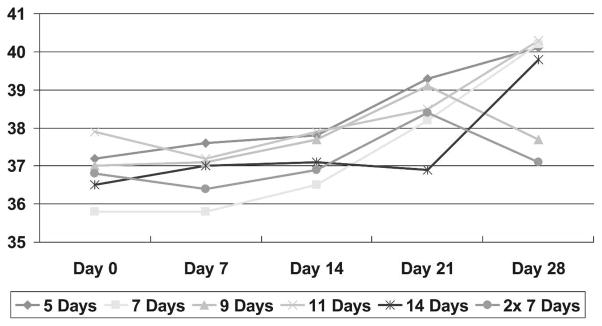
During the follow-up period, 77 patients left the hospital before completing 28 days of follow up (8 in group 1, 12 in group 2, 10 in group 3, 16 in group 4, 14 in group 5, and 17 in group 6) for personal reasons unrelated to side effects of treatment. All patients who left the hospital were asymptomatic and without parasitemia before being discharged. None of the patients who left the study before day 28 developed P. falciparum malaria. Fever and parasitemia disappeared in all patients within 48 hours (Table 2). No recurrence of parasitemia occurred before day 15; thus, all recurrences were classified as primaquine treatment failures. Almost all recurrences occurred after only 5, 7, or 9 days of daily primaquine dosing with 30 mg (9 of 60 treated, 6 of 57 treated, and 2 of 56 treated, respectively). No recurrences appeared after 11 or 14 days of the same dose. Among patients given twice-a-day primaquine dosing with 30 mg of primaquine for 7 days, 2 recurrences appeared among the 49 persons treated (Table 2). There were no changes in hematocrit levels (Figure 1). No serious adverse events were observed, and no significant differences in adverse events were observed among the groups (Table 3).
Table 2.
Therapeutic responses of patients in the study*
| Characteristic | Group 1 (n = 68) | Group 2 (n = 69) | Group 3 (n = 66) | Group 4 (n = 64) | Group 5 (n = 66) | Group 6 (n = 66) |
|---|---|---|---|---|---|---|
| No. of dropouts | 8 | 12 | 10 | 16 | 14 | 17 |
| No. of patients who completed follow-up | 60 | 57 | 56 | 48 | 52 | 49 |
| Cure rate at day 28 (%) | 51 (85) | 51 (89) | 54 (94) | 48 (100) | 52 (100) | 47 (96) |
| Relapse rate at day 28 (%) | 9 (15) | 6 (11) | 2 (4) | 0 | 0 | 2 (4) |
| Day of appearance | 19, 20, 22, 23, 25, 28 | 20, 21, 23, 24, 28 | 14, 21 | NA | NA | 22, 23 |
| Mean (SD) fever clearance time, hr | 16.8 (14.4) | 20.0 (21.6) | 14.5 (9.3) | 13.8 (11.4) | 19.6 (22.2) | 21.4 (23.5) |
| Mean (SD) parasite clearance time, hr | 34.9 (8.4) | 36.0 (10.5) | 35.7 (10.1) | 34.2 (9.9) | 37.2 (11.4) | 36.8 (10.4) |
NA = not available. Group 1 ≠ group 4 and group 5 (P = 0.004 and 0.003). Group 2 ≠ group 4 and group 5 (P = 0.015 and 0.014).
Figure 1.
Mean hematocrit level of patients receiving high-dose primaquine.
Table 3.
Potential adverse effects after treatment in patients in the study*
| Characteristic | Group 1 | Group 2 | Group 3 | Group 4 | Group 5 | Group 6 |
|---|---|---|---|---|---|---|
| Headache | 1 (1.47) | 3 (4.34) | 3 (4.54) | 2 (3.12) | 3 (4.54) | 3 (4.54) |
| Weakness | 0 | 0 | 0 | 0 | 0 | 0 |
| Dizziness | 3 (4.41) | 2 (2.89) | 5 (7.57) | 1 (1.56) | 2 (3.03) | 1 (1.51) |
| Anorexia | 2 (2.94) | 2 (2.89) | 4 (6.06) | 4 (6.05) | 1 (1.51) | 2 (3.03) |
| Nausea | 2 (2.94) | 1 (1.44) | 2 (3.03) | 1 (1.56) | 1 (1.51) | 1 (1.51) |
| Vomiting | 1 (1.47) | 0 | 1 (1.51) | 0 | 0 | 1 (1.51) |
| Insomnia | 0 | 0 | 0 | 0 | 0 | 0 |
| Abdominal pain | 3 (4.41) | 4 (5.79) | 1 (1.51) | 2 (3.12) | 2 (3.03) | 3 (4.54) |
| Diarrhea | 0 | 1 (1.44) | 0 | 0 | 1 (1.51) | 0 |
Values are no. (%).
DISCUSSION
Abbreviated high-dose regimens of primaquine after artesunate therapy provided efficacious, safe, and well-tolerated therapy against relapse by P. vivax acquired in Thailand. The complete efficacy of artestunate against P. vivax malaria7 and its short plasma half-life enabled us to evaluate the efficacy of primaquine against early relapse by P. vivax. In studies of patients infected by tropical Asian strains of P. vivax and not treated with primaquine, 197 (75%) of 263 persons who relapsed did so on or before day 28.24 We believe the 28-day period of follow-up captured most possible relapses in this study population. Regimens of 30 mg a day for 5 or 7 days proved significantly less efficacious (< 90%) against early relapse than 30 mg a day over 9, 11, or 14 days (> 90%) (P < 0.05). The regimen of 2 daily doses of 30 mg for 7 days was 94% efficacious against early relapse. Because of prolonged use of primaquine, which can eliminate the asexual erythrocytic stage of P. vivax, none of the patients developed recurrences before day 15.
Patients given the dose of 60 mg of primaquine divided into 2 daily doses over 7 days tolerated this drug without serious adverse events and without substantially altered blood or liver function profiles. Although methemoglobin levels were not measured in this study, none of the patients developed clinical signs and symptoms of methemoglobinemia, such as bluish discoloration of the skin. This corroborated similar findings of good tolerability of a 60-mg daily dose given in combination with chloroquine in the setting of a placebo-controlled, double-blinded trial.30 We consider that regimen a practical alternative to 30 mg of primaquine a day over 9, 11, or 14 days among patients considered good candidates to receive this regimen, i.e., not pregnant and a G6PD deficiency.
Many countries in malaria-endemic regions adopted a dose of 15 mg of primaquine a day for 5 days as standard anti-relapse therapy against P. vivax on the basis of findings in poorly controlled clinical trials.12 Recent well-controlled trials have shown that this regimen was almost completely ineffective against relapse by P. vivax in Asia.31 Health officers responsible for malaria therapy policies cite the impracticality of a 14-day regimen as the basis of opting for the abbreviated regimen. Our findings support the concept of adopting a 30 mg twice a day regimen for 7 days as a safe, well-tolerated, and efficacious alternative that may prove more practical. However, the safety of such a regimen in patients with G6PD deficiency is doubtful and adoption of such a regimen would depend upon availability of reliable G6PD testing prior to drug administration.
Acknowledgments
We thank the patients for participating in the study and the nurses and laboratory technicians of Bangkok Hospital for Tropical Diseases (Faculty of Tropical Medicine, Mahidol University) for help.
Financial support: The study was supported by the World Health Organization Regional Office for South-East Asia Region and a grant from Mahidol University.
Footnotes
Disclosure: The authors have no conflict of interest with respect to this study.
Authors’ addresses: Srivicha Krudsood, Department of Tropical Hygiene, Faculty of Tropical Medicine, Mahidol University, 420/6 Rajvithi Road, Bangkok 10400, Thailand. Noppadon Tangpukdee, Polrat Wilairatana, and Nantaporn Phophak, Department of Clinical Tropical Medicine, Faculty of Tropical Medicine, Mahidol University, Bangkok, Thailand. J. Kevin Baird, ALERTAsia Foundation, Jakarta, Indonesia. Gary M. Brittenham, Department of Pediatrics and Medicine, Columbia University College of Physicians and Surgeons, New York, NY 10032. Sornchai Looareesuwan (deceased).
References
- 1.Krotoski WA, Colllins WE, Bray RS, Garnham PC, Gogswell FB, Gwadz R, Killick-Kendrick R, Wolf RH, Sinden R, Koontz LC, Stanfill PS. Demonstarion of hypnozoites in sporozoite transmitted Plasmodium vivax infection. Am J Trop Med Hyg. 1982;31:1291–1293. doi: 10.4269/ajtmh.1982.31.1291. [DOI] [PubMed] [Google Scholar]
- 2.Mendis K, Sina BJ, Marchesini P, Carter R. The neglected burden of Plasmodium vivax malaria. Am J Trop Med Hyg. 2001;64(Suppl):97–106. doi: 10.4269/ajtmh.2001.64.97. [DOI] [PubMed] [Google Scholar]
- 3.Bunnag D, Karbwang J, Thanavibul A, Chittamas S, Rattanapong Y, Chalermrut K, Bangchang KN, Harinasuta T. High dose of primaquine in primaqune resistant vivax malaria. Trans R Soc Trop Med Hyg. 1994;88:218–219. doi: 10.1016/0035-9203(94)90305-0. [DOI] [PubMed] [Google Scholar]
- 4.Looareesuwan S, Buchachart K, Wilairatana P, Chalermrut K, Rattanapong Y, Amradee S, Siripipat S, Chullavichit S, Thimasarn K, Ittiverakul M, Triampon A, Walsh DS. Primaquine-tolerant vivax malaria in Thailand. Ann Trop Med Parasitol. 1997;91:939–943. doi: 10.1080/00034989760338. [DOI] [PubMed] [Google Scholar]
- 5.Doherty JF, Day JH, Warhurst DC, Chiodini PL. Treatment of Plasmodium vivax malaria—time for a change? Trans R Soc Trop Med Hyg. 1997;88:218–219. doi: 10.1016/s0035-9203(97)90403-x. [DOI] [PubMed] [Google Scholar]
- 6.Looareesuwan S, Wilairatana P, Krudsood S, Treeprasertsuk S, Singhasivanon P, Bussaratid V, Chokejindachai W, Virayavejakul P, Chalermrut K, Walsh DS, White NJ. Chloroquine sensitivity of Plasmodium vivax in Thailand. Ann Trop Med Parasitol. 1999;93:225–230. [PubMed] [Google Scholar]
- 7.Wilairatana P, Silachamroon U, Krudsood S, Singhasivanon P, Treeprasertsuk S, Bussaratid V, Phumratanaprapin W, Srivilairit S, Looareesuwan S. Efficacy of primaquine regimens for primaquine-resistant Plasmodium vivax malaria in Thailand. Am J Trop Med Hyg. 1999;61:973–977. doi: 10.4269/ajtmh.1999.61.973. [DOI] [PubMed] [Google Scholar]
- 8.Silachamroon U, Krudsood S, Treeprasertsuk S, Wilairatana P, Chalermrut K, Myint HY, Maneekan P, White NJ, Gourdeuk VR, Brittenham GM, Looareesuwan S. Clinical trial of oral artesunate with or without high-dose primaquine for the treatment of vivax malaria in Thailand. Am J Trop Med Hyg. 2003;69:14–18. [PMC free article] [PubMed] [Google Scholar]
- 9.Looareesuwan S, Wilairatana P, Glanarongran R, Indravijit KA, Supeeranontha L, Chinnapha S, Scott TR, Chulay JD. Atovaquone and proguanil hydrochloride followed by primaquine for treatment of Plasmodium vivax malaria in Thailand. Trans R Soc Trop Med Hyg. 1999;93:637–640. doi: 10.1016/s0035-9203(99)90079-2. [DOI] [PubMed] [Google Scholar]
- 10.Bunnag D, Karbwang J, Thanavibul A, Chittamas S, Ratanapongse Y, Chalermrut K, Bangchang KN, Harinasuta T. High dose of primaquine in primaquine resistant vivax malaria. Trans R Soc Trop Med Hyg. 1994;88:218–219. doi: 10.1016/0035-9203(94)90305-0. [DOI] [PubMed] [Google Scholar]
- 11.Looareesuwan S, Wilairatana P, Krudsood S, Singhasivanon P, Treeprasertsuk S, Bussaratid V, Chokjindachai W, Viriyavejakul P, Chalermrut K, Walsh DS, White NJ. Chloroquine sensitivity of Plasmodium vivax in Thailand. Ann Trop Med Parasitol. 1999;93:225–230. [PubMed] [Google Scholar]
- 12.Baird JK, Hoffman SL. Primaquine therapy for malaria. Clin Infect Dis. 2004;39:1336–1345. doi: 10.1086/424663. [DOI] [PubMed] [Google Scholar]
- 13.Clayman CB, Arnold J, Hochwald RS, Yount EH, Edgcomb JH, Alving AS. Toxicity of primaquine in Caucasians. JAMA. 1952;149:1563–1568. doi: 10.1001/jama.1952.72930340022010b. [DOI] [PubMed] [Google Scholar]
- 14.Hansen JE, Cleve EA, Pruitt FW. Relapse of vivax malaria treated with primaquine and report of one case of cyanosis (methemoglobinemia) due to primaquine. Am J Med Sci. 1954;227:9–12. doi: 10.1097/00000441-195401000-00002. [DOI] [PubMed] [Google Scholar]
- 15.Alving AS, Johnson CF, Tarlov AR, Brewer GJ, Kellermeyer RW, Carson PE. Mitigation of the hemolytic effect of primaquine and enhancement of its action against exoerythro-cytic forms of the Chesson strain of Plasmodium vivax by intermittent regimens of drug administration. Bull World Health Organ. 1960;22:621–631. [PMC free article] [PubMed] [Google Scholar]
- 16.Charoenlarp P, Areekul S, Pholphoti T, Harinasuta T. The course of primaquine induced hemolysis in G6PD deficient Thais. J Med Assoc Thai. 1973;56:392–397. [PubMed] [Google Scholar]
- 17.Buchachart K, Krudsood S, Singhasivanon P, Treeprasertsuk S, Phophak N, Srivilairit S, Chalermrut K, Ratttanapong Y, Supeeranuntha L, Wilairatana P, Brittenham GM, Looareesuwan S. Effect of primaquine standard dose (15 mg/day for 14 days) in the treatment of vivax malaria patients in Thailand. Southeast Asian J Trop Med Public Health. 2001;32:720–726. [PubMed] [Google Scholar]
- 18.Looareesuwan S, Olliaro P, White NJ, Chongsuphajaisiddhi T, Sabcharoen A, Thimasarn K, Nosten F, Singhasivanon P, Supavej S, Khusmith S, Wyling S, Kanyok T, Walsh D, Leggat PA, Doberstyn EB. Consensus recommendation on the treatment of malaria in Southeast Asia. Southeast Asian J Trop Med Public Health. 1998;29:355–360. [PubMed] [Google Scholar]
- 19.Baird JK, Rieckmann KH. Can primaquine therapy for vivax malaria be improved? Trends Parasitol. 2003;9:115–120. doi: 10.1016/s1471-4922(03)00005-9. [DOI] [PubMed] [Google Scholar]
- 20.Looareesuwan S, White NJ, Chittamas S, Bunnag D, Harinasuta T. High rate of Plasmodium vivax relapse following treatment of falciparum malaria in Thailand. Lancet. 1987;2:1052–1055. doi: 10.1016/s0140-6736(87)91479-6. [DOI] [PubMed] [Google Scholar]
- 21.Krudsood S, Wilairatana P, Mason DP, Treeprasertsuk S, Singhasivanon P, Looareesuwan S. Hidden Plasmodium falciparum infections. Southeast Asian J Trop Med Public Health. 1999;30:623–624. [PubMed] [Google Scholar]
- 22.Mason DP, Krudsood S, Wilairatana P, Viriyavejakul P, Silachamroon U, Chokejindachai W, Singhasivanon P, Supavej S, McKenzie FE, Looareesuwan S. Can treatment of P. vivax lead to unexpected appearance of falciparum malaria? Southeast Asian J Trop Med Public Health. 2001;32:57–63. [PMC free article] [PubMed] [Google Scholar]
- 23.Snounou G, White NJ. The co-existence of Plasmodium: sidelights from falciparum and vivax malaria in Thailand. Trends Parasitol. 2004;20:333–339. doi: 10.1016/j.pt.2004.05.004. [DOI] [PubMed] [Google Scholar]
- 24.Gustafsson LL, Walker O, Alvan G, Beermann B, Estevez F, Gliesner L, Lindstrom B, Sjoqvist F. Disposition of chloroquine in man after single intravenous and oral doses. Br J Clin Pharmacol. 1983;15:471–479. doi: 10.1111/j.1365-2125.1983.tb01532.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Baird JK, Wiady I, Fryauff DJ, Sutanihardja MA, Leksana B, Widjaya H, Kysdarmanto, Subianto B. In vivo resistance to chloroquine by Plasmodium vivax and Plasmodium falciparum at Nabire, Irian Jaya, Indonesia. Am J Trop Med Hyg. 1997;56:627–631. doi: 10.4269/ajtmh.1997.56.627. [DOI] [PubMed] [Google Scholar]
- 26.Walker O, Dawodu AH, Adeyokunnu AA, Salako LA, Alvan G. Plasma chloroquine and desethylchloroquine concentrations in children during and after chloroquine treatment of malaria. Br J Clin Pharmacol. 1983;16:701–705. doi: 10.1111/j.1365-2125.1983.tb02244.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.White NJ, Milller KD, Churchill FC, Berry C, Brown J, Williams SB, Greenwood BM. Chloroquine treatment of severe malaria in children. Pharmacokinetics, toxicity, and new dosage recommendations. N Engl J Med. 1988;319:1493–1500. doi: 10.1056/NEJM198812083192301. [DOI] [PubMed] [Google Scholar]
- 28.Beutler E, Glumbe KG, Kaplan JC, Lohr GW, Romot B, Valentine WN. International committee for standardization in hematology: recommended screening test for glucose-6-phosphate dehydrogenase (G-6-PD) deficiency. Br J Haematol. 1979;43:465–467. doi: 10.1111/j.1365-2141.1979.tb03774.x. [DOI] [PubMed] [Google Scholar]
- 29.Frank JE. Diagnosis and management of G6PD deficiency. Am Fam Physician. 2005;72:1277–1282. [PubMed] [Google Scholar]
- 30.Baird JK, Basri H, Subianto B, Fryauff DJ, McElroy PD, Leksana B, Richie T, Lm Masbar S, Wignall FS, Hoffman SL. Treatment of chloroquine-resistant Plasmodium vivax with chloroquine and primaquine or halofantrine. J Infect Dis. 1995;171:1678–1682. doi: 10.1093/infdis/171.6.1678. [DOI] [PubMed] [Google Scholar]
- 31.Gogtay NJ, Kshirsagar NA, Vaidya AB. Current challenges in drug-resistant malaria. J Postgrad Med. 2006;52:241–242. [PubMed] [Google Scholar]