Abstract
Objectives
Psoriasis (PsO) is a common chronic T cell-mediated inflammatory disorder traditionally thought to manifest in the skin and joints (psoriatic arthritis, PsA). Recently, it has been shown that these patients have an increased risk for myocardial infarction and this was greater with increasing severity of psoriasis. Patients with psoriasis have reported to have cardiometabolic disturbances including obesity, insulin resistance, and dyslipidemia. This constellation of risk factors, referred to as the metabolic syndrome, increases the risk for atherosclerotic cardiovascular disease (ASCVD) and type 2 diabetes mellitus. The aim of this study was to determine the prevalence of metabolic syndrome in PsA.
Methods
In our study, we examined the records of 105 patients with PsA to determine the prevalence of metabolic syndrome in PsA. This was a retrospective analysis of the Sacramento Veterans Affairs database.
Results
Our results demonstrated an increased prevalence of the metabolic syndrome in patients with PsA (61/105 patients or 58.1%) compared to the 35.2 % reported for the Third National Health and Nutrition Examination Survery (NHANES III) data.
Conclusions
Thus, patients with PsA have a very high prevalence of metabolic syndrome, which predisposes them to an increased risk of both diabetes and ASCVD.
Introduction
Heart disease, responsible for 26% of all deaths in the United States in 2006, is the leading cause of mortality in the United States and in patients with rheumatological diseases.1–4 Studies have demonstrated that cardiovascular disease is accelerated in this patient population, but the cause remains unclear.3 Whereas cardiovascular risk factors such as age, gender, smoking, hypertension (HTN), and dyslipidemia have been shown to play a role in atherosclerosis, they do not appear to fully account for the increased risk of cardiovascular disease in rheumatologic patients.5,6 In the past few years, there has been mounting literature on the metabolic syndrome, a constellation of central adiposity, atherogenic dyslipidemia, HTN, and abnormal glucose tolerance.7–10 Metabolic syndrome increases the risk of developing atherosclerotic cardiovascular disease (ASCVD) at least two-fold and type 2 diabetes mellitus (T2DM) by five-fold.7–10 Interestingly, various studies have suggested that metabolic syndrome is associated with a state of chronic, low-grade inflammation.11,12 The mechanism remains uncertain, but proinflammatory cytokines such as tumor necrosis factor-α (TNF-α) have been demonstrated to reduce the activity of insulin, contributing to insulin resistance.12–16 Furthermore, inflammation has not only been associated with obesity but also with insulin-resistance in the absence of an increase in total body fat.17
The literature on the relationship between rheumatological diseases and the metabolic sydnrome is limited. However, a number of studies of gout, systemic lupus erythematous, rheumatoid arthritis (RA), and ankylosing spondylitis reviewed elsewhere have demonstrated an increased frequency of metabolic syndrome in patients with rheumatologic disease.18 In addition, the association between the metabolic syndrome and psoriasis (PsO), a chronic inflammatory disorder of the skin involving immune-mediated disease involving T lymphocytes, has also been examined in cross-sectional and epidemiological studies.19–27 Symptoms of PsO are generally limited to the skin with the exception of an inflammatory arthropathy, known as psoriatic arthritis (PsA). Recent epidemiological surveys suggest PsA is more common than previously estimated.28,29 A study of nearly 5,000 patients found nearly 30% of patients with PsO had concomitant arthritis.30 Recently, Gelfand et al. showed that PsO confers an independent greater risk for myocardial infarction which increased with severity of psoriasis.31 However, there is scanty data on the prevalence of metabolic syndrome in patients with PsA. Here we investigated the prevalence of metaoblic syndrome in patients with PsA specifically.
Materials and Methods
We conducted a retrospective case study using data from 105 patients with diagnosed PsA obtained from patient charts at a Veterans Affairs (VA) Medical Center. These patients were recruited from the patient database of the VA Medical Center Mather, California. Relevant information including age, weight, body mass index (BMI), waist circumference, latest blood pressure, fasting lipid profile, and glucose levels. In addition, the patient charts were screened for the presence of coronary artery disease, chronic renal failure/kidney disease, HTN, hyperlipidemia, and T2DM along with the date of onset for the disease. The metabolic syndrome was defined according to the American Heart Association/National Heart, Lung, and Blood Institute (AHA/NHLBI) criteria.7 These criteria define the presence of the metabolic syndrome if three of the five following features are present: (1) Waist circumference ≥ 40 inches in men and ≥ 35 inches in women; (2) fasting triglycerides, ≥150 mg/dL or drug treatment for elevated triglycerides; (3) reduced high-density lipoprotein cholesterol (HDL-C), <40 mg/dL) in men and <50 mg/dL) in women, or drug treatment for reduced HDL-C; (4) blood pressure, ≥ 130 mmHg systolic blood pressure (SBP) or ≥85 mmHg diastolic blood pressure (DBP) or antihypertensive drug therapy; (5) fasting glucose, ≥100 mg/dL or drug treatment for hyperglycemia.
Results
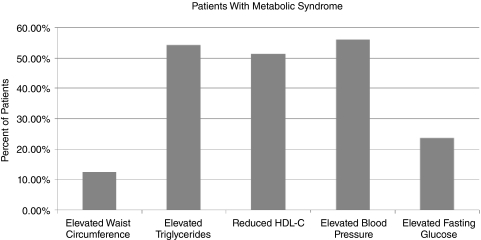
The study included 105 patients with psoriatic arthritis (100 males and 5 females). The mean age was 59.8 years with a range from 29 to 85 years. The prevalence of metabolic syndrome diagnosed according to AHA/NHLBI guidelines was 58.1%, with 61 out of 105 patients fulfilling at least three of the five features needed for diagnosing the syndrome. Whereas this was predominantly a study of males, 58% of the males and 60% of the females had metabolic syndrome. Of the patients with metabolic syndrome, 15 (24.6%) had coronary artery disease, 24 (39.3%) had T2DM, and 11 (18.0%) had chronic kidney disease. Of our 61 patients with metabolic syndrome, 45 patients had three features, 13 patients had four, and 6 patients had five features. Details of the distribution of these five conditions in patients with metabolic syndrome are depicted in Fig. 1. The three commonest features included increased triglycerides (54.3%), decreased HDL-C (51.4%), and hypertension (56.2%).
FIG. 1.
The frequency of features of the metabolic syndrome in psoriatic arthritis. Abbreviation: HDL-C, high-density lipoprotein cholesterol.
Discussion
Our results indicate that the prevalence of the metabolic syndrome is high in patients with PsA. We report a prevalence of 58.1%, which is much higher than the 35.2% of the NHANES III population.32 Patients with PsA appear to be at an increased risk of developing diabetes mellitus, arterial hypertension, dyslipidemia, obesity, and cardiac disease. Although the precise pathogenesis remains to be elucidated, chronic inflammatory changes, such as the secretion of proinflammatory cytokines, may be responsible.5,33 Data in patients with RA have confirmed a correlation between lasting arthritis and the development of metabolic syndrome with eventual coronary heart disease (CHD).34 Among the cytokines involved, TNF-α and interleukin-6 (IL-6) have been shown to play important roles.35 TNF-α has been shown to impair insulin-mediated glucose uptake in adipose tissue and glucose metabolism.36–38 Some studies suggest therapeutic intervention with antiinflammatory drugs such as methotrexate (MTX) and TNF-α antagonists may reduce risk.39,40 Studies of TNF-α antagonists in RA appear to demonstrate an improvement in insulin resistance and sensitivity, but suggest minimum benefit and possibly negative effects on lipid profiles.41,42 However, given the transient nature of lipid profiles and possible confounding factors such as concomitant therapy, conclusions are limited. Very little data exist regarding metabolic syndrome and TNF-α antagonists in PsA. Limited preliminary data from psoriatic patients appear to support an improvement in insulin resistance and sensitivity with TNF-α antagonist therapy.43 Factors such as smoking, age, gender, and alcohol may also play a role. However, studies have found that even when these factors are accounted for there is a higher prevalence of concomitant findings associated with metabolic syndrome in individuals with rheumatological disorders.19
Our findings of a high prevalence of metabolic syndrome (58%) emphasize the need for close monitoring of patients with PsA for concomitant diseases such as diabetes mellitus, hypertension, and dyslipidemia. Furthermore, patients are at increased risk for diabetes and ASCVD. Lifestyle interventions and drug therapies for abnormalities in the individual risk factors may be necessary. As with RA patients, effective treatment of PsA in an effort to minimize chronic inflammation may also be important. Additional prospective controlled studies with patients with PsA and the metabolic syndrome need to be undertaken to better understand the pathophysiology especially as it relates to circulating and cellular biomarkers of inflammation and the risk of both diabetes and ASCVD.
Acknowledgment
This work was supported by National Institutes of Health grant NIH K24 AT00596 to I. J.
Author Disclosure Statement
No competing financial interests exist for any of the authors.
References
- 1.Abou-Raya A. Abou-Raya S. Inflammation: A pivotal link between autoimmune diseases and atherosclerosis. Autoimmun Rev. 2006;5:331–337. doi: 10.1016/j.autrev.2005.12.006. [DOI] [PubMed] [Google Scholar]
- 2.Heron M. Hoyert DL. Murphy S. Xu J. Kochanek K. Tejada-Vera B. National Vital Statistics Reports. www.cdc.gov/nchs/data/nvsr/nvsr57/nvsr57_14.pdf/ [Apr;2009 ]. www.cdc.gov/nchs/data/nvsr/nvsr57/nvsr57_14.pdf/ [PubMed]
- 3.Manzi S. Meilahn EN. Rairie JE. Conte CG. Medsger TA., Jr Jansen-McWilliams L. D'Agostino RB. Kuller LH. Age-specific incidence rates of myocardial infarction and angina in women with systemic lupus erythematosus: comparison with the Framingham Study. Am J Epidemiol. 1997;145:408–415. doi: 10.1093/oxfordjournals.aje.a009122. [DOI] [PubMed] [Google Scholar]
- 4.Pincus T. Callahan LF. Taking mortality in rheumatoid arthritis seriously—predictive markers, socioeconomic status and comorbidity. J Rheumatol. 1986;13:841–845. [PubMed] [Google Scholar]
- 5.Kiani AN. Magder L. Petri M. Coronary calcium in systemic lupus erythematosus is associated with traditional cardiovascular risk factors, but not with disease activity. J Rheumatol. 2008;35:1300–1306. [PubMed] [Google Scholar]
- 6.Chung CP. Oeser A. Raggi P. Gebretsadik T. Shintani AK. Sokka T. Pincus T. Avalos I. Stein CM. Increased coronary-artery atherosclerosis in rheumatoid arthritis: Relationship to disease duration and cardiovascular risk factors. Arthritis Rheum. 2005;52:3045–3053. doi: 10.1002/art.21288. [DOI] [PubMed] [Google Scholar]
- 7.Grundy SM. Cleeman JI. Daniels SR. Donato KA. Eckel RH. Franklin BA. Gordon DJ. Krauss RM. Savage PJ. Smith SC., Jr Spertus JA. Costa F. Diagnosis and management of the metabolic syndrome: an American Heart Association/National Heart, Lung, and Blood Institute Scientific Statement. Circulation. 2005;112:2735–2752. doi: 10.1161/CIRCULATIONAHA.105.169404. [DOI] [PubMed] [Google Scholar]
- 8.Eckel RH. Grundy SM. Zimmet PZ. The metabolic syndrome. Lancet. 2005;365:1415–1428. doi: 10.1016/S0140-6736(05)66378-7. [DOI] [PubMed] [Google Scholar]
- 9.Alberti KG. Zimmet P. Shaw J. Metabolic syndrome—a new world-wide definition. A Consensus Statement from the International Diabetes Federation. Diabet Med. 2006;23:469–480. doi: 10.1111/j.1464-5491.2006.01858.x. [DOI] [PubMed] [Google Scholar]
- 10.Johnson LW. Weinstock RS. The metabolic syndrome: concepts and controversy. Mayo Clin Proc. 2006;81:1615–1620. doi: 10.4065/81.12.1615. [DOI] [PubMed] [Google Scholar]
- 11.Devaraj S. Rosenson RS. Jialal I. Metabolic Syndrome: An Appraisal of the Pro-inflammatory, procoagulant status. Endocrinol Metab Clin of N Am. 2004;33:431–443. doi: 10.1016/j.ecl.2004.03.008. [DOI] [PubMed] [Google Scholar]
- 12.Jialal I. Editorial: The role of the laboratory in the diagnosis of the metabolic syndrome. Am J Clin Pathol. 2009;132:161–162. doi: 10.1309/AJCP1B0DHHSAIJJR. [DOI] [PubMed] [Google Scholar]
- 13.Nilsson J JS. Niemann A. Reneland R. Lithell H. Relation between plasma tumor necrosis factor-alpha and insulin sensitivity in elderly men with non-insulin-dependent diabetes mellitus. Arterioscler Thromb Vasc Biol. 1998;18:1199–1202. doi: 10.1161/01.atv.18.8.1199. [DOI] [PubMed] [Google Scholar]
- 14.Shulman GI. Cellular mechanisms of insulin resistance. J Clin Invest. 2000;106:171–176. doi: 10.1172/JCI10583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hotamisligil GS. Inflammatory pathways and insulin action. Int J Obes Relat Metab Disord. 2003;27(Suppl 3):S53–S55. doi: 10.1038/sj.ijo.0802502. [DOI] [PubMed] [Google Scholar]
- 16.Ruan H. Lodish HF. Insulin resistance in adipose tissue: Direct and indirect effects of tumor necrosis factor-alpha. Cytokine Growth Factor Rev. 2003;14:447–455. doi: 10.1016/s1359-6101(03)00052-2. [DOI] [PubMed] [Google Scholar]
- 17.Chandalia M. Cabo-Chan AV., Jr Devaraj S. Jialal I. Grundy SM. Abate N. Elevated plasma high-sensitivity C-reactive protein concentrations in Asian Indians living in the United States. J Clin Endocrinol Metab. 2003;88:3773–3776. doi: 10.1210/jc.2003-030301. [DOI] [PubMed] [Google Scholar]
- 18.Pereira RM. de Carvalho JF. Bonfa E. Metabolic syndrome in rheumatological diseases. Autoimmun Rev. 2009;8:415–419. doi: 10.1016/j.autrev.2009.01.001. [DOI] [PubMed] [Google Scholar]
- 19.Sommer DM. Jenisch S. Suchan M. Christophers E. Weichenthal M. Increased prevalence of the metabolic syndrome in patients with moderate to severe psoriasis. Arch Dermatol Res. 2006;298:321–328. doi: 10.1007/s00403-006-0703-z. [DOI] [PubMed] [Google Scholar]
- 20.Christophers E. Comorbidities in psoriasis. Clin Dermatol. 2007;25:529–534. doi: 10.1016/j.clindermatol.2007.08.006. [DOI] [PubMed] [Google Scholar]
- 21.Cohen AD. Gilutz H. Henkin Y. Zahger D. Shapiro J. Bonneh DY. Vardty DA. Psoriasis and the metabolic syndrome. Acta Derm Venereol. 2007;87:506–509. doi: 10.2340/00015555-0297. [DOI] [PubMed] [Google Scholar]
- 22.Cohen AD. Sherf M. Vidavsky L. Vardy DA. Shapiro J. Meyerovitch J. Association between psoriasis, the metabolic syndrome. A cross-sectional study. Dermatology. 2008;216:152–155. doi: 10.1159/000111512. [DOI] [PubMed] [Google Scholar]
- 23.Cotena C. Gisondi P. Colato C. Girolomoni G. Acneiform eruption induced by cetuximab. Acta Dermatovenerol Croat. 2007;15:246–248. [PubMed] [Google Scholar]
- 24.Gisondi P. Tessari G. Conti A. Piaserico S. Schianchi S. Peserico A. Giannetti A. Girolomoni G. Prevalence of metabolic syndrome in patients with psoriasis: a hospital-based case-control study. Br J Dermatol. 2007;157:68–73. doi: 10.1111/j.1365-2133.2007.07986.x. [DOI] [PubMed] [Google Scholar]
- 25.Neimann AL. Shin DB. Wang X. Margolis DJ. Troxel AB. Gelfand JM. Prevalence of cardiovascular risk factors in patients with psoriasis. J Am Acad Dermatol. 2006;55:829–835. doi: 10.1016/j.jaad.2006.08.040. [DOI] [PubMed] [Google Scholar]
- 26.Sterry W. Strober BE. Menter A. Obesity in psoriasis: The metabolic, clinical and therapeutic implications. Report of an interdisciplinary conference and review. Br J Dermatol. 2007;157:649–655. doi: 10.1111/j.1365-2133.2007.08068.x. [DOI] [PubMed] [Google Scholar]
- 27.Channual J. Wu JJ. Dann FJ. Effects of tumor necrosis factor-alpha blockade on metabolic syndrome components in psoriasis and psoriatic arthritis and additional lessons learned from rheumatoid arthritis. Dermatol Ther. 2009;22:61–73. doi: 10.1111/j.1529-8019.2008.01217.x. [DOI] [PubMed] [Google Scholar]
- 28.Offidani A. Cellini A. Valeri G. Giovagnoni A. Subclinical joint involvement in psoriasis: magnetic resonance imaging and X-ray findings. Acta Derm Venereol. 1998;78:463–465. doi: 10.1080/000155598442809. [DOI] [PubMed] [Google Scholar]
- 29.Zachariae H. Prevalence of joint disease in patients with psoriasis: Implications for therapy. Am J Clin Dermatol. 2003;4:441–447. doi: 10.2165/00128071-200304070-00001. [DOI] [PubMed] [Google Scholar]
- 30.Zachariae H. Zachariae R. Blomqvist K. Davidsson S. Molin L. Mork C. Sigurdeirsson B. Quality of life and prevalence of arthritis reported by 5,795 members of the Nordic Psoriasis Associations. Data from the Nordic Quality of Life Study. Acta Derm Venereol. 2002;82:108–113. doi: 10.1080/00015550252948130. [DOI] [PubMed] [Google Scholar]
- 31.Gelfand JM. Neimann AL. Shin DB. Wang X. Margolis DJ. Troxel AB. Risk of myocardial inarction in patients With psoriasis. JAMA. 2006;296:1735–1741. doi: 10.1001/jama.296.14.1735. [DOI] [PubMed] [Google Scholar]
- 32.Alberti KG. Eckel RH. Grundy SM. Zimmet PZ. Cleeman JI. Donato KA. Fruchart JC. James WP. Loria CM. Smith SC., Jr International Diabetes Federation Task Force on Epidemiology Prevention; National Heart Lung, Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; International Association for the Study of Obesity. Harmonizing the metabolic syndrome: a joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation. 2009;120:1640–1645. doi: 10.1161/CIRCULATIONAHA.109.192644. [DOI] [PubMed] [Google Scholar]
- 33.Krishnan E. Gout and coronary artery disease: epidemiologic clues. Curr Rheumatol Rep. 2008;10:249–255. doi: 10.1007/s11926-008-0039-0. [DOI] [PubMed] [Google Scholar]
- 34.Fernandez-Real JM. Ricart W. Insulin resistance and chronic cardiovascular inflammatory syndrome. Endocr Rev. 2003;24:278–301. doi: 10.1210/er.2002-0010. [DOI] [PubMed] [Google Scholar]
- 35.Rotter V. Nagaev I. Smith U. Interleukin-6 (IL-6) induces insulin resistance in 3T3-L1 adipocytes and is, like IL-8 and tumor necrosis factor-alpha, overexpressed in human fat cells from insulin-resistant subjects. J Biol Chem. 2003;278:45777–45784. doi: 10.1074/jbc.M301977200. [DOI] [PubMed] [Google Scholar]
- 36.Petersen AM. Pedersen BK. The anti-inflammatory effect of exercise. J Appl Physiol. 2005;98:1154–1162. doi: 10.1152/japplphysiol.00164.2004. [DOI] [PubMed] [Google Scholar]
- 37.Plomgaard P. Bouzakri K. Krogh-Madsen R. Mittendorfer B. Zierath JR. Pedersen BK. Tumor necrosis factor-alpha induces skeletal muscle insulin resistance in healthy human subjects via inhibition of Akt substrate 160 phosphorylation. Diabetes. 2005;54:2939–2945. doi: 10.2337/diabetes.54.10.2939. [DOI] [PubMed] [Google Scholar]
- 38.Uysal KT. Wiesbrock SM. Marino MW. Hotamisligil GS. Protection from obesity-induced insulin resistance in mice lacking TNF-alpha function. Nature. 1997;389:610–614. doi: 10.1038/39335. [DOI] [PubMed] [Google Scholar]
- 39.Choi HK. Hernan MA. Seeger JD. Robins JM. Wolfe F. Methotrexate and mortality in patients with rheumatoid arthritis: a prospective study. Lancet. 2002;359:1173–1177. doi: 10.1016/S0140-6736(02)08213-2. [DOI] [PubMed] [Google Scholar]
- 40.Kiortsis DN. Mavridis AK. Vasakos S. Nikas SN. Drosos AA. Effects of infliximab treatment on insulin resistance in patients with rheumatoid arthritis and ankylosing spondylitis. Ann Rheum Dis. 2005;64:765–766. doi: 10.1136/ard.2004.026534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Popa C. van den Hoogen FH. Radstake TR. Netea MG. Eijsbouts AE. den Heijer M. van der Meer JW. van Riel PL. Stalenhoef AF. Barrera P. Modulation of lipoprotein plasma concentrations during long-term anti-TNF therapy in patients with active rheumatoid arthritis. Ann Rheum Dis. 2007;66:1503–1507. doi: 10.1136/ard.2006.066191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Dahlqvist SR. Engstrand S. Berglin E. Johnson O. Conversion towards an atherogenic lipid profile in rheumatoid arthritis patients during long-term infliximab therapy. Scand J Rheumatol. 2006;35:107–111. doi: 10.1080/03009740500474578. [DOI] [PubMed] [Google Scholar]
- 43.Marra M. Campanati A. Testa R. Sirolla C. Bonfigli AR. Franceschi C. Marchegiani F. Offidani A. Effect of etanercept on insulin sensitivity in nine patients with psoriasis. Int J Immunopathol Pharmacol. 2007;20:731–736. doi: 10.1177/039463200702000408. [DOI] [PubMed] [Google Scholar]