Abstract
Background:
Day care surgery is still in its infancy in India. Both regional and general anaesthesia can be used for this. Central neuraxial blocks are simple cheap and easy to perform. This study was done to evaluate usefulness of spinal and epidural anaesthesia for day care surgery.
Patients & Method:
100 patients were randomized to either spinal (n=50) or epidural (n=50) group anaesthetized with either 0.5% hyperbaric 2ml bupivacaine or 0.5% 20ml bupivacaine respectively. In spinal group 27 gauze quincke needle and in epidural group 18 gazue tuohy needle was used. Both the groups were compared for haemodynamic stability, side effects, complications, postanaesthesia discharge score (PADS), time taken to micturate, total duration of stay in hospital and patient satisfaction score for technique.
Results:
We observed that spinal anaesthesia had significantly early onset of anaesthesia and better muscle relaxation (p<0.05) as compared to epidural block otherwise both groups were comparable for haemodynamic stability, side effects or complications. Although more patients in spinal group (64% vs 48%) achieved PADS earlier (in 4-8 hours) but statistically it was insignificant. Time to micturition (6.02 0.55 v/s 6.03 0.47 hours) and total duration of stay (7.49 1.36 v/s 8.03 1.33 hours) were comparable in both the groups.
Conclusion:
Both spinal and epidural anaesthesia can be used for day care surgery. Spinal anaesthesia with 27 gauze quincke needle and 2ml 0.5% hyperbaric bupivacaine provides added advantage of early onset and complete relaxation.
Keywords: Day Care, Spinal, Epidural, Bupivacaine
Recent advances in anaesthetic and surgical techniques have resulted in increasing number of surgical procedures being performed on day care basis. According to international terminology, day surgery or ambulatory surgery is the admission of selected patients to hospital for a planned, non emergency surgical procedure, returning home on the same day1.
The requirements for anaesthesia for day care surgery are those of any anaesthetic agent having rapid, painless induction, profound analgesia and anaesthesia without depression of the cardiovascular and respiratory system and rapid smooth recovery2. There are so many benefits of ambulatory surgery like cost effectiveness, low morbidity and mortality, lower incidence of infection, lack of dependence on the availability of hospital beds and shorter surgical waiting lists3.
Different options are available e.g. general anaesthesia with newer short acting agents e.g. propofol and isoflurane4 or regional anaesthesia techniques5. Advantages of regional anaesthesia over general anaesthesia include less cardiovascular or respiratory complications, less initial postoperative pain, patient's ability to communicate with the surgeon and reduced cost of drugs and equipment involved in regional anaesthesia.6
However, there are few potential disadvantages of regional anaesthesia which includes time taken for block insertion and onset, needs active cooperation with patient and surgeon, risk of nerve damage, variable failure rates and urinary retention5.
The present study was done to evaluate usefulness of spinal and epidural anaesthesia for day care surgery in lower limb and inguinoscrotal region.
PATIENTS AND METHODS
After approval from the institutional ethical committee and written informed consent, 100 patients, in the age group 20-55 years of either sex, ASA grade I and II were included in the study. The patients were randomly divided into two groups of 50 each.
Group A received spinal anaesthesia with 2 ml 0.5% hyperbaric bupivacaine in L3-L4 space and group B received epidural anaesthesia with 20 ml 0.5% isobaric bupivacaine in L3-L4 space.
Written and informed consent was taken after explaining the procedure to the patient prior to administration of block. A day before surgery, all patients were examined and thoroughly investigated. Patients having bleeding diathesis, on any anticoagulant therapy, having history of drug abuse, morbidly obese, surgery expected to have major fluid or blood loss, patients who did not have any competent friend or relative to accompany or drive patient home after operation and to look after him or her at home for the next 24-48 hours were excluded from study.
All the patients were advised to take tab. alprazolam 0.5 mg at night. Midazolam 2 mg and 0.2 mg of glycopyrrolate intravenous was administered before anaesthesia was started.
All the patients were preloaded with 10 ml kg-1 body weight of ringer lactate solution over 15-20 minutes In group A spinal anaesthesia was given with Quincke needle No. 27 and 2 ml of 0.5% hyperbaric bupivacaine was injected into subarachnoid space. In group B epidural anaesthesia was given with 18 gauge Touhy needle and 20 ml of 0.5% bupivacaine was given after the test dose.
After the block gets fixed, the level of sensory block was checked with pin prick. Motor blockade was checked by modified Bromage score as used by Breen et al. Operation was started when full surgical anaesthesia had been attained. Pulse rate, blood pressure, respiratory rate and oxygen saturation of arterial pulsation (SpO2) was recorded every five minutes upto 20 minutes then every 10 minutes till the end of surgery.
If needed, supplementation of anaesthesia was given and if complete failure occurred then those patients were excluded from this study. Diclofenac rectal suppository 100 mg was given to all the patients in both the groups after surgical procedure was over. After the surgical procedure, all the vitals (pulse rate, blood pressure, SPO2 and respiratory rate) were monitored. Any side effects like hypotension, bradycardia/tachycardia nausea, vomiting, urinary retention, headache and backache were also noted. Presence of complications such as dural puncture in case of epidural anaesthesia, total spinal and signs/symptoms of local anaesthetic toxicity were also noted. Any additional analgesic besides diclofenac suppository and any other drug like anti emetics, sedatives and vasopressors if given, were noted. After discharge, patient and doctor remained in contact with each other telephonically upto 48 hours.
Patients were discharged on the same day according to postanaesthesia discharge scoring system (PADS ).Total duration of stay in the hospital was noted in each case. Then, patient satisfaction was noted on a 5 point scale for next 24 hours and 48 hours telephonically which was already explained to all the patients preoperatively Satisfaction score was: 5- Very satisfied, 4–Satisfied, 3–Neutral, –issatisfied, 1-Very dissatisfied.
All the results were recorded and analysed statistically using unpaired students ‘t’ test and chi square test, p values <0.05 were taken as significant.
RESULTS
There were no significant differences in age, sex, height, body weight, ASA (American Society of Anaesthesiologist) grade and duration of stay amongest two groups (table 1)
Table 1.
Demographics characteristics
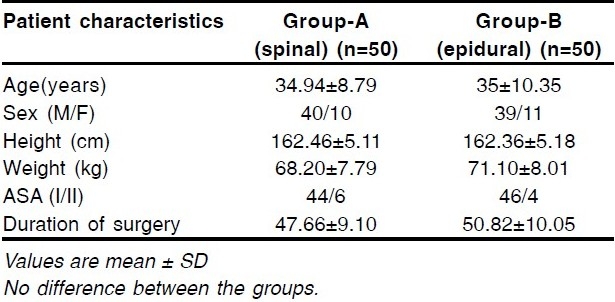
The anaesthesia onset time (as assessed by pin prick) was early in spinal group as compared to epidural group and significantly more number of patients in spinal group achieved modified bromage score of 1 as compared to epidural group (table 2). Both the groups were comparable regarding changes in pulse rate, systolic blood pressure, diastolic blood pressure, respiratory rate and SpO2 (saturation of arterial pulsation of oxygen) and there were few patients in both groups who developed hypotension and bradycardia intraoperatively (table 3) who promptly responded to intravenous fluids and inj atropine and inj ephedrine and none if patients in either group had postoperative hypotension and bradycardia.
Table 2.
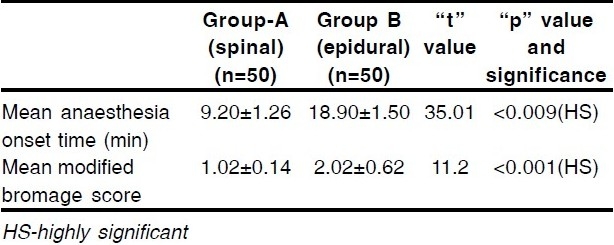
Table 3.
Side effects and complications
The overall side effect are listed in table 3. Only 1 patient in spinal group and 2 patients in epidural group had urinary retention and in rest of the patients time taken to micturite was comparable.
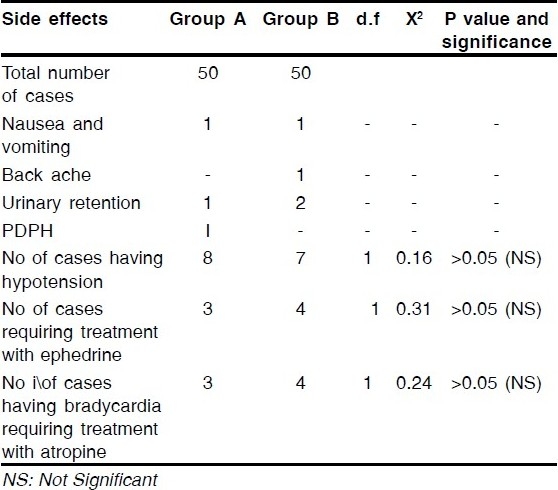
There was no statistical difference between the two groups regarding the time to achieve PAD score (figure 1) or in total duration of stay (figure 2). 92% of patients in spinal group and 90% of patients in epidural group were discharged on the same day. In spinal group 98% of patients and in epidural group 96% of patients(figure 3) were satisfied from technique used (satisfaction score 4 or 5).
Figure 1.
Showing Time To Achieve Post Anaesthesia Discharge Score
Figure 2.

Showing Mean Total Duration of Stay in Hospital in Day Case Patients
Figure 3.

Showing Overall Satisfaction Score At 24 And 48 Hours
DISCUSSION
Day surgery is a cost effective, quality approach to surgery that has rapidly expanded in the recent years1.
Moderen anaesthetic drugs for ambulatory general anaesthesia are expensive, Spinal and epidural are relatively simple techniques and the cost of drugs and equipment for regional anaesthesia are generally low. Cost of postoperative medication for pain or nausea may also be reduced with regional anaesthesia.
We observed shorter anaesthesia onset time in spinal anaesthesia (table 2) as compared to epidural anaesthesia. These results are in consistence with results shown by Davis et al.7 They observed time to achieve maximum cephalad spread to be 13±7 min in spinal anaesthesia with 0.5% hyperbaric bupivacaine and 21±4 min in epidural anaesthesia with 0.5% bupivacaine.
Muscle relaxation as assessed by modified bromage score was more in spinal group as compared to epidural group.(table 2) Davis et al7 has similarly found mean bromage score of 1 after spinal anaesthesia vs 3.86 after epidural anaesthesia.
Both the groups remained haemodynamically stable after spinal anaesthesia and epidural anaesthesia.
There were only few side effects and complication in both the groups. Less nausea and vomiting in our study is due to low level chosen because nausea and vomiting during regional anaesthesia are more common when sympathetic block extend above sixth thoracic segment8
Despond et al9 in their study, PDPH in young orthopaedic patients using 27 G needles (whittcre and Quincke), found incidence of 9.3% in both the groups. The incidence was more in women than men. In our study only single patient in spinal group developed post dural puncture headache (PDPH) which responded adequately to intravenous fluids and oral analgesics .Lower incidence of post dural puncture headache is attributable to use of fine gauze (27 number quincke) needle in our study . In our study maximum number of patients were males.
In spinal group 1 (2%) patient and in epidural group 2 (4%) patients had urinary retention (i.e. full bladder on palpation and inability to micturite 8 hours postoperatively and associated with discomfort). Davis et al7 in study comparing spinal and epidural anaesthesia reported 7 (out of 32) patients in spinal group and 14 (out of 30) in epidural group who needed catheterization. Low incidence of urinary retention in our study as compared to this was due to lower dose of anaesthetic used in spinal group (10 mg) and use of single shot technique for epidural anaesthesia. Moreover their mean catheterization time was 4.2 ±1.7 hours in in spinal group and 4.7±2.3 hours in epidural group and we waited for at least 8 hours for patient to micturite spontaneously and before that catheterization was done only if indicated clinically.
Post anaesthesia discharge score (PADS) was noted after surgery and patients were discharged only when they achieved total score of =9. In spinal group 32 (62%) patients and in epidural group 24 (48%) patients achieved discharge criteria with in 4-8 hours while (28%) patients in spinal group and 21(42%) patients in epidural group achieved discharge criteria with in 8-12 hours .So clinically more number of patients in spinal group achieved discharge criteria early within 4-8 hours but this difference from epidural group was statistically insignificant. 92% patients in spinal group and 90% patients in epidural group were discharged on the same day and both the groups were statistically in significant for total duration of stay in hospital after surgery.
Kallio et al10 also reported that their patients were fit for discharge after 6.0 hours (5.2-6.6hours) and were discharged after 6.6 hours (5.9-9.0 hours) after 10mg of plain bupivacaine with spinal anaesthesia .They discharged 80% of their patients on the same day .Pittoni et al8 also discharged their 97% of patients from hospital on the same day after spinal anaesthesia with hyperbaric bupivacaine with use of 22 gauze and 25 gauze sprotte needle and their patients recovered from block and were fit for discharge with in 10 hours. Gunal et al11 in their study comparing spinal anaesthesia (with 20 mg 0.5% hyperbaric bupivacaine) and epidural anaesthesia (with 100 mg 0.5% bupivacaine) for inguinal hernia repair found stand up time (ie time by which patient was able to ambulate after surgery) after epidural anaesthesia to be 9.4±1 hours and 5.7±1 hours after spinal anaesthesia but their average hospital stay after spinal anaesthesia was 1.8±0.2 days and 1.8±0.1 days after epidural anaesthesia and their greater number of patients in epidural group behaved as day case patients. They blamed postoperative pain for delay in discharge .we attribute our shorter discharge times to low dose of bupivacaine used in our study (10 mg 0.5% hyperbaric bupivacaine) in spinal group and better postoperative pain relief due to use of 100mg diclofenac rectal suppository at the end of procedure which provided painless postoperative period and speeded discharge in our study.
Patient's satisfaction score as noted telephonically was comparable between two groups. Patients having score of 4 (satisfied) or 5 (very satisfied) were taken as satisfied for the purpose of statistical analysis and it was found that 98% of patients who received spinal anaesthesia and 96% of patients who received epidural anaesthesia were satisfied from technique used. Similarly in study by Pollock12 comparing spinal and epidural anaesthesia for outpatient knee arthroscopy reported 92% patients of epidural group and 97% of spinal group were either extremely or very satisfied from their anaesthetic technique used.
From the present study, we conclude that spinal block produces an early and significantly more effective analgesia and more intense motor blockade than epidural block. The haemodynamic changes and side effects following the two techniques are similar with no significant difference. Two blocks are not different as per time taken to micturate and total duration of stay in hospital after the surgery. Thus both spinal and epidural anaestheisa can be satisfactorily used for day care surgery. Spinal anaesthesia with 27 gauze quincke needle and 2ml 0.5% hyperbaric bupivacaine provides added advantage of early onset and complete relaxation.
Footnotes
Authors disclosure Authors have no conflict of interest and financial considerations.
REFERENCES
- 1.Castoro C. Ambulatory Surgery: Current Status and Future Trends. East and Central African Journal of Surgery. 2006;11(1):67–68. [Google Scholar]
- 2.Goold JE. Anaesthesia for day-care surgery: a review. J R Soc Med. 1983;76:415–420. doi: 10.1177/014107688307600517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Miller RD, Fleisher LA, John RA, Young WL, Jeanine P, Kronish W, et al. Miller's Anaesthesia. Churchill Livingstone. (Sixth ed) 2005:2590. [Google Scholar]
- 4.Warner MA, Sheilds SE, Chute CG. Major morbidity and mortality within 1 month of ambulatory surgery and anaesthesia. JAMA. 1993;270:1437–1441. doi: 10.1001/jama.270.12.1437. [DOI] [PubMed] [Google Scholar]
- 5.Korttila K. Regional anaesthesia for outpatients. Eur Soc Anaesthesiol. 1999:1–8. [PubMed] [Google Scholar]
- 6.Raeder JC. Regional anaesthesia in ambulatory surgery. Can J Anaesth. 2001;48:1–8. [Google Scholar]
- 7.Davis S, Erskine R, James MF. A comparison of spinal and epidural anaesthesia for hip arthroplasty. Can J Anaesth. 1992;39:551–554. doi: 10.1007/BF03008316. [DOI] [PubMed] [Google Scholar]
- 8.Pittoni G, Toffoletto F, Calcarella G, Zanette G, Giron GP. Spinal anaesthesia in outpatient knee surgery: 22 gauze versus 25 gauze sprotte needle. Anesth Analg. 1995;81:73–79. doi: 10.1097/00000539-199507000-00015. [DOI] [PubMed] [Google Scholar]
- 9.Despond O, Meuret P, Hemmings G. Postdural puncture headache after spinal anaesthesia in young orthopaedic outpatients using 27-gauze needles. Can J Anaesth. 1998;45(11):1106–1109. doi: 10.1007/BF03012401. [DOI] [PubMed] [Google Scholar]
- 10.Kallio H, Snall EVT, Kero MP, Rosenberg PH. A comparison of intrathecal plain solutions containing Ropivacaine 20 or 15 mg versus bupivacaine 10 mg. Anesth Analg. 2004;99:713–717. doi: 10.1213/01.ANE.0000129976.26455.32. [DOI] [PubMed] [Google Scholar]
- 11.Gunal O, Arikan Y, Celikel N. Clinical assessment of spinal and epidural anaesthesia in inguinal hernia repair. J Anaesth Clin Pharmacol. 2002;16(2):119–122. doi: 10.1007/s005400200005. [DOI] [PubMed] [Google Scholar]
- 12.Pollock JE, Mulroy MF, Bent E, Polissar NL. A comparison of two regional anaesthetic techniques for outpatient knee arthroscopy. Anesth Analg. 2003;97:397–401. doi: 10.1213/01.ANE.0000070226.10440.3A. [DOI] [PubMed] [Google Scholar]


