Abstract
Context:
Boston ocular surface prosthesis (BOSP) is a scleral contact lens used in the management of patients who are rigid gas permeable (RGP) failures as with corneal ectasias such as keratoconus and in those patients who have ocular surface disease such as Stevens–Johnson syndrome (SJS).
Aim:
To report utilization of BOSP in a tertiary eye care center in India.
Materials and Methods:
We retrospectively reviewed charts of 32 patients who received BOSP from July 2008 to May 2009. Indications for fitting these lenses, improvement in visual acuity (VA) before and after lens fitting and relief of symptoms of pain and photophobia were noted. Paired t-test was used for statistical analysis using SPSS version 16.0 for Windows.
Results:
Thirty-two patients (43 eyes) received these lenses. These consisted of 23 eyes of 17 patients who failed RGP trials for irregular astigmatism and corneal ectasia such as keratoconus and post radial keratotomy and scar and 20 eyes of 15 patients with SJS. Mean age of RGP failures was 27.94 years. Pre- and post-BOSP wear mean LogMAR VA was 1.13 and 0.29, respectively, in RGP failures. The P value was statistically significant (P < 0.001). In patients with SJS, LogMAR VA was 0.84 ± 0.92 before and 0.56 ± 0.89 after lens wear. The P value was statistically significant (P < 0.001). VA improved by >2 lines in 7/20 eyes (35%) with SJS, with improvement in symptoms.
Conclusion:
BOSP improves VA in patients who have irregular astigmatism as in ectasias and RGP failures and improves vision and symptoms in patients with SJS.
Keywords: Boston ocular surface prosthesis, India, keratoconus, scleral contact lens, Stevens–Johnson syndrome
Boston ocular surface prosthesis (BOSP) is a fluid-filled scleral contact lens. Scleral contact lenses are useful in the visual rehabilitation of patients who have irregular astigmatism and corneal ectasia where the fitting of the regular corneal lenses is not possible, thus eliminating or delaying the need for keratoplasty. These are also beneficial for relief of symptoms and improvement in vision in patients with ocular surface disease such as Stevens–Johnson syndrome (SJS).
These lenses rest on sclera and do not touch the cornea [Fig. 1]. Being fluid ventilated, there is a constant pool of tears over the cornea, which acts as a liquid corneal bandage in various ocular surface disorders such as SJS, graft versus host disease (GvHD), chemical injuries, dry eyes, limbal stem cell deficiency, neurotrophic corneas, superior limbal keratoconjunctivitis, Sjogren syndrome, ocular cicatricial pemphigoid, exposure keratitis, and toxic epidermal necrolysis.[1–3] These lenses are also useful in patients who have irregular astigmatism and corneal ectasia where either the rigid gas permeable (RGP) fitting is not possible or the patients are intolerant to contact lens. The scleral contact lens masks the corneal surface astigmatism and improves vision in these patients.[1,4] As there is no literature on the use of these lenses in the Indian population, our aim is to report our experience of BOSP in a tertiary eye care center in India.
Figure 1.
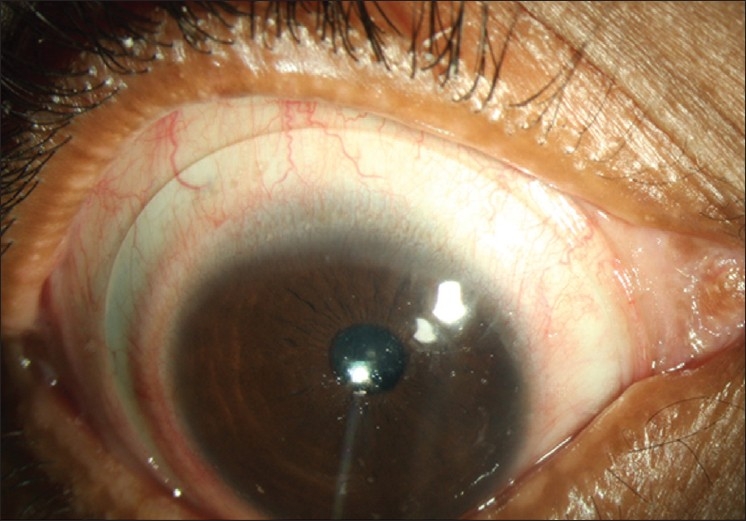
The scleral contact lens is resting on sclera. The haptic portion of the scleral lens showing no blanching of the conjunctival vessels as seen superiorly
Materials and Methods
We retrospectively reviewed the charts of patients who received the BOSP from July 2008 to May 2009, from the computerized database. These were referred patients by the cornea specialists. All patients who received BOSP for vision improvement for corneal ectasias were documented separately as RGP failures. All these patients had failed regular corneal lenses trial before they were fitted with BOSP. The patients who were given lenses for SJS had disabling symptoms of photophobia and pain. These patients were using lubricating eye drops and ointments. The main goal of giving BOSP in these patients was to alleviate the symptoms; the secondary goal was to improve the visual acuity (VA).
All patients gave informed consent regarding the risks and benefits of wearing BOSP with a clear, well-defined primary goal of improving vision as in ectasias or symptomatic relief as in ocular surface diseases.
The BOSP diameter ranged between 15.5 and 18.5 mm. These are lathe-cut lenses with a special CAD-CAM software to customize the lens design in terms of haptic bearing and vault for individual patients.[1] The acceptability of the fit was determined by direct observation of the haptic if resulting in any compression of conjunctival vessels [Fig. 1]. The corneal clearance was assessed directly on slit lamp with slit beam [Fig. 2]. The fitting procedure included assessment of fitting immediately after lens wear, then after 1 hour, 3–4 hours of lens wear and then after 6 hours of lens wear. This was done by assessing the compression pattern before lens removal and conjunctival fluorescein staining pattern after the lens removal. Once the initial fitting was done, the patients were seen again after a month of their lens wear.
Figure 2.
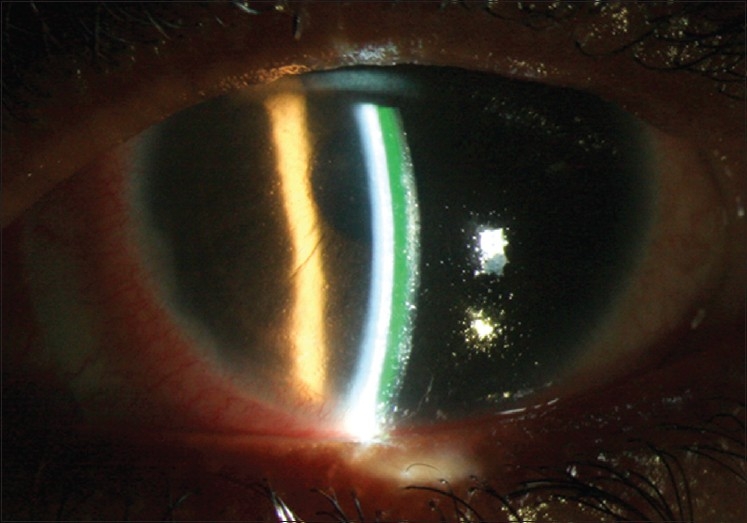
Slit view on slit lamp examination showing a clear, fluid-filled area between the posterior surface of the lens and the cornea, indicating vault and no touch to cornea
We analyzed indications and the outcomes in those patients who were dispensed with BOSP in our center from July 2008 to May 2009.
Results
Forty-three eyes of 32 patients were dispensed with BOSP. The primary indication for BOSP was divided into two categories: vision improvement in failed RGP lenses and for symptomatic relief in SJS. Some patients had multiple indications.
Twenty-three eyes of 17 patients were fitted with BOSP for vision improvement. Of these 17 patients, one patient had corneal scar in the visual axis after corneal tear repair for penetrating injury and one had irregular astigmatism after radial keratotomy (RK). Rest of the patients had keratoconus. All keratoconus patients had, in addition to ectasia, scars in the visual axis. One patient each had dry eye and vernal keratoconjunctivitis. Mean age of these patients was 27.94 ± 15.28 years. The pre- and post-BOSP fitting mean logMAR VA was 1.13 ± 0.67 and 0.29 ± 0.41, respectively. The P value was statistically significant (P < 0.001) as calculated by paired t-test using SPSS version 16.0 for windows. The mean follow-up was 6.9 months.
The BOSP was used as a liquid corneal bandage in 20 eyes of 15 consecutive patients who had SJS for symptomatic relief. One patient had, in addition to SJS, keratoconus in both eyes. The patients were given lenses mostly after the skin lesions healed in these patients. The lens diameter in these patients ranged from 15.5 to 18 mm depending on the presence of symblepharon.
In SJS, the VA deteriorated after some hours of lens wear, with collection of debris either in the fluid compartment or on the surface of the lenses in these patients. This required removal and reinsertion of the lenses for improving both comfort and clarity of vision. Eight eyes of five patients had debris formation which was more in the first month when they started using the lenses and subsequently these patients were using lenses on an average of 8 hours/day as the VA would deteriorate later. The lenses were worn whenever the patients were awake. The patients needed to clean the lenses off the debris and reinsert these lenses after an average of 8 hours. The frequency of instillation of the drops in the eye was same before and after the lens wear in these patients but the patients reported relief from symptoms of pain and photophobia, which they were experiencing before the lens wear. This was more so in patients who had associated trichiasis and severe keratinization of lid margins. The patients still had persistent epithelial erosions that did not resolve. In patients with SJS, LogMAR VA was 0.84 ± 0.92 before lens insertion and 0.56 ± 0.89 after lens insertion. The P value was statistically significant (P = 0.001). BCVA improved by more than 2 lines in 7/20 eyes (35%). None of the patients, even those from SJS group, thought that it was psychologically frightening or they were unable to wear lenses. No additional surgeries such as symblepharon release were performed for getting an acceptable fitting.
Discussion
BOSP is known to be effective in various corneal conditions like ectasias as well as severe ocular diseases.[1–5] In our series, eyes which had primary indication as improvement in the vision were patients who were RGP failures either because of inability to get an acceptable fit with regular RGP lenses or were contact lens intolerant. Most of these patients were with keratoconus except one each with scar and post RK. Keratoconus is the most common indication for optical penetrating keratoplasty and most of the patients are young. The main indication for surgery in keratoconus is either inability to get a good fit or contact lens intolerance. The patients with keratoconus were fitted with BOSP to assess the VA improvement before considering them for surgery as the last alternative. Mean age of patients who were fitted with BOSP for vision improvement was 27.94 years. Most of these patients may require surgery eventually in their lifetime.[6] Yildiz et al, had reported that about 59.8% of patients above 50 years underwent keratoplasty for keratoconus.[7] Keratoplasty is known to be associated with various complications such as rejection, infections and graft failures. BOSP helps in either delaying or obviating the need for keratoplasty in these patients as the complications reported in the literature are less with these lenses. This is similar to other series where the most common indication for scleral contact lenses is keratoconus.[2,4,5]
The patients who received BOSP for therapeutic purpose were mostly SJS. All the patients had relief from the symptoms of pain and photophobia. Penetrating keratoplasty has poor prognosis in SJS and may be performed for tectonic reasons, but prospects for restoration of sight are limited.[8] With the ability of opening the eye and relief from symptoms, the VA improved in these patients, which was a secondary goal. It is considered that BOSP reduces the shearing action of the lids on cornea and prevents desiccation of cornea. This may be because the precorneal fluid of lens acts as precorneal tear film and changes the environment of the cornea in these patients.[3] Romero-Rangel et al, had reported SJS as the most common indication for fitting of these lenses. Fifty-four out of 76 eyes had SJS in their series.[9] The scleral lenses with the precorneal tear film and corneal clearance protect the corneal surface from the progressive changes in various ocular surface diseases.[10] No patients had any untoward ocular complications.
In conclusion, although our study has the limitation of not being able to quantify the symptomatic relief, in patients with SJS, the results with BOSP are encouraging. So is the case in patients with irregular astigmatism and corneal ectasia, corneal scars and post RK. BOSP is useful in patients who fail with regular corneal contact lenses and would need keratoplasty and also in patients of SJS, for the relief of symptoms.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Rosenthal P, Cotter P. The Boston Scleral Lens in the management of severe ocular surface disease. Ophthalmol Clin North Am. 2003;16:89–93. doi: 10.1016/s0896-1549(02)00067-6. [DOI] [PubMed] [Google Scholar]
- 2.Pullum KW, Whiting MA, Buckley RJ. Scleral contact lenses: The expanding role. Cornea. 2005;24:269–77. doi: 10.1097/01.ico.0000148311.94180.6b. [DOI] [PubMed] [Google Scholar]
- 3.Jacobs DS, Rosenthal P. Boston Scleral lens prosthetic device for the treatment of severe dry eye in chronic graft-versus-host disease. Cornea. 2007;26:1195–9. doi: 10.1097/ICO.0b013e318155743d. [DOI] [PubMed] [Google Scholar]
- 4.Tan DT, Pullum KW, Buckley RJ. Medical applications of scleral contact lenses: 1, A retrospective analysis of 343 cases. Cornea. 1995;14:121–9. [PubMed] [Google Scholar]
- 5.Segal O, Barkana Y, Hourovitz D, Behrman S, Kamun Y, Avni I, et al. Scleral contact lenses may help where other modalities fail. Cornea. 2003;22:308–10. doi: 10.1097/00003226-200305000-00006. [DOI] [PubMed] [Google Scholar]
- 6.Siganos CS, Tsiklis NS, Miltsakakis DG, Georgiadis NS, Georgiadou IN, Kymionis GD, et al. Changing Indications for Penetrating Keratoplasty in Greece, 1982-2006: A multicenter study. Cornea. 2010;4:372–4. doi: 10.1097/ICO.0b013e3181bd44a1. [DOI] [PubMed] [Google Scholar]
- 7.Yildiz EH, Diehl GF, Cohen EJ, Hammersmith KM, Laibson PR, Rapuano CJ, et al. Demographics of patients older than 50 years with keratoconus. Eye Contact Lens. 2009;35:309–11. doi: 10.1097/ICL.0b013e3181be5784. [DOI] [PubMed] [Google Scholar]
- 8.Tugal-Tutkun I, Akova YA, Foster CS. Penetrating keratoplasty in cicatrizing conjunctival diseases. Ophthalmology. 1995;102:576–85. doi: 10.1016/s0161-6420(95)30980-3. [DOI] [PubMed] [Google Scholar]
- 9.Romero-Rangel T, Stavrou P, Cotter J, Rosenthal P, Baktatzis S, Foster CS. Gas-permeable scleral contact lens therapy in ocular surface disease. Am J Ophthalmol. 2000;130:25–32. doi: 10.1016/s0002-9394(00)00378-0. [DOI] [PubMed] [Google Scholar]
- 10.Pullum K, Buckley R. Therapeutic and ocular surface indications for scleral contact lenses. Ocul Surf. 2007;5:40–8. doi: 10.1016/s1542-0124(12)70051-4. [DOI] [PubMed] [Google Scholar]


