Abstract
Control conditions were introduced through the trial of Mesmerism in Paris. Placebo controls became codified standard in 1946. Although seemingly unchallenged, there are various problems with this received view. The notion of a placebo is only defined from the negative. A positive notion proposed that placebo effects are effects owing to the meaning an intervention has for an individual. Thus, placebo effects are individualized, whereas standard research paradigms reveal only grossly averaged behaviour. Also, placebo effects are context sensitive, dependent on psychological factors such as expectancy, relief of stress and anxiety, and hence can generate strong and long-lasting treatment effects. These, however, are not predictable. Such a situation can lead to the efficacy paradox: sometimes, sham interventions can be more powerful than proved, evidence-based treatments. This situation has methodological consequences. Placebo-controlled randomized trials reveal only part of the answer, whether an intervention is effective. This is valuable information for regulators, but not necessarily also for patients and of limited value for providers. Hence, I have argued that we need to complement the hierarchical model of evidence by a circular one, in which various methods are employed on equal footing to answer different questions.
Keywords: placebo effect, double blind, efficacy, paradox
1. Introduction
It has been part and parcel of therapeutic arts since time immemorial that active pharmacological ingredients1 are only one element in the therapeutic process. The other side is provided by the psychology of the patient who has to believe that what is being done or given to him is helpful, and that the healer knows his business and is trustworthy [1]. This can be already seen in Plato's dialogue Charmides, where Socrates points out that the pharmacology is only half of the treatment, and that a spell of the soul—a psychotherapeutic or psychosomatic intervention we would say today—is just as important, if not more so:
‘when he asked me, whether I knew the remedy against headache … [I answered] it is in fact a leaf, but in addition to the remedy a certain sentence had to be said, and only if that was spoken with its application, the remedy would cure completely, without the sentence however the leaf was useless … Therefore, let no one persuade you to treat his head with this remedy who was not previously willing to present his soul to be also treated by you with your words … And you, if you are willing to present your soul according to the teachings of this foreigner to have it cured by the words and sentences of this Thracian, then I will also present the remedy for your head; else I don't know what I could do for you, my dear Charmides.’ [2, 155e3–157c7]
It is only in quite recent times that we think we can, even have to, neglect this individual psychological and psychosomatic receptive action on the part of the patient. We think that what the recipient of a therapeutic action, the patient, thinks, feels, believes, fears, expects, hates or dreads is irrelevant, by and large, to the effectiveness of our therapeutic action. At least in theory we think this is how it should be. This research paradigm follows the classic line of reasoning of pharmacology. It was born out of a long tradition which I would like to highlight in this paper. But it also makes a few crucial assumptions that are probably wrong. The research around the placebo effect demonstrates this, and, more importantly, how wrong the assumptions actually are. This research points out the most important weakness in the mainstream picture: it degrades the patient, who really is an agent, into a passive recipient of therapeutic manipulation and stipulates that the active side of the patient, his or her psychology, his or her decisions, is largely irrelevant for therapeutic success. While this might be true for acute interventions and life-saving activities of emergency medicine, it is probably wrong for most other branches of medicine, especially for functional and chronic, as well as psychological disorders. These make up an important part of the typical modern medical case load. I suggest that we neglect the agency of our patients at our peril. For one, we do not harness the important powers of self-healing that arise from our patients' psychological collaboration with a treatment. Secondly, we over- or underestimate treatment effects. We underestimate them if and when a strong non-specific component of psychological treatment effects accompanies interventions that are comparatively mild in their active ingredients, such as in complementary and alternative medical interventions. We overestimate them if pharmacological ingredients are strong but either do not work well enough in large patient groups or only at the cost of strong side effects. The placebo effect points out the cracks in our conceptual edifice of efficacy and effectiveness. The paradoxes it leads us into also suggest a way forward: to not only conceptualize efficacy as net-effect against placebo, but also as general effectiveness. This would mean seeing research methods as complementing each other in a circular fashion, rather than as hierarchically building upon each other.
This is the argument I wish to lay out in this paper. Before we can do that systematically, we need to cast a brief glance on the history of the notion and the methodological consequences.
2. History of the notion
It has been pointed out that the word ‘placebo’ is derived from the Latin Psalm phrase ‘placebo domino in regione vivorum—I will please the Lord in the land of the living’ ([3], p. 116.8). This psalm was traditionally sung at the deathbed and part of the Christian mourning rite. During the later middle ages it became customary that semi-professional wailing women were employed to sing those psalms, whence the notion of ‘placebo’ as a substitute for the real thing. During the pre-pharmacological age it was quite customary to distribute sugar pills or other pharmacologically ineffective substances to sooth the patient, to test for ‘real illness’, or to placate people, when no real effective treatment was known [4]. Following this tradition, giving ‘placebos’ came to mean giving a weaker substitute for the real treatment, knowingly deceiving a patient by providing suboptimal treatment, and finally a sham or ineffective treatment [5].
To understand the rise of the pharmacological paradigm and the history of the blinded trial it is necessary to go back to an important period in the history of therapy: the time when Franz Anton Mesmer (1734–1815) propagated his theory of animal magnetism [6]. He stipulated that all diseases arise from the misdirected flow of an etheric substance, which he called ‘animal magnetism’. This he conceived in analogue to material magnetism to be an invisible life force that is normally aligned, and in diseased people disarranged. He claimed to rearrange it by certain strokes and circulations using magnetic rods in and around the ‘field’ of magnetism that was supposed to surround a person. He quickly became the therapeutic prodigy of his age. Having settled in Paris he opened clinics, one for poor and one for rich people, in which huge barrels with magnetized water were placed. Iron rods protruded from them, and patients grasped those rods and held each other by the hands in long chains, while a chamber orchestra played music in the background. This was probably the first holistic psychosomatic treatment in modern history. Patients were cured of all sorts of diseases and Mesmer's reputation as a miraculous healer spread far and wide. He even convinced the dean of the medical faculty of the University of Paris, d'Eslon. This led to the Académie Française conducting an official trial in 1884, the first one in history where blinding was employed. Contrary to many textbook descriptions, it was not Mesmer himself who was tested, but d'Eslon volunteered as the magnetist. Using magnetic passes, he was able to induce hysterical fits in a woman, simply by passing his magnetic rod around her in a certain fashion. However, when a curtain was placed between the magnetiseur and the test person, nothing happened. The committee concluded that animal magnetism was not proved as such, but that the phenomenon was obviously owing to the rapport between the magnetiseur and his patient [7–10].
This experience laid the foundation for the insight into the power of suggestion, hypnosis and psychological rapport between therapist and patients. The whole school of French hypnotists developed out of this tradition testifying to the power of the therapeutic relationship, the strength of hypnotic suggestion and the therapeutic value of such interventions. Ultimately, Flournoy, Jung, Bleuler and Freud who laid the ground for a modern type of psychological therapy cannot be understood without this hypnotist movement [11,12]. Out of it came the insight of how powerful suggestion is, and that if one wants to see how a therapeutic component works without its psychological ramifications and contexts, it needs to be tested blind and separated from this context. The curtain of the mesmerist trial became the blind of the modern pharmacological trial. But how to effectly blind? One has to employ a decoy strategy that resembles the real one in all aspects except that which is supposed to be the active ingredient. Here, the methodological reasoning is married to the older tradition of applying placebos: only placebo substances can do that. They are interventions that carry therapeutic contexts, but no active pharmacological ingredients [7]. But by the same token, a decisive precondition is implicitly codified: that it is possible, useful, even necessary, to think of therapeutic interventions in terms of additive elements that can be taken apart and put back together at will without losing the overall picture. The additivity stipulation arises from this type of reasoning.
The first blinded pharmacological studies were conducted by homeopaths and their critics in Nuremberg 1835: volunteer doctors took homeopathic natrum muriaticum (table salt: sodium chloride) in a dilution or potency of C30 (i.e. 10−60) or unmedicated sugar globules [13]. This and other early blinded experiments of homeopathy [14] were largely inconclusive, but introduced placebo controls into medical methodology. The first blinded psychological experiment was conducted by Peirce & Jastrow in 1884 [15]. They tested the sensory discrimination threshold of volunteers estimating tiny amounts of weight differences. Blinded, placebo-controlled experiments in pharmacology were postulated and exemplified by Martini in Bonn in the 1930s [16], and finally taken into medical mainstream methodology when the first blinded trial was conducted during the Streptomycin trial on tuberculosis in 1948 [13], and finally codified in the Conferences on Therapy [17,18].
In a winding history, the insight into the power of psychological suggestion and hypnotic intervention and the therapeutic application of placebo substances with no known pharmacological value were married to a new and powerful methodology: blinded trials. It has to be borne in mind that only indistinguishable placebos make blinding possible and only blinding can make use of placebo treatment as controls. Add to this Fisher's statistical methodology that introduces randomization and appropriate statistical theory, and the modern placebo-controlled trial is born.
Out of that history we learn one important lesson: the attempt to isolate the ‘true’ component of therapy comes at the cost of tearing a therapeutic system apart and partitioning a whole into allegedly separable entities: there are psychological effects of hypnosis, suggestion, expectation, etc. These are considered in this paradigm as ‘bad guys’ who need to be controlled. The placebo is meant to do this. More importantly, this stipulates that only material, pharmacological effects are really interesting. These are the ‘good guys’ that remain if everything else is eliminated by the control procedure. It is very important to highlight at this point the artificial nature of this set-up. Apart from injecting pharmacological substances into unconscious or sleeping people, there is no actual therapeutic situation where such a set-up is really happening. Every therapeutic intervention is always an interaction between a provider and a patient. Every patient is by definition and default an agent as well. He or she comes with his whole psychological make-up, expectations, history, fears and hopes, attitudes and beliefs. To assume that these are all irrelevant and that they do not, in any real and important way, interact with pharmacological interventions is a dangerous abstraction that is borne of the artificial partitioning of the therapeutic situation within the placebo-controlled trial. There are only a few studies that have actually tested this assumption, and all of them show that it is wrong [19].
This conundrum has been prolonged by unfruitful definitions of the placebo effect until comparatively recently.
3. Notions and definitions
The most recent and least heeded definition is that by Moerman, Brody and Jonas that defines placebo effects as ‘effects due to the meaning of an intervention’ [20–22]. This definition is an important improvement on older attempts. It stipulates that
— placebo effects are in fact effects (not chimeras),
— they are due to individual factors that comprise the meaning an intervention has for a particular patient, and
— this implies, as a consequence, that they reflect the individual psychology of a patient. Thus, they are, by default, not controllable or amenable to manipulation in a paradigmatic framework asking for average effects.
It is surely possible to take the individual psychological situation of a patient into account, for instance, in a close therapeutic encounter, in psychotherapy, or by a good family physician who has known a patient for a long time. This is exactly the art of individualized therapy. However, in a research setting where average effects are studied, where a purported true effect of an intervention is the only interesting target, individual perception of the situation, individual psychology is, technically speaking, error variance that cannot be actively used, but only controlled for. This is made explicit by the definition of Moerman, Brody and Jonas. This definition brings in the semiotic perspective.
(a). The placebo as a semiotic paradigm
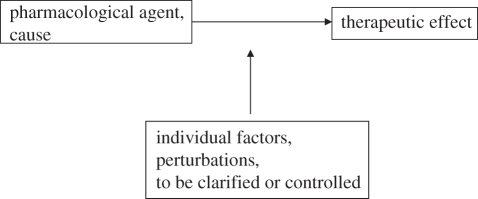
Let us digress here to really appreciate the significance of this move. Medicine has grown accustomed in the latter half of the twentieth century, and more so with the genetic and neuroscientific focus of the last decade, to understand itself purely in terms of natural science, according to the cause–effect relationships that govern these domains. Hence the pharmacological paradigm is also, basically, mechanistic: you put a pharmacological agent into the system and, provided your knowledge is complete enough, it will affect a particular change in the system, blocking or facilitating certain receptors with a comparatively predictable result. The range of the effect will be affected by some individual factors like enzymatic efficiency and clearance from the system. Hence pharmacological agents are, in principle, causal agents that are amenable to therapeutic manipulation. The relationship is, logically speaking, a bivalent relationship with some intermediate factors intervening that can be, eventually, controlled. Figure 1 illustrates this situation.
Figure 1.
Cause–effect relationship between pharmacological agent and effect. Individual factors are conceived as perturbations that need to be controlled or clarified. The relationship between cause and effect is bivalent with only two elements.
The semiotic perspective turns this image upside down. Semiotics is the science of signs, their meaning and effect. Saussure, starting from linguistics, and Charles S. Peirce, the same Peirce that conducted the first blinded experiment [15], are considered the founding fathers [23–25].
For Peirce, causal relationships of the type described in figure 1 were a special and ‘crystallized’ case of a more general paradigm of signs and signification. In other words, for Peirce signs are a more general and encompassing category that includes causes, or causes are a specific group of signs with very restricted meaning that are only valid in special cases, where the system has no degree of freedom to react otherwise, for instance, in strongly closed physical systems. In order to understand this, it is useful to consider Peirce's theory of signs briefly. A sign is something that stands for something else, namely an object that it signifies. It generates in a recipient a certain understanding or meaning. The recipient then acts according to the meaning it perceives. In the words of Peirce himself:
‘A Sign, or Representamen, is a First which stands in such a genuine triadic relation to a Second, called its Object, as to be capable of determining a Third, called its Interpretant. (2.274)’
‘A sign or representamen, is something which stands to somebody for something in some respect or capacity. It addresses somebody, … it creates in the mind of that person an equivalent sign … That sign which it creates I call the interpretant of the first sign. The sign stands for something, its object. (2.228)’. [26]
Thus, an object is not just an agent. But in nearly all, except the ‘crystallized’ cases of sheer necessity, an object is represented by a sign, which Peirce calls a ‘First’. Objects, as a rule, can become signs for recipients, because these recipients have minds and can interpret signs. Hence Peirce calls the meaning that is produced by these objects, via their sign character, an ‘interpretant’ or the ‘meaning’ of the sign that is created in the mind of the recipient.
To clarify this relationship by a few examples: a poster that I see next door to my home announcing a concert tomorrow is not a cause that causes me to go to the concert. It is a sign that stands for something else, namely the concert. It creates a meaning in my mind. If I am free, have the desire to experience some music and the music it announces suits me, I will go. If it announces some kind of music that I am not interested in, say heavy metal, I would not go, because the meaning it creates is not meaningful to me at all. But it might be meaningful to my son, who likes heavy metal and hence might go. In other words, the sign mediates the object to the recipient. The meaning I receive from a poster announcing a heavy metal concert is different from the meaning my son perceives. But even though we might have different meanings attached to the very same poster signifying the very same event, if I do not go to the concert, but my son does, the poster is not a cause. Else it would cause everybody, uniformly, to do something. It is a sign. It can only operate via the meaning it creates. If the poster is badly designed, even my son might not go to the concert, because the meaning generated is not consonant with his expectations. And even though we both might perceive the same poster, he wanting to go, me not, we might both not go because we have agreed to eat together in a restaurant the same evening. The meaning a sign creates and the propensity to act on this meaning is thus always dependent on a potentially infinite list of internal states of a recipient. Thus, signs always create meanings of an individual nature.
Now, the meaning that is created by the poster can itself become a sign for another object in me or in my son. It can represent, for instance, my desire to not go out and remind me of the fact that I have not had a quiet evening with my wife for a long time. The meaning of this situation may then be to go home and not do anything that very evening. In that sense, in a Peircean view all those triadic relationships between objects and meanings mediated by signs can be concatenated and, in principle, the whole world represented as a series of signs that stand for objects that have certain meanings for individual recipients. These meanings can again become objects, which are signs that convey certain meanings and so forth.
In such a view, semiotics not only becomes a particular analysis of signs and their meaning, but a paradigm of viewing regular relationships in the world. The important point is: there is no such thing as strict causation except in very artificial, exceptional experiences, when the meaning of a situation is so overdetermined that it can only be seen as one particular meaning. For instance, if a hitman pulls the trigger of a gun, the bullet will shoot out and hit the target, if aimed for correctly. There is no signal, there is no multiple meaning, there is just an object that has one meaning, or cause and effect. Likewise, if the hitman threatening me with a loaded gun wants my money I will give it to him, because I do not want to be shot. For me, the gun has then taken a very particular meaning, namely a threat to my life, which I have very little leeway to react on but to comply. In that sense it has become a cause that has a very specific effect: me handing over my money. However, suppose I was a very skilled martial arts fighter, and suppose that my specialty is grabbing at guns pointed at me, I would then have two options, and suddenly the very same loaded gun takes on a different meaning. I could hand over my money, because the gun means a threat to my life, as it normally does. Or I could grab it lightening quick, because I perceive its meaning as a provocation to self-defence.
Thus, signs can provoke various types of meanings, depending on the state, the history, the present well-being and the inner milieu of the recipient. All this is taken together in the Peircean term ‘meaning in the mind of a receiver’.
Now, this is pretty clear for humans who have minds. It is very interesting to note here that Peirce, and later on others, started to see that in fact this is true for most of the biological world [25,27,28].
In biology, a lot of examples can be found [29]. For instance, a hungry cat will try to catch a butterfly, and so will a young, playful one. But an old or a satiated cat will not stir even though a butterfly may fly across its very mouth. The sign character of the butterfly depends on the cat's state. Sometimes, a butterfly signifies ‘prey’, sometimes ‘play’, sometimes nothing. Likewise, a moving human being will become a signal for attack, for instance, for a bull defending a herd of cows, but a human being that stands stock still will be ignored, as he or she is not a sign for the bull at all (except, of course, if the bull has been alerted otherwise). The whole of the natural sciences could be reformulated as a semiotic discipline, and the movement of bio-semiotics is trying to achieve just that [30].
Thure von Uexküll [31–35] has frequently pointed out that the only way of really making sense of medical treatment is a biosemiotic approach. This means bringing the Peircean perspective to medicine. In such an approach, diseases become signs for complex processes of disturbance in an organism that have a certain meaning that needs to be understood by the physician. Likewise, medical interventions are not causes that are applied to a machinery, the body, with a certain effect to be produced. Rather, they are complex signs that stand for complex objects—the causal part of medical interventions, the caring environment, the social agreement to help the sick, the historical tradition that led to a well-functioning healthcare system, the scientific paradigm that has fostered certain interventions, and so forth. And they create complex meanings in patients. The decisive thing now is that the meaning that is created is highly individual. It surely, most of the time, contains some causal element, for instance, the pharmacological property of an agent. But on top of this, there is a wide range of meanings attached to it that are created in the mind of the recipient, the patient. If, for instance, the patient has had bad experiences with injections, an injection will trigger different meanings than if previous experiences were good. If the patient holds the opinion that interventions will likely be more effective the more painful and invasive they are, then injections will surely be better than pills.
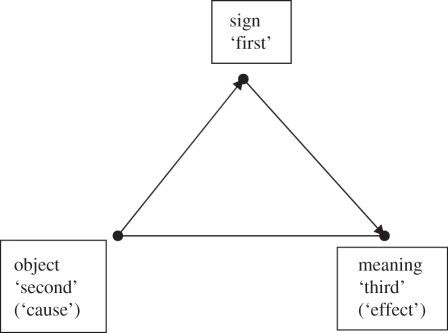
Thus, the individual meaning of a medical intervention is dependent on culture, historical background and individual history. In the context of medical treatment, there is always some objective component to every treatment. This is the causal, physical side. But there is also a strong individual component, be this individual physiological-enzymatic efficiency or individual psychology. At any rate, the semiotic perspective denotes that medical interventions are not causes, but signs for active organisms. Such organisms interact with their environment and are not just automatons that react to causes. The placebo effect is the phenomenological indication of this, and the semiotic reconstruction reintroduces agency into the medical theoretical enterprise. Meaning is, after all, quite an individual thing, and what for one patient may signify rescue from catastrophe may be a sure sign of doom for the next. Only a recipient that generates meaning also has the potential freedom2 to act in different ways. The semiotic analysis of the placebo effect points to this freedom to act in various ways. This is schematically depicted in figure 2.
Figure 2.
Triadic semiotic relationship. What is a dyadic relationship between cause and effect in the mechanistic model becomes a triadic relationship. The cause–effect relationship is mediated by the meaning that the intervention has as a sign.
The placebo effect is exactly the epistemological and theoretical junction where the insufficiency of the mechanistic model for understanding therapeutic phenomena becomes obvious. Any intervention has a certain individual meaning attached to it, as long as patients are conscious and psychologically active, i.e. as long as they are agents. And this meaning component can interact with the physiological-objective properties of an intervention in various ways: it can enhance the action, it can block it, or it may even act in a way that potentially beneficial interventions become laden with negative effects, in which case we speak of nocebo-effects, negative placebo effects [36]. This is also the reason why the study of placebo effects is not only of peripheral interest, but also of foundational-paradigmatic importance for medical theory building.
(b). Other notions
This also explains why previously held notions are not really useful. They define placebo effects either in tautological terms (‘Placebo effects are non-specific effects produced by placebos’) [3,37], or in terms of a causal-theoretical framework as ‘incidental effects’, i.e. effects that are not really intended by an intervention [38,39]. While the latter approach has some merits, it means that whenever a theory changes, all effects that had been placebo effects previously suddenly become ‘real’ later on, or depending on what is intended and how some intervention is viewed, something might be a placebo sometimes or real on other occasions. Other attempts, also starting from an implicitly causal modelling, denote placebo effects as effects that occur owing to a non-active intervention [40].
It seems to me that only the semiotic definition can solve the puzzle: placebo effects are real physiological effects. But they are not caused by a physical intervention but arise from the intrinsic meaning-making of an active organism that interacts with the environment. The placebo effect actually reinvests patients with their original dignity as agents. Every other notional attempt has led to a definitorial conundrum. Using a mechanistic paradigm in pharmacological testing works quite well on average. But here we also see paradoxes and problems arise that point to a common denominator. Patients are agents. Because this is so, therapeutic components are not simply additive. Depending on the context, non-specific effects—the shorthand notion I use here to denote effects that are seen as a consequence of placebo procedures—may be more important than specific ones and even outmarch them. This can be illustrated by what I have called the efficacy paradox.
4. The efficacy paradox
The Efficacy Paradox was introduced a while ago as a thought experiment to illustrate the potential importance of such non-specific effects [41,42]. It is illustrated in figure 3. Suppose we have two different placebo-controlled trials in the same condition. Suppose treatment x has a difficulty showing superiority over its placebo in an adequately powered trial. We would then say treatment x is not efficacious, because it failed to show superiority over placebo. Suppose treatment y has actually shown superiority over its placebo and was significantly better than placebo y. We would then call treatment y efficacious. Now it could happen that the overall effect of treatment x is larger than that of treatment y. Hence, a non-efficacious treatment could be more effective than an efficacious one. This is, because the non-specific component, i.e. the placebo effect, might vary between trials. It might even be the case that placebo x produces effects larger than real treatment y. In this situation, we have a real paradox: an efficacious, evidence-based treatment might be less effective than a ‘placebo’. It is normally assumed that placebo effects are comparatively stable across trials and document a kind of generic background noise. I think we need to conceptualize these effects as more dynamic. They reflect the meaning response, and this might be quite different, dependent on the meaning an intervention creates, for individual patients or depending on particular contexts and circumstances.
Figure 3.
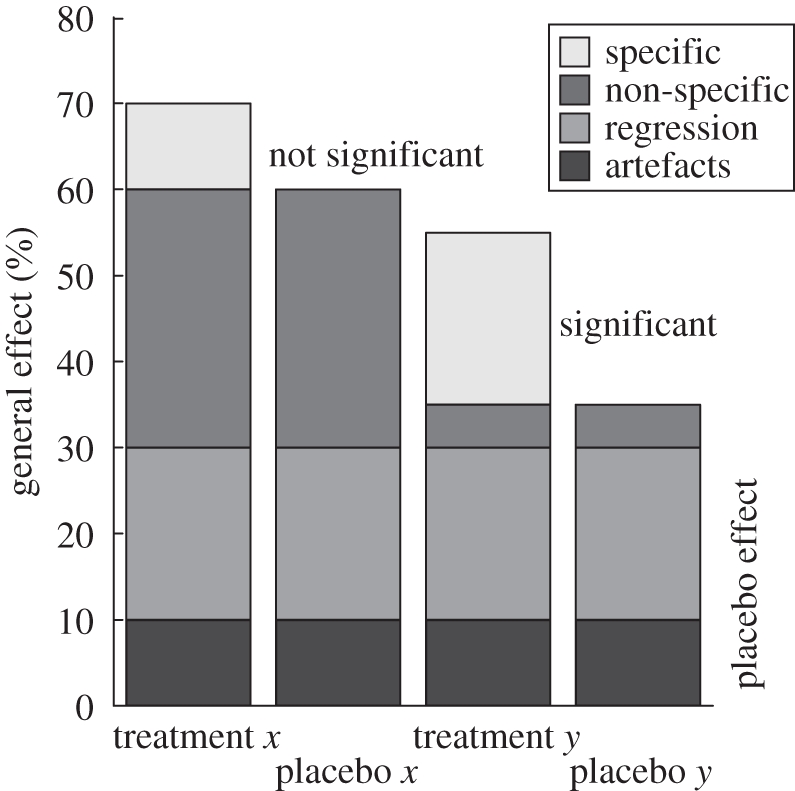
The Efficacy Paradox. A trial might prove one intervention (treatment y) as efficacious, because it is superior to a placebo control, yet this efficacious treatment might be ineffective compared with another treatment (treatment x), which is indistinguishable from its own placebo (placebo x), because the non-specific effects in treatment x are larger.
At the time I thought about this paradox it was purely hypothetical. Meanwhile, the three large German acupuncture trials have yielded empirical evidence that this paradox can actually be real, and they pose major epistemological challenges to interpretation. All of them tested acupuncture against sham acupuncture and the best-evidence conventional standard that was supposed to be superior and well covered by clinical trial evidence. This active comparator was not just ‘treatment as usual’ but the best that conventional medicine could muster at the time, according to German guidelines, designed and expected to be clearly superior to placebo and at least as effective as real acupuncture. The three trials were identical in design and covered migraine prophylaxis, osteoarthritis and chronic low back pain. Acupuncture was semi-individualized. Sham acupuncture was flat needling of non-acupuncture points that had been agreed upon as inactive by a panel of experts. Two of the trials [43,44] showed that acupuncture and sham acupuncture are indistinguishable, but both were clinically nearly twice as effective—with statistical significance, of course—as conventional medicine. The third trial [45] showed that all three arms were roughly equal. A recent US study confirmed these results in low back pain, only that here as sham, the authors used tooth picks that were just put on the skin, i.e. without penetration, and the active comparator was not the best-available conventional therapy but ‘usual care’ [46]. Also, here all the acupuncture arms, including the sham, were indistinguishable from each other but all were clinically and statistically superior to usual care.
These results obviously mean that what has been depicted in the Efficacy Paradox can, at times, become true. What does this mean for treatment? Clearly, if we were to stick blindly to the pharmacological paradigm, we would have to claim that sham acupuncture is better than some of the best of clinically tested, evidence-based interventions in these diagnoses. Intuitively, nobody does that, since we recognize that in certain situations special interventions, such as acupuncture, carry meanings that may outweigh the meaning-cum-pharmacology of other treatments for certain types of patients. But this clearly shows that meaning can be more important than material causation or pharmacology.
(a). Why does the paradox arise? What does this mean for methodology?
The paradox arises, because we make two unwarranted assumptions. We assume that the placebo control controls for background noise that is comparatively uniform across patient groups and interventions, at least for certain types of disease categories. The contrary is true: it is highly variable and it can, at times, be larger than specific effects. It is highly dependent on context. For instance, the same intervention, paracetamol, was twice as effective when tested against another active ingredient than when tested against placebo [47–49]. Naproxen given as a mere bedside medication to alleviate pain in cancer patients was only half as effective than when given to the same type of patients within the context of a clinical trial, and it was less effective than the respective placebo of the controlled trial [50]. One of the first trials of second-generation serotonin agonists to treat acute migraine pain was unable to show an effect over and above placebo [51]. Why? Because it was also compared with sumatriptan, the first generation serotonin agonist that had already been shown to be effective, and because the placebo group was much smaller than the two active comparator groups. Hence, patients knew that their likelihood to receive placebo was only 1 : 16, and they were expecting active treatment more often than not. In a meta-analysis it was shown that the higher the likelihood of receiving active treatment in unbalanced designs the larger the placebo effect in trials [52]. These are only a few striking examples how context modifies the otherwise known efficacy of an active pharmacological ingredient. This demonstrates that those context effects of meaning are more than just a nasty by-product. They are central because they can be just as big as the effects produced by the pharmacological or therapeutic agents themselves.
The paradox arises because we normally see efficacy only in terms of differences between active and control condition. For patients, however, the important measure is the absolute effect they can get from any intervention. They do not care whether the intervention is carried by a strong pharmacological agent or by a weak intervention such as homoeopathy or acupuncture. They are only interested in the overall effect. This can sometimes be strong despite the fact that controlled trials have shown no or only marginally important specific effects, exactly because the meaning that is carried by an intervention can do the therapy just as well as the active ingredients in other types of interventions. This is strikingly exemplified by homoeopathic therapy of chronic headaches. In controlled trials, it was very difficult to show any specific effect of homoeopathy at all over placebo [53–55]. In a careful epidemiological observational study, effects of the very same intervention are massive, nearly 2.5 standard deviation difference after two years compared with initial status [56]. To negate these effects by saying they are ‘only’ placebo does not really do justice to patients' reality. One would have to say that these effects are obviously effects owing to the meaning the treatment has for those patients who chose that intervention.
(b). Methodological consequences: the circular model
Methodologically speaking this situation points to an important consequence: evidence-based medicine (EBM) obviously cannot only be built on placebo-controlled trial evidence and the effect sizes meta-analytically derived from such trials. Why not? Because these trials neglect, by design and default, all individual meaning. They are only asking about the pharmacological or causally specific net effect an intervention has. This is valuable information, but it is not the only information that is interesting for patients, purchasers and providers.
EBM cannot even be built on randomized trials only, although, theoretically speaking, such trials give unbiased estimates of effect sizes vis-à-vis other active treatments. Why not? All randomized studies, by default, have to exclude the agency of the patient, since only those patients can be randomized that consent to being allocated and hence that consent to giving up the choice of what should be their treatment. In other words, randomized studies can only be done, by design and default, on a subgroup of patients, namely those who do not really care what their treatment should be or who are willing to delegate the decision about their treatment to a physician or a computer system. Thus, knowledge coming from such trials, worthwhile though it might be, can only be applied to this particular group of patients. In cases where new treatments are being introduced this might be an option. But whenever treatments have come to be imbued by meaning, studying an intervention through patients that do not care which one they might get strips the meaning off treatments. Many complex interventions, whether they are traditional treatments or modern surgical procedures, are laden with meaning, and to strip this meaning can mean reducing these interventions to mere shadows. Would this mean they are ineffective? Probably not. They are only ineffective from a certain perspective.
Thus, study designs are implicitly linked to certain perspectives. These perspectives express typical questions, and these questions are again typical examples of certain interests and speak to particular stakeholders.
This is where different interests come into play. Purchasers may wish for cheap interventions that do not create a lot of follow-up costs. Patients want their problems gone, no matter how, and they do not want a lot of other problems to follow from the interventions. Academicians are interested in the specific effects and mechanisms. And regulators insist on specific effects being demonstrated should a new intervention be reimbursed by public money. Health technology assessment (HTA) agencies want to see that the therapeutic effects come at reasonable costs and that the effect sizes produced are worth the public money. Thus, every perspective demands different viewpoints. And each viewpoint is in fact the call for a different methodology. What patients want can be answered by well conducted large epidemiological cohort studies over a long period of time. They can show us what the chances of durable improvement for a certain type of patient under a certain treatment are and what the costs and side effects are involved. What academicians want to know has to be answered in experimental models, in vitro or in vivo. The outcomes of such studies are largely irrelevant for patients or regulators. What regulators want normally demands placebo-controlled trials. What HTA requires is often a mix of studies and very often randomized comparisons against best evidence active interventions. Thus, these different perspectives, and the different importance the meaning response has for certain stakeholder groups, points to the fact that one simple methodological model would not do. Rather, the different methodologies have to complement each other in order to represent the whole.
This is, why we have proposed a circular model of methodology instead of a hierarchical one [57]. Such a circular model acknowledges the fact that each methodology has strengths and weaknesses, and that no method has the answer to all questions that are important. While a hierarchical approach, stipulating that only randomized trial evidence and the meta-analytic compression of evidence-derived thereof is good evidence, the circular approach argues for even handedness. What is good evidence depends on the question. And what type of evidence informs us about effectiveness depends on the perspective taken.
If we want to have the knowledge to answer a patient's question on whether an intervention will have a high likelihood of relieving him or her from suffering at comparatively low cost and with little side effects, it is evidence from large cohort studies that we need. These studies, however, would not be able to tell us whether this intervention is likely to be better than an established standard or some other intervention. It will be comparative studies that are necessary for that. Randomized comparison trials will tell us whether interventions differ, but only for patients that are indifferent as to which treatment they are being offered. As soon as preference comes into play comparisons will need to be conducted with groups of patients that choose their treatments. And so forth. In that sense, the meaning effect and its importance points us to the multi farious nature of evidence. There is no simple answer to the question: is an intervention effective? The answer is: it depends. It will depend on the circumstances, on the context, on the choice of the patient and on the meaning which the intervention has for a certain type of patient. Hence we will have to acknowledge, as a consequence of the importance of the meaning response, that only a mix of research methods tackling the question from different perspectives and complementing each other in a circular fashion will be able to give us the full picture.
The metaphor of a circle transports the meaning that methods and outcomes are of equal value. The importance does not lie in an intrinsic marker, such as research design, but in the fit with a certain question and a certain perspective. The fact that a majority of researchers and regulators still opt for the outcomes of randomized, ideally placebo-controlled trials, is a sign that the importance of the individual meaning of an intervention has not really been universally adopted. Research around the placebo effect, however, has been highlighting exactly the importance of individual meaning of interventions. It is not a logically consistent option to take into consideration the findings from placebo research and not think carefully about the concepts of efficacy, effectiveness and research methodology.
5. Concluding remarks
The placebo effect, or meaning response, thus points us to the lacunae of our knowledge. It makes obvious where our modern mechanistic pharmacological paradigm fails. It fails where it neglects the meaning that an intervention has for an agent. Individual meaning is probably relevant for most therapeutic situations in medicine, because medicine deals with humans, and humans have experiences, have histories and are meaning makers. The meaning response teaches us to think of patients in terms of agents and of interventions in terms of complex actions that have certain types of meanings that are not necessarily amenable to manipulation and that are not necessarily uniform across patients. The meaning response, as a consequence, teaches us that our notions of efficacy and the methodology to demonstrate and pinpoint efficacy are insufficient. Thus, the very method that used placebos to get rid of the placebo effect has produced the insight that we cannot get rid of it, except we change the method and the notion. And if we do that we do not get rid of the placebo effect, we see it as the most important and most powerful ally of the doctor in the quest for cure: the meaning response that encapsulates the power of patients to heal themselves.
Acknowledgements
My work on placebo effects has profited immensely from discussions I had over the years with Wayne Jonas, who also supported me and my group financially through funds from the Samueli Institute. Currently my position is supported by Heel Pharmaceuticals Baden-Baden, Germany. This does not constitute a conflict of interest, as this company believes in the specificity of their products.
Endnotes
An active therapeutic ingredient could be anything that influences pathological processes, such as an acupuncture needle, a surgical intervention, a physiotherapeutic or chiropractic handling, etc.
The term ‘freedom’ here does of course not refer to conscious choices, for some of those reactions will be automated and unconscious. Nevertheless, semiotics points to the many degrees of freedom a system has to react to signs. And in that sense ‘freedom’ has to be seen as an array of options a system chooses from to react.
One contribution of 17 to a Theme Issue ‘Placebo effects in medicine: mechanisms and clinical implications’.
References
- 1.Frank J. D. 1961. Persuasion and healing: a comparative study of psychotherapy. Baltimore, MD: Johns Hopkins University Press [Google Scholar]
- 2.Plato 1964. Plato with an english translation by W.R.M. Lamb. London, UK: Heinemann; The Loeb Classical Library. (Plato I: Charmides, Alcibiades I & II, etc.) [Google Scholar]
- 3.Shapiro A. K., Morris L. A. 1978. The placebo effect in medicine and psychological therapies. In Handbook of psychotherapy and behavior change: an empirical analysis (eds Garfield S. L., Bergin A.), pp. 369–410 2nd edn. New York, NY: Wiley [Google Scholar]
- 4.de Craen A. J. M., Kaptchuk T. J., Tijssen J. G. P., Kleijnen J. 1999. Placebos and placebo effects in medicine: historical overview. J .R. Soc. Med. 92, 511–515 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kaptchuk T. J. 1998. Powerful placebo: the dark side of the randomised controlled trial. Lancet 351, 1722–1725 10.1136/bmj.39524.439618.25 (doi:10.1136/bmj.39524.439618.25) [DOI] [PubMed] [Google Scholar]
- 6.Florey E. 1995. Ars Magnetica. Franz Anton Mesmer 1734–1815: Magier vom Bodensee. Konstanz: Universitätsverlag Konstanz [Google Scholar]
- 7.Kaptchuk T. J. 1998. Intentional ignorance: a history of blind assessment and placebo controls in medicine. Bull. Hist. Med. 72, 389–433 10.1353/bhm.1998.0159 (doi:10.1353/bhm.1998.0159) [DOI] [PubMed] [Google Scholar]
- 8.Miller J. 1997. Going unconscious. In Hidden histories of science (ed. Silver R. B.), pp. 1–35 London, UK: Granta Books [Google Scholar]
- 9.Crabtree A. 1993. From Mesmer to Freud: magnetic sleep and the roots of psychological healing. New Haven, CT: Yale University Press [Google Scholar]
- 10.Bailly J. S., Academic des Sciences (France) 1784. Rapport des Commissaires chargés par le Roi de l'examen du Magnétisme Animal. Paris, Italy: Imprimerie Royale [Google Scholar]
- 11.Ellenberger H. F. 1970. The discovery of the unconscious. The history and evolution of dynamic psychiatry. New York, NY: Basic Books [Google Scholar]
- 12.Shamdasani S. 2003. Jung and the making of modern psychology: the dream of a science. Cambridge, UK: Cambridge University Press [Google Scholar]
- 13.Stolberg M. 1996. Die Homöopathie auf dem Prüfstein. Der erste Doppelblindversuch der Medizingeschichte im Jahr 1835. Munchn. Med. Wochen 138, 364–366 [Google Scholar]
- 14.Kaptchuk T. J. 1997. Early use of blind assessment in a homoeopathic scientific experiment. Br. Homoeopath. J. 86, 49–50 10.1016/S0007-0785(97)80036-1 (doi:10.1016/S0007-0785(97)80036-1) [DOI] [Google Scholar]
- 15.Peirce C. S., Jastrow J. 1884. On small differences of sensation. Messages Natl Acad. Sci. 3, 73–83 [Google Scholar]
- 16.Martini P. 1932. Methodenlehre der therapeutischen Untersuchung. Berlin, Germany: Springer [Google Scholar]
- 17.Therapy C. 1954. How to evaluate a new drug. Am. J. Med. 17, 722–727 10.1016/0002-9343(54)90031-5 (doi:10.1016/0002-9343(54)90031-5) [DOI] [PubMed] [Google Scholar]
- 18.Therapy C. 1946. The use of placebos in therapy. New York J. Med. 46, 1718–1727 [PubMed] [Google Scholar]
- 19.Kleijnen J., de Craen A. J. M., Van Everdingen J., Krol L. 1994. Placebo effect in double-blind clinical trials: a review of interactions with medications. Lancet 344, 1347–1349 10.1016/S0140-6736(94)90699-8 (doi:10.1016/S0140-6736(94)90699-8) [DOI] [PubMed] [Google Scholar]
- 20.Brody H., Moerman D. E. 1996. Symbolic and meaningful dimensions of the placebo effect. In Placebo and Nocebo Effects: Developing a Research Agenda Conf., 2–4 December Bethesda, MD: NIH [Google Scholar]
- 21.Moerman D. E., Jonas W. B. 2002. Deconstructing the placebo effect and finding the meaning response. Ann. Intern. Med. 136, 471–476 [DOI] [PubMed] [Google Scholar]
- 22.Moerman D. E., et al. 1996. Placebo effects and research in alternative and conventional medicine. Chin J. Integr. Trad. West Med. 2, 141–148 10.1007/BF02969672 (doi:10.1007/BF02969672) [DOI] [Google Scholar]
- 23.Hulswit M. 2000. A Semeiotic account of causation. The ‘Cement of the Universe’ from a Peircean Perspective. PhD Thesis, Katholieke Universiteit Nijmegen, Nijmegen, The Netherlands
- 24.Peirce C. S. 1992. The essential writings. Selected philosophical writings. Vol 1: 1867–1893; Vol 2: 1893–1913. Bloomington, IN: Indiana University Press [Google Scholar]
- 25.Sebeok T. A. 1986. The doctrine of signs. J. Soc. Biol. Struct. 9, 345–352 10.1016/S0140-1750(86)90203-4 (doi:10.1016/S0140-1750(86)90203-4) [DOI] [Google Scholar]
- 26.Peirce C. S. 1931. Collected papers, vol. 1–6; vol. 7–8 (eds Hartshorne C., Weiss P., Burks A.). Cambridge, MA: Harvard University Press [Google Scholar]
- 27.Sebeok T. A. 1972. Perspect zoosemiotics. The Hague: Mouton [Google Scholar]
- 28.Yates F. E. 1991. Pharmacosemiotics: where is the message in the drug? In Semiotic perspectives on clinical theory and practice medicine, neuropsychiatry and psychoanalysis (eds Litowitz B. E., Epstein P. S.), pp. 65–79 Berlin, Germany: Mouton de Gruyter [Google Scholar]
- 29.Uexküll J. V., Kriszat G. 1970. Streifzüge durch die Umwelt von Tieren und Menschen. Bedeutungslehre. Stuttgart, Germany: Fischer [Google Scholar]
- 30.Hoffmeyer J. 1996. Für eine semiotisch reformulierte Naturwissenschaft. Z. Semiotik. 1, 31–34 [Google Scholar]
- 31.von Uexküll T. 1982. Semiotics and medicine. Semiotica 38, 205–215 10.1515/semi.1982.38.3-4.205 (doi:10.1515/semi.1982.38.3-4.205) [DOI] [Google Scholar]
- 32.von Uexküll T. 1986. Commentaries on ‘The doctrine of signs’ by Thomas Sebeok. J. Soc. Biol. Struct. 9, 353–354 10.1016/S0140-1750(86)90216-2 (doi:10.1016/S0140-1750(86)90216-2) [DOI] [Google Scholar]
- 33.von Uexküll T. 1989. Naturwissenschaft als Zeichenlehre. Merkur-Deut Z Eur D 43, 225–234 [Google Scholar]
- 34.von Uexküll T. 1995. Biosemiotic research and not further molecular analysis is necessary to describe pathways between cells, personalities, and social systems. Adv. J. Mind Body Health 11, 24–27 [Google Scholar]
- 35.von Uexküll T., Wesiack W. 1988. Theorie der Humanmedizin. Grundlagen ärztlichen Denkens und Handelns. München, Germany: Urban & Schwarzenberg [Google Scholar]
- 36.Hahn R. A. 1997. The nocebo phenomenon: scope and foundations. In The placebo effect: an interdisciplinary exploration (ed. Harrington A.), pp. 56–76 Cambridge, MA: Harvard University Press [Google Scholar]
- 37.Borkovec T. D. 1985. Placebo: defining the unknown. In Placebo (eds White L., Tursky B.), pp. 59–67 New York, NY: Guilford Press [Google Scholar]
- 38.Grünbaum A. 1981. The placebo concept. Behav. Res. Ther. 19, 157–167 10.1016/0005-7967(81)90040-1 (doi:10.1016/0005-7967(81)90040-1) [DOI] [PubMed] [Google Scholar]
- 39.Grünbaum A. 1989. The placebo concept in medicine and psychiatry. In Non-Specific aspects of treatment (eds Shepherd M., Sartorius N.), pp. 7–38 Toronto: Huber [Google Scholar]
- 40.Kienle G. S., Kiene H. 1997. The powerful placebo effect: fact or fiction? J. Clin. Epidemiol. 50, 1311–1318 10.1016/S0895-4356(97)00203-5 (doi:10.1016/S0895-4356(97)00203-5) [DOI] [PubMed] [Google Scholar]
- 41.Walach H. 2001. Das Wirksamkeitsparadox in der Komplementärmedizin. Forsch. Komp. Klas. Nat. 8, 193–195 10.1159/000057221 (doi:10.1159/000057221) [DOI] [PubMed] [Google Scholar]
- 42.Walach H. 2001. The efficacy paradox in randomized controlled trials of CAM and elsewhere: beware of the placebo trap. J. Altern. Complem. Med. 7, 213–218 10.1089/107555301300328070 (doi:10.1089/107555301300328070) [DOI] [PubMed] [Google Scholar]
- 43.Haake M., Muller H. H., Schade-Brittinger C., Basler H. D., Schafer H., Maier C., Endres H. G., Trampisch H. J., Molsberger A. 2007. German Acupuncture Trials (GERAC) for chronic low back pain: randomized, multicenter, blinded, parallel-group trial with 3 groups. Arch. Intern. Med. 167, 1892–1898 10.1001/archinte.167.17.1892 (doi:10.1001/archinte.167.17.1892) [DOI] [PubMed] [Google Scholar]
- 44.Scharf H.-P., Mansmann U., Streitberger K., Witte S., Krämer J., Maier C., Trampisch H. J., Victor N. 2006. Acupuncture and knee osteoarthritis. Ann. Intern. Med. 145, 12–20 [DOI] [PubMed] [Google Scholar]
- 45.Diener H. C., et al. 2006. Efficacy of acupuncture for the prophylaxis of migraine: a multicentre randomised controlled clinical trial. Lancet Neurol. 5, 310–316 10.1016/S1474-4422(06)70382-9 (doi:10.1016/S1474-4422(06)70382-9) [DOI] [PubMed] [Google Scholar]
- 46.Cherkin D. C., et al. 2009. A randomized trial comparing acupuncture, simulated acupuncture, and usual care for chronic low back pain. Arch. Intern. Med. 169, 858–866 10.1001/archinternmed.2009.65 (doi:10.1001/archinternmed.2009.65) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Skovlund E. 1991. Should we tell trials patients that they might receive placebo? Lancet 337, 1041. 10.1016/0140-6736(91)92701-3 (doi:10.1016/0140-6736(91)92701-3) [DOI] [PubMed] [Google Scholar]
- 48.Skovlund E., Fyllingen G., Landre H., Nesheim B.-I. 1991. Comparison of postpartum pain treatments using a sequential trial design I: paracetamol versus placebo. Eur. J. Clin. Pharmacol. 40, 343–347 10.1007/BF00265841 (doi:10.1007/BF00265841) [DOI] [PubMed] [Google Scholar]
- 49.Skovlund E., Fyllingen G., Landre H., Nesheim B.-I. 1991. Comparison of postpartum pain treatments using a sequential trial design II: naproxen versus paracetamol. Eur. J. Clin. Pharmacol. 40, 539–542 10.1007/BF00279965 (doi:10.1007/BF00279965) [DOI] [PubMed] [Google Scholar]
- 50.Bergmann J.-F., Chassany O., Gandiol J., Deblos P., Kanis J. A., Segrestaa J. M., Caulin C., Dahan R. 1994. A randomised clinical trial of the effect of informed consent on the analgesic activity of placebo and naproxen in cancer patients. Clin. Trial Meta-Anal. 29, 41–47 [PubMed] [Google Scholar]
- 51.Diener H. C., Klein K. B. Group MOCaSCS. 1996. The first comparison of the efficacy and safety of 311C90 and sumatriptan in the treatment of migraine. In 3rd European Headache Conf., 5–8 June Italy: S Margherita di Pula [Google Scholar]
- 52.Diener H.-C., Dowson A. J., Ferrari M., Nappi G., Tfelt-Hansen P. 1999. Unbalanced randomization influences placebo response: scientific versus ethical issues around the use of placebo in migraine trials. Cephalalgia 19, 699–700 10.1046/j.1468-2982.1999.019008699.x (doi:10.1046/j.1468-2982.1999.019008699.x) [DOI] [PubMed] [Google Scholar]
- 53.Whitmarsh T. E., Coleston-Shields D. M., Steiner T. J. 1997. Double-blind randomized placeo-controlled study of homoeopathic prophylaxis of migraine. Cephalalgia 17, 600–604 10.1046/j.1468-2982.1997.1705600.x (doi:10.1046/j.1468-2982.1997.1705600.x) [DOI] [PubMed] [Google Scholar]
- 54.Walach H., Gaus W., Haeusler W., Lowes T., Mussbach D., Schamell U., Springer W., Stritzl W., Haag G. 1997. Classical homoeopathic treatment of chronic headaches. A double-blind, randomized, placebo-controlled study. Cephalalgia 17, 119–126 10.1046/j.1468-2982.2000.00129.x (doi:10.1046/j.1468-2982.2000.00129.x) [DOI] [PubMed] [Google Scholar]
- 55.Straumsheim P., Borchgrevink C., Mowinkel P., Kierulf H., Hafslund O. 2000. Homoepathic treatment of migraine: a double blind, placebo controlled trial of 68 patients. Br. Homoeopath. J. 89, 4–7 10.1054/homp.1999.0332 (doi:10.1054/homp.1999.0332) [DOI] [PubMed] [Google Scholar]
- 56.Witt C. M., Lüdtke R., Willich S. N. 2009. Homeopathic treatment of chronic headache (ICD-9: 784.0)—a prospective observational study with 2 year follow-up. Forsch Komplementmed 16, 227–235 10.1159/000226770 (doi:10.1159/000226770) [DOI] [PubMed] [Google Scholar]
- 57.Walach H., Falkenberg T., Fonnebo V., Lewith G., Jonas W. 2006. Circular instead of hierarchical—methodological principles for the evaluation of complex interventions. BMC Med. Res. Method 6, 29. 10.1186/1471-2288-6-29 (doi:10.1186/1471-2288-6-29) [DOI] [PMC free article] [PubMed] [Google Scholar]