Abstract
Empirical findings have identified spirituality as a potential health resource. Whereas older research has associated such effects with the social component of religion, newer conceptualizations propose that spiritual experiences and the intrapersonal effects that are facilitated by regular spiritual practice might be pivotal to understanding potential salutogenesis. Ongoing studies suggest that spiritual experiences and practices involve a variety of neural systems that may facilitate neural ‘top-down’ effects that are comparable if not identical to those engaged in placebo responses. As meaningfulness seems to be both a hallmark of spirituality and placebo reactions, it may be regarded as an overarching psychological concept that is important to engaging and facilitating psychophysiological mechanisms that are involved in health-related effects. Empirical evidence suggests that spirituality may under certain conditions be a predictor of placebo response and effects. Assessment of patients' spirituality and making use of various resources to accommodate patients' spiritual needs reflect our most current understanding of the physiological, psychological and socio-cultural aspects of spirituality, and may also increase the likelihood of eliciting self-healing processes. We advocate the position that a research agenda addressing responses and effects of both placebo and spirituality could therefore be (i) synergistic, (ii) valuable to each phenomenon on its own, and (iii) contributory to an extended placebo paradigm that is centred around the concept of meaningfulness.
Keywords: spirituality, spiritual practice, salutogenetic effects, meaningfulness, placebo, neuronal top-down effects
1. Introduction
The last decades have seen a significant increase in scientific research endeavours that attempt to identify and understand processes relevant to the somewhat enigmatic phenomenon known as ‘placebo’ or, more precisely, the ‘placebo response’. By definition, placebo refers to ‘a reduction in a symptom in an individual that results from ones perception of the therapeutic intervention. This response may be considered both a biological and psychological event’ [1]. Critical to such research is the finding that placebo responses involve expectation, optimism and other states of motivational, emotional or cognitive appetence or aversion. These states appear to initiate and/or mediate salutary (i.e. health generating and/or sustaining) effects, in part, through neural ‘top-down’ mechanisms that engage brain/mind substrates to alter bodily processes. Studies have suggested that certain types of practices and person–environment interactions, including types of meditation, yogic states and so-called ‘optimal healing environments’, may involve common neural networks to produce health and healing effects [2,3]. Many of these manifest ‘spiritual’ connotations and meanings, reflecting a formal definition provided by the Fetzer Institute that defines spirituality as ‘concerned with the transcendent, addressing ultimate questions about life's meaning, with the assumption that there is more to life than what we see or fully understand’ [4, p. 2]. Recent research addressing the relationship between spirituality and health has provided empirical findings to support that spirituality—in a generic sense (i.e. beliefs, practices and experiences)—can incur salutogenic consequences [5–8]. Thus, in this contribution we investigate whether spiritual practices and experiences may be regarded as a potential form, correlate, and/or predictor of placebo response and effects, particularly as they seem to be driven by psychophysiological mechanisms that are similar—if not identical—to ‘conventional’ placebo phenomena. Indeed, experimental studies by Hyland et al. have identified spirituality as a predictive variable of placebo response—independent of expectancy—in an open self-treatment design [9,10].
Neuroscience has shed new light upon the role of the brain and cognitive and emotional processes in both placebo and spiritual experiences and effects, and has revealed that overlapping anatomical and neurochemical substrates appear to be involved in (many aspects of) these phenomena [11–15]. It has additionally been suggested that cognitive processes of learning and memory are involved, and experiments have provided evidence for salutary training effects derived from regular spiritual, contemplative or meditative practice [16,17]. As well, epidemiological data from twin studies indicate that spiritual experiences and behaviours are also influenced by environmental and cultural factors [18,19]. This is especially true of psychological variables such as expectation, meaningfulness, purposefulness and optimism [20–23], which seem to be key features common to both spiritual experiences and placebo responses. These involve multi-factorial cognitive, emotional, motivational and even behavioural domains and functions, and therefore are unlikely to be subserved by, or relegated, to a single, neural network, brain region or site. Rather, it seems that spiritual experiences—and placebo responses—are complex phenomena that, although facilitated by neuropsychophysiological processes, are largely dependent upon both personal and cultural contexts, and thus are reliant upon multiple types and extent(s) of bio-psychosocial interactions and effects [24,25]. However, posing the question of whether spiritual practices and/or the experiences they provoke might be a form of placebo response may generate consternation from certain factions. This may in no small part be due to the fact that the terms placebo and placebo effect retain a considerable burden of ‘folk’ or colloquial meaning, reflecting the connotation of a ‘dummy’ or ‘sham’ treatment. This may reflect the epistemology of medicine and neuroscience, which until only quite recently was rather closed to such concepts [26,27]. Yet, the fact that spiritual and placebo effects have been clinically observed and documented has tacitly affected the worldview of neuroscience, and medicine as well, and has resulted in a re-address and re-consideration of such mind-body effects. Indeed, Giordano has claimed that such definitional ambiguity (regarding both placebo and the notion of ‘spirituality’ as confused with religion or religiosity) can generate and ‘…sustain both philosophical and pragmatic problems’ related to the veridicality, value and utility of spirituality and placebo in health sciences and medicine. Therefore, as Giordano & Engebretson [24] have noted, although the effects of spirituality on the body cannot be seen as monocausal events, a mechanistic understanding of spiritual and placebo effects may nevertheless be critical to establishing explanatory models that are relevant and resonant to scientists, clinicians and patients alike. There is a growing corpus of literature—and increasing interest—to further elucidate how such mechanisms could deepen insight(s) into the proverbial ‘mind–body problem’, and also perhaps open new and promising venues for medical care and forms of healing [28,29].
In this review, we advocate the position that such a research agenda addressing mechanisms, responses and effects of both placebo and spiritual experiences and practices could therefore be (i) synergistic, (ii) valuable to each phenomenon on its own, and (iii) important to an extended placebo paradigm that is centred around the concept of meaningfulness. We shall present an overview of the results and problems arising in and from investigations of the spirituality–health connection, discuss the mechanisms involved in spiritual experiences and practices and offer the premise that such effects may co-mediate placebo response, and that individual patterns of spiritual belief, conditioning, expectation and experience may be important factors in (i) reflecting the aforementioned mechanisms, and (ii) predicting placebo response.
2. Investigating the relationship between spirituality and health
(a). Problems defining key terms: spirituality–religiosity–religion–mindfulness
Investigations of the spirituality–health connection suffer from a lack of consensual agreement about key concepts, including a definition of the term spirituality [30,31]. We have therefore offered a rather broad definition of spirituality as an implicit or explicit habit of being oriented towards, searching for and expressing a reality transcending immediate and mediate personal needs, and/or a striving for experiencing a universal or transcendental dimension [32]. This engagement with a spiritual or transcendental dimension may be individually manifest on cognitive, emotional, motivational and behavioural levels, and may also have social and cultural dimensions and effect(s).
Problems arise when attempting to differentiate the term spirituality from other, somewhat related terms and constructs such as religion, religiosity, meaningfulness or purposefulness. Whereas the early literature had frequently used the terms spirituality and ‘religion’ in a fungible manner and thus a rather naive way, newer research seems to increasingly differentiate between these two constructs [8,33]. Still, it is important to briefly consider common ground as well as points of divergence between these terms and concepts [34]. An individual may possess and enact spiritual faith in a higher being, ultimate power of nature and/or transcendental principle, while not necessarily being aligned to any form of orthodox religion. On the other hand, it is also possible to develop a deep-rooted spiritual conviction that is adherent to tenets of an established and culturally shaped and reinforced religious creed, but at the same time, not have experienced any personal sense of a divine or transcendental component. As these examples show, identifying precise demarcation criteria for differentiating spirituality and religiosity or religious behaviour and other related constructs is far from easy, as these all describe complex, multi-dimensional phenomena that are difficult to grasp, and are not necessarily mutually exclusive.
However, there is an aspect that might at least provide a heuristic for such differentiation: whereas spirituality points to the subjective, experiential and private dimensions of transcendence, religion refers to objective (i.e. culturally manifested) and social dimensions that offer a cultural framework for the interpretation of spirituality. In other words, religious traditions may be interpreted as cultural venues that codify, structure and interpret spiritual experiences by providing rituals and explanatory models that are accepted within specific social and/or populational frameworks.
Problems associated with scientifically understanding and defining a complex construct such as spirituality contribute to the tendency in more recent research to operationalize spirituality as a solely psychological function, without further conceptual embellishment. Alternatively, certain types of mind–body practices, such as yoga, tai chi or qi gong, are also frequently regarded as behavioural exemplars of (or substitutes for) spirituality. In particular, a state of consciousness known as mindfulness, and the corresponding mind–body technique, mindfulness meditation, has gained considerable attention in the health sciences, both as a viable salutary practice [35] and as a ‘de-confessionalized’ and secular form of consciousness exercise, owing largely to the work of Kabat-Zinn [36]. First models for explaining how mindfulness conveys health effects have been developed [37,38]. Mindfulness may be broadly defined as the ability to focus upon the direct and immediate perception of the present moment with a state of non-judgemental awareness, thereby voluntarily suspending evaluative cognitive feedback [39]. Mindfulness was originally derived from applied Buddhist philosophical practices and has frequently been empirically associated with the development of empathy, curiosity, kindness, compassion and acceptance, and can be framed in secular contexts (as a psychological skill), as well as religious contexts (as a form of contemplative state) [40]. Although mindfulness can be trained [17], some authors have argued that it may be better to uncouple it from any given technique by defining it only in terms of the functional psychological processes involved [41].
(b). Spirituality and salutogenesis
Empirical findings have identified both spirituality and religiosity as potential health resources [7,29,42,43]. The three main mechanisms that have traditionally been proposed for conveying positive health effects are (i) healthy lifestyle and avoidance of health risk behaviours due to religious and spiritual inclination, (ii) social support and engagement owing to religious participation, and (iii) an increased sense of coherence and meaningfulness of life owing to spiritual ideation and practices.
Older research tended to explain such effects as being derived from active engagement with religion, and suggested that it is mainly social coherence that conveys observed health benefits [44,45]. However, newer conceptualizations propose that spiritual experiences (and the intrapersonal effects that are facilitated by regular spiritual, contemplative or meditative practice rather than belief sets, attitudes or behaviour alone) might be pivotal to understanding potential/putative salutogenic effects [30,46–48]. There are several arguments in favour of this hypothesis that highlight the importance of the experiential and practical dimension of spirituality for producing such health-relevant effects.
First, spiritual or mystical experiences may be regarded as a (special) subcategory of exceptional experiences that are perceived as being in some way ‘different’, ‘extraordinary’ and/or ‘superlative’ to the common sense reality of the everyday world [32,49,50]. This has been reported in most of the mystical and religious traditions, and in secular settings, as well [32,49]. With regard to the prevalence of such events in modern Western societies, spiritual experiences can be regarded as rather common events [51]. An older research study looking into frequency of spiritual experiences in a large sample of randomly selected students and adults living in Virginia, USA, found that 35 per cent of the students and 28 per cent of the adults reported to have experienced ‘a profound and deeply moving spiritual, ‘mystical’ or ‘transcendental’ experience’ at least once in their lifetime [52]. Another survey study found that 19 per cent of a sample of randomly selected inhabitants of the city of Bristol, UK reported to have experienced a ‘profound or moving religious or mystical experience’ at least once [53]. Hardy [54], analysing more than 4000 written reports of spiritual experiences, found that the following phenomenological features were commonly present: sense of certainty, enlightenment (19%), visions (18%), sense of purpose behind events (11%), contact with the dead (8%), voices (7%), exaltation, ecstasy (5%) and telepathic phenomena (4%). Yet, despite their phenomenological commonalities, such experiences remain difficult to objectify as they are frequently described as ineffable and emotionally polyvalent [32]. In sum, a hallmark feature of spiritual experiences seems to be that they are frequently perceived and/or interpreted as purposeful and meaningful, and not merely unique events.
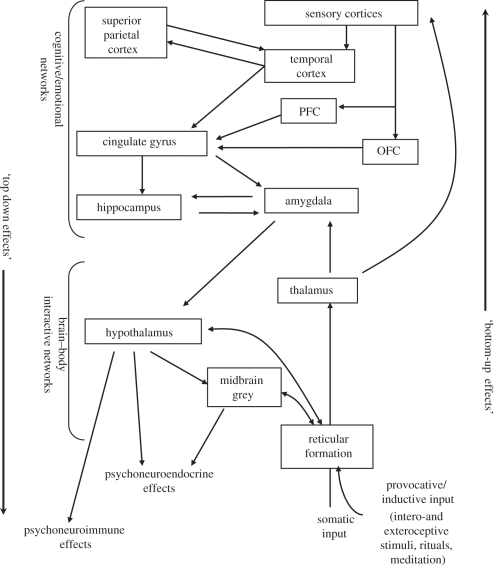
Second, although there is consensus within the philosophy and psychology of religion that spiritual experiences—like all other types of experiences—are largely dependent on social, cultural or religious context [55], it is also important to recognize these experiences as psychophysiological events that involve, and are mediated by, peripheral and central neural (and neuroendocrine and/or neuroimmunological) substrates [56,57]. In the main, it appears that spiritual practices—and experiences—engage hierarchical activation of peripheral and central neuraxes, which involve iterative complexification of signal processing, from sensory transduction/transmission to (ultimately) cognitive and emotional perceptions and ideation. As depicted in figure 1, a number of brain loci and hierarchical networks have been shown to be involved [24,58,59]. Lower tiers of the neuraxis (i.e. brainstem systems) aggregate sensory inputs from external and internal environmental events to attend to stimulus features and provide an orienting response. Ascending activation can differentially engage reticulo-thalamic pathways and may recruit intermediate-tier networks that are involved in attention, emotion and ‘directed’ consciousness (i.e. what has been regarded as ‘being conscious of’ an event, circumstance and its attendant emotional ‘valence’). Prinz [59] states that such intermediate-tier activation need not evoke attentional focus, but can instead create a basal emotional state that is then subsequently imbued with a sense of ‘intentionality’ as a process of higher order, third-tier processing. Such intermediate processing involves the amygdala, insula and regions of the associative, cingulate, temporal and parietal cortices. Stimulation of this system engages hippocampal and parahippocampal cortical neuraxes that function to conjoin working and declarative memory to emotional cognitive component(s) and frame experience to past and current circumstance(s), and can activate third-tier networks inclusive of the (left and/or right) prefrontal and orbitofrontal cortex. These third-tier networks appear to subserve, at least in part, higher order dimensions of expectational or anticipatory cognitions that (i) contribute a sense of situational objectification and/or intentionality to the experience, and/or (ii) relate/ground the experience to prior, current or potential situations and circumstances [24,25,60,61].
Figure 1.
Schematic of neural structures and networks putatively involved in spiritual experience and practices, as well as placebo responses and effect. Provocative inputs include internal and/or external sensory stimuli that are evoked by environmental effects, including specific circumstances, behaviours and/or rituals. These may incur bottom-up body–brain/mind events that activate ascending and intracerebral integrative networks. Cognitive awareness of—and emotionality related to—these effects produces distinct conscious experience(s) by engaging attentional and non-attentional mechanisms to produce ‘consciousness of’ and ‘state(s) of consciousness’, respectively, as related to particular stimuli and their environmental circumstance(s). These events are important for the induction of top-down processes that activate brain/mind–body mechanisms, inclusive of physiological responses that may mediate or induce salutogenesis. OFC, orbitofrontal cortex; PFC, prefrontal cortex. Adapted with permission from Giordano & Engebretson [24].
These mechanisms differentially engage distinct and neurochemically heterogeneous components of the neuraxis, and involve monoaminergic systems of arousal, reinforcement and reward, opioid systems subserving analgesia and pleasure, cholinergic systems of memory and other putative neurotransmitter systems (e.g. endogenous cannabinoids, nitric oxide, glutamate, gamma amino butyric acid, etc.) that modulate these effects. A complete discussion of this neurochemistry is beyond the scope of this paper, and the reader is referred to selected contributions that provide a more detailed explanation [62–64]. Yet, while certain sites and regions in the brain appear to mediate aspects of spiritual experience(s) and placebo responses, it remains important to avoid what Bennett & Hacker call the ‘mereological fallacy’, namely the error of ascribing the function of the system as a whole to its particular component parts when addressing the possible role(s) of various neural substrates and mechanisms [65]. In this case, it is not a specific brain site that mediates aspects of these experiences, but rather the differential spatial and temporal activation of neural pathways and networks. Moreover, caution is warranted when addressing putative neural substrates in reference to cognitions, emotions and behaviours; while we may discuss neural mechanisms involved in these processes, the experiences themselves are higher order phenomena of the person in whom the nervous system is embodied, and in this way reflect a functional ‘bottom-up’ and top-down complementarity that is inherent to consciousness [66,67].
Further, persons are embedded within socio-cultural environments, and as we have noted, the neuro-cognitive and emotional substrates that are activated in spiritual experience(s) reflect ‘…hierarchical levels of brain function, from acquisition of purely sense data, to the more extrapolative cognitive events of linking emotions and memories to expectation and/or contextual objectification’ [24]. The correspondence of these mechanisms with those of placebo responses [68,69] suggests (i) reciprocity of predisposition and/or effect, (ii) the role—and importance—of belief, expectation and environmental conditioning in eliciting these psychobiological events and effects (vide infra), and (iii) that spiritual experiences seem to be able to exert profound psychological and physiological effects.
These suggestions have been supported by recent studies of Benson [70], Benson & Dusek [71], Lazar et al. [16] and Stefano et al. [72]. Important to these studies—and likely to the abundant reports of spiritual and religious conversion phenomena reported in the clinical literature and throughout human history—is the finding that expectation and ‘belief’ play a strong role in the occurrence, induction and magnitude of neural response(s) and related (top-down) psychophysiological effects [13,73–75].
It is however important to note that clinical, empirical and experimental evidence have shown that the health effects associated with the experiential dimensions of spirituality are by no means unambiguously favourable, as might be—at least implicitly—assumed, but rather that such experiences should be regarded as a ‘double-edged sword’. An older review reporting the findings of 91 studies analysing the relationship between spirituality, religiosity and health found that 47 studies showed a negative relationship, 37 a positive relationship and 31 showed no clear relationship whatsoever [76]. It could be argued that this profile of effect actually reflects the relative distribution of placebo effects (and susceptibility) seen in any given population [77]. Thus, the potential for producing such bi-valent effects seems to be a distinct hallmark of both spirituality and placebo (and nocebo). Whereas the term ‘nocebo’ effect (from the Latin, ‘I will harm’) has been reserved for describing negative effects, i.e. harmful or undesired reactions stemming from inert, sham or dummy treatment [78], research on religious and spiritual coping has identified ‘anger at God or a deity’ as an important predictor for poor mental health and poor coping outcomes [79,80]. It has also been suggested that some spiritual experiences may induce severe distress [81,82], states of crisis [83], and/or abjectly negative physiological effects, and in this regard, literature addressing Voodoo rituals is particularly illustrative of the relative power of nocebo (for review, see [84,85]).
Such negativity may have contributed to prior studies characterizing spiritual experiences as either identical to or indistinguishable from psychopathological states [86–88]. However, the lexical patterns used to describe spiritual experiences are different from those experiences described by psychotic patients, individuals using hallucinogenic drugs and persons recounting negatively valent personal experiences [89]. Additionally, we have empirically shown that spiritually practising individuals evaluate negative spiritual experiences (i.e. non-pathological experiences that endanger, question or attack the integrity of the self) more positively than individuals with lack of spiritual practice, whereas no difference was found for the emotional assessment of psychopathological experiences [32,49,50]. These findings suggest that spiritual experiences—at least on a phenomenological level—are categorically distinct from psychopathological symptoms and that spiritual practitioners have better abilities to distinguish between these two categories of experience.
Additionally, practices such as meditation, different forms of contemplation, many mind–body practices and/or prayer may be regarded as any regular activity that is intended and designed to elicit spiritual experiences [90]. Spiritual or meditative practices can also be considered to be introspective training methods that lead to change in self-perception and self-reflection [91]; it can be assumed that individuals who engage in regular spiritual and meditative practice might be more capable of focusing awareness of their current inner states than those who do not perform such practices. For example, a recent study has found that individuals practising some form of mindfulness meditation seem to be able to alter their personal psychological model, so they can dissociate their self-awareness of the present from their long-term ‘self-image’ [92]. Thus, these practices may not only lead to characteristic changes in self-perception and organization leading to more resilience against distressful events threatening the integrity of self [48], but may also influence physiological variables such as immune function [17]; (vide supra, see also figure 1).
Finally, although certainly not least of all, research has shown that spiritual practices are able to alter neural processes and psychological effects of pain and analgesia. It has been posed that this effect may be driven by top-down processes that enable improved ability to cope with pain, rather than actually altering the level of pain that is experienced (i.e. ‘sensed’). Indeed, spiritually oriented individuals seem to be able to reinterpret the perception and ‘meaning’ of pain, possibly allowing them some capacity for emotional detachment [93,94]. There is also evidence to support that individuals who regularly exercise spiritual and meditative practice(s) seem to perceive distress as a temporary state rather than as a stable trait. We have recently shown that individuals who regularly participate in spiritual practice have a significantly lower six month test–retest reliability for distress than a comparable sample of individuals who do not participate in such practice(s) [95]. This suggests that spiritual activities are highly relevant for individual assessment of distress. However, it is also noteworthy to consider the possibility that spiritual experience(s) may arise as a bottom-up consequence of experiencing pain, and that in some cases certain individuals may view pain as a spiritual experience [25].
Although studies investigating the relationship between spirituality and health have been repeatedly criticized for failure to control for important confounds and lack of longitudinal research [5,45,96], there is nevertheless good reason to assume that (i) the effects of spiritual experiences and various forms of meditative or contemplative practice cannot be merely explained as consequences of interpersonal or social factors, and (ii) intrapersonal, top-down and/or bottom-up neurophysiological factors must be taken into account as well. This speaks to the fact that both spiritual/meditative practices and the placebo response are useful paradigms for further elucidating so-called mind–body (or perhaps more appropriately brain/mind–body) effects, and that these effects—and expectation and meaningfulness—are important for mediating responses to certain (physiologically and/or psychologically) stressful situations and salutogenesis.
(c). Spirituality: engaging the brain/mind–body connection through enhancement of meaningfulness
Clinical studies have identified three important components for healing and coping processes: (i) hope in the face of illness, (ii) receiving and embracing a sense of ‘loving acceptance’, and (iii) meaning and purpose in life [97]. Similarly, medical sociologist Antonovsky [98,99] has attempted to determine why and how some people are able to survive, adapt and overcome severe distress and manage to remain healthy, while others are not able to cope, and succumb to trauma, disease and/or illness. In short, the core concept of Antonovsky's theory is the ‘sense of coherence’ (SOC) that consists of three subcomponents representing ‘a global orientation that expresses the extent to which one has a pervasive, enduring though dynamic feeling of confidence that (i) the stimuli deriving from one's internal and external environments in the course of living are structured, predictable and explicable (comprehensibility); (ii) the resources are available to one to meet the demands posed by these stimuli (manageability); and (iii) these demands are challenges, worthy of investment and engagement (meaningfulness)’. According to Antonovsky, an individual may be able to develop a sense of coherence if she is able to perceive her environment as comprehensible and manageable and the life situation as meaningful.
It is interesting to compare salutogenetic theory with clinical observations associated with placebo responses. Barett et al. [100] have recently suggested that at least two encompassing psychological processes appear to be relevant for eliciting health-related placebo phenomena:
— A feeling of security and support stemming from encouragement from others; what the authors describe as ‘feeling cared for’, ‘being helped’ or ‘receiving treatment’, thereby suggesting that this process may be related to the manageability component of SOC.
— A sense of ‘empowerment’, ‘taking care of one's self’, ‘achieving health’ and even ‘self-actualization’ that may be related to the meaningfulness component of the SOC theory, and—in part—to the component of comprehensibility.
Both processes may also be understood as healing attempts that are either driven by endogenous (i.e. intrapersonal) or exogenous (i.e. interpersonal, cultural and environmental) factors. Specifically, the component of meaningfulness may incur health effects arising from ‘internal’ resource (‘i-resource’) management influencing cognition, emotion, expectancy, perception or motivation, as well as ‘external’ resource (‘e-resource’) management such as building and maintaining social relationships and engaging with significant symbols and rituals. This is reflected in the following eight simple actions that, according to Barett et al., clinicians may perform in order to facilitate placebo response: (i) speak positively about treatments (‘e’), (ii) provide encouragement (‘e’), (iii) develop trust (‘i,e’), (iv) provide reassurance (‘i,e’), (v) support relationships (‘e’), (vi) respect uniqueness (‘i’), (vii) explore values (‘i’), and (viii) create ceremony (‘i’). Thus, on a psychological level, spirituality may be regarded as a way for perceiving and enhancing meaningfulness; on a behavioural level, it may allow an individual to express meaningfulness through rituals and symbols; and on a functional level, it may engage the corresponding neurobiological networks that are involved in eliciting health effects by activation of top-down physiological, endocrinological and immunological processes.
(d). Spiritual experience as ‘experiential meaning response’?
Based upon extant evidence, we opine that it is at least plausible, if not likely, that there are similarities in the complex interplay of inter- and intrapersonal factors required for placebo responses and interpreting an exceptional experience as a distinct spiritual event. It is noteworthy to recall that spiritual experiences are frequently reported to have occurred in emotionally rich contexts such as states of crisis, suffering, and distress, and are often subjectively perceived to be catalytic to healing processes. It is thereby interesting to note that some placebo researchers have argued for interpreting the placebo phenomenon as a ‘therapeutic meaning response’ in order to better understand how brain/mind, body and culture interact in order to heal [101,102]. As Moerman & Jonas [103] have suggested, the placebo effect is defined as a ‘positive healing effect resulting from the use of any healing intervention presumed to be mediated by the effect the meaning has upon the patient’. This definition is not restricted to pharmacological interventions, but also embraces the use of any technology or technique in ‘mainstream medicine’, as well as more integrative or specifically complementary and alternative medicine (e.g. chiropractic, therapeutic touch, hypnosis, homeopathy; [104–106]). Moreover, if we extend that definition, an intervention may also be an event that has major impact on the existential outlook of an individual, for example, by interpreting a disease or distressful event as a consequence of spiritual failure or growth. This broad handling of the term therapeutic meaning response seems to be in accordance with cultural–anthropological findings demonstrating that symbolic interventions and sham treatments have been used within the context of medicine (and religion) since time immemorial for pleasing, encouraging and fortifying rather than ‘curing’ patients [106].
Therefore, we pose the question of whether an extended concept of ‘meaning response’ could also be useful for explaining why and how an experience becomes so inflated with personal value (viz. meaning) that it may be perceived and interpreted as a special spiritual event, thereby allowing and/or eliciting potential placebo or nocebo mechanisms? In other words, could we possibly refer to a spiritual event as an ‘existential meaning response’, thereby referring to well-known mechanisms proposed for, and explaining placebo responses?
(e). Psychological mechanisms conveying health-related effects of spirituality and placebo: explanations from expectancy and conditioning theory
Until now, two important models for the (neuro)psychological mechanisms of the placebo and placebo-type responses and effects have been proposed: expectancy theory and classical conditioning [107]. While expectancy theory assumes that implicit or explicit sets of expectancies can influence disease and health processes, conditioning theory suggests that placebo effects can be regarded as a type of classical (i.e. Pavlovian) or mixed classical-operant (i.e. quasi-Skinnerian) conditioning. Other studies, designed to clarify whether placebo effects are due to either expectancy or conditioning, have suggested that both processes are involved, and cannot be conceptually or mechanistically disentangled [68,107,108]. Thus, enhancement or even inflation of meaningfulness might be considered as an overarching concept or process to describe the effects of both expectancy and conditioning models, and insight into mechanisms of increasing meaningfulness may be useful to explain the health-related effects of spirituality and placebo (and nocebo).
Spirituality may be seen as a form of private outlook upon and towards life that reflects an existential epistemological framework. Personal epistemic values (inclusive of spirituality) may contribute to expectancies (such as anticipations about the nature and extent of disease/illness, treatment and/or trust in the clinician) that can influence or engage top-down networks operative in brain/mind–body response(s) that affect health and health-related dispositions. These anticipations and expectancies could be environmentally and circumstantially conditioned and behaviourally entrenched, and thus, conditioning theory may also explain some of the health-related effects of spirituality and religiosity on both individual and group/cohort levels.
3. Clinical and ethical implications
The interpersonal and situational variables that are critical to expectancy and conditioning are therefore important to consider when framing both spirituality and placebo responses and effects in the context of the clinical encounter. We have previously argued—and reiterate here—that it is imperative for clinicians to actively assess their patients' spirituality, given its potential bio-psychosocial influence upon health [24]. Simple inquiry about religious orientation is insufficient, as more comprehensive and finely grained evaluations of secular and/or religious spiritual values, practices and experiences may be warranted to obtain the richness of information necessary to enable provision of those resources that can best meet individual needs [109–111].
Furthermore, insights gained from spiritual assessment may be useful in (i) determining patients' susceptibility to placebo responses and effects, (ii) assessing patient's level of distress, particularly with regard to its time stability [95], and (iii) creating a positively valent, motivationally concordant, socially coherent (or even incoherent) and thus meaningful healing environment that empowers the patient [112] and enables or precipitates placebo responses [24,113]. However, clinicians' management of both patients' spirituality and any potential use of placebo responses mandates ethical consideration. We have advocated that while in-depth assessment of spiritual practices and values is vital, clinicians should not ‘partake in their patients' spiritually inductive practices’ in light of the deeply personal and individually unique nature of these experiences. But we have also argued that ‘acknowledgement of patients' spiritual needs, understanding the physiological basis of spiritual experience and accommodation of patients' desires for spiritual resources permit the clinician to assume an accepting stance and thereby fortify the clinician–patient relationship as a fundamental domain of healing’ [24,25]. This latter dimension (i.e. a positive clinician–patient relationship) is essential to generating and sustaining trust and to creating an environment in which (i) the patient feels safe and secure, and (ii) the clinician may evaluate whether certain beliefs or practices may exert salutory or negative influences relevant to patients' health and care [114].
A complete discussion of ethical issues that occur in, and from, the clinical use of any technique or technology that might induce placebo responses and effects is beyond the scope of this manuscript; for an overview, see [113,115]. When considering spiritual—as well as placebo—responses and effects, it is important that clinicians do not deceive their patients, but rather that they make it clear that such approaches appear to induce physiological mechanisms within the patient, which while not fully understood, seem to affect and may augment the healing process. Allowing and/or enabling patients to fully engage their spiritual practices could prove to be instrumental to this process (of course, provided that such practices do not interfere with, or divert other, well-established and necessary medical interventions). For it may be that as Smith has noted: ‘…one…continually places one's faith in premises, assumptions, and suppositions that cannot be objectively substantiated or justified without recourse to other believed-in premises, assumptions, and presuppositions. Everyone—the secularist and non-religious included—is a believing animal’ [116]. Perhaps, on some level, there is considerable capacity for such beliefs, values and meaning (e.g. as related to physiological processes, health and medicine) to facilitate and/or elicit healing processes.
4. Conclusions
In this paper, we have opined that the psychophysiological responses and putative health effects stemming from spiritual experiences and spirituality may at least partially be relevant for explaining placebo responses. We have argued that an extended placebo paradigm centred around the concept of meaningfulness, and harnessing insights gained from expectancy and conditioning theory, may be useful for explaining and interpreting these effects as related to spirituality—and particularly spiritual experiences—as an ‘existential meaning response’. The engagement of bottom-up and top-down neural (and endocrinological and immunological) mechanisms and effects in response to various internal and external stimuli may be important to generating psychophysiological events that are cognitively and emotionally perceived/regarded as situationally and existentially exceptional in manifestation and meaning. In brief, if an individual is able to construe and fortify existential value(s) of certain environmental situations, circumstances, rituals and activities, this may transform an ordinary event into a spiritual experience, thereby possibly eliciting placebo-type responses. If a clinician is able to engage such positive valuations and meanings in a therapeutic setting, the clinical encounter may be transformed into a deep healing relationship. Thus, (i) the assessment of patients' spirituality, (ii) acknowledgement and reflection of the effects of and upon pain and analgesia, as well as (iii) making use of various resources to accommodate patients' spiritual needs not only reflect our most current understanding of the physiological, psychological and socio-cultural aspects of spirituality and spiritual experiences, but may also increase the likelihood of eliciting self-healing processes that we have come to know as placebo response. However, although we believe that this information provides considerable potential for development of techniques that could be useful in—and for—modern medicine, we must also advocate caution because, at least for some patients, focusing upon spiritual dimensions may become an additional source of distress, anxiety and sorrow.
It is thereby noteworthy that the discussion about spirituality, health and their predicted value in, for and perhaps as placebo responses is not merely of theoretical interest, but is also clinically relevant, given that the majority of individuals (of both secular and religious orientation) claim to have experienced one or more spiritual events. Moreover, with religiosity being on the decline in many secularized Western societies, the importance of spirituality as a private and existential mindset should not be underestimated. We have grounded our discussion of placebo and spiritual experience(s) not to supernatural explanations, but to a progressively expanding knowledge of the brain–mind as an event of the natural world. However, this in no way impugns the notion of the transcendent, for in the light of neuroscience as a human endeavour, we must recognize that its focus is upon what many feel to be ‘the final frontier’—the substrate and basis of the self and knowledge itself—and given that this information is iterative, we must acknowledge that any such understanding remains contingent and viable for revision and interpretation. We are confident that research addressing both spirituality and placebo may benefit from reciprocal insight into causes, mechanism(s) and effects, and that spirituality may thus be established as a significantly important (physiological, psychological and cultural–anthropological) predictor of placebo (and nocebo) responses.
Acknowledgements
Niko Kohls' work is made possible through the long-standing support of the Samueli Institute, Alexandria, USA, and Niko Kohls and Sebastian Sauer are supported by the Peter-Schilffarth-Institute for Sociotechnology, Bad Tölz. James Giordano's work is supported by the Center for Neurotechnology Studies of the Potomac Institute for Policy Studies, Arlington, VA, USA, Center for Theology and Natural Sciences (CTNS; USA), Nour Foundation (USA), Office of Naval Research (USA) and the William H. and Ruth Crane Schaefer Endowment of Gallaudet University, Washington, DC, USA.
Footnotes
One contribution of 17 to a Theme Issue ‘Placebo effects in medicine: mechanisms and clinical implications’.
References
- 1.Vase L., Riley J. L., Price D. D. 2002. A comparison of placebo effects in clinical analgesic trials versus studies of placebo analgesia. Pain 99, 443–452 10.1016/S0304-3959(02)00205-1 (doi:10.1016/S0304-3959(02)00205-1) [DOI] [PubMed] [Google Scholar]
- 2.Jonas W. B., Chez R. A., Duffy B., Strand D. 2003. Investigating the impact of optimal healing environments. Altern. Ther. Health Med. 9, 36–40 [PubMed] [Google Scholar]
- 3.Jonas W. B., Chez R. A. 2004. Toward optimal healing environments in health care. J. Altern. Complement. Med. 10, 1–6 10.1089/1075553042245818 (doi:10.1089/1075553042245818) [DOI] [PubMed] [Google Scholar]
- 4.Fetzer Institute NIoAWG 1999. Multidimensional measurement of religiousness/spirituality for use in health research. A report of a national working group supported by the Fetzer institute in collaboration with the national institute on aging. Kalamazoo, MI: Fetzer Institute [Google Scholar]
- 5.Miller W. R., Thoresen C. E. 2003. Spirituality, religion, and health: an emerging field. Am. Psychol. 58, 24–35 10.1037/0003-066X.58.1.24 (doi:10.1037/0003-066X.58.1.24) [DOI] [PubMed] [Google Scholar]
- 6.Sloan R. P., Bagiella E., Powell T. 1999. Religion, spirituality and medicine. Lancet 353, 664–667 10.1016/S0140-6736(98)07376-0 (doi:10.1016/S0140-6736(98)07376-0) [DOI] [PubMed] [Google Scholar]
- 7.Koenig H., McCullough M., Larson D. (eds) 2001. Handbook of religion and health. New York, NY: Oxford University Press [Google Scholar]
- 8.Weaver A. J., Koenig H. G. 2006. Religion, spirituality, and their relevance to medicine: an update. Am. Fam. Physician 73, 1336–1337 [PubMed] [Google Scholar]
- 9.Hyland M., Whalley B., Geraghty A. 2007. Dispositional predictors of placebo responding: a motivational interpretation of flower essence and gratitude therapy. J. Psychosom. Res. 62, 331–340 10.1016/j.jpsychores.2006.10.006 (doi:10.1016/j.jpsychores.2006.10.006) [DOI] [PubMed] [Google Scholar]
- 10.Hyland M., Geraghty A., Joy O., Turner S. 2006. Spirituality predicts outcome independently of expectancy following flower essense self-treatment. J. Psychosom. Res. 60, 53–58 10.1016/j.jpsychores.2005.06.073 (doi:10.1016/j.jpsychores.2005.06.073) [DOI] [PubMed] [Google Scholar]
- 11.Azari N. P., et al. 2001. Neural correlates of religious experience. Eur. J. Neurosci. 13, 1649–1652 10.1046/j.0953-816x.2001.01527.x (doi:10.1046/j.0953-816x.2001.01527.x) [DOI] [PubMed] [Google Scholar]
- 12.Beauregard M., Paquette V. 2006. Neural correlates of a mystical experience in Carmelite nuns. Neurosci. Lett. 405, 186–190 10.1016/j.neulet.2006.06.060 (doi:10.1016/j.neulet.2006.06.060) [DOI] [PubMed] [Google Scholar]
- 13.Aquili E., Newberg A. 2002. The mystical mind. Minneapolis, MN: Fortress Press [Google Scholar]
- 14.Borg J., Andree B., Soderstrom H., Farde L. 2003. The serotonin system and spiritual experiences. Am. J. Psychiatry 160, 1965–1969 10.1176/appi.ajp.160.11.1965 (doi:10.1176/appi.ajp.160.11.1965) [DOI] [PubMed] [Google Scholar]
- 15.Nilsson K. W., Damberg M., Ohrvik J., Leppert J., Lindstrom L., Anckarsater H., Oreland L. 2007. Genes encoding for AP-2beta and the serotonin transporter are associated with the personality character spiritual acceptance. Neurosci. Lett. 411, 233–237 10.1016/j.neulet.2006.10.051 (doi:10.1016/j.neulet.2006.10.051) [DOI] [PubMed] [Google Scholar]
- 16.Lazar S., Bush G., Gollub R. L., Fricchione G. L., Khalsa G., Benson H. 2000. Functional brain mapping of the relaxation response and meditation. NeuroReport 11, 1581–1585 10.1097/00001756-200005150-00041 (doi:10.1097/00001756-200005150-00041) [DOI] [PubMed] [Google Scholar]
- 17.Davidson R. J., et al. 2003. Alterations in brain and immune function produced by mindfulness meditation. Psychosom. Med. 65, 564–570 10.1097/01.PSY.0000077505.67574.E3 (doi:10.1097/01.PSY.0000077505.67574.E3) [DOI] [PubMed] [Google Scholar]
- 18.Bouchard T. J., Jr, Lykken D. T., McGue M., Segal N. L., Tellegen A. 1990. Sources of human psychological differences: the Minnesota study of twins reared apart. Science 250, 223–228 10.1126/science.2218526 (doi:10.1126/science.2218526) [DOI] [PubMed] [Google Scholar]
- 19.Kirk K. M., Eaves L. J., Martin N. G. 1999. Self-transcendence as a measure of spirituality in a sample of older Australian twins. Twin Res. 2, 81–87 10.1375/136905299320565942 (doi:10.1375/136905299320565942) [DOI] [PubMed] [Google Scholar]
- 20.Geers A., Helfer S., Weiland P., Kosbab K. 2006. Expectations and placebo response: a laboratory investigation into the role of somatic focus. J. Behav. Med. 29, 171–178 10.1007/s10865-005-9040-5 (doi:10.1007/s10865-005-9040-5) [DOI] [PubMed] [Google Scholar]
- 21.Geers A. L., Kosbab K., Helfer S. G., Weiland P. E., Wellman J. A. 2007. Further evidence for individual differences in placebo responding: an interactionist perspective. J. Psychosom. Res. 62, 563–570 10.1016/j.jpsychores.2006.12.005 (doi:10.1016/j.jpsychores.2006.12.005) [DOI] [PubMed] [Google Scholar]
- 22.Geers A. L., Wellman J. A., Fowler S. L., Helfer S. G., France C. R. 2010. Dispositional optimism predicts placebo analgesia. J. Pain 11, 1165–1171 10.1016/j.jpain.2010.02.014 (doi:10.1016/j.jpain.2010.02.014) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Morton D. L., Watson A., El-Deredy W., Jones A. K. 2009. Reproducibility of placebo analgesia: effect of dispositional optimism. Pain 146, 194–198 10.1016/j.pain.2009.07.026 (doi:10.1016/j.pain.2009.07.026) [DOI] [PubMed] [Google Scholar]
- 24.Giordano J., Engebretson J. 2006. Neural and cognitive basis of spiritual experience: biopsychosocial and ethical implications for clinical medicine. Explore 2, 216–225 10.1016/j.explore.2006.02.002 (doi:10.1016/j.explore.2006.02.002) [DOI] [PubMed] [Google Scholar]
- 25.Giordano J., Kohls N. 2008. Spirituality, suffering, and the self. Mind Matter 6, 179–191 [Google Scholar]
- 26.Walach H. 2007. Mind–body–spirit. Mind Matter 5, 215–239 [Google Scholar]
- 27.Kohls N., Benedikter R. 2010. The origins of the modern concept of ‘neuroscience’—Wilhelm Wundt between empiricism and idealism: implications for contemporary neuroethics. In Scientific and philosophical perspectives in neuroethics. (eds Giordano J., Gordijn B.), pp. 37–65 Cambridge, UK: University Press [Google Scholar]
- 28.Colloca L., Benedetti F. 2005. Placebos and painkillers: is mind as real as matter? Nat. Rev. Neurosci. 6, 545–552 10.1038/nrn1705 (doi:10.1038/nrn1705) [DOI] [PubMed] [Google Scholar]
- 29.Seeman T. E., Dubin L. F., Seeman M. 2003. Religiosity/spirituality and health: a critical review of the evidence for biological pathways. Am. Psychol. 58, 53–63 10.1037/0003-066X.58.1.53 (doi:10.1037/0003-066X.58.1.53) [DOI] [PubMed] [Google Scholar]
- 30.George L. K., Larson D. B., Koenig H. G., McCullough M. E. 2000. Spirituality and health: what we know, what we need to know. J. Soc. Clin. Psychol. 19, 102–116 10.1521/jscp.2000.19.1.102 (doi:10.1521/jscp.2000.19.1.102) [DOI] [Google Scholar]
- 31.Thoresen C., Harris A. 2002. Spirituality and health: what's the evidence and what's needed? Ann. Behav. Med. 24, 3–13 10.1207/S15324796ABM2401_02 (doi:10.1207/S15324796ABM2401_02) [DOI] [PubMed] [Google Scholar]
- 32.Kohls N. 2004. Aussergewöhnliche Erfahrungen—Blinder Fleck der Psychologie? Eine Auseinandersetzung mit aussergewöhnlichen Erfahrungen und ihrem Zusammenhang mit geistiger Gesundheit. Münster, Germany: Lit-Verlag [Google Scholar]
- 33.Weaver A. J., Flanelly K. J., Oppenheimer J. E. 2003. Religion, spirituality, and chaplains in the biomedical literature 1965–2000. Int. J. Psychiatry Med. 33, 155–161 10.2190/B0H1-38QG-7PLG-6Q4V (doi:10.2190/B0H1-38QG-7PLG-6Q4V) [DOI] [PubMed] [Google Scholar]
- 34.Hill P. C., Pargament K. I., Hood R. W., McCullough M. E., Swyers J. P., Larson D. B., Zinnbauer B. J. 2000. Conceptualizing religion and spirituality: points of commonality, points of departure. J. Theor. Soc. Behav. 30, 51–77 10.1111/1468-5914.00119 (doi:10.1111/1468-5914.00119) [DOI] [Google Scholar]
- 35.Rubia K. 2009. The neurobiology of meditation and its clinical effectiveness in psychiatric disorders. Biol. Psychol. 82, 1–11 10.1016/j.biopsycho.2009.04.003 (doi:10.1016/j.biopsycho.2009.04.003) [DOI] [PubMed] [Google Scholar]
- 36.Kabat-Zinn J. 1994. Wherever you go, there you are. New York, NY: Hyperion Books [Google Scholar]
- 37.Kohls N., Sauer S., Walach H. 2009. Facets of mindfulness—results of an online study investigating the Freiburg mindfulness inventory. Pers. Indiv. Differ. 46, 224–230 10.1016/j.paid.2008.10.009 (doi:10.1016/j.paid.2008.10.009) [DOI] [Google Scholar]
- 38.Shapiro S. L., Carlson L. E., Astin J. A., Freedman B. 2006. Mechanisms of mindfulness. J. Clin. Psychiatry 62, 373–386 (doi:10.1002/1097-4679(198603)42:2<228::AID-JCLP2270420202>3.0.CO;2-L) [DOI] [PubMed] [Google Scholar]
- 39.Hayes S. C., Shenk C. 2004. Operationalizing mindfulness without unnecessary attachments. Clin. Psychol. Sci. Prac. 11, 249–254 10.1093/clipsy.bph079 (doi:10.1093/clipsy.bph079) [DOI] [Google Scholar]
- 40.Hayes A. M., Feldman G. 2004. Clarifying the construct of mindfulness in the context of emotion regulation and the process of change in therapy. Clin. Psychol. Sci. Prac. 11, 255–262 10.1093/clipsy.bph080 (doi:10.1093/clipsy.bph080) [DOI] [Google Scholar]
- 41.Bishop S. R., et al. 2004. Mindfulness: a proposed operational definition. Clin. Psychol. Sci. Prac. 11, 230–241 10.1093/clipsy.bph077 (doi:10.1093/clipsy.bph077) [DOI] [Google Scholar]
- 42.Larson D. B., Swyers J. P., McCullough M. E. 1998. Scientific research on spirituality and health: a consensus report. Rockville, IN: National Institute [Google Scholar]
- 43.McCullough M. E., Hoyt W. T., Larson D. B., Koenig H. G., Thoresen C. 2000. Religious involvement and mortality: a meta-analytic review. Health Psychol. 19, 211–222 10.1037//0278-6133.19.3.211 (doi:10.1037//0278-6133.19.3.211) [DOI] [PubMed] [Google Scholar]
- 44.Levin J. S., Chatters L. M., Ellison C. G., Taylor R. J. 1996. Religious involvement, health outcomes, and public health practice. Curr. Issues Public Health 2, 220–225 [Google Scholar]
- 45.Powell L. H., Shahabi L., Thoresen C. E. 2003. Religion and spirituality: linkages to physical health. Am. Psychol. 58, 36–52 10.1037/0003-066X.58.1.36 (doi:10.1037/0003-066X.58.1.36) [DOI] [PubMed] [Google Scholar]
- 46.Kohls N., Walach H., Wirtz M. 2009. The relationship between spiritual experiences, transpersonal trust, social support, sense of coherence and mental distress—a comparison of spiritually practising and non-practising samples. Mental Health Relig. Cult. 12, 1–23 10.1080/13674670802087385 (doi:10.1080/13674670802087385) [DOI] [Google Scholar]
- 47.Kohls N., Walach H. 2007. Psychological distress, experiences of ego loss and spirituality: exploring the effects of spiritual practice. Soc. Behav. Personal. 35, 1301–1316 10.2224/sbp.2007.35.10.1301 (doi:10.2224/sbp.2007.35.10.1301) [DOI] [Google Scholar]
- 48.Kohls N., Walach H., Lewith G. 2009. The impact of positive and negative spiritual experiences on distress and the moderating role of mindfulness. Arch. Psychol. Relig. 31, 1–18 10.1163/008467209X12524724282032 (doi:10.1163/008467209X12524724282032) [DOI] [Google Scholar]
- 49.Kohls N., Walach H. 2006. Exceptional experiences and spiritual practice—a new measurement approach. Spiritual. Health Int. 7, 125–150 10.1002/shi.296 (doi:10.1002/shi.296) [DOI] [Google Scholar]
- 50.Kohls N., Hack A., Walach H. 2008. Measuring the unmeasurable by ticking boxes and actually opening Pandoras box? Mixed methods research as a useful tool for thinking out of the box while investigating exceptional human experiences. Arch. Psychol. Relig. 30, 155–187 10.1163/157361208X317123 (doi:10.1163/157361208X317123) [DOI] [Google Scholar]
- 51.Hay D., Morisy A. 1978. Reports of ecstatic, paranormal, or religious experience in Great Britain and the United States—a comparison of trends. J. Sci. Stud. Relig. 17, 255–268 10.2307/1386320 (doi:10.2307/1386320) [DOI] [Google Scholar]
- 52.Palmer J. 1979. A community mail survey of psychic experiences. J. Am. Soc. Psychical Res. 73, 221–251 [Google Scholar]
- 53.Blackmore S. 1984. A postal survey of OBEs and other experiences. J. Soc. Psychical Res. 52, 225–244 [Google Scholar]
- 54.Hardy A. 1979. The spiritual nature of man: a study of contemporary religious experience. Oxford, UK: Clarendon Press [Google Scholar]
- 55.Katz S. T. 1992. Mysticism and language. New York, NY: Oxford University Press [Google Scholar]
- 56.Vaitl D., et al. 2005. Psychobiology of altered states of consciousness. Psych. Bull. 131, 98–127 10.1037/0033-2909.131.1.98 (doi:10.1037/0033-2909.131.1.98) [DOI] [PubMed] [Google Scholar]
- 57.Cahn B. R., Polich J. 2006. Meditation states and traits: EEG, ERP, and neuroimaging studies. Psychol. Bull. 132, 180–211 10.1037/0033-2909.132.2.180 (doi:10.1037/0033-2909.132.2.180) [DOI] [PubMed] [Google Scholar]
- 58.Rees G., Kreiman G., Koch C. 2002. Neural correlates of consciousness in humans. Nat. Rev. Neurosci. 3, 261–270 10.1038/nrn783 (doi:10.1038/nrn783) [DOI] [PubMed] [Google Scholar]
- 59.Prinz J. 2005. A neurofunctional theory of consciouness. In Cognition and the brain: the philosophy and neuroscience movement (eds Brook A., Akins K.), pp. 381–396 Cambridge, UK: Cambridge University Press [Google Scholar]
- 60.LeDoux J. E. 1993. Emotional memory systems in the brain. Behav. Brain Res. 58, 69–79 10.1016/0166-4328(93)90091-4 (doi:10.1016/0166-4328(93)90091-4) [DOI] [PubMed] [Google Scholar]
- 61.Eichenbaum H., Bodkin J. A. 2000. Belief and knowledge as distinct forms of memory. In Memory, brain, and belief (eds Schachter D., Scarry E.), pp. 176–207 Cambridge, MA: Harvard University Press [Google Scholar]
- 62.Austin J. H. 1999. Zen and the brain. Cambridge, MA: MIT Press [Google Scholar]
- 63.Esch T., Stefano G. B. 2004. The neurobiology of pleasure, reward processes, addiction and their health implications. Neuroendocrinol. Lett. 25, 235–251 [PubMed] [Google Scholar]
- 64.De la Fuente-Fernández R., Stoessl A. J. 2004. The biochemical bases of the placebo effect. Sci. Eng. Ethics 10, 143–150 10.1007/s11948-004-0071-z (doi:10.1007/s11948-004-0071-z) [DOI] [PubMed] [Google Scholar]
- 65.Bennett M., Hacker P. M. S. 2003. The philosophical basis of neuroscience. London, UK: Blackwell Publishing [Google Scholar]
- 66.Damasio A. 1999. The feeling of what happens: body and emotion in the making of consciousness. New York, NY: Harcourt [Google Scholar]
- 67.Giordano J. 2008. Complementarity, brain/mind, and pain. Forsch Komplementmed 15, 2–6 10.1159/000121106 (doi:10.1159/000121106) [DOI] [PubMed] [Google Scholar]
- 68.Amanzio M., Benedetti F. 1999. Neuropharmacological dissection of placebo analgesia expectation-activated opioid systems versus conditioning-activated specific subsystems. J. Neurosci. 19, 484–494 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Stewart-Williams S. 2004. The placebo puzzle: putting together the pieces. Health Psychol. 23, 198–206 10.1037/0278-6133.23.2.198 (doi:10.1037/0278-6133.23.2.198) [DOI] [PubMed] [Google Scholar]
- 70.Benson H. 1983. The relaxation response: its subjective and objective historical precedents and physiology. Trends Neurosci. 6, 281–284 10.1016/0166-2236(83)90120-0 (doi:10.1016/0166-2236(83)90120-0) [DOI] [Google Scholar]
- 71.Benson H., Dusek J. A. 1999. Self-reported health, and illness and the use of conventional and unconventional medicine and mind/body healing by Christian scientists and others. J. Nerv. Ment. Dis. 187, 539–548 10.1097/00005053-199909000-00003 (doi:10.1097/00005053-199909000-00003) [DOI] [PubMed] [Google Scholar]
- 72.Stefano G. B., Fricchione G. L., Slingsby B. T., Benson H. 2001. The placebo effect and relaxation response: neural processes and their coupling to constitutive nitric oxide. Brain Res. Rev. 35, 1–19 10.1016/S0165-0173(00)00047-3 (doi:10.1016/S0165-0173(00)00047-3) [DOI] [PubMed] [Google Scholar]
- 73.Fenwick P. 2001. The neurophysiology of religious experience. In Psychosis and spirituality: exploring the new frontier (ed. Clarke I.), pp. 15–26 London, UK: Whurr [Google Scholar]
- 74.Persinger M. A. 1983. Religious and mystical experiences as artifacts of temporal lobe function: a general hypothesis. Percept. Motor Skill 57, 1255–1262 [DOI] [PubMed] [Google Scholar]
- 75.Spiro H. 1997. Clinical reflections on the placebo phenomenon. In The placebo effect: an interdisciplinary exploration (ed. Harrington A.), pp. 37–55 Cambridge, MA: Harvard University Press [Google Scholar]
- 76.Batson C. D., Schoenrade P., Ventis W. L. 1993. Religion and the individual: a social-psychological perspective. Oxford, UK: Oxford University Press [Google Scholar]
- 77.Stahl S. 1996. Essential psychopharmacology: neuroscientific basis and clinical applications. Cambridge, UK: Cambridge University Press [Google Scholar]
- 78.Pogge R. C. 1963. The toxic placebo. Med. Times 91, 773–781 [PubMed] [Google Scholar]
- 79.Pargament K. I., Smith B. W., Koenig H. G., Perez L. 1998. Patterns of positive and negative religious coping with major life stressors. J. Sci. Stud. Relig. 37, 710–724 10.2307/1388152 (doi:10.2307/1388152) [DOI] [Google Scholar]
- 80.Pargament K. I., Zinnbauer B. J., Scott A. B., Butter E. M., Zerowin J., Stanik P. 2003. Red flags and religious coping: Identifying some religious warning signs among people in crisis. J. Clin. Psychol. 59, 1335–1348 10.1002/(SICI)1097-4679(199801)54:1%3C77::AID-JCLP9%3E3.0.CO;2-R (doi:10.1002/(SICI)1097-4679(199801)541<77::AID-JCLP9>3.0.CO;2-R) [DOI] [PubMed] [Google Scholar]
- 81.Hufford D. J. 2005. Sleep paralysis as spiritual experience. Transcult. Psychiatry 42, 11–45 10.1177/1363461505050709 (doi:10.1177/1363461505050709) [DOI] [PubMed] [Google Scholar]
- 82.Smucker C. 1996. A phenomenological description of the experience of spiritual distress. Int. J. Nurs. Terminol. Classif. 7, 81–91 10.1111/j.1744-618X.1996.tb00297.x (doi:10.1111/j.1744-618X.1996.tb00297.x) [DOI] [PubMed] [Google Scholar]
- 83.Grof S., Grof C. 1989. Spiritual emergency: when personal transformation becomes a crisis. Los Angeles, CA: Jeremy P. Tarcher [Google Scholar]
- 84.Hahn R. A. 1997. The nocebo phenomenon: scope and foundations. The Placebo effect: an interdisciplinary exploration. pp. 56–76 Cambridge, MA: Harvard University Press [Google Scholar]
- 85.Urgesi C., Aglioti S. M., Skrap M., Fabbro F. 2010. The spiritual brain: selective cortical lesions modulate human self-transcendence. Neuron 65, 309–319 10.1016/j.neuron.2010.01.026 (doi:10.1016/j.neuron.2010.01.026) [DOI] [PubMed] [Google Scholar]
- 86.Lukoff D., Lu F., Turner R. 1998. From spiritual emergency to spiritual problem: the transpersonal roots of the new DSM IV category. J. Humanist Psychol. 38, 21–50 10.1177/00221678980382003 (doi:10.1177/00221678980382003) [DOI] [Google Scholar]
- 87.Lukoff D., Lu F., Turner R. 1992. Toward a more culturally sensitive DSM-IV. Psychoreligious and psychospiritual problems. J. Nerv. Ment. Dis. 180, 673–682 10.1097/00005053-199211000-00001 (doi:10.1097/00005053-199211000-00001) [DOI] [PubMed] [Google Scholar]
- 88.Thalbourne M. A. 1991. The psychology of mystical experience. Except. Hum. Exp. 9, 168–183 [Google Scholar]
- 89.Oxman T. E., Rosenberg S. D., Schnurr P. P., Tucker G. J., Gala G. 1988. The language of altered states. J. Nerv. Ment. Dis. 176, 401–408 10.1097/00005053-198807000-00002 (doi:10.1097/00005053-198807000-00002) [DOI] [PubMed] [Google Scholar]
- 90.Meraviglia M. G. 1999. Critical analysis of spirituality and its empirical indicators—prayer and meaning in life. J. Holist. Nurs. 17, 18–33 10.1177/089801019901700103 (doi:10.1177/089801019901700103) [DOI] [PubMed] [Google Scholar]
- 91.Walsh R., Shapiro S. L. 2006. The meeting of meditative disciplines and western psychology: a mutually enriching dialogue. Am. Psychol. 61, 227–339 10.1037/0003-066X.61.3.227 (doi:10.1037/0003-066X.61.3.227) [DOI] [PubMed] [Google Scholar]
- 92.Farb N. A. S., Segal Z. V., Mayberg H., Bean J., McKeon D., Fatima Z., Anderson A. K. 2007. Attending to the present: mindfulness meditation reveals distinct neural modes of self-reference. Soc. Congn. Affect. Neurosci. 2, 313–322 10.1093/scan/nsm030 (doi:10.1093/scan/nsm030) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Keefe F. J., Affleck G., Lefebvre J., Underwood L., Caldwell D. S., Drew J., Egert J., Gibson J., Pargament K. 2001. Living with rheumatoid arthritis: the role of daily spirituality and daily religious and spiritual coping. J. Pain 2, 101–110 10.1054/jpai.2001.19296 (doi:10.1054/jpai.2001.19296) [DOI] [PubMed] [Google Scholar]
- 94.Wiech K., Farias M., Kahane G., Shackel N., Tiede W., Tracey I. 2008. An fMRI study measuring analgesia enhanced by religion as a belief system. Pain 139, 467–476 10.1016/j.pain.2008.07.030 (doi:10.1016/j.pain.2008.07.030) [DOI] [PubMed] [Google Scholar]
- 95.Kohls N., Walach H. 2008. Validating four standard scales in spiritually practicing and non-practicing samples using propensity score matching. Eur. J. Psychol. Assess. 24, 165–173 10.1027/1015-5759.14.3.165 (doi:10.1027/1015-5759.14.3.165) [DOI] [Google Scholar]
- 96.Devon B. 2005. Methodological pitfalls in the study of religiosity and spirituality. Western J. Nurs. Res. 27, 628–647 10.1177/0193945905275519 (doi:10.1177/0193945905275519) [DOI] [PubMed] [Google Scholar]
- 97.Pamela G. R. 1992. An emerging paradigm for the investigation of spirituality in nursing. Res. Nurs. Health 15, 349–357 10.1002/nur.4770150505 (doi:10.1002/nur.4770150505) [DOI] [PubMed] [Google Scholar]
- 98.Antonovsky A. 1987. Unraveling the mystery of health. How people manage stress and stay well. San Francisco, CA: Jossey-Bass [Google Scholar]
- 99.Antonovsky A. 1979. Health, stress, and coping: new perspectives on mental and physical well-being. San Francisco, CA: Jossey-Bass [Google Scholar]
- 100.Barrett B., Muller D., Rakel D., Rabago D., Marchand L., Scheder J. 2006. Placebo, meaning, and health. Perspect. Biol. Med. 49, 178–198 10.1353/pbm.2006.0019 (doi:10.1353/pbm.2006.0019) [DOI] [PubMed] [Google Scholar]
- 101.Moerman D. E., Jonas W. B. 2002. Deconstructing the placebo effect and finding the meaning response. Ann. Intern. Med. 136, 471–476 [DOI] [PubMed] [Google Scholar]
- 102.Walach H., Jonas W. B. 2004. Placebo research: the evidence base for harnessing self-healing capacities. J. Altern. Complem. Med. 10, 103–112 10.1089/acm.2004.10.S-103 (doi:10.1089/acm.2004.10.S-103) [DOI] [PubMed] [Google Scholar]
- 103.Moerman D. E., Jonas W. B. 2000. Toward a research agenda on placebo. Adv. Mind Body Med. 16, 33–46 [DOI] [PubMed] [Google Scholar]
- 104.Giordano J. 2004. Pain research: Can paradigmatic revision bridge the needs of medicine, scientific philosophy and ethics. Pain Physician 7, 459–463 [PubMed] [Google Scholar]
- 105.Giordano J., Engebretson J., Garcia M. K. 2005. Challenges to complementary and alternative medical research: focal issues influencing integration into a cancer care model. Integr. Cancer Ther. 4, 210–218 10.1177/1534735405279179 (doi:10.1177/1534735405279179) [DOI] [PubMed] [Google Scholar]
- 106.Giordano J., Jonas W. 2007. Asclepius and hygieia in dialectic: philosophical, ethical and educational foundations of an integrative medicine. Integr. Med. Insight 23, 53–60 [Google Scholar]
- 107.Stewart-Williams S., Podd J. 2004. The placebo effect: dissolving the expectancy versus conditioning debate. Psychol. Bull. 130, 324–340 10.1037/0033-2909.130.2.324 (doi:10.1037/0033-2909.130.2.324) [DOI] [PubMed] [Google Scholar]
- 108.Voudouris N. J., Peck C. L., Coleman G. 1990. The role of conditioning and verbal expectancy in the placebo response. Pain 43, 121–128 10.1016/0304-3959(90)90057-K (doi:10.1016/0304-3959(90)90057-K) [DOI] [PubMed] [Google Scholar]
- 109.Byrum C. S., Materson R. S. 2005. Assessing patient spirituality: a compelling avenue for discovery (eds Cole B. E., Boswell M. V.). Boca Raton, FL: CRC/Informa [Google Scholar]
- 110.Lee B. Y., Newberg A. B. 2005. Religion and spirituality in pain management. In Weiner's pain management: a guide for clinicians (eds Cole B. E., Boswell M. V.). Boca Raton, FL: CRC/Informa [Google Scholar]
- 111.Sulmasy D. 1997. The healer's calling: a spirituality for physicians and other health care professionals. New York, NY: Paulist Press [Google Scholar]
- 112.Pellegrino E. D. 1983. The healing relationship: architectonics of clinical medicine. In The clinical encounter: the moral fabric of the patient–physician relationship. (ed. Shelp E. E.). Boston, MA: Reidel [Google Scholar]
- 113.Giordano J., Boswell M. V. 2005. Pain, placebo, and nocebo: epistemic, ethical, and practical issues. Pain Physician 8, 331–333 [PubMed] [Google Scholar]
- 114.Giordano J. 2007. Chronic pain and spirituality. Pract. Pain Manag. 7, 64–68 [Google Scholar]
- 115.Giordano J. 2008. Placebo and placebo effects: practical considerations, ethical concerns. Am. Fam. Physician 77, 1316–1318 [PubMed] [Google Scholar]
- 116.Smith C. 2003. Moral, believing animals. New York, NY: Oxford University Press [Google Scholar]