Abstract
Background:
Open discectomy remains the standard method for treatment of lumbar disc herniation, but can traumatize spinal structure and leaves symptomatic epidural scarring in more than 10% of cases. The usual transforaminal approach may be associated with difficulty reaching the epidural space due to anatomical peculiarities at the L5–S1 level. The endoscopic interlaminar approach can provide a direct pathway for decompression of disc herniation at the L5–S1 level. This study aimed to evaluate the clinical results of endoscopic interlaminar lumbar discectomy at the L5–S1 level and compare the technique feasibility, safety, and efficacy under local and general anesthesia (LA and GA, respectively).
Methods:
One hundred twenty-three patients with L5–S1 disc herniation underwent endoscopic interlaminar lumbar discectomy from October 2006 to June 2009 by two spine surgeons using different anesthesia preferences in two medical centers. Visual analog scale (VAS) scores for back pain and leg pain and Oswestry Disability Index (ODI) sores were recorded preoperatively, and at 3, 6, and 12 months postoperatively. Results were compared to evaluate the technique feasibility, safety, and efficacy under LA and GA.
Results:
VAS scores for back pain and leg pain and ODI revealed statistically significant improvement when they were compared with preoperative values. Mean hospital stay was statistically shorter in the LA group. Complications included one case of dural tear with rootlet injury and three cases of recurrence within 1 month who subsequently required open surgery or endoscopic interlaminar lumbar discectomy. There were no medical or infectious complications in either group.
Conclusion:
Disc herniation at the L5–S1 level can be adequately treated endoscopically with an interlaminar approach. GA and LA are both effective for this procedure. However, LA is better than GA in our opinion.
Keywords: General anesthesia, interlaminar approach, local anesthesia, lumbar disc herniation, percutaneous endoscopic discectomy
INTRODUCTION
Open discectomy is still a standard procedure for treating lumbar disc herniation and has provided good results. Nonetheless, one operative consequence is epidural scarring, which may not be apparent on magnetic resonance imaging (MRI) but becomes clinically symptomatic in more than 10% of cases.[3,10,18] Additionally, the occurrence of operation induced destabilization due to the necessary resection of spinal canal structures may result in post-discotomy syndrome.[12,16,18] In the past decades, many new surgical techniques have been developed to reduce tissue damage and its consequences. Endoscopes have been used since the early 1980s to inspect the intervertebral space after completion of open discectomy. The endoscopic transforaminal procedure with posterolateral access evolved from this technique. Endoscopic assisted interlaminar procedures were reported in the literature in the late 1990s.[6,28,33] Lateral access of transforaminal endoscopic surgery to optimize the route to the spinal canal under continuous visualization has been performed since the late 1990s.[29] Currently, the most widely used percutaneous endoscopic procedure in patients with lumbar disease is transforaminal surgery via the posterolateral approach; however, difficulty in achieving adequate resection of herniated discs within the spinal canal can occur.[15,19,20,34,37,39] The lateral approach can provide better access to the spinal canal under direct and continuous visualization. The transforaminal approach to L5–S1 is difficult in some cases because of anatomical constraints. A large L5 transverse process, large facet joints, a narrowed disc space, and neuroforamen with a high iliac crest all limit operative access to the L5–S1 disc space.[22,27]
In such situations, an interlaminar endoscopic discectomy has been used to overcome the anatomic limitations at the L5–S1 level, and it can be performed under local anesthesia (LA) or general anesthesia (GA). We present the technique and evaluate its feasibility, safety, and efficacy in patients undergoing GA or LA.
Key points
This is the first report to compare clinical results, technique feasibility, safety, and efficacy of endoscopic interlaminar discectomy at L5–S1 under LA and GA.
The endoscopic interlaminar operation provides an alternative route to overcome the anatomical peculiarities of the L5–S1 level that hinder the transforaminal operation.
The endoscopic interlaminar approach to L5–S1 disc herniation can achieve satisfactory clinical results with LA or GA.
Under GA, the joystick principle, medial and lateral as well as cranial and caudal mobility within the spinal canal, could be easily applied to search and remove the protruding disc by controlling optics and the bipolar system.
The most important contribution of using LA to the endoscopic interlaminar operation is that the surgeon can receive continuous feedback from the patient to prevent neural damage and help to monitor clinical improvement during surgery.
Mini abstract
The interlaminar endoscopic discectomy procedure can overcome the osseous limitations of the transforaminal approach at the L5–S1 level and it can be performed under LA or GA.
MATERIALS AND METHODS
There were 123 patients enrolled in this prospective study, who had received endoscopic excision of lumbar disc herniation at the L5–S1 level via an interlaminar approach between October 2006 and June 2009 in two medical centers in middle Taiwan. All the patients were followed up for at least more than 12 months after surgery. Eighty-three were men and 40 were women. The average patient age was 39 years (range, 18–61 years). All the patients suffered from symptomatic leg pain, and underwent plain X-ray and MRI examinations. The duration of leg pain ranged from 2 days to 13 months (mean, 61 days). Thirty patients with severe pain symptoms were operated on immediately, and 93 had received conservative treatment for at least for 6 weeks prior to surgery. All disc herniations occurred at the L5–S1 level with unilateral symptoms and correlated with image findings. GA was administrated by an anesthesiologist to 50 patients in one medical center where the operations were performed by an orthopedic surgeon, and LA was used for the other 73 patients in another medical center where the operations were done by a neurosurgeon.
Follow-up examinations were performed at 3, 6, and 12 months postoperatively. In addition to the general parameters, visual analog scale (VAS) scores for back pain and leg pain and the Oswestry Disability Index (ODI) scores were recorded preoperatively and at follow-up visits. The descriptive analysis of group characteristics was performed with SPSS version 15.0 for Windows (SPSS, Chicago, IL, USA). The independent two-sample t-test was applied to compare the clinical results of interlaminar endoscopic lumbar discectomy employed between LA and GA. Statistical significance was assumed when P < 0.05.
Inclusion criteria
Patients were included if they met the following criteria: 1) unilateral radiating leg pain that was more predominant than back pain; 2) MRI investigation revealed a single level of posterolateral disc herniation at L5–S1 and correlated with the clinical findings; and 3) no previous surgery at the same level of the lumbar spine.
Exclusion criteria
Patients with the following criteria were excluded: 1) recurrent disc herniation at the same level; 2) severe narrowing of the interlaminar distance <6 mm; 3) central or lateral stenosis of the lumbar spine; and 4) craniocaudal sequestering disc beyond half the adjacent vertebral body .
Operative technique
Surgery was performed with the patient prone on a radiolucent table under LA or GA. The choice of anesthesia depended on the preference of the neurosurgeon or orthopedic surgeon performing the operation. The skin incision was made as close to medial in the craniocaudal middle of the interlaminar window as possible. A dilator, 7.0 mm in outer diameter, was bluntly inserted to the lateral edge of the interlaminar window. Then, an operative sheath with an 8.0 mm outer diameter and beveled opening was directed toward the ligamentum flavum [Figure 1]. The rest of the procedure was performed under direct visual control and constant irrigation. A lateral incision window of approximately 4–6 mm was made in the ligamentum flavum. The neural structures and epidural fat tissue were exposed [Figure 2]. The operating sheath with beveled opening can be turned and used as a nerve hook. The joystick principle, medial and lateral as well as cranial and caudal mobility within the spinal canal, could be used to search for and remove the protruding disc by the controlling optics and bipolar system.
Figure 1.
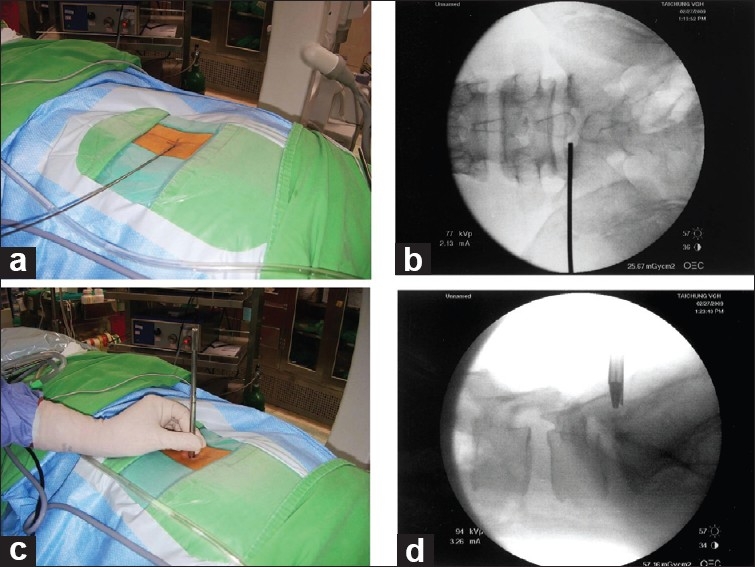
Intraoperative image showing the placement of the guide pin in the interlaminar window in anteroposterior view (a, b) and blunt insertion of the dilator with the beveled working sheath to the ligamentum flavum (c, d)
Figure 2.
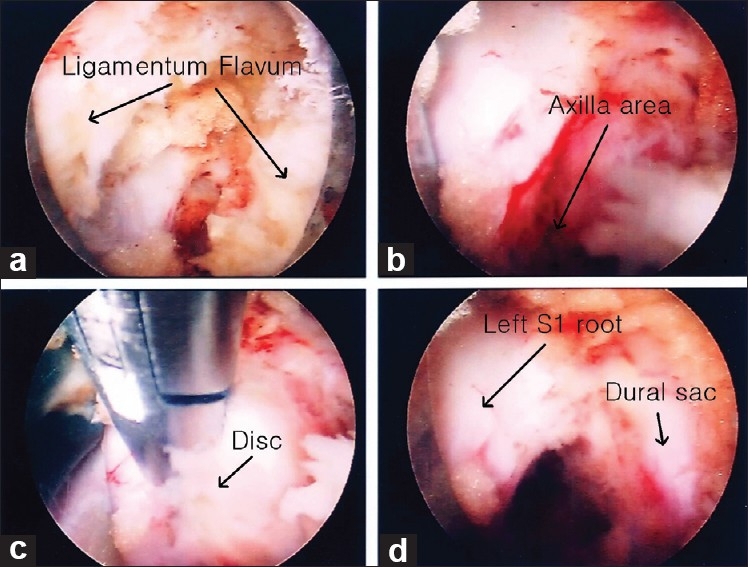
Intraoperative endoscopic view showing the following: (a) opening the ligamentum flavum, (b) exposure of the left axilla area, (c) extruded disc material in the axilla, and (d) dural sac with left S1 root and axilla after decompression
All the operating instruments and endoscopic system were supplied by Richard and Wolf (Knittlingen, Germany). The high-resolution endoscope has a diameter of 8 mm with a 4.1 mm intra-endoscopic working channel. The angle of vision is 25°. The working sheath has an 8.0 mm outer diameter and a beveled opening, both of which enable the creation of visual and working fields in an area without a clear, anatomically preformed cavity. In addition, a high-voltage bipolar probe (Ellman Innovations, New York, USA) was used.
RESULTS
Clinical outcome
A total of 123 patients were operated on between October 2006 and June 2009 for lumbar disc herniation at the L5–S1 level via the interlaminar approach. Seventy-three patients at one medical center received LA and were operated on by a single neurosurgeon, and 50 patients at another medical center received GA and were operated on by a single orthopedic surgeon. There were no statistically significant differences in patient demographics between the LA and GA groups [Table 1]. All the patients were followed up for more than 12 months. Two patients in the LA group and two in the GA group had recurrent disc herniation (recurrent rate, 3.2%) within 1 month after surgery. Three patients were treated with an open procedure and one was treated with endoscopic interlaminar lumbar discectomy again. One patient in the GA group was converted to open discectomy due to tear of the dural sac and rootlet injury. All the patients in the LA group tolerated the procedure well, though some patients felt varying degrees of discomfort during the procedure.
Table 1.
Demographic and preoperative clinical features of 123 patients
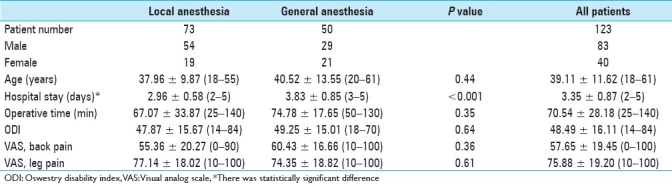
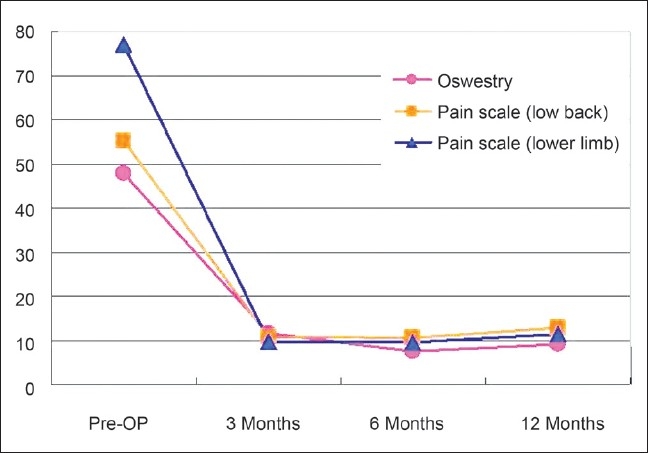
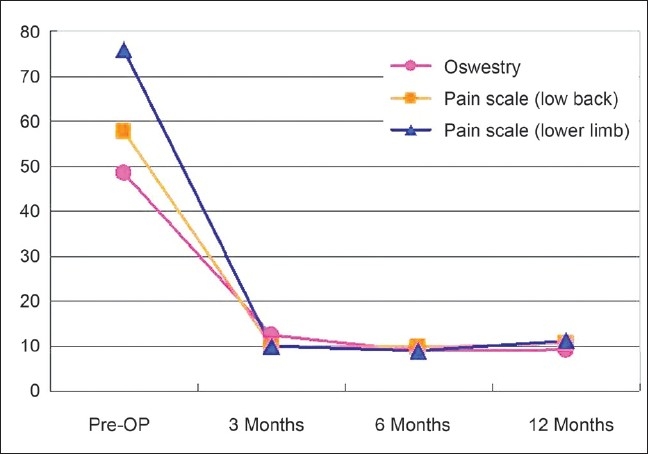
Overall, the recurrence rate was 4% in the GA group and 2.7% in the LA group. The failure rate was 2% in the GA group with none in the LA group. The success rate of surgery was 94% in the GA group and 97.3% in the LA group. The mean preoperative VAS score for back pain was 57.65 (range, 0-100) and for leg pain was 75.88 (range, 10–100), and the mean preoperative ODI was 48.49 (range, 14–84). At 12 months after surgery, the mean VAS for back pain was 10.54 (range, 0–20), the mean VAS for leg pain was 11.11 (range, 0–30), and mean ODI was 9.13 (range, 0–22) [Figures 3–5]. There was constant and significant improvement in back pain, leg pain, and daily activities in both the groups after surgery (P < 0.05). There were no statistically significant differences in VAS or ODI scores between the LA and GA groups. The mean operative time in the LA group was 67.07 min (range, 25–140), and in the GA group was 74.78 min (range, 50–130), but this difference was not statistically significant. The mean hospital stay in the LA group was 2.96 days (range, 2–5), which was significantly shorter (P < 0.05) than 3.83 days (range, 3–5) in the GA group.
Figure 3.
Mean values of visual analog scale scores for back pain, leg pain, and Oswestry Disability Index results in the local anesthesia group
Figure 5.
Mean values of visual analog scale scores for back pain, leg pain, and Oswestry Disability Index in all patients
Figure 4.
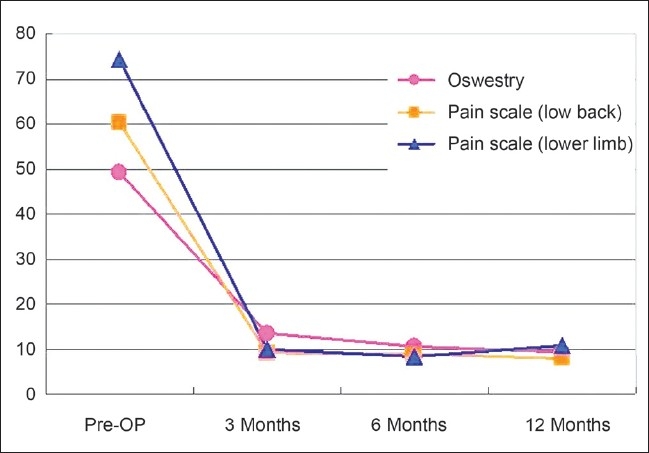
Mean values of visual analog scale scores for back pain, leg pain, and Oswestry Disability Index results in the general anesthesia group
Perioperative complications
No resection of spinal bony structure was required in either group. In the GA group, a case of dural injury and damage to the nerve root occurred when the surgeon was removing the disc with disc forceps. Only mild numbness and hypoesthesia in the distal leg and lateral foot were noted. There was no need to repair the dura and the patient's leg pain improved. Transient postoperative dysesthesia occurred in 22 patients (12 in the GA group, 10 in the LA group). There was no uncontrolled epidural bleeding, wound infections, or associated medical complications in either group.
DISCUSSION
Success rates for conventional open discectomy for lumbar disc herniation range from 75 to 100%.[2,13,23,38] The outcomes of lumbar discectomy do not seem to be affected by the introduction of the microscope and depend on patient selection rather than surgical technique.[21] From the point of avoidance or reduction of traumatic injury to spinal canal structures, endoscopic surgery may be an option for treating lumbar disc herniation. A patient's preoperative functioning is attained to a high extent and rehabilitative programs are not needed after surgery.[7] Additionally, there is no surgery related deterioration of existing symptoms in the epidural and intra-disc procedure.[28] Associated medical diseases do not increase the morbidity.
Yeung and Tsou[39] have improved the percutaneous transforaminal endoscopic technique by using the principles of targeted fragmentectomy under LA with the introduction of high-resolution working channel endoscopes, lasers, and RF bipolar flexible probes. The technique is now more versatile after improvements have been made in the endoscopic system and surgical technique. There are several anatomical peculiarities at the L5–S1 level that hinder the transforaminal approach to the L5–S1 disc space, including facet joints overlapping the disc space cephalocaudally and laterally. The transverse process at the L5 level is larger than in the upper lumbar spine. Ebraheim et al.[9] have found that the intertransverse space was the narrowest at the L5–S1 level (average, 13.4 mm ± 4.1 mm), compared with an average of 24 mm ± 3 mm at all the other lumbar intertransverse spaces in cadaveric dissection. All the above-described anatomical peculiarities with high iliac wing hinder transforaminal access to the L5–S1 disc space. Although many different techniques have evolved to overcome these problems,[1,17,25] it is still difficult to access the migrated disc and centrally located disc herniation.
Ebraheim et al.[8] found the interlaminar distance to be the greatest at L5–S1 level and the width of the interlaminar space was also a maximum of 31 mm (range, 21–40 mm). In the coronal plane, the L5 lamina is not directed vertically as the upper lumbar lamina, and it has a backward and downward angulation. This anatomical peculiarity helps to access the interlaminar space of the spinal canal at the L5–S1 level if the trajectory of the endoscope is 5°–10° in the craniocaudal direction. The spinal canal at the L5–S1 level contains the thecal sac with only the sacral roots, and the proportion of free space at the L5–S1 level is also greater. The S1 root exits at the L5–S1 disc space with an average 22° (range, 18°–26°) of take-off angle, and it is possible to access the herniation in the axilla of the S1 root within this angle.[5,11] In cases of a posterolateral herniated L5–S1 disc, the nerve root is displaced and this creates more space for entry because of the mass effect. Irrespective of the location in the shoulder or axilla areas, the mass effect of a herniated disc always has the same displaced vector to the nerve root.
The ligamentum flavum forms a tented recess with the apex in the midline and just inferior to the inferior edge of the cephalic lamina. The depth of this recess up to the dura measures 3–4 mm and is usually occupied by epidural fat.[24] This depth may be partly obliterated in cases of a disc prolapsed in the canal. This recess forms the working space for the entry of the endoscopic in an interlaminar lumbar discectomy. Peridural fibrosis is the direct consequence of intrusion into the spinal canal with a break of this effective barrier.[4] The epidural fat, which acts as a lubricant, is largely preserved. Postoperative MRI revealed no scar in the access area and only slight scarring in the spinal canal. The revision procedures, unlike those following conventional procedures, were no more difficult and did not require a longer operative time.[4,36]
In cases with a large annular defect, the posterior third of the intra-disc nucleus should be cleaned to prevent recurrence. Because of the difference in level between the interlaminar window and the intervetebral disc space, resection of the intra-discal nucleus is frequently limited.[14,35] This might explain the shorter time period of recurrent disc herniation. The new endoscope with its 4.1 mm working channel and corresponding instruments has largely overcome the technical problems associated with previous devices.[30,31,32] The following advantages are gained from this surgical technique and endoscopic system: 1) good illumination and expanded field of vision with 25° optics; 2) cost effectiveness due to shorter hospital stay and reduced anatomical trauma; 3) reduced bleeding; 4) facilitation of revision surgery; 5) no need for postoperative rehabilitation; and 6) a high degree of patient satisfaction. The disadvantages of this technique are the steep learning curve and the expense of the equipment.
The clinical results of this prospective study are comparable to those obtained with conventional procedures. Although a case of injury to the dura and nerve root occurred in GA group, we have not shown a definite difference in outcomes for VAS and ODI scores between LA and GA . Both the anesthetic techniques applied in endoscopic interlaminar lumbar discectomy at L5–S1 level achieved good outcomes and high patient satisfaction, but LA was associated with significantly shorter hospital stay. The patients in the LA group usually felt discomfort in the low back and leg during intraoperative manipulation of the dural sac and nerve root, but they tolerated the procedure well under mild conscious sedation with pethidine (25–50 mg intramuscularly) and fentanyl (1–2 ml intravenously) . To prevent over irritation of dural sac and nerve root, we sometimes kept the working sheath out of the incision window of ligamentum flavum and extracted the protruding disc with disc forceps. Fewer transient postoperative dysesthesia occurred in the LA group (13.7%) than in the GA group (24%). The most important contribution of using LA is that we can get continuous feedback from the patient to prevent excessive neural manipulation or damage and help to monitor clinical improvement during the operation.
We compared performing the surgery with LA and GA because of the different problems that would potentially be encountered during surgery. The avoidance of intraoperative nerve injury might be easier due to intraoperative feedback from patients under LA, but it is relatively difficult to use the working sheath as a nerve hook and the joystick principle to search for and remove the protruding disc due to patient's feeling discomfort. However, the technique can be mastered by an experienced surgeon. In contrast, GA affords freedom from discomfort, and allows manipulation of the instruments and retraction of the dural sac and nerve root in the spinal canal, but does not allow patient's feedback. The majority of protruded disc was through the axilla area in the LA group and it was usually approached via the shoulder area in the GA group.
We conclude that endoscopic interlaminar discectomy at the L5–S1 level is an effective operation, regardless of which method of anesthesia is used. Both the anesthetic methods achieved good outcomes and high patient satisfaction. LA is associated with significantly shorter hospital stay and fewer transient postoperative dysesthesia due to continuous patient's feedback and helps to monitor clinical improvement during surgery. In our opinion, the LA is preferred than the GA in percutaneous endoscopic lumbar discectomysurgery.
Footnotes
Available FREE in open access from: http://www.surgicalneurologyint.com/text.asp?2011/2/1/93/82570
Contributor Information
Hsien-Te Chen, Email: bonekid@ms25.hinet.net.
Chun-Hao Tsai, Email: ritsai@giga.net.tw.
Shao-Ching Chao, Email: yanwawa@yahoo.com.tw.
Ting-Hsien Kao, Email: thkao@vhgtc.gov.tw.
Yen-Jen Chen, Email: yenjenc.tw@yahoo.com.tw.
Horng-Chaung Hsu, Email: hsud4749@yahoo.com.tw.
Chiung-Chyi Shen, Email: ccshen@vghtc.gov.tw.
Hsi-Kai Tsou, Email: tsouhsikai@gmail.com.
REFERENCES
- 1.Ahn Y, Lee SH, Park WM, Lee HY. Posterolateral percutaneous endoscopic lumbar foraminotomy for L5–S1 foraminal or lateral exit zone stenosis. Technical note. J Neurosurg. 2003;99(Suppl 3):320–3. doi: 10.3171/spi.2003.99.3.0320. [DOI] [PubMed] [Google Scholar]
- 2.Andrew DW, Lavyne MH. Retrospective analysis of microsurgical and standard lumbar discectomy. Spine (Phila Pa 1976) 1990;15:329–35. doi: 10.1097/00007632-199004000-00015. [DOI] [PubMed] [Google Scholar]
- 3.Annertz M, Jönsson B, Strömqvist B, Holtås S. No relationship between epidural fibrosis and sciatica in the lumbar postdiscectomy syndrome.A study with contrast-enhanced magnetic resonance imaging in symptomatic patients. Spine (Phila Pa 1976) 1995;20:449–53. doi: 10.1097/00007632-199502001-00007. [DOI] [PubMed] [Google Scholar]
- 4.Choi G, Lee SH, Raiturker PP, Lee S, Chae YS. Percutaneous endoscopic interlaminar discectomy for intracanalicular disc herniations at L5-S1 using a rigid working channel endoscope. Neurosurgery. 2006;58(Suppl 1):ONS59–68. doi: 10.1227/01.neu.0000192713.95921.4a. [DOI] [PubMed] [Google Scholar]
- 5.Cohen MS, Wall EJ, Brown RA, Rydevik B, Garfin SR. 1990 AcroMed Award in basic science.Cauda equina anatomy. II: Extrathecal nerve roots and dorsal root ganglia. Spine (Phila Pa 1976) 1990;15:1248–51. [PubMed] [Google Scholar]
- 6.Destanddau J. A special device for endoscopic surgery of lumbar disc herniation. Neurol Res. 1999;21:39–42. doi: 10.1080/01616412.1999.11740889. [DOI] [PubMed] [Google Scholar]
- 7.Donceel P, Du Bois M. Fitness for work after lumbar disc herniation: A retrospective study. Eur Spine J. 1998;7:29–35. doi: 10.1007/s005860050023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ebraheim NA, Miller RM, Xu R, Yeasting RA. The location of the intervertebral lumbar disc on the posterior aspect of the spine. Surg Neurol. 1997;48:232–6. doi: 10.1016/s0090-3019(96)00176-0. [DOI] [PubMed] [Google Scholar]
- 9.Ebraheim NA, Xu R, Huntoon M, Yeasting RA. Location of the extraforaminal lumbar nerve roots.An Anatomic study. Clin Orthop Relat Res. 1997;340:230–5. doi: 10.1097/00003086-199707000-00030. [DOI] [PubMed] [Google Scholar]
- 10.Fritsch EW, Heisel J, Rupp S. The failed back surgery syndrome: Reasons, intraoperative findings and long term results: A report of 182 operative treatments. Spine (Phila Pa 1976) 1996;21:626–33. doi: 10.1097/00007632-199603010-00017. [DOI] [PubMed] [Google Scholar]
- 11.Hasegawa T, Mikawa Y, Watanabe R, An HS. Morphometric analysis of the lumbosacral nerve roots and dorsal root ganglia by magnetic resonance imaging. Spine (Phila Pa 1976) 1996;21:1005–9. doi: 10.1097/00007632-199605010-00001. [DOI] [PubMed] [Google Scholar]
- 12.Hedtmann A. The so-called post-discotomy syndrome - failure to intervertebral disc surgery? Z Orthop Ihre Grenzgeb. 1992;130:456–66. doi: 10.1055/s-2008-1039653. [DOI] [PubMed] [Google Scholar]
- 13.Hermantin FU, Peters T, Quartarato LA. A prospective, randomized study comparing the results of open discectomy with those of video-assisted arthroscopic microdiscectomy. J Bone Joint Surg. 1999;81:958–65. doi: 10.2106/00004623-199907000-00008. [DOI] [PubMed] [Google Scholar]
- 14.Hirabayashi S, Kumano K, Ogawa Y, Aota Y, Maehiro S. Microdiscectomy and second operation for lumbar disc herniation. Spine (Phila Pa 1976) 1993;18:2206–11. doi: 10.1097/00007632-199311000-00010. [DOI] [PubMed] [Google Scholar]
- 15.Kambin P, Zhou L. History and current status of percutaneous arthroscopic disc surgery. Spine (Phila Pa 1976) 1996;21:57–61. doi: 10.1097/00007632-199612151-00006. [DOI] [PubMed] [Google Scholar]
- 16.Kim SS, Michelsen CB. Revision surgery for failed back surgery syndrome. Spine (Phila Pa 1976) 1992;17:957–60.5. doi: 10.1097/00007632-199208000-00015. [DOI] [PubMed] [Google Scholar]
- 17.Knight MT. An x-ray jig to facilitate the percutaneous posterolateral approach to the lumbar spine. In: Gerber BE, Knight M, Siebert WE, editors. Lasers in Musculoskeletal System. Berlin Germany: Springer-Verlag; 2001. pp. 277–82. [Google Scholar]
- 18.Krämer J. Stuttgart: Thieme; 1990. Intervertebral Disk Diseases. [Google Scholar]
- 19.Lew SM, Mehalic TF, Fagone KL. Transforaminal percutaneous endoscopic discectomy in the treatment of far-lateral and foraminal lumbar disc herniations. J Neurosurg. 2001;94(Suppl 2):216–20. doi: 10.3171/spi.2001.94.2.0216. [DOI] [PubMed] [Google Scholar]
- 20.Mayer HM, Brock M. Percutaneous endoscopic discectomy: Surgical technique and preliminary results compared to microsurgical discectomy. J Neurosurg. 1993;78:216–25. doi: 10.3171/jns.1993.78.2.0216. [DOI] [PubMed] [Google Scholar]
- 21.McCulloch JA. Focus issue on lumbar disc herniation: Macro- and microdiscectomy. Spine (Phila Pa 1976) 1996;21:S45–56. doi: 10.1097/00007632-199612151-00005. [DOI] [PubMed] [Google Scholar]
- 22.Mirkovic SR, Schwartz DG, Glazier KD. Anatomic considerations in lumbar posterolateral percutaneous procedures. Spine (Phila Pa 1976) 1995;20:1965–71. doi: 10.1097/00007632-199509150-00001. [DOI] [PubMed] [Google Scholar]
- 23.Nystrom B. Experience of microsurgical compared with conventional technique in lumbar disc operations. Acta Neurol Scand. 1987;76:129–41. doi: 10.1111/j.1600-0404.1987.tb03556.x. [DOI] [PubMed] [Google Scholar]
- 24.Olszewski AD, Yaszemski MJ, White AA. The anatomy of the human lumbar ligamentum flavum.New observations and their surgical importance. Spine (Phila Pa 1976) 1996;21:2307–12. doi: 10.1097/00007632-199610150-00001. [DOI] [PubMed] [Google Scholar]
- 25.Onik G, Maroon J, Davis GW. Automated percutaneous discectomy at the L5-S1 level.Use of a curved cannula. Clin Orthop. 1989;238:71–6. [PubMed] [Google Scholar]
- 26.Perez-Cruet MJ, Foley KT, Isaacs RE, Rice-Wyllie L, Wellington R, Smith MM, et al. Microendoscopic lumbar discectomy: Technical note. Neurosurgery. 2002;51(Suppl 5):S129–36. [PubMed] [Google Scholar]
- 27.Reulan HD, Muller AD, Ebeling UD. Microsurgical anatomy of the lateral approach to extraforaminal lumbar disc herniations. Neurosurgery. 1996;39:345–51. doi: 10.1097/00006123-199608000-00022. [DOI] [PubMed] [Google Scholar]
- 28.Rompe JD, Eysel P, Zöllner J, Heine J. Intra- and postoperative risk analysis after lumbar intervertebral disc operation. Z Orthop Ihre Grenzgeb. 1999;137:201–5. doi: 10.1055/s-2008-1037393. [DOI] [PubMed] [Google Scholar]
- 29.Ruetten S, Komp M, Godolias G. An extreme lateral access for the surgery of lumbar disc herniations inside the spinal canal using the full-endoscopic uniportal transforaminal approach: Technique and prospective results of 463 patients. Spine (Phila Pa 1976) 2005;30:2570–8. doi: 10.1097/01.brs.0000186327.21435.cc. [DOI] [PubMed] [Google Scholar]
- 30.Ruetten S, Komp M, Godolias G. A new full-endoscopic technique for the interlaminar operation of lumbar disc herniations using 6 mm endoscopes: Prospective 2-year results of 331 patients. Minim Invasive Neurosurg. 2006;49:80–7. doi: 10.1055/s-2006-932172. [DOI] [PubMed] [Google Scholar]
- 31.Ruetten S, Komp M, Godolias G. Full-endoscopic interlaminar operation of lumbar disc herniations using new endoscopes and instruments. Orthop Praxis. 2005;10:527–32. [Google Scholar]
- 32.Ruetten S, Komp M, Merk H, Godolias G. Full-endoscopic interlaminar and transforaminal lumbar discectomy versus conventional microsurgical technique: A prospective, randomized, controlled study. Spine (Phila Pa 1976) 2008;33:931–9. doi: 10.1097/BRS.0b013e31816c8af7. [DOI] [PubMed] [Google Scholar]
- 33.Schick U, Döhnert J, Richter A, König A, Vitzthum HE. Microendoscopic lumbar discectomy versus open surgery: An intraoperative EMG study. Eur Spine J. 2002;11:20–6. doi: 10.1007/s005860100315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Siebert W. Percutaneous nucleotomy procedures in lumbar intervertebral disc displacement. Orthopade. 1999;28:598–608. doi: 10.1007/s001320050390. [DOI] [PubMed] [Google Scholar]
- 35.Stambough JL. Lumbar disc herniation: An analysis of 175 surgically treated cases. J Spinal Disord. 1997;10:488–92. [PubMed] [Google Scholar]
- 36.Suk KS, Lee HM, Moon SH, Kim NH. Recurrent lumbar disc herniation: Results of operative management. Spine (Phila Pa 1976) 2001;26:672–6. doi: 10.1097/00007632-200103150-00024. [DOI] [PubMed] [Google Scholar]
- 37.Tsou PM, Yeung AT. Transforaminal endoscopic decompression for radiculopathy secondary to intracanal noncontained lumbar disc herniations: Outcome and technique. Spine J. 2002;2:41–8. doi: 10.1016/s1529-9430(01)00153-x. [DOI] [PubMed] [Google Scholar]
- 38.Williams RW. Microlumbar discectomy. A 12-year statistical review. Spine (Phila Pa 1976) 1986;11:851–2. [PubMed] [Google Scholar]
- 39.Yenug AT, Tsou PM. Posterolateral endoscopic excision for lumbar disc herniation: Surgical technique, outcome and complications in 307 consecutive cases. Spine (Phila Pa 1976) 2002;27:722–31. doi: 10.1097/00007632-200204010-00009. [DOI] [PubMed] [Google Scholar]


