Introduction
In survivors of acute coronary syndromes (ACS; unstable angina or myocardial infarction), depression is highly prevalent [1] and increases the risk of adverse medical outcomes, independent of other prognostic risk markers [2,3]. After ACS, adherence to recommended medications (e.g. aspirin, statins and β-blockers) is crucial to prevent recurrent events or mortality [4,5,6], yet rates of adherence to these medications are poor [7,8,9]. Depressed patients are especially likely to be poorly adherent [8,9,10,11]. Thus, poor medication adherence may explain some of the increased risk of depression and adverse clinical outcomes after ACS.
We used data from 168 participants in the medication monitoring substudy [12] of the observational Coronary Psychosocial Evaluation Studies (COPES) [13] to test this hypothesis. This substudy included hospitalized ACS patients who were prescribed a daily dose of aspirin, neither used a weekly pillbox nor lived in a nursing home, and had a score of ≥10 or <5 on the Beck Depression Inventory [14] (see Rieckmann et al. [12] for study sample characteristics and eligibility criteria, and Davidson et al. [13] for details on outcome event ascertainment). Aspirin adherence over 90 days after hospital discharge was measured using the Medication Event Monitoring System (MEMS; APREX Corp., Fremont, Calif., USA) device. Each time the MEMS bottle is opened, the date and time is permanently recorded on a computer chip in the cap. Patients received a 90-day supply of their prescribed aspirin dose in an MEMS bottle. They were informed that their adherence was being monitored, but they did not receive adherence counseling. The outcome was the 1-year first occurrence of a major adverse cardiac event (MACE; nonfatal myocardial infarction, urgent cardiac revascularization or unstable angina hospitalization) or all-cause mortality (ACM). The study complies with the Declaration of Helsinki. The institutional review boards of each study site approved the study [12].
Adherence, defined as the percentage of days the correct number of pills (1) was taken, was computed across the first 7 days after discharge, the first month and the first 3 months. The percentage was subtracted from 100 to obtain the percentage of nonadherent days, so that the hazard ratios (HR) in the Cox proportional hazards models reflected risk associated with poorer adherence. For patients who had an MACE or who died in the first 3 months, adherence was computed up until the week of the event. Medical covariates included the Charlson comorbidity index [15] and left ventricular ejection fraction (normal/mild dysfunction: ≥40%; moderate/severe dysfunction: <40%) [16]. Partial correlations and Cox proportional hazards models were used, adjusting for age and sex, treating study site as stratum. All continuous predictors were standardized. The degree of mediation was assessed by the percent reduction in the Cox regression coefficient for depressive symptoms when aspirin adherence was included in the model.
The COPES parent study included 457 ACS patients, of which 172 took part in the aspirin monitoring study. Refusers of the monitoring study had higher levels of in-hospital depressive symptoms [12]. Four patients had an MACE within the first 7 days after discharge and were excluded from the present analyses. The mean age was 59.4 years (SD = 12.2 years), 45% of the patients were female and 86% white.
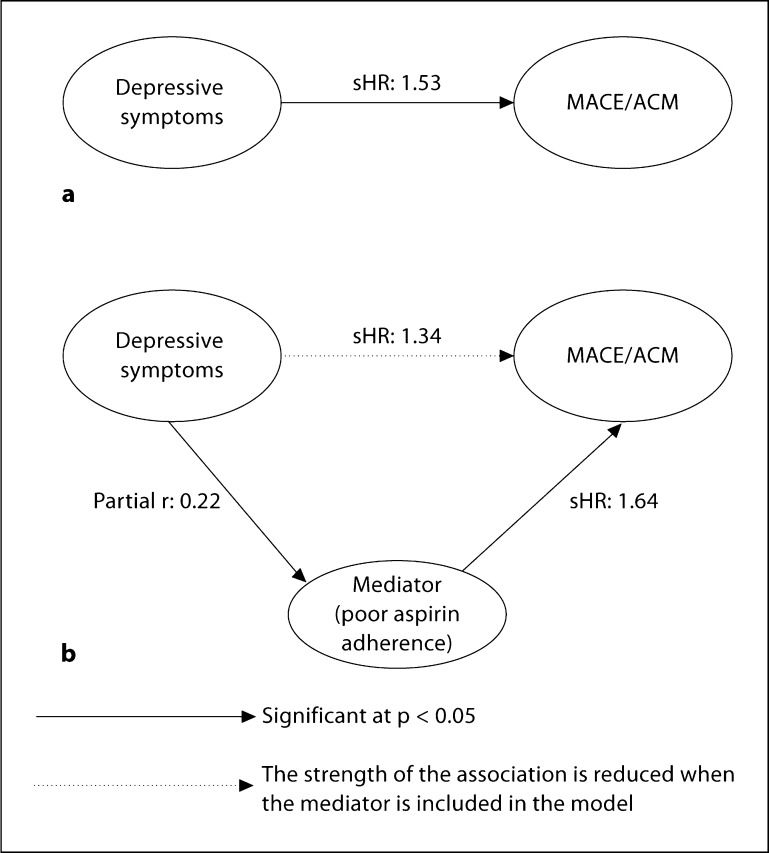
Controlling for age, sex and site, baseline depressive symptoms were significantly correlated with poorer 7-day, 1-month and 3-month aspirin adherence (partial r: 0.22, 0.26 and 0.19, respectively; all p < 0.02). After 1 year, there had been 14 MACE/ACM events (8%). Adjusting for age, sex and site, poorer 7-day (adjusted standardized HR, sHR: 1.76; CI: 1.14–2.73) and 1-month aspirin adherence (adjusted sHR: 1.75; CI: 1.18–2.60) as well as baseline depressive symptoms (adjusted sHR: 1.53; CI: 1.02–2.29) were each individually associated with 1-year MACE/ACM. A similar, yet nonsignificant association was found for poorer 3-month aspirin adherence (adjusted sHR: 1.45; CI: 0.97–2.17; p = 0.054). When both baseline depressive symptoms and 7-day aspirin adherence were entered into the age- and sex-adjusted model, the HR for depressive symptoms decreased substantially (adjusted sHR: 1.34; CI: 0.89–2.01), whereas poorer 7-day aspirin adherence remained a significant predictor (adjusted sHR: 1.64; CI: 1.06–2.54). The effect size for depressive symptoms decreased by 31% (fig. 1) when 7-day aspirin adherence was included in the analysis. Controlling for left ventricular ejection fraction and Charlson comorbidity index did not alter these results (data not shown). Similarly, poorer 1-month aspirin adherence decreased the effect size for baseline depressive symptoms by 29% (adjusted sHR for depressive symptoms: 1.37; CI: 0.88–2.13; adjusted sHR for poorer 1-month adherence: 1.65; CI: 1.11–2.45).
Fig. 1.
The effect of in-hospital depressive symptoms on MACE/ ACM is reduced by 31% when aspirin adherence is added as a predictor. The correlation and the HR are adjusted for age and sex, with study site treated as stratum. a Direct effect model. b Mediational model.
Depression in cardiac patients has been linked to several biological and behavioral dysregulations [16,17]. The present study shows that a modifiable patient behavior – medication adherence – may account for some of the clinical outcome risk associated with increased depressive symptoms after ACS. The Heart and Soul Study, which tested biological and behavioral depression mediators in a sample of 1,017 patients with stable coronary heart disease [18], found that self-reported medication adherence explained only a small portion (5%) of the association between depressive symptoms and future clinical events, as opposed to 31% in our study. However, different mechanisms may account for the increased risk in depressed stable heart disease patients (the population of the Heart and Soul Study) as compared to depressed ACS patients. Also, electronic monitoring in our study provided a more objective measure of adherence and yielded higher nonadherence rates in comparison to the Heart and Soul Study [12]. In addition, our follow-up was shorter than that in the Heart and Soul Study, and the impact of adherence on event-free survival may decrease over time.
Generalizability of the current study is limited by the relatively small sample size. Also, the study participants had lower levels of depressive symptoms than the study refusers [12], and the restriction of range may have attenuated both the associations between adherence and depression, and between depressive symptoms and MACE/ACM. It also remains to be shown whether poor aspirin adherence is a marker of overall poor medication adherence across all cardioprotective medications [6]. Lastly, it is possible that aspirin, due to anti-inflammatory effects, may reduce depressive symptoms. A recent case-control study of a sample of 345 community-dwelling women showed that the use of aspirin was associated with a significantly decreased incidence of major depressive disorder after the age of 50 years [19]. In the current COPES substudy, however, we had previously found that higher aspirin adherence was not associated with subsequent improvements in depressive symptoms over time; in fact, changes in depressive symptoms preceded changes in aspirin adherence, but not vice versa [12]. Still, it is possible that better aspirin adherence may lead to later changes in depressive symptoms in the long run. This will need to be explored in future studies with repeated assessments of depressive symptoms further away from the index ACS event.
In conclusion, this study provides evidence that poorer aspirin adherence may account for a substantial part of the excess prognostic risk associated with depressive symptoms after ACS. Promoting medication adherence in combination with depression treatment may more effectively improve the medical prognosis for depressed patients than simply treating depression.
Disclosure Statement
The authors have no conflict of interest to declare.
Acknowledgments
This study was supported by grants HC-25197, HL-088117, HL-76857 and HL-84034 from the National Institutes of Health (NIH), Bethesda, Md., USA, and by grant UL1 RR024156 from the National Center for Research Resources (NCRR), a component of the NIH and NIH Roadmap for Medical Research.
References
- 1.Thombs BD, Bass EB, Ford DE, Stewart KJ, Tsilidis KK, Patel U, Fauerbach JA, Bush DE, Ziegelstein RC. Prevalence of depression in survivors of acute myocardial infarction. J Gen Intern Med. 2006;21:30–38. doi: 10.1111/j.1525-1497.2005.00269.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Barth J, Schumacher M, Herrmann-Lingen C. Depression as a risk factor for mortality in patients with coronary heart disease: a meta-analysis. Psychosom Med. 2004;66:802–813. doi: 10.1097/01.psy.0000146332.53619.b2. [DOI] [PubMed] [Google Scholar]
- 3.van Melle JP, de Jonge P, Spijkerman TA, Tijssen JG, Ormel J, van Veldhuisen DJ, van den Brink RH, van den Berg MP. Prognostic association of depression following myocardial infarction with mortality and cardiovascular events: a meta-analysis. Psychosom Med. 2004;66:814–822. doi: 10.1097/01.psy.0000146294.82810.9c. [DOI] [PubMed] [Google Scholar]
- 4.DiMatteo MR, Giordani PJ, Lepper HS, Croghan TW. Patient adherence and medical treatment outcomes: a meta-analysis. Med Care. 2002;40:794–811. doi: 10.1097/00005650-200209000-00009. [DOI] [PubMed] [Google Scholar]
- 5.Hulten E, Jackson JL, Douglas K, George S, Villines TC. The effect of early, intensive statin therapy on acute coronary syndrome: a meta-analysis of randomized controlled trials. Arch Intern Med. 2006;166:1814–1821. doi: 10.1001/archinte.166.17.1814. [DOI] [PubMed] [Google Scholar]
- 6.Rasmussen JN, Chong A, Alter DA. Relationship between adherence to evidence-based pharmacotherapy and long-term mortality after acute myocardial infarction. JAMA. 2007;297:177–186. doi: 10.1001/jama.297.2.177. [DOI] [PubMed] [Google Scholar]
- 7.Ho PM, Spertus JA, Masoudi FA, Reid KJ, Peterson ED, Magid DJ, Krumholz HM, Rumsfeld JS. Impact of medication therapy discontinuation on mortality after myocardial infarction. Arch Intern Med. 2006;166:1842–1847. doi: 10.1001/archinte.166.17.1842. [DOI] [PubMed] [Google Scholar]
- 8.Carney RM, Freedland KE, Eisen SA, Rich MW, Jaffe AS. Major depression and medication adherence in elderly patients with coronary artery disease. Health Psychol. 1995;14:88–90. doi: 10.1037//0278-6133.14.1.88. [DOI] [PubMed] [Google Scholar]
- 9.Rieckmann N, Kronish IM, Haas D, Gerin W, Chaplin WF, Burg MM, Vorchheimer D, Davidson KW. Persistent depressive symptoms lower aspirin adherence after acute coronary syndromes. Am Heart J. 2006;152:922–927. doi: 10.1016/j.ahj.2006.05.014. [DOI] [PubMed] [Google Scholar]
- 10.DiMatteo MR, Lepper HS, Croghan TW. Depression is a risk factor for noncompliance with medical treatment: meta-analysis of the effects of anxiety and depression on patient adherence. Arch Intern Med. 2000;160:2101–2107. doi: 10.1001/archinte.160.14.2101. [DOI] [PubMed] [Google Scholar]
- 11.Gehi A, Haas D, Pipkin S, Whooley MA. Depression and medication adherence in outpatients with coronary heart disease: findings from the Heart and Soul Study. Arch Intern Med. 2005;165:2508–2513. doi: 10.1001/archinte.165.21.2508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rieckmann N, Gerin W, Kronish IM, Burg MM, Chaplin WF, Kong G, Lespérance F, Davidson KW. Course of depressive symptoms and medication adherence after acute coronary syndromes: an electronic medication monitoring study. J Am Coll Cardiol. 2006;48:2218–2222. doi: 10.1016/j.jacc.2006.07.063. [DOI] [PubMed] [Google Scholar]
- 13.Davidson KW, Burg MM, Kronish IM, Shimbo D, Dettenborn L, Mehran R, Vorchheimer D, Clemow L, Schwartz JE, Lespérance F, Rieckmann N. Association of anhedonia with recurrent major adverse cardiac events and mortality 1 year after acute coronary syndrome. Arch Gen Psychiatry. 2010;67:480–488. doi: 10.1001/archgenpsychiatry.2010.36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Beck AT, Steer RA. Manual for the Beck Depression Inventory. San Antonio: Psychological Corporation; 1993. [Google Scholar]
- 15.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 16.Carney RM, Freedland KE, Miller GE, Jaffe AS. Depression as a risk factor for cardiac mortality and morbidity: a review of potential mechanisms. J Psychosom Res. 2002;53:897–902. doi: 10.1016/s0022-3999(02)00311-2. [DOI] [PubMed] [Google Scholar]
- 17.Skala JA, Freedland KE, Carney RM. Coronary heart disease and depression: a review of recent mechanistic research. Can J Psychiatry. 2006;51:738–745. doi: 10.1177/070674370605101203. [DOI] [PubMed] [Google Scholar]
- 18.Whooley MA, de Jonge P, Vittinghoff E, Otte C, Moos R, Carney RM, Ali S, Dowray S, Na B, Feldman MD, Schiller NB, Browner WS. Depressive symptoms, health behaviors, and risk of cardiovascular events in patients with coronary heart disease. JAMA. 2008;300:2379–2388. doi: 10.1001/jama.2008.711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pasco JA, Jacka FN, Williams LJ, Henry MJ, Nicholson GC, Kotowicz MA, Berk M. Clinical implications of the cytokine hypothesis of depression: the association between use of statins and aspirin and the risk of major depression. Psychother Psychosom. 2010;79:323–325. doi: 10.1159/000319530. [DOI] [PubMed] [Google Scholar]