Abstract
Objective:
To determine the incidence and risk factors of secondary cataract.
Materials and methods:
A retrospective study involving a review of medical records in the ophthalmology unit of the Yaoundé Gynaeco-obstetric and Paediatric Hospital in Yaoundé, Cameroon, was carried out. All patients who had cataract surgery between January 2006 and September 2010 were included. Variables included age, sex, past medical history, morphology of primary cataract, type of surgery, intraocular lens implantation, site of implantation, intra- and postoperative complications, and the time lapse for the presentation of secondary cataract. Both univariate and bivariate analyses were carried out. The χ2 test was used to compare proportions, and P-values <0.05 were considered statistically significant.
Results:
A total of 864 eyes of 718 patients had cataract surgery. Ninety-two eyes developed posterior capsule opacification, giving an incidence of 10.65%. The mean age of patients who developed secondary cataract was 52.3 ± 23.05 years, with a range of 4 years to 84 years. Secondary cataract was more frequent in the age group of 0–20 years. The time lapse for presentation of secondary cataract was 64.7 ± 9.53 days, with a range of 1 to 504 days. Risk factors for the development of secondary cataract were age (P = 0.000), sex (P = 0.011), cortical cataract (P = 0.000), and postoperative inflammation (P = 0.000).
Conclusion:
The incidence of secondary cataract, though high in this study, is lower than that reported in other studies.
Keywords: cataract, secondary cataract, incidence, Cameroon
Introduction
Manual extracapsular extraction is the most frequently used surgical technique in the management of cataract in developing countries.1–3 Posterior capsule opacification, which is also known as secondary cataract, is the most frequent complication following this technique.4,5 Secondary cataract is the proliferation and migration of residual epithelial cells into the visual axis, causing a decrease in visual acuity.4 It is an unpredictable and inevitable complication. Its incidence varies in the literature from 10% to 50% by 3 to 5 years after surgery.4,6–8 Significant risk factors for the development of secondary cataract include age, type of surgical technique, lack of posterior chamber intraocular lens (IOL), poor preoperative dilatation, large IOL optic diameter (7 mm), lens material, lens design, experience of the surgeon, and persistence of cortical material.7,9
Treatment is mainly by neodymium:yttrium aluminum garnet (Nd:YAG) laser capsulotomy.7 However, this is not available in most ophthalmology units in Cameroon due to the cost. Even when available, the high cost of treatment, which is estimated at about €125, is not affordable by the majority of the population. Laser capsulotomy may lead to complications such as retinal detachment, secondary glaucoma, macular edema, and IOL damage or dislocation.10
Knowledge of the incidence and risk factors in our setting is essential in the prevention of secondary cataract.
The objectives of this study were therefore to determine the incidence, risk factors, and time lapse for the development of secondary cataract at the Yaoundé Gynaeco-obstetric and Paediatric Hospital in Yaoundé, Cameroon.
Patients and methods
All the medical records of patients who consulted the ophthalmology unit of the Yaoundé Gynaeco-obstetric and Paediatric Hospital were reviewed. Patients included were both males and females of all ages who underwent cataract surgery in one or both eyes between January 2006 and September 2010.
All patients had received a comprehensive ophthalmic examination including visual acuity testing, refraction, slit-lamp examination of the anterior segment, posterior segment examination using a 78D Volk lens or Gold-mann three-mirror contact lens, and intraocular pressure measurement using a noncontact tonometer. Younger children were examined under general anesthesia after a pediatric consultation that aimed at finding any systemic associations.
At the end of the examination, cataract was classified with respect to laterality (unilateral, bilateral), etiology (congenital, traumatic, complicated, or age related), and morphology of the opacity (white, cortical, nuclear, posterior subcapsular). Indication for surgery was either to improve vision or to prevent amblyopia.
Surgical technique used was either the conventional extracapsular cataract extraction (ECCE) or manual small incision cataract surgery (MSICS), which is a variant of the conventional ECCE. Phacoemulsification is not carried out in our setting due to lack of equipment and expertise. Peribulbar block was done with a combination of 3 mL of bupivacaine 0.5% and 3 mL of lidocaine 2% in adults, and general anesthesia with propofol was used in children. The lens was replaced by a polymethyl methacrylate IOL when implantation was possible.
Postoperative treatment included topical administration of a combination of corticosteroid (dexamethasone 0.1%) and antibiotics (neomycin and polymyxin B) as well as a mydriatic (tropicamide 0.5%). Postoperative follow-up consisted of the measurement of visual acuity and the search for early or late complications, including a posterior capsule opacification (secondary cataract). For bilateral cataracts, the second eye was operated on after an interval of 2 months. Patients with secondary cataract were referred for Nd:Yag laser posterior capsulotomy at the Douala General Hospital (located about 250 km from Yaoundé). The cost was about €125, excluding transportation.
Variables studied were epidemiologic (age, sex), clinical (etiology, morphology of primary cataract), therapeutic (type of surgery, presence of IOL, implantation site, intra- and postoperative complications), and the time lapse for the development of secondary cataract. Data were analyzed using SPSS software for Windows, version 16.0 (SPSS, Inc., Chicago, IL). Both univariate and bivariate analyses were carried out. The χ2 test was used to compare proportions, and P-values <0.05 were considered statistically significant.
Results
Epidemiologic characteristics of secondary cataract
A total of 864 eyes of 718 patients, including 363 females and 355 males, had cataract surgery between 2006 and 2010, amongst whom 92 eyes (85 patients) developed a secondary cataract. The incidence as a percentage of operated patients and eyes was 11.8% and 10.65, respectively (Table 1). There were more females than males (P = 0.011) (Table 2).
Table 1.
Incidence of secondary cataract
| Cataract surgery (n) |
Secondary cataract |
||
|---|---|---|---|
| n | % | ||
| Number of patients | 718 | 85 | 11.84 |
| Number of eyes | 864 | 92 | 10.65 |
Table 2.
Distribution of secondary cataract according to sex
| Sex | Patients operated (n) |
Secondary cataract |
|
|---|---|---|---|
| n | % | ||
| Males | 355 | 31 | 8.73 |
| Females | 363 | 54 | 14.88 |
| Total | 718 | 85 | 11.84 |
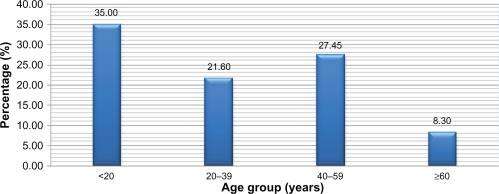
The mean age was 52.30 ± 23.05 years with a range from 4 to 84 years. Secondary cataract was more frequent in patients aged below 20 years (P = 0.000) (Figure 1).
Figure 1.
Distribution of secondary cataract according to age.
Clinical aspects
Preoperative visual acuity amongst eyes that developed secondary cataract was between light perception and 0.2 in 95.65% of cases (n = 88). Amongst all operated cataracts, age-related cataract was the most frequent, representing 73.40% of cases (n = 634/864). The incidence of secondary cataract was higher amongst cases with congenital and traumatic cataracts (P = 0.066) (Table 3). White cataract was the most frequent morphology, constituting 61.60% of cases (n = 532/864), and secondary cataract occurred more frequently amongst cases with cortical cataract (P = 0.000) (Table 4). The right and left eyes were affected in equal proportions of 10.69% (48/449) and 10.60% (44/415), respectively (P = 0.967).
Table 3.
Distribution of secondary cataract according to etiology of primary cataract
| Patients operated (n) |
Secondary cataract |
||
|---|---|---|---|
| Frequency | % | ||
| Age related | 634 | 58 | 9.14 |
| Post-traumatic | 124 | 19 | 15.32 |
| Congenital | 72 | 12 | 16.67 |
| Iatrogenic | 34 | 3 | 8.82 |
Table 4.
Secondary cataract according to the morphology of primary cataract
| Eyes operated (n) |
Secondary cataract |
||
|---|---|---|---|
| n | % | ||
| White | 532 | 49 | 9.20 |
| Cortical | 48 | 15 | 31.25 |
| Posterior subcapsular | 171 | 13 | 7.60 |
| Nuclear | 113 | 15 | 13.27 |
MSICS was the most frequently performed surgical technique (70.6% [n = 610/864]), and IOL implantation in the capsular bag was carried out in 783 of the 829 operated eyes (94.5%). The occurrence of secondary cataract was not influenced by the surgical technique (MSICS = 63/610, 10.3%; standard ECCE = 29/254, 11.4%) (P = 0.964).
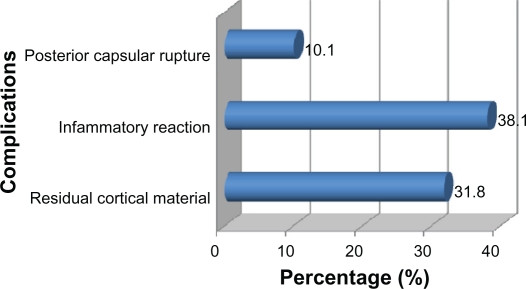
A total of 38.1% of those with postoperative inflammation and 10.1% of those with posterior capsule rupture developed secondary cataract. Postoperative inflammation was associated with the occurrence of secondary cataract (P = 0.000) (Figure 2). The mean time lapse for the presentation of secondary cataract was 64.7 ± 99.53 days, with a range of 1 to 504 days. Time lapse was greater than 30 days in 56.5% (n = 52/92) of cases, and less than 30 days in 43.5% (n = 40/92) of cases. This difference was not statistically significant (P = 0.211).
Figure 2.
Distribution of secondary cataract according to intra- and postoperative complications.
Secondary cataract developed in 15.2% of cases (84/783) in whom IOL was implanted in the sulcus compared with 10.7% of cases (7/46) in whom implantation was carried out in the capsular bag, but this difference was not statistically significant (P = 0.344). Secondary cataract was symptomatic in 65.2% of cases and discovered on routine examination in 34.8% of cases (P = 0.004).
Discussion
Epidemiologic characteristics of secondary cataract
The incidence of secondary cataract in the literature ranges from 10% to 50% after 3 to 5 years.4,6,7,11–13 The incidence in this series was 10.65%. Guzek and Ching14 in Ghana and Yorston and Foster15 in Kenya reported values of 10.5% and 10.8%, respectively. Bensaid et al16 however, reported an incidence of 33% in north Cameroon, and Shrestha et al17 reported an incidence of 59.3% in Nepal refugee camps. Our value is higher than the 4.7% reported by Muhammad et al18 in Pakistan. Factors such as age, etiology of cataract, type of surgery, and duration of postoperative follow-up could account for these differences.19,20
The mean age of patients who developed secondary cataract was 52.30 ± 23.05 years. This is similar to the 57.43 ± 13.53 years reported by Daboué et al11 in Burkina Faso and lower than the 65.08 years reported by Georgalas et al21 and the 60 years reported by Prajna et al22 in India. This difference could be due to the relative low life expectancy in sub-Saharan countries. Secondary cataract was more frequent in patients aged below 20 years. The incidence of secondary cataract has been reported to be higher in young patients with values near 100% after 3 years.23,24 There is greater residual lens epithelial cell proliferation and severe inflammatory reaction in young patients, which are major mechanisms by which secondary cataract occurs.7
Secondary cataract was more frequent in female patients. A similar finding was reported by Prajna et al.23
Characteristics of primary cataract
Age-related cataract was the most frequent of all operated cataracts. It is the most common etiology of cataracts.25–27 The occurrence of secondary cataract was more frequent in congenital and post-traumatic cataract than age-related cataract. However, this difference was nonsignificant (P = 0.066). Several authors report that close to 100% of cases with congenital and post-traumatic cataract develop a secondary cataract.28–31 Patients with congenital cataract are young and therefore have greater epithelial cell proliferation and severe inflammatory reaction. On the other hand, trauma stimulates residual lens cells, increasing cytokine production, which is responsible for secondary cataract.7,21,32
In this series, secondary cataract was more frequent in cases with cortical cataract. Schein et al33 reported a similar finding. In an experimental study reported by Argento et al,34 secondary cataract was least frequent with white cataract, as cataract maturity induces changes in the anterior and equatorial cells, which are responsible for posterior capsular opacification.
Surgical technique
There was no statistically significant difference in the development of secondary cataract between conventional ECCE and MSICS. Similar results were reported by Moulick et al20 in India (standard or conventional ECCE = 28.1%, MSICS = 15.4%, P = 0.69) and Guzek and Ching14 in Ghana (MSICS = 21.9%, conventional ECC = 12.5%; P = 0.127). Surgical technique is therefore not a risk factor for the development of secondary cataract.
There was no statistically significant difference in the development of secondary cataract between eyes with sulcus implantation and those with capsular bag implantation.
According to Ayed et al,9 sulcus implantation is a risk factor of secondary cataract development, because it may trigger uveal reaction and blood–aqueous barrier breakdown. They concluded that capsular bag implantation could prevent the development of secondary cataract.
Postoperative complications
The occurrence of secondary cataract was statistically linked to postoperative inflammatory reaction (P = 0.000). This relationship was reported by Ayed et al.9 Postoperative inflammation might stimulate capsular opacification by the release of mediators such as transforming growth factor β, interleukin, and basic fibroblast growth factor.32
Secondary cataract: time lapse and symptoms
The mean time lapse for secondary cataract development was 64.7 ± 99.53 days. This period is below the 10 months reported by Georgalas et al.21 No explanation for this differerence has been found.
According to Pandey et al,35 visual impairment does not correlate with the degree of posterior capsular opacification. Some patients are asymptomatic with an advanced fibrosis, whereas others present a significant decrease in visual acuity in spite of a lesser degree of fibrosis. In this study, two-thirds of patients were symptomatic.
Conclusion
The incidence of secondary cataract is high in our series, but it is lower than that in other studies. Risk factors in our setting include cortical cataract, post-traumatic cataract, congenital cataract, and postoperative intraocular inflammation. Thorough cortical clean-up will help reduce the incidence of secondary cataract.
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Fany A, Keita CT, Adjorlolo AC, et al. Accessibilité à l’intervention chirurgicale de la cataracte dans les pays en développement nos résultats des 6 derniers mois CHU de Treichville–Abidjan–Cote d’Ivoire. Médecine d’Afrique Noire. 2001;48:26–29. [Google Scholar]
- 2.Doutetien C, Traore J, Bassabi SK, Auzemery A. La chirurgie de la cataracte à l’IOTA de Bamako. Le Bénin Médical. 1999;12/13:45–52. [Google Scholar]
- 3.Lawani R, Pommier S, Roux L, et al. Magnitude et stratégies de prise en charge de la cataracte dans le monde. Med Trop. 2007;67:644–650. [PubMed] [Google Scholar]
- 4.Apple DJ, Solomon KD, Tetz MR, et al. Posterior capsule opacification. Surv Ophthalmol. 1992;37:73–116. doi: 10.1016/0039-6257(92)90073-3. [DOI] [PubMed] [Google Scholar]
- 5.Sandford-Smith J. La chirurgie de la cataracte in Chirurgie oculaire sous les climats chauds. International Centre for Eye Health (ICEH) 2006;5:81–200. [Google Scholar]
- 6.Flament J. Ophtalmologie, Pathologie du Système Visuel. Paris, France: Masson; 2002. p. 197. [Google Scholar]
- 7.Flament J, Lenoble P. Encycl Med Chir Ophtalmologie. Paris, France: Elsevier; 1997. Cataracte secondaire. [Google Scholar]
- 8.Schaumberg DA, Reza Dana M, Christen WG, Glynn RJ. A systematic overview of the incidence of posterior capsule opacification. Ophthalmology. 1998;105:1213–1221. doi: 10.1016/S0161-6420(98)97023-3. [DOI] [PubMed] [Google Scholar]
- 9.Ayed T, Rannen R, Naili K, et al. Les facteurs de risque de la cataracte secondaire: étude cas-témoins avec analyse multivariée. J Fr Ophtalmol. 2002;25:615–620. [PubMed] [Google Scholar]
- 10.Arné J-L. Complications de la chirurgie de la cataracte. J Fr Ophtalmol. 2000;23:62. [PubMed] [Google Scholar]
- 11.Daboué A, Meda ND, Ahnoux-Zabsonre A, et al. Complications de l’implantation de cristallin artificiel en chambre postérieure. Médecine d’Afrique Noire. 2002;49:161–165. [Google Scholar]
- 12.Mahmoud BA, Mansur MR, Yinka OO. Long-term complications of extracapsular cataract extraction with posterior chamber intraocular lens implantation, in Nigeria. Int Ophthalmol. 2004;25:27–31. doi: 10.1023/b:inte.0000018526.45216.31. [DOI] [PubMed] [Google Scholar]
- 13.Borzeix A, Rivaud C, Lam A, et al. L’implantation de chambre postérieure en Afrique noire. A propos de 150 cas suivis pendant 18 mois. J Fr Ophtalmol. 1993;16:663–667. [PubMed] [Google Scholar]
- 14.Guzek JP, Ching A. Small-incision manual extracapsular cataract surgery in Ghana, West Africa. J Cataract Refract Surg. 2003;29:57–64. doi: 10.1016/s0886-3350(02)01440-2. [DOI] [PubMed] [Google Scholar]
- 15.Yorston D, Foster A. Audit of extracapsular cataract extraction and posterior chamber lens implantation as a routine treatment for age related cataract in east Africa. Br J Ophthalmol. 1999;83:897–901. doi: 10.1136/bjo.83.8.897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bensaid P, Bella L, Stork L. Ophtalmo Sans Frontières au Nord-Cameroun: évaluation des cataractes secondaires dans 4 centres pendant 6 mois. J Fr Ophtalmol. 2003;26:1S271. [Google Scholar]
- 17.Shrestha JK, Pradhan YM, Snellingen T. Outcomes of extracapsular surgery in eye camps of eastern Nepal. Br J Ophthalmol. 2001;85:648–652. doi: 10.1136/bjo.85.6.648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Khan MT, Jan S, Hussain Z, et al. Visual outcome and complications of manual sutureless small incision cataract surgery. Pak J Ophthalmol. 2010;26:32–39. [Google Scholar]
- 19.El Kettani, Lahlou G, Mazzouz H, et al. Cataractes post-traumatiques de l’enfant au Maroc. J Fr Ophtalmol. 2009;32:26. [Google Scholar]
- 20.Moulick PS, Rodrigues FEA, Shyamsundar K. Evaluation of posterior capsular opacification following different cataract surgery techniques. MJAFI. 2009;65:225–228. doi: 10.1016/S0377-1237(09)80008-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Georgalas I, Petrou P, Kalantzis G, et al. Nd:YAG capsulotomy for posterior capsule opacification after combined clear corneal phacoemulsification and vitrectomy. Ther Clin Risk Manag. 2009;5:133–137. doi: 10.2147/tcrm.s4754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Prajna NV, Ellwein LB, Selvaraj S, et al. The Madurai intraocular lens study IV: posterior capsule opacification. Am J Ophthalmol. 2000;130:304–309. doi: 10.1016/s0002-9394(00)00481-5. [DOI] [PubMed] [Google Scholar]
- 23.Yakoubi S, Baba A, Ghorbel M, et al. La cataracte secondaire chez l’enfant: choix de la technique chirurgicale: à propos de 108 cas. J Fr Ophtalmol. 2009;32:1S29. [Google Scholar]
- 24.Lam A, Seck CM, Gueye NN, et al. Chirurgie de la cataracte avec implantation en chambre postérieure chez l’enfant de moins de 15 ans au Sénégal. J Fr Ophtalmol. 2001;24:590. [PubMed] [Google Scholar]
- 25.Lawani R, Pommier S, Roux L, et al. Magnitude et stratégies de prise en charge de la cataracte dans le monde. Med Trop. 2007;67:644–650. [PubMed] [Google Scholar]
- 26.Negrel A-D, Khazraji YC, Azelmat M. La cataracte cécitante au Maroc. Med Trop. 1995;55:421–424. [PubMed] [Google Scholar]
- 27.Dawson CR, Schwab IR. Epidémiologie de la cataracte-importante cause de cécité évitable. Bulletin de l’Organisation Mondiale de la Santé. 1981;59:827–836. [Google Scholar]
- 28.Fagerholm PP, Philipson BT. Experimental traumatic cataract II. A transmission electron microscopy and extracellular tracer study. Invest Ophthalmol Vis Sci. 1979;18:1160–1171. [PubMed] [Google Scholar]
- 29.Zaman M, Iqbal S, Sannaullah, Khan MD. Frequency and visual outcome of traumatic cataract. JPMI. 2006;20:330–334. [Google Scholar]
- 30.Eckstein M, Vijayalakshmi P, Killedar M, et al. Use of intraocular lenses in children with traumatic cataract in south India. Br J Ophthalmol. 1998;82:911–915. doi: 10.1136/bjo.82.8.911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Baklouti K, Mhiri N, Mghaieth F, El Matri L. Les cataractes traumatiques: aspects cliniques et thérapeutiques. Bull Soc Belge Ophtalmol. 2005;298:13–17. [PubMed] [Google Scholar]
- 32.Meacock WR, Spalton DJ, Stanford MR. Role of cytokines in the pathogenesis of posterior capsule opacification. Br J Ophthalmol. 2000;84:332–336. doi: 10.1136/bjo.84.3.332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Schein OD, Steinberg EP, Javitt JC, et al. Variation in cataract surgery. Practice and clinical outcomes. Ophthalmology. 1997;101:1142–1152. doi: 10.1016/s0161-6420(94)31209-7. [DOI] [PubMed] [Google Scholar]
- 34.Argento C, Nunez E, Wainsztrein R. Incidence of post operative posterior capsular opacification with types of senile cataracts. J Cataract Refract Surg. 1992;18:586–588. doi: 10.1016/s0886-3350(13)80448-8. [DOI] [PubMed] [Google Scholar]
- 35.Pandey SK, Apple DJ, Werner L. Posterior capsule opacification: a review of the aetiopathologenesis experimental and clinical studies and factors for prevention. India J Ophthalmol. 2004;52:99–112. [PubMed] [Google Scholar]